Construction of the Infection Curve of Local Cases of COVID-19 in Hong Kong using Back-Projection
Abstract
:1. Introduction
2. Materials and Methods
3. Results
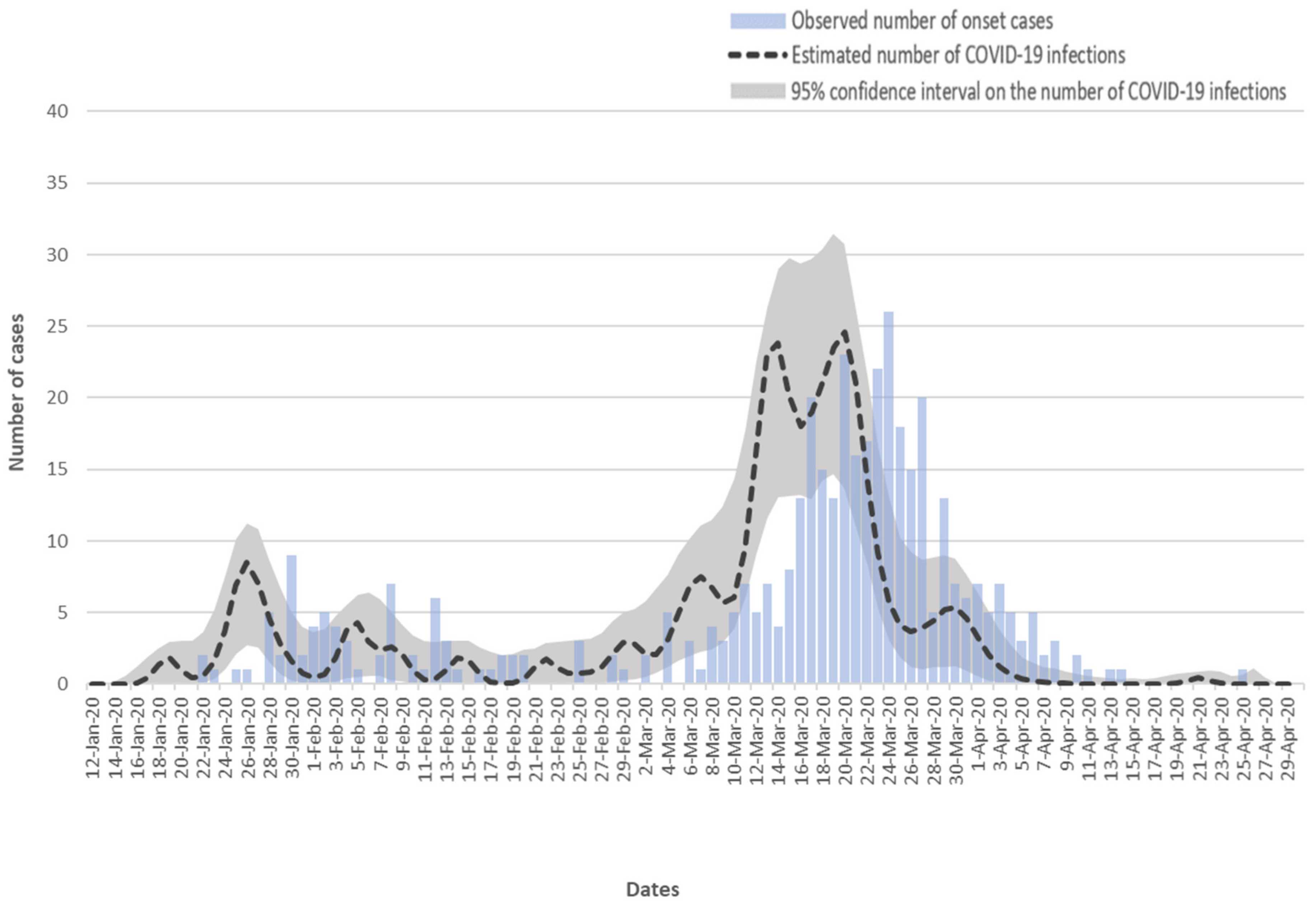
3.1. Estimated Infection Curve
3.2. Possible Association with Social Gathering
3.3. Possible Association with Prevention Policies
3.4. Sensitivity Analysis
4. Discussion
5. Conclusion
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Research Ethics Approval
References
- World Health Organization. Rolling updates on coronavirus disease (COVID-19). 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen (accessed on 28 April 2020).
- Cowling, B.J.; Ali, S.T.; Ng, T.W.Y.; Tsang, T.K.; Li, J.C.M.; Fong, M.W.; Liao, Q.; Kwan, M.Y.; Lee, S.L.; Chiu, S.S.; et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study. Lancet Public Heal. 2020, 5, e279–e288. [Google Scholar] [CrossRef]
- Hellewell, J.; Abbott, S.; Gimma, A.; I Bosse, N.; I Jarvis, C.; Russell, T.W.; Munday, J.D.; Kucharski, A.J.; Edmunds, W.J.; Funk, S.; et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob. Heal. 2020, 8, e488–e496. [Google Scholar] [CrossRef] [Green Version]
- Hou, C.; Chen, J.; Zhou, Y.; Hua, L.; Yuan, J.; He, S.; Guo, Y.; Zhang, S.; Jia, Q.; Zhao, C.; et al. The effectiveness of quarantine of Wuhan city against the Corona Virus Disease 2019 (COVID-19): A well-mixed SEIR model analysis. J. Med Virol. 2020, 92, 841–848. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koo, J.R.; Cook, A.R.; Park, M.; Sun, Y.; Sun, H.; Lim, J.T.; Tam, C.; Dickens, B.L. Interventions to mitigate early spread of SARS-CoV-2 in Singapore: A modelling study. Lancet Infect. Dis. 2020, 20, 678–688. [Google Scholar] [CrossRef] [Green Version]
- Ng, Y.; Li, Z.; Chua, Y.X.; Chaw, W.L.; Zhao, Z.; Er, B.; Pung, R.; Chiew, C.J.; Lye, D.C.; Heng, D.; et al. Evaluation of the Effectiveness of Surveillance and Containment Measures for the First 100 Patients with COVID-19 in Singapore—January 2–February 29, 2020. Mmwr. Morb. Mortal. Wkly. Rep. 2020, 69, 307–311. [Google Scholar] [CrossRef] [PubMed]
- Nussbaumer-Streit, B.; Mayr, V.; Dobrescu, A.I.; Chapman, A.; Persad, E.; Klerings, I.; Wagner, G.; Seibert, U.; Christof, C.; Zachariah, C.; et al. Quarantine alone or in combination with other public health measures to control COVID-19: A rapid review. Cochrane Database Syst Rev. 2020, 4, Cd013574. [Google Scholar]
- Pan, A.; Liu, L.; Wang, C.; Guo, H.; Hao, X.; Wang, Q.; Huang, J.; He, N.; Yu, H.; Lin, X.; et al. Association of Public Health Interventions With the Epidemiology of the COVID-19 Outbreak in Wuhan, China. JAMA 2020, 323, 1915. [Google Scholar] [CrossRef] [Green Version]
- Ruan, L.; Wen, M.; Zeng, Q.; Chen, C.; Huang, S.; Yang, S.; Yang, J.; Wang, J.; Hu, Y.; Ding, S.; et al. New Measures for the Coronavirus Disease 2019 Response: A Lesson From the Wenzhou Experience. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef] [Green Version]
- Saez, M.; Tobias, A.; Varga, D.; Barceló, M.A. Effectiveness of the measures to flatten the epidemic curve of COVID-19. The case of Spain. Sci. Total. Env. 2020, 727, 138761. [Google Scholar] [CrossRef]
- Tobías, A. Evaluation of the lockdowns for the SARS-CoV-2 epidemic in Italy and Spain after one month follow up. Sci. Total. Env. 2020, 725, 138539. [Google Scholar] [CrossRef]
- Wang, G.; Chen, W.; Jin, X.; Chen, Y.-P. Description of COVID-19 cases along with the measures taken on prevention and control in Zhejiang, China. J. Med Virol. 2020. [Google Scholar] [CrossRef] [Green Version]
- Yezli, S.; Khan, A. COVID-19 social distancing in the Kingdom of Saudi Arabia: Bold measures in the face of political, economic, social and religious challenges. Travel Med. Infect. Dis. 2020, 101692. [Google Scholar] [CrossRef]
- Nishiura, H. Backcalculating the Incidence of Infection with COVID-19 on the Diamond Princess. J. Clin. Med. 2020, 9, 657. [Google Scholar] [CrossRef] [Green Version]
- McAloon, C.; Collins, Á.; Hunt, K.; Barber, A.; Byrne, A.W.; Butler, F.; Casey, M.; Griffin, J.; Lane, E.; McEvoy, D.; et al. Incubation period of COVID-19: A rapid systematic review and meta-analysis of observational research. Bmj Open 2020, 10, e039652. [Google Scholar] [CrossRef] [PubMed]
- Becker, N.G.; Watson, L.F.; Carlin, J.B. A method of non-parametric back-projection and its application to aids data. Stat. Med. 1991, 10, 1527–1542. [Google Scholar] [CrossRef]
- Chau, P.H.; Yip, P.S.F.; Cui, J.S. Reconstructing the incidence of human immunodeficiency virus (HIV) in Hong Kong by using data from HIV positive tests and diagnoses of acquired immune deficiency syndrome. J. R. Stat. Soc. 2003, 52, 237–248. [Google Scholar] [CrossRef]
- Chau, P.H.; Yip, P.S.F. Monitoring the severe acute respiratory syndrome epidemic and assessing effectiveness of interventions in Hong Kong Special Administrative Region. J. Epidemiol. Community Heal. 2003, 57, 766–769. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Global surveillance for COVID-19 caused by human infection with COVID-19 virus (Interim guidance). Available online: https://apps.who.int/iris/bitstream/handle/10665/331506/WHO-2019-nCoV-SurveillanceGuidance-2020.6-eng.pdf (accessed on 31 August 2020).
- Van Rossum, G.; Drake, F.L. Python 3 Reference Manual; CreateSpace: Scotts Valley, CA, USA, 2009. [Google Scholar]
- Yip, P.S.; Cheung, Y.; Chau, P.H.; Law, Y. The impact of epidemic outbreak. Crisis 2010, 31, 86–92. [Google Scholar] [CrossRef]
- Cheung, Y.T.; Chau, P.H.; Yip, P.S.F. A revisit on older adults suicides and Severe Acute Respiratory Syndrome (SARS) epidemic in Hong Kong. Int. J. Geriatr. Psychiatry 2008, 23, 1231–1238. [Google Scholar] [CrossRef]
- Yip, P.S.F.; Chau, P.H. Physical distancing and emotional closeness amidst COVID-19. Crisis 2020, 41, 153–155. [Google Scholar] [CrossRef]
- Quilty, B.J.; Clifford, S.; Flasche, S.; Eggo, R.M. Group2C. nCoV working Effectiveness of airport screening at detecting travellers infected with novel coronavirus (2019-nCoV). Eurosurveillance 2020, 25, 2000080. [Google Scholar] [CrossRef] [PubMed]
- Viner, R.M.; Russell, S.J.; Croker, H.; Packer, J.; Ward, J.; Stansfield, C.; Mytton, O.; Bonell, C.; Booy, R. School closure and management practices during coronavirus outbreaks including COVID-19: A rapid systematic review. Lancet Child Adolesc. Health 2020, 4, 397–404. [Google Scholar] [CrossRef]

© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chau, P.H.; Li, W.Y.; Yip, P.S.F. Construction of the Infection Curve of Local Cases of COVID-19 in Hong Kong using Back-Projection. Int. J. Environ. Res. Public Health 2020, 17, 6909. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17186909
Chau PH, Li WY, Yip PSF. Construction of the Infection Curve of Local Cases of COVID-19 in Hong Kong using Back-Projection. International Journal of Environmental Research and Public Health. 2020; 17(18):6909. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17186909
Chicago/Turabian StyleChau, Pui Hing, Wei Ying Li, and Paul S. F. Yip. 2020. "Construction of the Infection Curve of Local Cases of COVID-19 in Hong Kong using Back-Projection" International Journal of Environmental Research and Public Health 17, no. 18: 6909. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17186909




