Quality of Life Changes in Acute Coronary Syndromes Patients: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Protocol
2.2. Population
2.3. Search Strategy
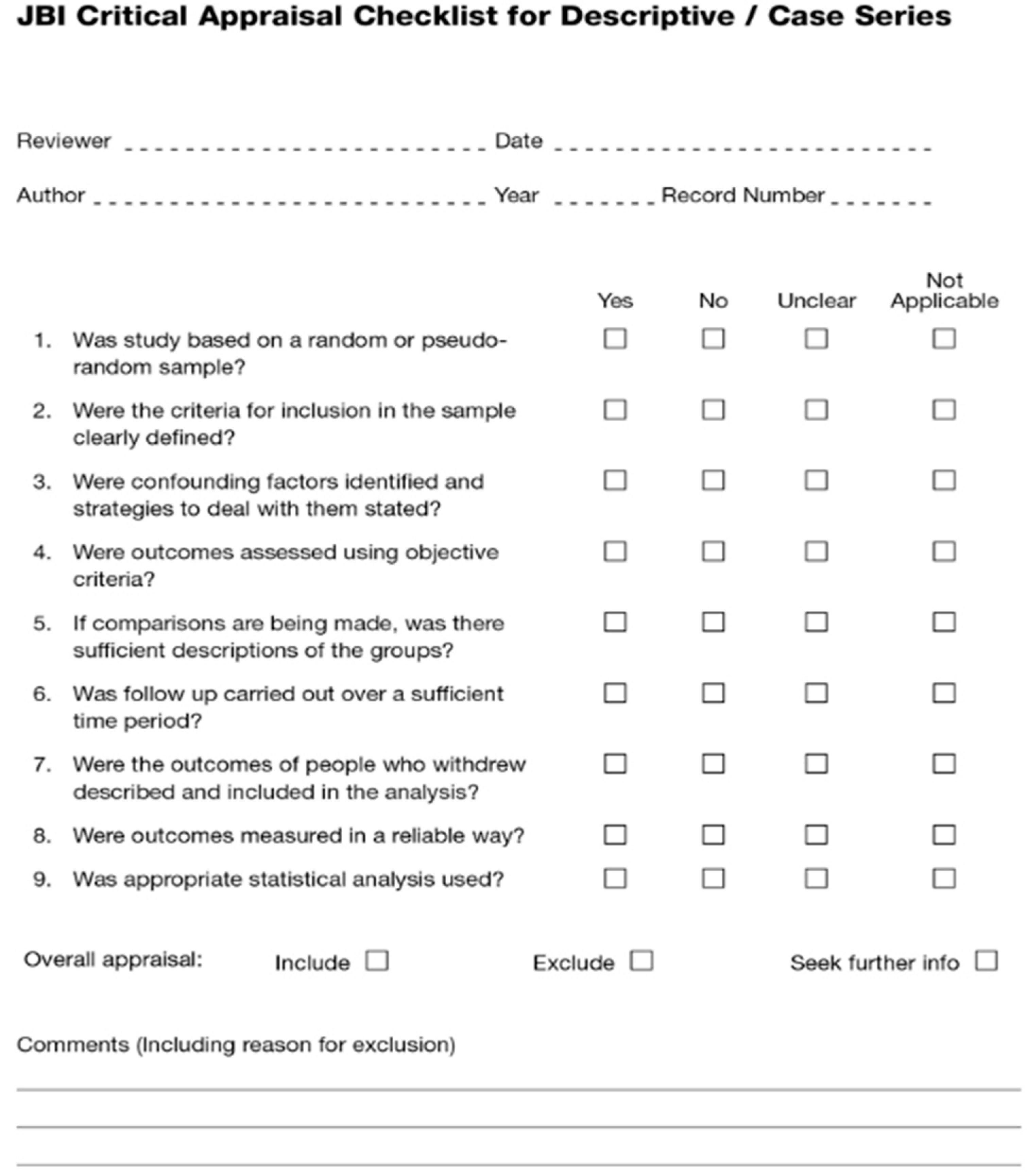
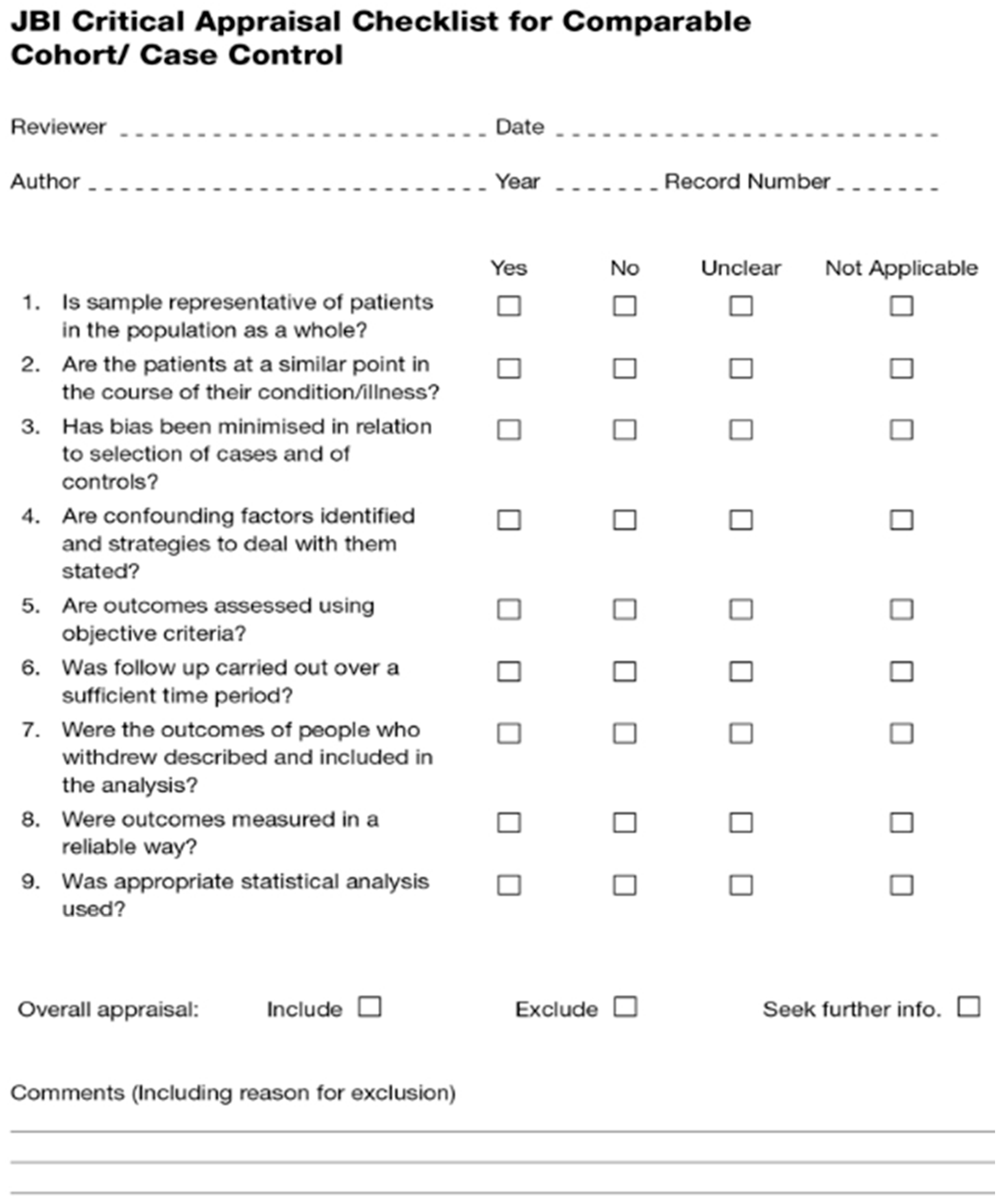
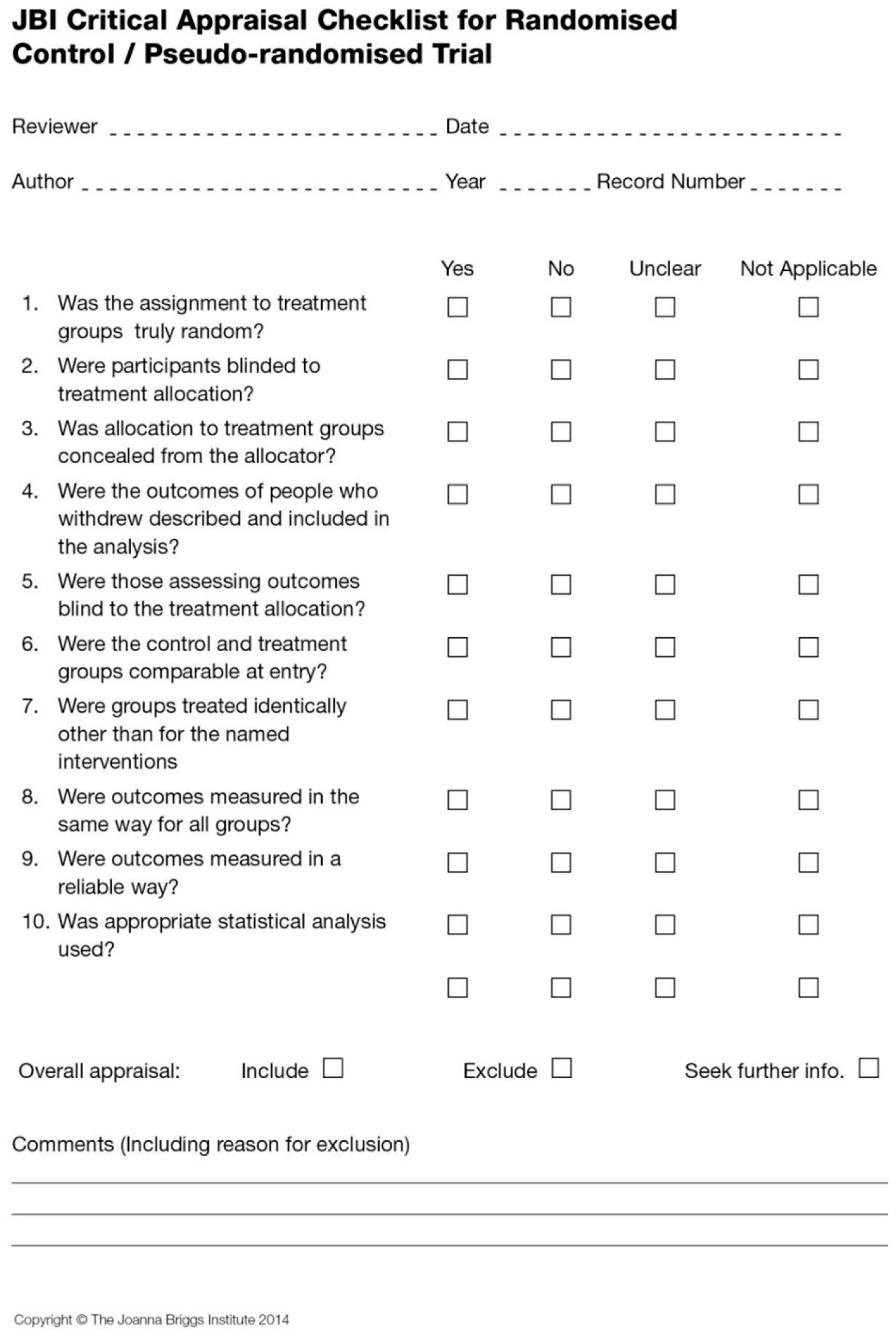
2.4. Study Selection and Quality Assessment
2.5. Data Extraction
2.6. Outcomes
2.7. Data Analysis
3. Results
3.1. Description of Studies
3.2. Methodological Quality
3.3. Measurement of QoL
3.4. Changes in QoL among ACS Patients after Treatment
3.5. Meta-Analysis of Status of QoL among ACS Patients at Baseline and after Receiving Treatment
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A. Full Search Strategy
| 1 | (“quality of life” or “life quality” or “health related quality of life” or QOL or QL or HRQOL or “health status” or HS or “health profile” or well-being or “recovery function” or “disability evaluation” or “short form 6” or SF-6 or SF-12 or SF-36 or “Seattle angina questionnaire” or SAQ or “duke activity status index” or DASI or “Nottingham health profile” or NHP or “Euro-Qol 5 dimensions 3 level” or “Euro-Qol 5 dimensions 5 level” or EQ-5D-3L or EQ-5D-5L or “functional Status Questionnaire” or “Dartmouth COOP Poster Charts” or “Quality of Well-Being Scale” or “Sickness Impact Profile” or “McMaster Health Index Questionnaire” or “Index of Activities of Daily Living” or “Health Utilities Index” or HUI or HUI2 or HUI3).tw. |
| 2 | (“clinical decision” or “decision making” or DM or preference or “patient preference” or “clinical reasoning” or “physician prescription” or “physician therap*” or “decisional conflict” or “physician role” or “decision regret” or “decision satisfaction” or “decision self-efficacy” or “percutaneous coronary intervention” or “PCI” or angiography or revascularization or “bleeding event” or mortality or death or “clinical intuition” or “perceived benefit” or “perceived risk” or “risk stratification” or “estimated benefit” or “estimated risk”).tw. |
| 3 | (“acute coronary syndrome” or “ACS” or “coronary heart disease” or “myocardial infarction” or “MI” or heart infarction).tw. |
| 4 | 1 and 2 and 3 |
| 1 | (“quality of life” OR “life quality” OR “health related quality of life” OR QOL OR QL OR HRQOL OR “health status” OR HS OR “health profile” OR “health profile 30” OR well-being OR “recovery function” OR “disability evaluation” OR “short form 6” OR SF-6 OR SF-12 OR SF-36 OR “Seattle angina questionnaire” OR SAQ OR “duke activity status index” OR DASI OR “Nottingham health profile” OR NHP OR “Euro-Qol 5 dimensions 3 level” OR “Euro-Qol 5 dimensions 5 level” OR EQ-5D-3L OR EQ-5D-5L OR “functional Status Questionnaire” OR “Dartmouth COOP Poster Charts” OR “Quality of Well-Being Scale” OR “Sickness Impact Profile” OR “McMaster Health Index Questionnaire” OR “Index of Activities of Daily Living” OR “Health Utilities Index” OR HUI OR HUI2 OR HUI3) |
| 2 | (“clinical decision” OR “decision making” OR DM OR preference OR “patient preference” OR “clinical reasoning” OR “physician prescription” OR “physician therap*” OR “decisional conflict” OR “physician role” OR “decision regret” OR “decision satisfaction” OR “decision self-efficacy” OR “percutaneous coronary intervention” OR “PCI” OR angiography OR revascularization OR “bleeding events” OR mortality OR death OR “clinical intuition” OR “perceived benefit” OR “perceived risk” OR “risk stratification” OR “estimated benefit” OR “estimated risk”) |
| 3 | (“acute coronary syndrome” OR acs OR “coronary heart disease” OR “myocardial infarction” OR mi OR heart infarction) NOT Medline[sb])” LIMITED to English |
| 4 | 1 AND 2 AND 3 |
| 1 | TS = (“quality of life” or “life quality” or “health related quality of life” or QOL or QL or HRQOL or “health status” or HS or “health profile” or well-being or “recovery function” or “disability evaluation” or “short form 6” or SF-6 or SF-12 or SF-36 or “Seattle angina questionnaire” or SAQ or “duke activity status index” or DASI or “Nottingham health profile” or NHP or “Euro-Qol 5 dimensions 3 level” or “Euro-Qol 5 dimensions 5 level” or EQ-5D-3L or EQ-5D-5L or “functional Status Questionnaire” or “Dartmouth COOP Poster Charts” or “Quality of Well-Being Scale” or “Sickness Impact Profile” or “McMaster Health Index Questionnaire” or “Index of Activities of Daily Living” or “Health Utilities Index” or HUI or HUI2 or HUI3) |
| 2 | TS = (“clinical decision” or “decision making” or DM OR preference or “patient preference” or “clinical reasoning” or “physician prescription” or “physician therap*” or “decisional conflict” or “physician role” or “decision regret” or “decision satisfaction” or “decision self-efficacy” or “percutaneous coronary intervention” or “PCI” or angiography or revascularization or “bleeding events” or mortality or death or “clinical intuition” or “perceived benefit” or “perceived risk” or “risk stratification” or “estimated benefit” or “estimated risk”) |
| 3 | TS = (“acute coronary syndrome” or “ACS” or “coronary heart disease” or “myocardial infarction” or “MI” or heart infarction) |
| 4 | 1 AND 2 AND 3; Limited by language (English) |
| 1 | ALL (“quality of life” OR “life quality” OR “health related quality of life” OR QOL OR QL OR HRQOL OR “health status” OR HS OR “health profile” OR well-being OR “recovery function” OR “disability evaluation” OR “short form 6” OR SF-6 OR SF-12 OR SF-36 OR “Seattle angina questionnaire” OR SAQ OR “duke activity status index” OR DASI OR “Nottingham health profile” OR NHP OR “Euro-Qol 5 dimensions 3 level” OR “Euro-Qol 5 dimensions 5 level” OR EQ-5D-3L OR EQ-5D-5L OR “functional Status Questionnaire” OR “Dartmouth COOP Poster Charts” OR “Quality of Well-Being Scale” OR “Sickness Impact Profile” OR “McMaster Health Index Questionnaire” OR “Index of Activities of Daily Living” OR “Health Utilities Index” OR HUI OR HUI2 OR HUI3) |
| 2 | ALL(“clinical decision” OR “decision making” OR DM OR preference OR “patient preference” OR “clinical reasoning” OR “physician prescription” OR “physician therap*” OR “decisional conflict” OR “physician role” OR “decision regret” OR “decision satisfaction” OR “decision self-efficacy” OR “percutaneous coronary intervention” OR “PCI” OR angiography OR revascularization OR “bleeding events” OR mortality OR death OR “clinical intuition” OR “perceived benefit” OR “perceived risk” OR “risk stratification” OR “estimated benefit” OR “estimated risk”) |
| 3 | ALL(“acute coronary syndrome” OR ACS OR “coronary heart disease” OR “myocardial infarction” OR MI OR “heart infarction”) LIMITED to English |
| 4 | 1 AND 2 AND 3; Limited Subject area medicine/sociology/psychology AND English |
| S1 | Tx “quality of life” or “life quality” or “health related quality of life” or QOL or QL or HRQOL or “health status” or HS or “health profile” or well-being or “recovery function” or “disability evaluation” or “short form 6” or SF-6 or SF-12 or SF-36 or “Seattle angina questionnaire” or SAQ or “duke activity status index” or DASI or “Nottingham health profile” or NHP or “Euro-Qol 5 dimensions 3 level” or “Euro-Qol 5 dimensions 5 level” or EQ-5D-3L or EQ-5D-5L or “functional Status Questionnaire” or “Dartmouth COOP Poster Charts” or “Quality of Well-Being Scale” or “Sickness Impact Profile” or “McMaster Health Index Questionnaire” or “Index of Activities of Daily Living” or “Health Utilities Index” or HUI or HUI2 or HUI3 |
| S2 | Tx “clinical decision” OR “decision making” OR DM OR preference OR “patient preference” OR “clinical reasoning” OR “physician prescription” OR “physician therap*” OR “decisional conflict” OR “physician role” OR “decision regret” OR “decision satisfaction” OR “decision self-efficacy” OR “percutaneous coronary intervention” OR “PCI” OR angiography OR revascularization OR “bleeding event” OR mortality OR death OR “clinical intuition” OR “perceived benefit” OR “perceived risk” OR “risk stratification” OR “estimated benefit” OR “estimated risk” |
| S3 | Tx “acute coronary syndrome” or “ACS” or “coronary heart disease” or “myocardial infarction” or “MI” or heart infarction |
| S4 | S1 AND S2 AND S3 AND; Limited to English |
Appendix B. JBI Quality Appraisal and Selection Tool

Appendix C. JBI-Data Extraction Instruments

References
- Beck, C.A.; Joseph, L.; Belisle, P.; Pilote, L.; Investigators, Q. Predictors of quality of life 6 months and 1 year after acute myocardial infarction. Am. Heart J. 2001, 142, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Harjola, V.-P.; Parissis, J.; Bauersachs, J.; Brunner-La Rocca, H.-P.; Bueno, H.; Čelutkienė, J.; Chioncel, O.; Coats, A.J.S.; Collins, S.P.; de Boer, R.A.; et al. Acute coronary syndromes and acute heart failure: A diagnostic dilemma and high-risk combination. A statement from the Acute Heart Failure Committee of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2020, 22. [Google Scholar] [CrossRef]
- Kumar, A.; Cannon, C.P. Acute Coronary Syndromes: Diagnosis and Management, Part I. Mayo Clin. Proc. 2009, 84, 917–938. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amsterdam, E.A.; Wenger, N.K.; Brindis, R.G.; Casey, D.E.; Ganiats, T.G.; Holmes, D.R.; Jaffe, A.S.; Jneid, H.; Kelly, R.F.; Kontos, M.C.; et al. 2014 AHA/ACC Guideline for the Management of Patients With Non–ST-Elevation Acute Coronary Syndromes. Circulation 2014, 130, e344–e426. [Google Scholar] [CrossRef]
- Falk, V.; Baumgartner, H.; Bax, J.J.; De Bonis, M.; Hamm, C.; Holm, P.J.; Iung, B.; Lancellotti, P.; Lansac, E.; Muñoz, D.R.; et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. J. Cardio Thorac. Surg. 2017, 52, 616–664. [Google Scholar] [CrossRef]
- Fischer, J.P.; Wink, J.D.; Tuggle, C.T.; Nelson, J.A.; Kovach, S.J. Wound risk assessment in ventral hernia repair: Generation and internal validation of a risk stratification system using the ACS-NSQIP. Hernia 2015, 19, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Henriques, J.P.; Claessen, B.E.; Dangas, G.D.; Kirtane, A.J.; Popma, J.J.; Massaro, J.M.; Cohen, B.M.; Ohman, E.M.; Moses, J.W.; O’Neill, W.W. Performance of currently available risk models in a cohort of mechanically supported high-risk percutaneous coronary intervention--From the PROTECT II randomized trial. Int. J. Cardiol. 2015, 189, 272–278. [Google Scholar] [CrossRef]
- Kirtane, A.J.; Doshi, D.; Leon, M.B.; Lasala, J.M.; Ohman, E.M.; O’Neill, W.W.; Shroff, A.; Cohen, M.G.; Palacios, I.F.; Beohar, N.; et al. Treatment of Higher-Risk Patients With an Indication for Revascularization: Evolution Within the Field of Contemporary Percutaneous Coronary Intervention. Circulation 2016, 134, 422–431. [Google Scholar] [CrossRef]
- De Backer, G.; Ambrosioni, E.; Borch-Johnsen, K.; Brotons, C.; Cifkova, R.; Dallongeville, J.; Ebrahim, S.; Faergeman, O.; Graham, I.; Mancia, G.; et al. European guidelines on cardiovascular disease prevention in clinical practice: Third joint task force of European and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of eight societies and by invited experts). Eur. J. Cardiovasc. Prev. Rehabil. 2003, 10, S1–S10. [Google Scholar] [CrossRef]
- Karimi, M.; Brazier, J. Health, Health-Related Quality of Life, and Quality of Life: What is the Difference? Pharmacoeconomics 2016, 34, 645–649. [Google Scholar] [CrossRef]
- Sandström, L.; Ståhle, A. Rehabilitation of elderly with coronary heart disease – Improvement in quality of life at a low cost. Adv. Physiother. 2005, 7, 60–66. [Google Scholar] [CrossRef]
- Anchah, L.; Hassali, M.A.; Lim, M.S.H.; Ibrahim, M.I.M.; Sim, K.H.; Ong, T.K. Health related quality of life assessment in acute coronary syndrome patients: The effectiveness of early phase I cardiac rehabilitation. Health Qual. Life Outcomes 2017, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levine, G.N.; Bates, E.R.; Blankenship, J.C.; Bailey, S.R.; Bittl, J.A.; Cercek, B.; Chambers, C.E.; Ellis, S.G.; Guyton, R.A.; Hollenberg, S.M.; et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: Executive Summary. Catheter. Cardiovasc. Interv. 2012, 79, 453–495. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, S.S.; Versteeg, H.; Denollet, J.; Cheng, J.M.; Serruys, P.W.; van Domburg, R.T. Patient-rated health status predicts prognosis following percutaneous coronary intervention with drug-eluting stenting. Qual. Life Res. 2011, 20, 559–567. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schenkeveld, L.; Pedersen, S.S.; van Nierop, J.W.I.; Lenzen, M.J.; de Jaegere, P.P.T.; Serruys, P.W.; van Domburg, R.T. Health-related quality of life and long-term mortality in patients treated with percutaneous coronary intervention. Am. Heart J. 2010, 159, 471–476. [Google Scholar] [CrossRef]
- Gardner, A.W.; Montgomery, P.S.; Ritti-Dias, R.M.; Thadani, U. Exercise performance, physical activity, and health-related quality of life in participants with stable angina. Angiology 2011, 62, 461–466. [Google Scholar] [CrossRef] [Green Version]
- Kaambwa, B.; Gesesew, H.; Horsfall, M.; Chew, D.P. Impact of patient’s health-related quality of life on physicians’ therapy and perceived benefit in acute coronary syndromes: Protocol for a systemic review of quantitative and qualitative studies. BMJ Open 2019, 9, e026595. [Google Scholar] [CrossRef] [Green Version]
- JBI. Joanna Briggs Institute Reviewers’manual; Joanna Briggs Institute: Adelaide, SA, USA, 2014. [Google Scholar]
- Viswanathan, M.; Ansari, M.T.; Berkman, N.D.; Chang, S.; Hartling, L.; McPheeters, M.; Santaguida, P.L.; Shamliyan, T.; Singh, K.; Tsertsvadze, A.; et al. AHRQ Methods for Effective Health Care: Assessing the Risk of Bias of Individual Studies in Systematic Reviews of Health Care Interventions. In Methods Guide for Effectiveness and Comparative Effectiveness Reviews; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2008; p. 14. [Google Scholar]
- Viswanathan, M. Assessing the Risk of Bias of Individual Studies in Systematic Reviews of Health Care Interventions; AHRQ (US Agency for Healthcare Research and Quality): Rockville, MD, USA, 2012.
- Owens, D.K.; Lohr, K.N.; Atkins, D.; Treadwell, J.R.; Reston, J.T.; Bass, E.B.; Chang, S.; Helfand, M. AHRQ series paper 5: Grading the strength of a body of evidence when comparing medical interventions--agency for healthcare research and quality and the effective health-care program. J. Clin. Epidemiol. 2010, 63, 513–523. [Google Scholar] [CrossRef]
- Chew, D.P.; Juergens, C.; French, J.; Parsonage, W.; Horsfall, M.; Brieger, D.; Quinn, S. An examination of clinical intuition in risk assessment among acute coronary syndromes patients: Observations from a prospective multi-center international observational registry. Int. J. Cardiol. 2014, 171, 209–216. [Google Scholar] [CrossRef]
- Pursnani, S.; Korley, F.; Gopaul, R.; Kanade, P.; Chandra, N.; Shaw, R.E.; Bangalore, S. Percutaneous coronary intervention versus optimal medical therapy in stable coronary artery disease: A systematic review and meta-analysis of randomized clinical trials. Circ. Cardiovasc. Interv. 2012, 5, 476–490. [Google Scholar] [CrossRef] [Green Version]
- Sally, C.; Charles, H. Coronary Artery Bypass Grafting (CABG). In Decision Making in Anesthesiology, 7th ed.; Churchill Livingstone: Oxford, UK, 2007; pp. 125–170. [Google Scholar] [CrossRef] [Green Version]
- Van Domburg, R.T.; Daemen, J.; Morice, M.C.; de Bruyne, B.; Colombo, A.; Macaya, C.; Richardt, G.; Fajadet, J.; Hamm, C.; van Es, G.A.; et al. Short- and long-term health related quality-of-life and anginal status of the Arterial Revascularisation Therapies Study part II, ARTS-II; sirolimus-eluting stents for the treatment of patients with multivessel coronary artery disease. Eurointervention J. Eur. Collab. Work. Group Interv. Cardiol. Eur. Soc. Cardiol. 2010, 5, 962–967. [Google Scholar] [CrossRef] [PubMed]
- Favarato, M.E.; Hueb, W.; Boden, W.E.; Lopes, N.; Nogueira, C.R.; Takiuti, M.; Gois, A.F.; Borges, J.C.; Favarato, D.; Aldrighi, J.M.; et al. Quality of life in patients with symptomatic multivessel coronary artery disease: A comparative post hoc analyses of medical, angioplasty or surgical strategies-MASS II trial. Int. J. Cardiol. 2007, 116, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Thiele, H.; Neumann-Schniedewind, P.; Jacobs, S.; Boudriot, E.; Walther, T.; Mohr, F.W.; Schuler, G.; Falk, V. Randomized comparison of minimally invasive direct coronary artery bypass surgery versus sirolimus-eluting stenting in isolated proximal left anterior descending coronary artery stenosis. J. Am. Coll. Cardiol. 2009, 53, 2324–2331. [Google Scholar] [CrossRef] [PubMed]
- Koltowski, L.; Koltowska-Haggstrom, M.; Filipiak, K.J.; Kochman, J.; Golicki, D.; Pietrasik, A.; Huczek, Z.; Balsam, P.; Scibisz, A.; Opolski, G. Quality of life in patients with ST-segment elevation myocardial infarction undergoing percutaneous coronary intervention—Radial versus femoral access (from the OCEAN RACE Trial). Am. J. Cardiol. 2014, 114, 516–521. [Google Scholar] [CrossRef] [PubMed]
- Borkon, A.M.; Muehlebach, G.F.; House, J.; Marso, S.P.; Spertus, J.A. A comparison of the recovery of health status after percutaneous coronary intervention and coronary artery bypass. Ann. Thorac. Surg. 2002, 74, 1526–1530, discussion 1530. [Google Scholar] [CrossRef]
- Zhang, Z.; Mahoney, E.M.; Stables, R.H.; Booth, J.; Nugara, F.; Spertus, J.A.; Weintraub, W.S. Disease-specific health status after stent-assisted percutaneous coronary intervention and coronary artery bypass surgery: One-year results from the Stent or Surgery trial. Circulation 2003, 108, 1694–1700. [Google Scholar] [CrossRef]
- Hlatky, M.A.; Boothroyd, D.B.; Melsop, K.A.; Brooks, M.M.; Mark, D.B.; Pitt, B.; Reeder, G.S.; Rogers, W.J.; Ryan, T.J.; Whitlow, P.L.; et al. Medical costs and quality of life 10 to 12 years after randomization to angioplasty or bypass surgery for multivessel coronary artery disease. Circulation 2004, 110, 1960–1966. [Google Scholar] [CrossRef] [Green Version]
- Pocock, S.J.; Henderson, R.A.; Seed, P.; Treasure, T.; Hampton, J.R. Quality of life, employment status, and anginal symptoms after coronary angioplasty or bypass surgery. 3-year follow-up in the Randomized Intervention Treatment of Angina (RITA) Trial. Circulation 1996, 94, 135–142. [Google Scholar] [CrossRef]
- Wahrborg, P. Quality of life after coronary angioplasty or bypass surgery. 1-year follow-up in the Coronary Angioplasty versus Bypass Revascularization investigation (CABRI) trial. Eur. Heart J. 1999, 20, 653–658. [Google Scholar] [CrossRef] [Green Version]
- Melsen, W.G.; Bootsma, M.C.J.; Rovers, M.M.; Bonten, M.J.M. The effects of clinical and statistical heterogeneity on the predictive values of results from meta-analyses. Clin. Microbiol. Infect. 2014, 20, 123–129. [Google Scholar] [CrossRef] [Green Version]
- Jo, L.-B.; Viv, R. Presenting and Interpreting Meta-Analyses: Heterogenity. Available online: http://www.nottingham.ac.uk/nmp/sonet/rlos/ebp/meta-analysis2/4.html (accessed on 2 May 2007).
- Borenstein, M.; Hedges, L.; Rothstein, H. Meta-Analysis: Fixed Effect vs. Random Effects. Available online: https://www.meta-analysis.com/downloads/Meta-analysis%20fixed%20effect%20vs%20random%20effects.pdf (accessed on 17 May 2007).
- Tufanaru, C.; Munn, Z.; Stephenson, M.; Aromataris, E. Fixed or random effects meta-analysis? Common methodological issues in systematic reviews of effectiveness. Int. J. Evid. Based Healthc. 2015, 13, 196–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cochrane. Review Manager (RevMan) [Computer program] 5.3; The Nordic Cochrane Centre; The Cochrane Collaboration: Copenhagen, Denmark, 2014. [Google Scholar]
- Aasa, M.; Henriksson, M.; Dellborg, M.; Grip, L.; Herlitz, J.; Levin, L.A.; Svensson, L.; Janzon, M. Cost and health outcome of primary percutaneous coronary intervention versus thrombolysis in acute ST-segment elevation myocardial infarction-Results of the Swedish Early Decision reperfusion Study (SWEDES) trial. Am. Heart J. 2010, 160, 322–328. [Google Scholar] [CrossRef] [PubMed]
- Abdallah, M.S.; Wang, K.J.; Magnuson, E.A.; Osnabrugge, R.L.; Kappetein, A.P.; Morice, M.C.; Mohr, F.A.; Serruys, P.W.; Cohen, D.J.; Investigators, S.T. Quality of Life After Surgery or DES in Patients With 3-Vessel or Left Main Disease. J. Am. Coll. Cardiol. 2017, 69, 2039–2050. [Google Scholar] [CrossRef] [PubMed]
- Abdallah, M.S.; Wang, K.J.; Magnuson, E.A.; Spertus, J.A.; Farkouh, M.E.; Fuster, V.; Cohen, D.J.; Investigators, F.T. Quality of Life After PCI vs CABG Among Patients With Diabetes and Multivessel Coronary Artery Disease A Randomized Clinical Trial. JAMA J. Am. Med. Assoc. 2013, 310, 1581–1590. [Google Scholar] [CrossRef] [Green Version]
- Benzer, W.; Hofer, S.; Oldridge, N.B. Health-related quality of life in patients with coronary artery disease after different treatments for angina in routine clinical practice. Herz 2003, 28, 421–428. [Google Scholar] [CrossRef]
- Cohen, D.J.; Van Hout, B.; Serruys, P.W.; Mohr, F.W.; Macaya, C.; den Heijer, P.; Vrakking, M.M.; Wang, K.; Mahoney, E.M.; Audi, S.; et al. Quality of life after PCI with drug-eluting stents or coronary-artery bypass surgery. N. Engl. J. Med. 2011, 364, 1016–1026. [Google Scholar] [CrossRef]
- Kim, M.J.; Jeon, D.S.; Gwon, H.C.; Kim, S.J.; Chang, K.; Kim, H.S.; Tahk, S.J. Health-related quality-of-life after percutaneous coronary intervention in patients with UA/NSTEMI and STEMI: The Korean multicenter registry. J. Korean Med. Sci. 2013, 28, 848–854. [Google Scholar] [CrossRef]
- Kim, J.; Henderson, R.A.; Pocock, S.J.; Clayton, T.; Sculpher, M.J.; Fox, K.A. Health-related quality of life after interventional or conservative strategy in patients with unstable angina or non-ST-segment elevation myocardial infarction: One-year results of the third Randomized Intervention Trial of unstable Angina (RITA-3). J. Am. Coll. Cardiol. 2005, 45, 221–228. [Google Scholar] [CrossRef]
- Li, R.J.; Yan, B.P.; Dong, M.; Zhang, Q.; Yip, G.W.K.; Chan, C.P.; Zhang, M.; Zhang, Q.H.; Sanderson, J.E.; Yu, C.M. Quality of life after percutaneous coronary intervention in the elderly with acute coronary syndrome. Int. J. Cardiol. 2012, 155, 90–96. [Google Scholar] [CrossRef]
- Rinfret, S.; Grines, C.L.; Cosgrove, R.S.; Ho, K.K.; Cox, D.A.; Brodie, B.R.; Morice, M.C.; Stone, G.W.; Cohen, D.J.; Stent, P.I. Quality of life after balloon angioplasty or stenting for acute myocardial infarction. One-year results from the Stent-PAMI trial. J. Am. Coll. Cardiol. 2001, 38, 1614–1621. [Google Scholar] [CrossRef] [Green Version]
- Tegn, N.; Abdelnoor, M.; Aaberge, L.; Ranhoff, A.H.; Endresen, K.; Gjertsen, E.; SkÅRdal, R.; Gullestad, L.; Bendz, B. Health-related quality of life in older patients with acute coronary syndrome randomised to an invasive or conservative strategy. The After Eighty randomised controlled trial. Age Ageing 2018, 47, 42–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takousi, M.G.; Schmeer, S.; Manaras, I.; Olympios, C.D.; Makos, G.; Troop, N.A. Health-related quality of life after coronary revascularization: A systematic review with meta-analysis. Hell. J. Cardiol. 2016, 57, 223–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Veenstra, M.; Pettersen, K.I.; Rollag, A.; Stavem, K. Association of changes in health-related quality of life in coronary heart disease with coronary procedures and sociodemographic characteristics. Health Qual. Life Outcomes 2004, 2, 56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azmi, S.; Goh, A.; Fong, A.; Anchah, L. Quality of life among Patients with Acute Coronary Syndrome in Malaysia. Value Health Reg. Issues 2015, 6, 80–83. [Google Scholar] [CrossRef] [Green Version]
- Bahramnezhad, F.; Khajeh, M.; Shiri, M.; Asgari, P.; Afshar, P.F. Quality of Life in Patients Undergoing Percutaneous Transluminal Coronary Angioplasty (PTCA). Glob. J. Health Sci. 2015, 7, 246–250. [Google Scholar] [CrossRef] [Green Version]
- Bakhai, A.; Ferrieres, J.; James, S.; Iniguez, A.; Mohacsi, A.; Pavlides, G.; Belger, M.; Norrbacka, K.; Sartral, M.; Investigators, A. Treatment, Outcomes, Costs, and Quality of Life of Women and Men With Acute Coronary Syndromes Who Have Undergone Percutaneous Coronary Intervention: Results From the Antiplatelet Therapy Observational Registry. Postgrad. Med. 2013, 125. [Google Scholar] [CrossRef]
- Blankenship, J.C.; Marshall, J.J.; Pinto, D.S.; Lange, R.A.; Bates, E.R.; Holper, E.M.; Grines, C.L.; Chambers, C.E. Effect of percutaneous coronary intervention on quality of life: A consensus statement from the Society for Cardiovascular Angiography and Interventions. Catheter. Cardiovasc. Interv. Off. J. Soc. Card. Angiogr. Interv. 2013, 81, 243–259. [Google Scholar] [CrossRef] [Green Version]
- Berry, C.; Tardif, J.C.; Bourassa, M.G. Coronary Heart Disease in Patients With Diabetes. Part II: Recent Advances in Coronary Revascularization. J. Am. Coll. Cardiol. 2007, 49, 643–656. [Google Scholar] [CrossRef] [Green Version]
- Chudek, J.; Kowalczyk, A.; Kowalczyk, A.K.; Kwiatkowska, J.; Raczak, G.; Kozlowski, D. Quality of life (QOL) evaluation after acute coronary syndrome with simultaneous clopidogrel treatment. Arch 2014, 10, 33–38. [Google Scholar] [CrossRef]
- Koch, C.G.; Khandwala, F.; Cywinski, J.B.; Ishwaran, H.; Estafanous, F.G.; Loop, F.D.; Blackstone, E.H. Health-related quality of life after coronary artery bypass grafting: A gender analysis using the Duke Activity Status Index. J. Thorac. Cardiovasc. Surg. 2004, 128, 284–295. [Google Scholar] [CrossRef] [Green Version]
- Sipotz, J.; Friedrich, O.; Hofer, S.; Benzer, W.; Chatsakos, T.; Gaul, G. Health related quality of life and mental distress after PCI: Restoring a state of equilibrium. Health Qual Life Outcomes 2013, 11, 144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sjoland, H.; Wiklund, I.; Caidahl, K.; Hartford, M.; Karlsson, T.; Herlitz, J. Improvement in quality of life differs between women and men after coronary artery bypass surgery. J. Intern. Med. 1999, 245, 445–454. [Google Scholar] [CrossRef] [PubMed]
- Spertus, J.A.; Salisbury, A.C.; Jones, P.G.; Conaway, D.G.; Thompson, R.C. Predictors of quality-of-life benefit after percutaneous coronary intervention. Circulation 2004, 110, 3789–3794. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yan, B.P.; Chan, L.L.Y.; Lee, V.W.Y.; Yu, C.-M.; Wong, M.C.S.; Sanderson, J.; Reid, C.M. Sustained 3-Year Benefits in Quality of Life After Percutaneous Coronary Interventions in the Elderly: A Prospective Cohort Study. Value Health 2018, 21, 423–431. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krzych, L.J.; Woznica, A.; Pawlak, A.; Skarysz, J.; Eysymontt, Z.; Chromanska-Matera, B.; Krupka-Matuszczyk, I.; Bochenek, A.; Cisowski, M. Quality of life in young, professionally active men undergoing on-pump coronary artery bypass grafting-short-term follow-up results. Kardiol. Pol. 2009, 67, 1078–1087. [Google Scholar] [PubMed]
- Sutherland, H.J.; Till, J.E. Quality of life assessments and levels of decision making: Differentiating objectives. Qual. Life Res. 1993, 2, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Detmar, S.B.; Aaronson, N.K. Quality of life assessment in daily clinical oncology practice: A feasibility study. Eur. J. Cancer (Oxf. Engl. 1990) 1998, 34, 1181–1186. [Google Scholar] [CrossRef]
- Matthis, S. Measuring the Unmeasurable? Quality of Life and Medical Decision Making (from the editor). Ethics J. Am. Med. Assoc. 2005, 7, 133–135. [Google Scholar]
- Sztankay, M.; Giesinger, J.M.; Zabernigg, A.; Krempler, E.; Pall, G.; Hilbe, W.; Burghuber, O.; Hochmair, M.; Rumpold, G.; Doering, S.; et al. Clinical decision-making and health-related quality of life during first-line and maintenance therapy in patients with advanced non-small cell lung cancer (NSCLC): Findings from a real-world setting. BMC Cancer 2017, 17, 565. [Google Scholar] [CrossRef] [Green Version]
- Hajjaj, F.M.; Salek, M.S.; Basra, M.K.; Finlay, A.Y. Non-clinical influences on clinical decision-making: A major challenge to evidence-based practice. J. R. Soc. Med. 2010, 103, 178–187. [Google Scholar] [CrossRef] [Green Version]
- Zafar, S.Y.; Alexander, S.C.; Weinfurt, K.P.; Schulman, K.A.; Abernethy, A.P. Decision making and quality of life in the treatment of cancer: A review. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2009, 17, 117–127. [Google Scholar] [CrossRef] [PubMed]
- Menichetti, J.; Valdagni, R.; Bellardita, L. Quality of life in active surveillance and the associations with decision-making-a literature review. Transl. Androl. Urol. 2018, 7, 160–169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goodwin, P.J.; Black, J.T.; Bordeleau, L.J.; Ganz, P.A. Health-related quality-of-life measurement in randomized clinical trials in breast cancer--taking stock. J. Natl. Cancer Inst. 2003, 95, 263–281. [Google Scholar] [CrossRef] [PubMed]
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; de Haes, J.C.; et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef] [PubMed]
- King, S.; Exley, J.; Parks, S.; Ball, S.; Bienkowska-Gibbs, T.; MacLure, C.; Harte, E.; Stewart, K.; Larkin, J.; Bottomley, A.; et al. The use and impact of quality of life assessment tools in clinical care settings for cancer patients, with a particular emphasis on brain cancer: Insights from a systematic review and stakeholder consultations. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2016, 25, 2245–2256. [Google Scholar] [CrossRef] [Green Version]
- Brazier, J.E.; Yang, Y.; Tsuchiya, A.; Rowen, D.L. A review of studies mapping (or cross walking) non-preference based measures of health to generic preference-based measures. Eur. J. Health Econ. 2010, 11, 215–225. [Google Scholar] [CrossRef]
- Shabason, J.E.; Mao, J.J.; Frankel, E.S.; Vapiwala, N. Shared decision-making and patient control in radiation oncology: Implications for patient satisfaction. Cancer 2014, 120, 1863–1870. [Google Scholar] [CrossRef]
- Philip, S. Meta-analyses: How to read a funnel plot. BMJ 2013, 346, f1342. [Google Scholar]


| Author | Year, Country | Sample Size | Study Design | Measurement | Summary |
|---|---|---|---|---|---|
| Secondary outcome: QoL change after treatment options | |||||
| Aasa et al. [39] | 2010, Sweden | 205 | RCT | EQ-5D |
|
| Abdallah et al. [40] | 2017, USA and Europe | 1800 | RCT | SAQ and SF-36 |
|
| Abdallah et al. [41] | 2013, Multi- countries (18) | 1900 | RCT | SAQ |
|
| Benzer et al. [42] | 2003, Austria | 267 | Cohort study | MacNew |
|
| Borkon et al. [29] | 2002, USA | 495 | RCT | SAQ |
|
| Cohen et al. [43] | 2011, Europe/North America | 1800 | RCT | SAQ 2, and SF-36& EQ-5D 3 |
|
| Kim et al. [44] | 2013, Korea | 3577 | RCT | SAQ, and EQ-5D |
|
| Kim et al. [45] | 2005, United Kingdom | 1810 | RCT | SAQ&SF-36 4, and EQ-5D |
|
| Koltowski et al. [28] | 2014, Poland | 103 | RCT | EQ-5D, MacNew, QLI |
|
| Li et al. [46] | 2012, China | 624 | Cohort study | SF-36 |
|
| Rinfret et al. [47] | 2001, France | 509 | RCT | SAQ and SF-36 |
|
| Schenkeveld et al. [15] | 2010, Holland | 872 | Cohort study | SF-36 |
|
| Tegn et al. [48] | 2018, Norway | 457 | RCT | SF-36 |
|
| Takousi et al. [49] | 2016 | 15992 | Systematic review and meta-analysis | MAcNEW, SF-36, NHP, SAQ, EQ-5D, RAND-36 5, WHOQOL-Brief, |
|
| Veenstra et al. [50] | 2004, Norway | 254 | Cross-sectional study | SF-36 |
|
| Wahrborg et al. [33] | 1999, Sweden | 154 | RCT | Nottingham Health Profile and a set of 12 other questions |
|
| Secondary outcome: Health-related or generic QoL | |||||
| Azmi et al. [51] | 2015, Malaysia | 104 | Retrospective cohort | EuroQol |
|
| Bahramnezhad et al. [52] | 2015, Iran | 115 | Longitudinal Study | No tool described |
|
| Bakhai et al. [53] | 2015, Europe (14 countries) | 4546 | Cohort study | EQ-5D |
|
| Blankenship et al. [63] | 2013, USA | --- | Literature review | Ferrans and Powers Quality of Life Index, McMaster Health Index Questionnaire, SF-36, SF-12, NHP, Psychological wellbeing index, Quality of wellbeing scale, Sickness Impact Profile, Swedish HRQoL survey, DASI |
|
| Bourassa et al. [55] | 2000, US/Canada | 1095 | Cohort study | DASI 7 |
|
| Chudek et al. [56] | 2014, Poland | 3220 | Survey | SF-12 |
|
| Favarato et al. [26] | 2007, Brazil | 542 | RCT | SF-36 |
|
| Koch et al. [57] | 2003, USA | 1825 | Survey | DASI |
|
| Krzych et al. [62] | 2009, Poland | 50 8 | Cohort | MacNew |
|
| Sipotz et al. [58] | 2013, Austria | 163 | Record review or registry | MacNew Health Related Quality of Life |
|
| Sjoland et al. [59] | 1999, Sweden | 2121 | Cohort study | Physical Activity Score, the Nottingham Health Profile (NHP) & Psychological General Well-being Index |
|
| Spertus et al. [60] | 2004, USA | 1518 | Cohort study | SAQ |
|
| Yan et al. [61] | 2018, China | 1957 | Prospective cohort study | EQ-5D, VAS |
|
| Secondary Outcome | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Authors | Cross-Sectional Studies | |||||||||||
| Was study based on a random or pseudo-random sample? | Were the criteria for inclusion in the sample clearly defined? | Were confounding factors identified and strategies to deal with them stated? | Were outcomes assessed using objective criteria? | If comparisons are being made, was there sufficient comparison of groups? | Was the follow-up carried out over a sufficient period? | Were the outcomes of people who withdrew described and included in the analysis? | Were outcomes measured in reliable way? | Was appropriate statistical analysis used? | % | |||
| Kim et al. [44] | NA | Y | N | Y | Y | NA | NA | Y | Y | 83 | ||
| Koch et al. [57] | NA | Y | Y | Y | Y | NA | NA | Y | Y | 100 | ||
| Veenstra et al. [50] | N | Y | Y | Y | Y | NA | Y | Y | Y | 88 | ||
| Cohort Studies | ||||||||||||
| Is the sample representative of patients in the population? | Are the patients at a similar point in the course of their condition/illness? | Has bias been minimized in relation to selection of cases and controls? | Are confounding factors identified and strategies to deal with them stated? | Are outcomes assessed using objective criteria? | Was the follow-up carried out over a sufficient period? | Were the outcomes of people who withdrew described and included in the analysis? | Were outcomes measured in reliable way? | Was appropriate statistical analysis used? | % | |||
| Azmi et al. [51] | Y | Y | NA | N | Y | Y | NA | Y | Y | 86 | ||
| Bahramnezhad et al. [52] | Y | Y | NA | N | Y | Y | N | Y | Y | 75 | ||
| Bakhai et al. [53] | Y | Y | NA | Y | Y | Y | N | Y | Y | 88 | ||
| Benzer et al. [42] | Y | Y | NA | N | Y | Y | N | Y | Y | 75 | ||
| Chudek et al. [56] | Y | Y | NA | N | Y | Y | NA | Y | Y | 86 | ||
| Krzych et al. [62] | N | Y | Y | Y | Y | Y | NA | Y | Y | 86 | ||
| Li et al. [46] | Y | Y | NA | Y | Y | Y | NA | Y | Y | 100 | ||
| Schenkeveld et al. [15] | Y | Y | NA | Y | Y | Y | NA | Y | Y | 100 | ||
| Sipotz et al. [58] | Y | Y | Y | Y | Y | Y | NA | Y | Y | 100 | ||
| Sjoland et al. [59] | Y | Y | Y | Y | Y | Y | NA | Y | Y | 100 | ||
| Spertus et al. [60] | Y | Y | Y | Y | Y | Y | NA | Y | Y | 100 | ||
| Yan et al. [61] | Y | Y | Y | Y | Y | Y | N | Y | Y | 89 | ||
| Clinical Trial Studies | ||||||||||||
| Was the assignment to treatment groups truly random? | Were participants blinded to treatment allocation? | Was allocation to treatment groups concealed from the allocator? | Were the outcomes of people who withdrew described and included in the analysis? | Were those assessing outcomes blind to the treatment allocation? | Were the control and treatment groups comparable at entry? | Were groups treated identically other than for the named intervention? | Were outcomes measured in the same way for all age groups | Were outcomes measured in a reliable way? | Was appropriate statistical analysis used? | % | ||
| Aasa et al. [39] | Y | NA | Y | N | Y | Y | Y | Y | Y | Y | 89 | |
| Abdallah et al. [40] | Y | N | NA | N | NA | Y | Y | Y | Y | Y | 75 | |
| Abdallah et al. [41] | Y | N | NA | N | NA | Y | Y | Y | Y | Y | 75 | |
| Borkon et al. [29] | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | 90 | |
| Bourassa et al. [55] | Y | N | Y | NA | Y | Y | Y | Y | Y | Y | 89 | |
| Cohen et al. [43] | Y | Y | Y | N | U | Y | Y | Y | Y | Y | 80 | |
| Favarato et al. [26] | Y | U | U | Y | Y | Y | Y | Y | Y | Y | 80 | |
| Kim et al. [45] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 100 | |
| Koltowski et al. [28] * | Y | N | N | Y | N | Y | Y | Y | Y | Y | 70 | |
| Rinfret et al. [47] | Y | N | NA | NA | NA | Y | Y | Y | Y | Y | 86 | |
| Tegn et al. [48] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 100 | |
| Wahrborg et al. [33] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 100 | |
| Review Studies | ||||||||||||
| Is the review question clearly and explicitly stated? | Were the inclusion criteria appropriate for the review question? | Was the search strategy appropriate? | Were the sources and resources used to search for studies adequate? | Were the criteria for appraising studies appropriate? | Was critical appraisal conducted by two or more reviewers independently? | Were there methods to minimize errors in data extraction? | Were the methods used to combine studies appropriate? | Was the likelihood of publication bias assessed? | Were recommendations for policy and/or practice supported by the reported data? | Were the specific directives for new research appropriate? | % | |
| Takousi et al. [49] | Y | Y | Y | Y | Y | N | Y | Y | N | Y | Y | 82 |
| Blankenship et al. [63] | P 1 | |||||||||||
| Study | Random Sequence Generation (Selection Bias) | Allocation Concealment (Selection Bias) | Blinding of Participants and Personnel (Performance Bias) | Blinding of Outcome Assessment (Detection Bias) | Incomplete Outcome Data (Attrition Bias) | Selective Reporting (Reporting Bias) | Other |
|---|---|---|---|---|---|---|---|
| Aasa et al. [39] | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Abdallah et al. [40] | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Abdallah et al. [41] | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Azmi et al. [51] | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
| Bahramnezhad et al. [52] | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
| Bakhai et al. [53] | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
| Benzer et al. [42] | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
| Blankenship et al. [63] | Low risk | Unclear risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
| Borkon et al. [29] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Bourassa et al. [55] | Low risk | Unclear risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
| Chudek et al. [56] | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
| Cohen et al. [43] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Favarato et al. [26] | Low risk | Unclear risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
| Kim et al. [44] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Kim et al. [45] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Koch et al. [57] | Low risk | Unclear risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
| Koltowski et al. [28] | Low risk | High risk | High risk | Low risk | Low risk | Low risk | Low risk |
| Krzych et al. [62] | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
| Li et al. [46] | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
| Rinfret et al. [47] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Schenkeveld et al. [15] | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
| Sipotz et al. [58] | Low risk | Unclear risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
| Sjoland et al. [59] | Low risk | Unclear risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
| Spertus et al. [60] | Low risk | Unclear risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
| Takousi et al. [49] | Low risk | Unclear risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
| Tegn et al. [48] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Veenstra et al. [50] | Low risk | Unclear risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
| Wahrborg et al. [33] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Yan et al. [61] | Low risk | Unclear risk | Unclear risk | Low risk | Low risk | Low risk | Low risk |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaambwa, B.; Gesesew, H.A.; Horsfall, M.; Chew, D. Quality of Life Changes in Acute Coronary Syndromes Patients: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 6889. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17186889
Kaambwa B, Gesesew HA, Horsfall M, Chew D. Quality of Life Changes in Acute Coronary Syndromes Patients: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2020; 17(18):6889. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17186889
Chicago/Turabian StyleKaambwa, Billingsley, Hailay Abrha Gesesew, Matthew Horsfall, and Derek Chew. 2020. "Quality of Life Changes in Acute Coronary Syndromes Patients: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 17, no. 18: 6889. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17186889





