Unplanned Absenteeism: The Role of Workplace and Non-Workplace Stressors
Abstract
:1. Introduction
2. Materials and Methods
3. Results
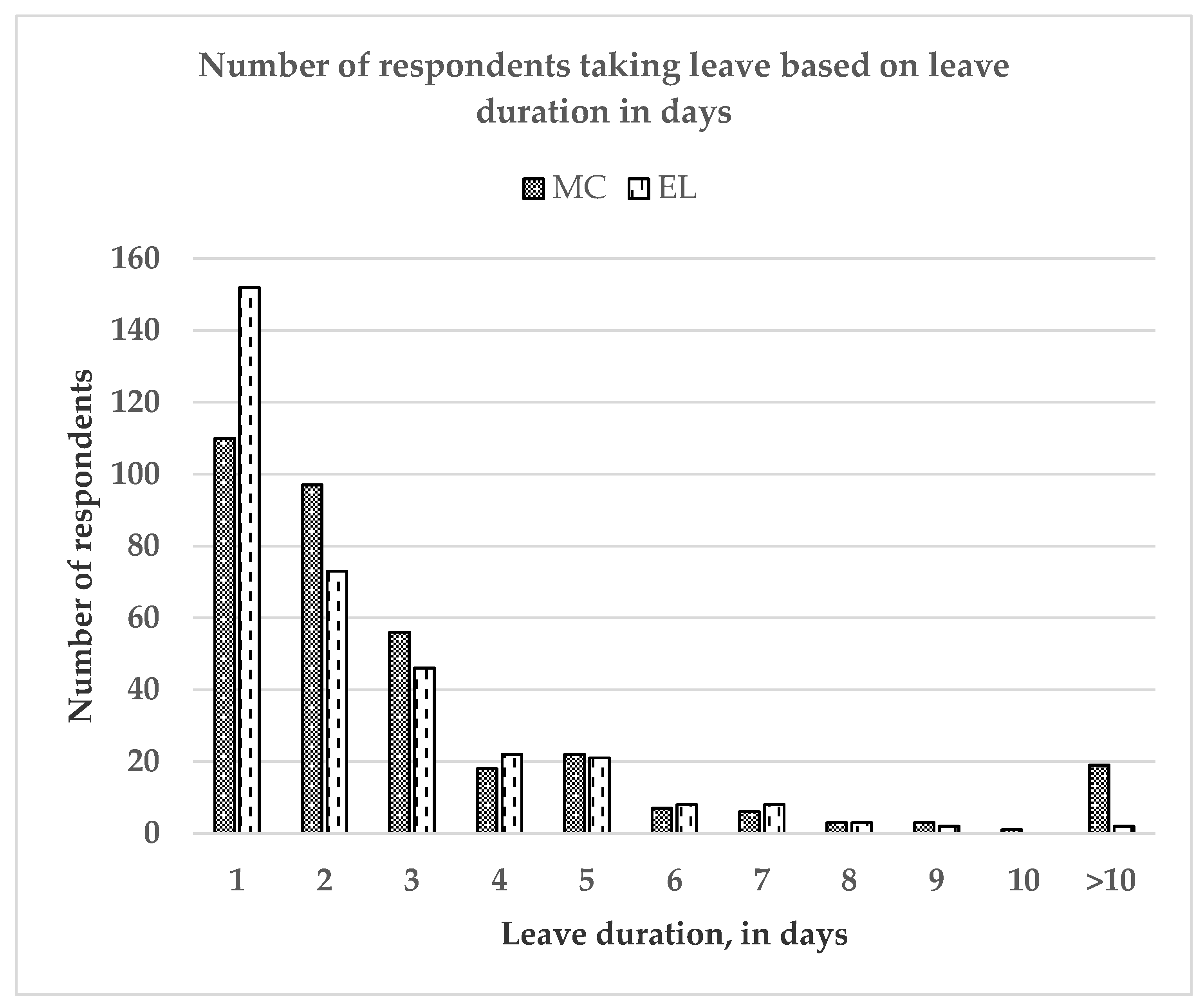
3.1. Descriptive Statistics
3.2. Predictors of Those Taking MC, Taking EL, Those Taking MC and EL, and Those neither Take MC nor EL
3.3. Predictors of Durations in Days of MC and EL among Those Who Ever Took MC and EL
3.4. Predictors of Frequency of MC and EL among Those Who Ever Took MC and EL
4. Discussions
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Daouk-Öyry, L.; Anouze, A.L.; Otaki, F.; Dumit, N.Y.; Osman, I. The JOINT model of nurse absenteeism and turnover: A systematic review. Int. J. Nurs. Stud. 2014, 51, 93–110. [Google Scholar] [CrossRef] [PubMed]
- Belita, A.; Mbindyo, P.; English, M. Absenteeism amongst health workers—Developing a typology to support empiric work in low-income countries and characterizing reported associations. Hum. Resour. Health 2013, 11, 34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bermingham, C. Employee’s Understanding of Workplace Absenteeism and the Investigation of Stress as a Contributing Factor. Bachelor’s Thesis, National College of Ireland, Dublin, Ireland, 2013. [Google Scholar]
- Davey, M.M.; Cummings, G.; Newburn-Cook, C.V.; Lo, E.A. Predictors of nurse absenteeism in hospitals: A systematic review. J. Nurs. Manag. 2009, 17, 312–330. [Google Scholar] [CrossRef] [PubMed]
- Becker, S.G.; Oliveira, M.L.C.D. Study on the Absenteeism of Nursing Professionals in a Psychiatric Center in Manaus, Brazil. Rev. Lat. Am. Enferm. 2008, 16, 109–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manzi, F.; Schellenberg, J.A.; Hutton, G.; Wyss, K.; Mbuya, C.; Shirima, K.; Mshinda, H.; Tanner, M.; Schellenberg, D. Human resources for health care delivery in Tanzania: A multifaceted problem. Hum. Resour. Health 2012, 10, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gaudine, A.; Gregory, C. The accuracy of nurses’ estimates of their absenteeism. J. Nurs. Manag. 2010, 18, 599–605. [Google Scholar] [CrossRef]
- Gimeno, D.; Felknor, S.A.; Burau, K.D.; Delclos, G.L.; Barrientos-Gutiérrez, T. Association of occupation and safety practices with work-injury absence among public hospital employees in Latin America: A study from Costa Rica. Inj. Prev. 2007, 13, 264–269. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Human Resource Malaysia. Employment Act, Section 60F; Ministry of Human Resource Malaysia: Federal Territory of Kuala Lumpur, Malaysia, 1955. [Google Scholar]
- Ministry of Human Resource. General Order of Malaysia; Percetakan Nasional Malaysia Berhad: Federal Territory of Kuala Lumpur, Malaysia, 2000. [Google Scholar]
- Groenewold, M.; Burrer, S.; Ahmed, F.; Uzicanin, A. National Surveillance for Health-Related Workplace Absenteeism, United States 2017-18. Online J. Public Health Inform. 2019, 11, 11. [Google Scholar] [CrossRef] [Green Version]
- Rantanen, I.; Tuominen, R. Relative magnitude of presenteeism and absenteeism and work-related factors affecting them among health care professionals. Int. Arch. Occup. Environ. Health 2011, 84, 225–230. [Google Scholar] [CrossRef]
- Saruan, N.A.; Yusoff, H.M.; Fauzi, M.F. Family responsibilities and involuntary job Absenteeism among nurses in teaching hospital. Malays. J. Public Health Med. 2019, 19, 38–46. [Google Scholar]
- Tripathi, M.; Mohan, U.; Tripathi, M.; Verma, R.; Masih, L.; Pandey, H.C. Absenteeism among nurses in a tertiary care hospital in India. Natl. Med. J. India. 2010, 23, 143–146. [Google Scholar] [PubMed]
- Tomey, A.M. Guide to nursing management and leadership. Aust. Nurs. Midwifery J. 2008, 15, 41. [Google Scholar]
- Ministry of Health, Malaysia. Health Indicators. 2018. Available online: http://www.moh.gov.my/moh/resources/.pdf (accessed on 16 February 2020).
- Bodenheimer, T.; Bauer, L. Rethinking the primary care workforce—an expanded role for nurses. N. Engl. J. Med. 2016, 375, 1015–1017. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yaacob, S.S.; Shaarial, S.Z.M.; Noor, N.M.; Ismail, K.I.; Selvaraju, R.; Gani, H.A. Prevalence of Sickness Absence and Its Sociodemographic and Occupational Factors in a Public Service Organization. KnE Life Sci. 2018, 4, 687–696. [Google Scholar] [CrossRef]
- Wee, L.H.; Yeap, L.L.; Chan, C.M.; Wong, J.E.; Jamil, N.A.; Nantha, Y.S.; Siau, C.S. Anteceding factors predicting absenteeism and presenteeism in urban area in Malaysia. BMC Public Health 2019, 19, 540. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holmgren, K.; Fjällström-Lundgren, M.; Hensing, G. Early identification of work-related stress predicted sickness absence in employed women with musculoskeletal or mental disorders: A prospective, longitudinal study in a primary health care setting. Disabil. Rehabil. 2013, 35, 418–426. [Google Scholar] [CrossRef]
- Heo, Y.S.; Leem, J.H.; Park, S.G.; Jung, D.Y.; Kim, H.C. Job stress as a risk factor for absences among manual workers: A 12-month follow-up study. Ind. Health 2015, 53, 542–552. [Google Scholar] [CrossRef]
- Thorsen, S.V.; Pedersen, J.; Flyvholm, M.A.; Kristiansen, J.; Rugulies, R.; Bültmann, U. Perceived stress and sickness absence: A prospective study of 17,795 employees in Denmark. Int. Arch. Occup. Environ. Health 2019, 92, 821–828. [Google Scholar] [CrossRef] [Green Version]
- Duclay, E.; Hardouin, J.B.; Sébille, V.; Anthoine, E.; Moret, L. Exploring the impact of staff absenteeism on patient satisfaction using routine databases in a university hospital. J. Nurs. Manag. 2015, 23, 833–841. [Google Scholar] [CrossRef]
- Atefi, N.; Abdullah, K.L.; Wong, L.P. Job satisfaction of Malaysian registered nurses: A qualitative study. Nurs. Crit. Care 2016, 21, 8–17. [Google Scholar] [CrossRef]
- Mbombi, M.O.; Mothiba, T.M.; Malema, R.N.; Malatji, M. The effects of absenteeism on nurses remaining on duty at a tertiary hospital of Limpopo province. Curationis 2018, 41, e1–e5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Department of Statistics, Malaysia. Population Distribution and Basic Demographic Characteristic Report 2010. 2011. Available online: www.dosm.gov.my (accessed on 16 February 2020).
- Department of Statistics, Malaysia. Buku Tahunan Perangkaan Malaysia. 2019. Available online: www.dosm.gov.my (accessed on 16 February 2020).
- Kish, L. Survey Sampling; John Wiley & Sons, Inc.: New York, NY, USA, 1965. [Google Scholar]
- Rokiah, M. Prevalence and Causes of Occupational Stress among Staff Nurses in HKL. Master’s Thesis, Universiti Kebangsaan Malaysia, Federal Territory of Kuala Lumpur, Malaysia, 1994. [Google Scholar]
- Rosnawati, M.R.; Moe, H.; Masilamani, R.; Darus, A. The Bahasa Melayu version of the Nursing Stress Scale among nurses: A reliability study in Malaysia. Asia Pac. J. Public Health. 2010, 22, 501–506. [Google Scholar] [CrossRef] [PubMed]
- Kang, H. The prevention and handling of the missing data. Korean J. Anesthesiol. 2013, 64, 402. [Google Scholar] [CrossRef] [PubMed]
- Oche, M.O.; Oladigbolu, R.A.; Ango, J.T.; Okafoagu, N.C.; Ango, U.M. Work Absenteeism amongst Health Care Workers in a Tertiary Health Institution in Sokoto, Nigeria. J. Adv. Med. Med. Res. 2018, 26, 1–9. [Google Scholar] [CrossRef]
- Isah, E.C.; Omorogbe, V.E.; Orji, O.; Oyovwe, L. Self-reported absenteeism among hospital workers in Benin city, Nigeria. Ghana Med. J. 2008, 42, 2–7. [Google Scholar] [PubMed]
- King, R.B.; Karuntzos, G.; Casper, L.M.; Moen, P.; Davis, K.D.; Berkman, L.; Durham, M.; Kossek, E.E. Work–Family Balance Issues and Work–Leave Policies. In Handbook of Occupational Health and Wellness; Springer: Boston, MA, USA, 2012; pp. 323–339. [Google Scholar]
- Josephson, M. The same factors influence job turnover and long spells of sick leave—A 3-year follow-up of Swedish nurses. Eur. J. Public Health 2008, 18, 380–385. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fekedulegn, D.; Burchfiel, C.M.; Hartley, T.A.; Andrew, M.E.; Charles, L.E.; Tinney-Zara, C.A.; Violanti, J.M. Shiftwork and sickness absence among police officers: The BCOPS study. Chronobiol. Int. 2013, 30, 930–941. [Google Scholar] [CrossRef] [Green Version]
- Kivimaki, M. Sickness absence in hospital physicians: 2 year follow up study on determinants. Occup. Environ. Med. 2001, 58, 361–366. [Google Scholar] [CrossRef] [Green Version]
- Burch, J.B.; Tom, J.; Zhai, Y.; Criswell, L.; Leo, E.; Ogoussan, K. Shiftwork impacts and adaptation among health care workers. Occup. Med. 2009, 59, 159–166. [Google Scholar] [CrossRef] [Green Version]
- Gilbreath, B.; Karimi, L. Supervisor behavior and employee presenteeism. Int. J. Leadersh. Stud. 2012, 7, 114–131. [Google Scholar]
- Kocakulah, M.C.; Kelley, A.G.; Mitchell, K.M.; Ruggieri, M.P. Absenteeism problems and costs: Causes, effects and cures. Int. Bus. Econ. Res. J. 2016, 15, 89. [Google Scholar] [CrossRef] [Green Version]
- Barnett, T.; Namasivayam, P.; Narudin, D.A. A critical review of the nursing shortage in Malaysia. Int. Nurs. Rev. 2010, 57, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Krohne, K.; Magnussen, L.H. Go to work or report sick? A focus group study on decisions of sickness presence among offshore catering section workers. BMC Res. Note 2011, 4, 70. [Google Scholar]
- Kim, J.; Suh, E.E.; Ju, S.; Choo, H.; Bae, H.; Choi, H. Sickness experiences of Korean registered nurses at work: A qualitative study on presenteeism. Asian Nurs. Res. 2016, 10, 32–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferreira, A.I.; Martinez, L.F.; Cooper, C.; Gui, D.M. LMX as a negative predictor of presenteeism climate. J. Organ. Eff. People Perform. 2015, 2, 282–302. [Google Scholar] [CrossRef]
- Yu, H.U.; Chan, S. Nurses’ response to death and dying in an intensive care unit—A qualitative study. J. Clin. Nurs. 2010, 19, 1167–1169. [Google Scholar] [CrossRef]
- Sedgwick, P. Cross sectional studies: Advantages and disadvantages. BMJ 2014, 26, 348. [Google Scholar] [CrossRef] [Green Version]
- Lu, L.; Kao, S.F.; Cooper, C.L.; Allen, T.D.; Lapierre, L.M.; O’driscoll, M.; Poelmans, S.A.; Sanchez, J.I.; Spector, P.E. Work resources, work-to-family conflict, and its consequences: A Taiwanese-British cross-cultural comparison. Int. J. Stress Manag. 2009, 16, 25. [Google Scholar] [CrossRef]
- Lipscomb, M.; Snelling, P.C. Student nurse absenteeism in higher education: An argument against enforced attendance. Nurse Educ. Today 2010, 30, 573–578. [Google Scholar] [CrossRef]

| Variables, n = 697 | Min. | Max. | n (%) | Mean (SD) |
|---|---|---|---|---|
| Age, in years | 20 | 59 | 34.67 (8.148) | |
| Gender | ||||
| Male | 19 (2.73) | |||
| Female | 678 (97.27) | |||
| Marital Status | ||||
| Single | 100 (14.35) | |||
| Married | 581 (83.36) | |||
| Separated/Divorced/Others | 16 (2.30) | |||
| No. of Children | 0 | 7 | 1.84 (1.516) | |
| None | 176 (25.25) | |||
| At least one child | 521 (74.75) | |||
| Body Mass Index (BMI), in kg/m2 | 25.79 (5.508) | |||
| Underweight (<18.50 kg/m2) | 32 (4.59) | |||
| Normal (18.50 to 24.99 kg/m2) | 321 (46.05) | |||
| Overweight (25.00 to 29.99 kg/m2) | 205 (29.41) | |||
| Obese (30.00 kg/m2 and above) | 139 (19.94) | |||
| Other Comorbid | ||||
| Having hypertension | 53 (7.60) | |||
| Having diabetes mellitus | 34 (4.88) |
| Variables, n = 697 | Min. | Max. | n (%) | Mean (SD) |
|---|---|---|---|---|
| Workplace | ||||
| Hospital | 448 (64.28) | |||
| Public Health and Primary Healthcare | 249 (35.72) | |||
| Work tenure as nurse, in years | 11.42 (7.591) | |||
| Position | ||||
| Community Nurse | 162 (23.24) | |||
| Staff Nurse/Midwife | 428 (61.41) | |||
| Sister a | 90 (12.91) | |||
| Matron b | 17 (2.44) | |||
| Work Schedule | ||||
| Non-Shift Work | 248 (35.58) | |||
| Shift Work | 449 (64.42) |
| Variables, n = 697 | n (%) | Mean (SD) |
|---|---|---|
| STRESS STATUS | 25.69 (20.836) | |
| Non-stress (Score less than 36) | 501 (71.88) | |
| Stress (Score 36 and above) | 196 (28.12) | |
| NON-WORKPLACE STRESSOR | 5.90 (5.497) | |
| Not enough money | 0.68 (0.796) | |
| Conflicts with spouse | 0.48 (0.693) | |
| Conflicts over household tasks | 0.48 (0.682) | |
| Conflicts with children | 0.36 (0.598) | |
| Pressure from relatives | 0.44 (0.713) | |
| Fixing up of house | 0.43 (0.681) | |
| No time with family | 1.08 (0.966) | |
| Sexual conflicts | 0.21 (0.513) | |
| Dangerous surroundings | 0.42 (0.663) | |
| Conflict with close friends | 0.40 (0.603) | |
| Personal problems cause strain | 0.40 (0.636) | |
| No babysitter | 0.51 (0.797) | |
| WORKPLACE STRESSOR | 25.92 (13.549) | |
| Workload | 8.39 (3.640) | |
| Death and dying | 4.39 (3.831) | |
| Inadequate preparation | 1.80 (1.572) | |
| Lack of staff support | 2.11 (1.908) | |
| Uncertainty concerning treatment | 3.19 (2.429) | |
| Conflict with doctors | 3.22 (2.552) | |
| Conflict with other nurses | 2.81 (2.453) |
| Variables, n = 697 | Medically-Certified Leave (MC) | Emergency Leave (EL) | ||||||
|---|---|---|---|---|---|---|---|---|
| n (%) | Min. | Max. | Mean (SD) | n (%) | Min. | Max. | Mean (SD) | |
| Prevalence | ||||||||
| Never taken | 355 (50.93) | 360 (51.65) | ||||||
| Ever taken | 342 (49.07) | 337 (48.35) | ||||||
| Duration in days of taking leave a | 1 | 140 | 4.24 (10.355) | 1 | 16 | 2.39 (1.966) | ||
| Frequency of taking leave a | 1 | 25 | 1.80 (1.593) | 1 | 8 | 1.92 (1.272) | ||
| Variables | n (%) | No. of Leave Days for Each Reason | |||
|---|---|---|---|---|---|
| Min | Max | Mean (SD) | Total | ||
| MEDICALLY-CERTIFIED LEAVE (MC) b | |||||
| Unspecified fever | 134 (39.18) | 1 | 4 | 1.54 (0.732) | 206 |
| Non-specified | 42 (12.28) | 1 | 33 | 3.17 (5.231) | 133 |
| Upper respiratory tract infection, sinusitis | 33 (9.65) | 1 | 9 | 2.00 (1.581) | 66 |
| AGE, food poisoning | 29 (8.48) | 1 | 4 | 1.38 (0.820) | 40 |
| Dizziness, headache, vertigo, migraine | 29 (8.48) | 1 | 4 | 1.72 (0.751) | 50 |
| Unspecified symptoms (ache, cough) | 26 (7.60) | 1 | 5 | 1.73 (1.079) | 45 |
| Tooth-related pain and procedure | 23 (6.73) | 1 | 5 | 1.65 (1.027) | 38 |
| Eye-related (e.g., conjunctivitis) | 18 (5.26) | 1 | 5 | 2.44 (1.338) | 44 |
| Trauma-related (fracture, tissue injury) | 16 (4.68) | 1 | 60 | 8.25 (15.159) | 132 |
| Medical appointment/procedure | 15 (4.29) | 1 | 4 | 1.80 (1.014) | 27 |
| Others (otitis, pneumonia, burn, allergy) | 12 (3.51) | 1 | 10 | 3.33 (2.964) | 40 |
| Surgery (I&D, laparotomy, TAHBSO) | 11 (3.22) | 10 | 140 | 39.45 (38.816) | 434 |
| AEBA | 10 (2.92) | 1 | 7 | 2.50 (2.121) | 25 |
| CVS-related (ACS, hypertension, stroke) | 8 (2.34) | 1 | 30 | 5.75 (9.867) | 46 |
| MSD (CTS, PID, backache) | 7 (2.05) | 1 | 16 | 4.71 (5.499) | 33 |
| Viral fever, dengue fever | 7 (2.05) | 1 | 7 | 3.71 (2.498) | 26 |
| GERD, gastritis | 5 (1.46) | 1 | 3 | 2.00 (1.000) | 10 |
| Urinary tract infection | 4 (1.17) | 1 | 7 | 3.25 (2.630) | 13 |
| Menstrual-related | 3 (0.88) | 1 | 1 | 1.00 (0.000) | 3 |
| Child sickness | 2 (0.58) | 5 | 6 | 5.50 (0.707) | 11 |
| EMERGENCY LEAVE (EL) c | |||||
| Child sickness | 175 (51.93) | 1 | 16 | 2.23 (1.789) | 390 |
| Sick family members or relatives | 61 (18.10) | 1 | 7 | 2.18 (1.658) | 133 |
| Death of family members | 53 (15.73) | 1 | 5 | 1.51 (0.993) | 80 |
| Unspecified reasons | 35 (10.39) | 1 | 5 | 1.71 (1.073) | 60 |
| Child matters except sickness | 31 (9.20) | 1 | 3 | 1.35 (0.709) | 42 |
| Self-certified health problem | 21 (6.23) | 1 | 3 | 1.33 (0.658) | 28 |
| Unspecified family- or self-related matters | 16 (4.75) | 1 | 3 | 1.38 (0.719) | 22 |
| Vehicle problem or MVA | 9 (2.67) | 1 | 1 | 1.00 (0.000) | 9 |
| Medical appointment | 1 (0.30) | 1 | 1 | 1.00 (0.000) | 1 |
| Others | 1 (0.30) | 1 | 1 | 1.00 (0.000) | 1 |
| Variables, n = 697 | Exp (B) (95% CI) a | |||
|---|---|---|---|---|
| MC b | EL c | MC + EL d | None e | |
| SOCIODEMOGRAPHIC | ||||
| Age | 1.029 (1.004, 1.056) | |||
| Marital status (Ref. = ever married) | 0.252 (0.135, 0.473) | 2.193 (1.404, 3.425) | ||
| Having children (Ref. = have children) | 2.120 (1.323, 3.395) | 0.414 (0.238, 0.718) | ||
| BMI (Ref. = overweight/obese) | ||||
| OCCUPATIONAL | ||||
| Workplace (Ref. = hospital) | 1.696 (1.195, 2.407) | 0.625 (0.432, 0.905) | ||
| Work schedule (Ref. = non-shift) | ||||
| STRESS STATUS (Ref. = yes) | ||||
| NON-WORKPLACE STRESSOR | ||||
| Not enough money | ||||
| Conflicts with spouse | ||||
| Conflicts over household tasks | ||||
| Conflicts with children | ||||
| Pressure from relatives | 1.658 (1.228, 2.239) | 0.687 (0.516, 0.916) | ||
| Fixing up of house | ||||
| No time with family | ||||
| Sexual conflicts | ||||
| Dangerous surrounding | 0.712 (0.542, 0.936) | |||
| Conflict with close friends | 1.394 (1.007, 1.928) | |||
| Personal problems cause strain | ||||
| No babysitter | ||||
| WORKPLACE STRESSOR | ||||
| Workload | ||||
| Death and dying | 0.921 (0.875, 0.969) | |||
| Inadequate preparation | 0.754 (0.644, 0.820) | 1.210 (1.082, 1.353) | ||
| Lack of staff support | ||||
| Uncertainty concerning treatment | ||||
| Conflict with doctors | ||||
| Conflict with other nurses | ||||
| Variables | Adj.b (95% CI) a | |
|---|---|---|
| Duration of MC among Those Ever Took MC (n = 342) b | Duration of EL among Those Ever Took EL (n = 337) c | |
| SOCIODEMOGRAPHIC PROFILE | ||
| Age | ||
| Marital status (0 = never married; 1 = ever married) | ||
| Having children (0 = no children; 1 = have children) | 0.781 (0.242, 1.320) | |
| Body mass index (0 = underweight/normal; 1 = overweight/obese) | 0.417 (0.019, 0.816) | |
| OCCUPATIONAL PROFILE | ||
| Workplace (0 = non-hospital; 1 = hospital) | 3.411 (0.721, 6.101) | |
| Work schedule (0 = shift; 1 = non-shift) | 0.463 (0.039, 0.888) | |
| STRESS STATUS (0 = no; 1 = yes) | ||
| NON-WORKPLACE STRESSOR | ||
| Not enough money | ||
| Conflicts with spouse | 0.536 (0.184, 0.888) | |
| Conflicts over household task | ||
| Conflicts with children | ||
| Pressure from relatives | ||
| Fixing up of house | ||
| No time with family | ||
| Sexual conflict | −0.435 (−0.848, −0.022) | |
| Dangerous surrounding | ||
| Conflict with close friends | ||
| Personal problem cause strain | ||
| No babysitter | 0.440 (0.166, 0.714) | |
| WORKPLACE STRESSOR | ||
| Workload | ||
| Death and dying | ||
| Inadequate preparation | −1.065 (−1.849, −0.282) | 0.257 (0.104, 0.409) |
| Lack of staff support | −0.190 (−0.322, −0.059) | |
| Uncertainty concerning treatment | ||
| Conflict with doctors | 0.491 (0.000, 0.982) | −0.112 (−0.220, −0.003) |
| Conflict with other nurses | ||
| Adj.b (95% CI) a | ||
|---|---|---|
| Variables, n = 337 | Frequency of MC among Those Ever Took MC (n = 342) b | Frequency of EL among Those Ever Took EL (n = 337) c |
| SOCIODEMOGRAPHIC PROFILE | ||
| Age | −0.024 (−0.042, −0.006) | |
| Marital status (0 = never married; 1 = ever married) | ||
| Having children (0 = no children; 1 = have children) | 0.601 (0.210, 0.991) | 0.521 (0.161, 0.881) |
| OCCUPATIONAL PROFILE | ||
| Body mass index (0 = underweight/normal; 1 = overweight/obese) | 0.385 (0.121, 0.648) | |
| Workplace (0 = non-hospital; 1 = hospital) | −0.327 (−0.594, −0.060) | |
| Work schedule (0 = shift; 1 = non-shift) | ||
| STRESS STATUS (0 = no; 1 = yes) | −0.368 (−0.661, −0.076) | |
| NON-WORKPLACE STRESSOR | ||
| Not enough money | −0.334 (−0.523, −0.145) | |
| Conflicts with spouse | 0.383 (0.157, 0.610) | |
| Conflicts over household task | −0.261 (−0.519, −0.002) | |
| Conflicts with children | ||
| Pressure from relatives | 0.207 (0.015, 0.398) | |
| Fixing up of house | ||
| No time with family | 0.257 (0.066, 0.448) | |
| Sexual conflict | ||
| Dangerous surrounding | 0.734 (0.438, 1.031) | |
| Conflict with close friends | −0.467 (−0.779, −0.154) | |
| Personal problem cause strain | ||
| No babysitter | ||
| WORKPLACE STRESSOR | ||
| Workload | ||
| Death and dying | 0.051 (0.004, 0.099) | |
| Inadequate preparation | 0.090 (0.006, 0.173) | |
| Lack of staff support | ||
| Uncertainty concerning treatment | ||
| Conflict with doctors | ||
| Conflict with other nurses | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mat Saruan, N.A.; Mohd Yusoff, H.; Mohd Fauzi, M.F.; Wan Puteh, S.E.; Muhamad Robat, R. Unplanned Absenteeism: The Role of Workplace and Non-Workplace Stressors. Int. J. Environ. Res. Public Health 2020, 17, 6132. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17176132
Mat Saruan NA, Mohd Yusoff H, Mohd Fauzi MF, Wan Puteh SE, Muhamad Robat R. Unplanned Absenteeism: The Role of Workplace and Non-Workplace Stressors. International Journal of Environmental Research and Public Health. 2020; 17(17):6132. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17176132
Chicago/Turabian StyleMat Saruan, Nur Adibah, Hanizah Mohd Yusoff, Mohd Fadhli Mohd Fauzi, Sharifa Ezat Wan Puteh, and Rosnawati Muhamad Robat. 2020. "Unplanned Absenteeism: The Role of Workplace and Non-Workplace Stressors" International Journal of Environmental Research and Public Health 17, no. 17: 6132. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17176132





