Sexual Behaviours and Practices before and after Phase I/II HIV Vaccine Trial: A Qualitative Study among Volunteers in Dar es Salaam Tanzania
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design, Setting, and Population
2.2. Sampling and Sample Size
2.3. Data Collection
- Why do you think people of your age engage in sexual relationships?
- What is your current experience in a sexual relationship?
- What is your experience in the use of protection against HIV and other sexually transmitted infections (STIs)?
- What is your perception concerning HIV or other STIs testing?
- To what extent was the information about safer sex practice beneficial to you during and after HIV vaccine trials?
- What challenges did you face to maintain safer sexual practices after participation in HIV vaccine trials?
2.4. Data Analysis
2.5. Ethical Consideration
3. Results
3.1. Socio-Demographic Characteristics of Informants
3.2. Themes and Categories
3.3. Engaging in Risky Sexual Behavior and Practices before the HIV Vaccine Trial
3.3.1. Multiple Sexual Partners
3.3.2. Unprotected Sexual Intercourse
3.3.3. Perceived Barriers to the Use of Condoms
- Inability to access condoms
- Perception of condoms
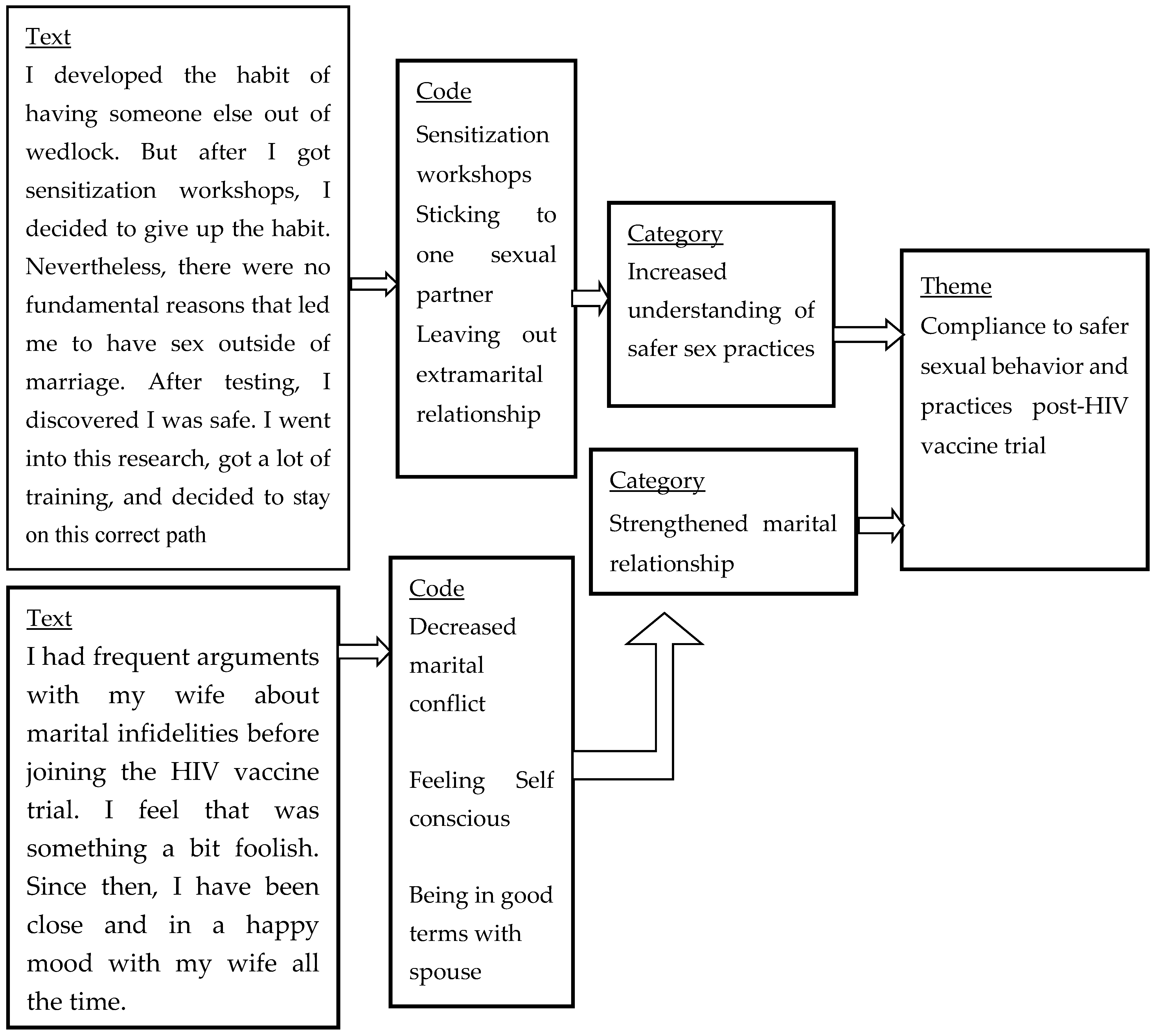
3.4. Compliance to Safer Sexual Behavior and Practices Post-HIV Vaccine Trial
3.4.1. Strengthened Marital Relationship
3.4.2. Increased Understanding of the Safer Sexual Practice
3.4.3. Regular HIV Testing with Extramarital Relationships
3.5. Challenges after the HIV Vaccine Trial
3.5.1. Experienced HIV Vaccine-Induced Seropositivity
3.5.2. Perceived HIV Protection after Vaccine Trial
3.6. Opportunities towards Safer Sexual Behavior and Practices
3.6.1. Continuing Safer Sex Educational Interventions
3.6.2. Involvement of the Community in Promoting Safer Sexual Practices
4. Discussion
4.1. Engaging in Risky Sexual Behavior and Practices before the HIV Vaccine Trial
4.2. Compliance to Safer Sexual Behavior and Practices after the HIV Vaccine Trial
4.3. Challenges after the HIV Vaccine Trial
4.4. Opportunities towards Safer Sexual Behavior and Practices
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- United Nations Joint Programme on HIV/AIDS (UNAIDS). UNAIDS Data 2019. 2019, p.476. Available online: https://www.unaids.org/sites/default/files/media_asset/2019-UNAIDS-data_en.pdf_aidsinfo.unaids.org (accessed on 4 April 2020).
- NBS. Tanzania HIV Impact Survey (THIS) a Population-Based HIV Impact Assessment; NBS: Dar es Salaam, Tanzania, 2018. [Google Scholar]
- Pinkerton, S.D.; Abramson, P.R. Effectiveness of condoms in preventing HIV transmission. Soc. Sci. Med. 1997, 44, 1303–1312. [Google Scholar] [CrossRef]
- Fomboh, R.N. Assessment of youths’ knowledge on the use of condom for HIV/AIDS prevention in the North West region of Cameroon. Sindhological Stud. 2016, 4, 35–40. [Google Scholar]
- Bonell, C.; Imrie, J. Behavioural interventions to prevent HIV infection: Rapid evolution, increasing rigour, moderate success. Br. Med. Bull. 2001, 58, 155–170. [Google Scholar] [CrossRef]
- Setswe, G. Abstinence and faithfulness programmes for prevention of HIV/AIDS among young people: What are the current debates? S. Afr. Fam. Pract. 2007, 49, 5–10. [Google Scholar] [CrossRef]
- Painter, T.M.; Diaby, K.L.; Matia, D.M.; Lin, L.S.; Sibailly, T.S.; Kouassi, M.K.; Ekpini, E.R.; Roels, T.H.; Wiktor, S.Z. Faithfulness to partners: A means to prevent HIV infection, a source of HIV infection risks, or both? A qualitative study of women’s experiences in Abidjan, Côte d’Ivoire. Afr. J. AIDS Res. 2007, 6, 25–31. [Google Scholar] [CrossRef]
- Hicks, M.R.; Kogan, S.M.; Cho, J.; Oshri, A. Condom Use in the Context of Main and Casual Partner Concurrency: Individual and Relationship Predictors in a Sample of Heterosexual African American Men. Am. J. Mens Health 2017, 11, 585–591. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murphy, E.M.; Greene, M.E.; Mihailovic, A.; Olupot-Olupot, P. Was the “ABC” approach (abstinence, being faithful, using condoms) responsible for Uganda’s decline in HIV? PLoS Med. 2006, 3, 1443–1447. [Google Scholar] [CrossRef] [PubMed]
- WHO. Antiretroviral Treatment as Prevention (TasP): Opportunities and Challenges. WHO: Geneva, Switzerland, 2012. [Google Scholar]
- Hull, M.W.; Montaner, J.S.G. HIV treatment as prevention: The key to an AIDS-free generation. J. Food Drug Anal. 2013, 21, S95–S101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guest, G.; Shattuck, D.; Johnson, L.; Akumatey, B.; Kekawo Clarke, E.E.; Chen, P.L.; MacQueen, K. Changes in sexual risk behavior among participants in a prep hiv prevention trial. Sex. Transm. Dis. 2008, 35, 1002–1008. [Google Scholar] [PubMed]
- Faini, D.; Hanson, C.; Baisley, K.; Kapiga, S.; Hayes, R. Sexual behaviour, changes in sexual behaviour and associated factors among women at high risk of HIV participating in feasibility studies for prevention trials in Tanzania. PLoS ONE 2020, 15, e0231766. [Google Scholar] [CrossRef]
- Eaton, L.A.; Kalichman, S.C. Risk Compensation in HIV Prevention: Implications for Vaccines, Microbicides, and Other Biomedical HIV Prevention Technologies. Curr. HIV/AIDS Rep. 2007, 4, 165–172. [Google Scholar] [CrossRef] [PubMed]
- MacPhail, C.L.; Sayles, J.N.; Cunningham, W.; Newman, P.A. Perceptions of sexual risk compensation following posttrial HIV vaccine uptake among young South Africans. Qual. Health Res. 2012, 22, 668–678. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marcus, J.L.; Glidden, D.V.; Mayer, K.H.; Liu, A.Y.; Buchbinder, S.P.; Amico, K.R.; Mcmahan, V.; Kallas, E.G.; Montoya-Herrera, O.; Pilotto, J.; et al. No Evidence of sexual risk compensation in the iPrEx trial of daily oral HIV preexposure prophylaxis. PLoS ONE 2013, 8, e81997. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersson, K.M.; Vardas, E.; Niccolai, L.M.; Van Niekerk, R.M.; Mogale, M.M.; Holdsworth, I.M.; Bogoshi, M.; McIntyre, J.A.; Gray, G.E. Anticipated changes in sexual risk behaviour following vaccination with a low-efficacy HIV vaccine: Survey results from a South African township. Int. J. STD AIDS 2013, 23, 736–741. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barrington, C.; Moreno, L.; Kerrigan, D. Perceived influence of an HIV vaccine on sexual-risk behaviour in the Dominican Republic. Cult. Health Sex. 2008, 10, 391–401. [Google Scholar] [CrossRef]
- Bartholow, B.N.; Buchbinder, S.; Celum, C.; Goli, V.; Koblin, B.; Para, M.; Marmor, M.; Novak, R.M.; Mayer, K.; Creticos, C.; et al. HIV Sexual Risk Behavior Over 36 Months of Follow-Up in the World’ s First HIV Vaccine Efficacy Trial. J. Acquir. Immune Defic. Syndr. 2005, 39, 90–101. [Google Scholar] [CrossRef]
- Gray, G.E.; Metch, B.; Churchyard, G.; Mlisana, K.; Nchabeleng, M.; Allen, M.; Moodie, Z.; Kublin, J.; Bekker, L.-G. Does participation in an HIV vaccine efficacy trial affect risk behaviour in South Africa? Vaccine 2013, 31, 2089–2096. [Google Scholar] [CrossRef] [Green Version]
- Buchbinder, S.P.; Metch, B.; Holte, S.E.; Scheer, S.; Coletti, A.; Vittinghoff, E. Determinants of Enrollment in a Preventive HIV Vaccine Trial Hypothetical Versus Actual Willingness and Barriers to Participation. J. Acquir. Immune Defic. Sndromes 2004, 36, 604–612. [Google Scholar] [CrossRef]
- Cooper, C.J.; Metch, B.; Dragavon, J.; Coombs, R.W.; Baden, L.R. Vaccine-Induced HIV Seropositivity/Reactivity in Noninfected HIV Vaccine Recipients. JAMA J. Am. Med. Assoc. 2010, 304, 275–283. [Google Scholar] [CrossRef] [Green Version]
- Allen, M.; Israel, H.; Rybczyk, K.; Pugliese, M.A.; Loughran, K.; Wagner, L.; Erb, S. Trial-related discrimination in HIV vaccine clinical trials. AIDS Res. Hum. Retrovir. 2001, 17, 667–674. [Google Scholar] [CrossRef]
- Durier, C.; Desaint, C.; Lelièvre, J.D.; Silbermann, B.; Pialoux, G.; Cuzin, L.; Bonnet, B.; Poizot-Martin, I.; Bouakane, A.; Paul, C.; et al. Long-term safety and vaccine-induced seropositivity in healthy volunteers from HIV vaccine trials. AIDS 2019, 33, 2061–2071. [Google Scholar] [CrossRef] [PubMed]
- Sheon, A.R.; Wagner, L.; McElrath, M.J.; Keefer, M.C.; Zimmerman, E.; Israel, H.; Berger, D.; Fast, P. Prevention of discrimination Against Volunteers in Prophylactic HIV vaccine Trials: Lessons from a Phasse II Trial. J. Acquir. Immune Defic. Sndromes Hum. Retrovirol. 1998, 19, 519–526. [Google Scholar] [CrossRef] [PubMed]
- Voronin, Y.; Zinszner, H.; Karg, C.; Brooks, K.; Coombs, R.; Hural, J.; Holt, R.; Fast, P.; Allen, M.; Busch, M.; et al. HIV Vaccine-Induced Sero-Reactivity: A Challenge for Trial Participants, Researchers, and Physicians. Vaccine 2015, 33, 1243–1249. [Google Scholar] [CrossRef] [Green Version]
- Newman, P.A.; Duan, N.; Rudy, E.T.; Roberts, K.J.; Swendeman, D. Posttrial HIV Vaccine Adoption : Concerns, Motivators, and. J. Acquir. Immune Defic. Syndr. 2004, 37, 1393–1403. [Google Scholar] [CrossRef] [PubMed]
- Tarimo, E.A.M.; Munseri, P.; Aboud, S.; Bakari, M.; Mhalu, F.; Sandstrom, E. Experiences of social harm and changes in sexual practices among volunteers who had completed a phase I/II HIV vaccine trial employing HIV-1 DNA priming and HIV-1 MVA boosting in Dar es Salaam, Tanzania. PLoS ONE 2014, 9, e90938. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tarimo, E.A.M.; Kakoko, D.C.V.; Kohi, T.W.; Bakari, M.; Sandstrom, E.; Siyame, D.; Mhalu, F.; Kulane, A. Gender aspects on HIV prevention efforts and participation in HIV vaccine trials among Police officers in Dar es Salaam, Tanzania. BMC Public Health 2018, 18, 905. [Google Scholar] [CrossRef] [Green Version]
- Tarimo, E.A.M.; Kohi, T.W.; Bakari, M.; Kulane, A. A qualitative study of perceived risk for HIV transmission among police officers in Dar es Salaam, Tanzania. BMC Public Health 2013, 13, 785. [Google Scholar] [CrossRef] [Green Version]
- Bakari, M.; Lyamuya, E.; Mugusi, F.; Aris, E.; Chale, S.; Magao, P.; Jossiah, R.; Janabi, M.; Swai, A.; Pallangyo, N.; et al. The prevalence and incidence of HIV-1 infection and syphilis in a cohort of police officers in Dar es Salaam, Tanzania: A potential population for HIV vaccine trials. AIDS 2000, 14, 313–320. [Google Scholar] [CrossRef]
- Malterud, K.; Siersma, V.D.; Guassora, A.D. Sample Size in Qualitative Interview Studies : Guided by Information Power. Qual. Health Res. 2016, 26, 1753–1760. [Google Scholar] [CrossRef]
- Graneheim, U.H.; Lundman, B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Educ. Today 2004, 24, 105–112. [Google Scholar] [CrossRef]
- Richard, W. Brislin. Back Translation for Cross-Cultural Research. J. Cross Cult. Psychol. 1970, 1, 185–216. [Google Scholar]
- Beutel, M.E.; Stöbel-Richter, Y.; Brähler, E. Sexual desire and sexual activity of men and women across their lifespans: Results from a representative German community survey. BJU Int. 2008, 101, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Dawson, L.H.; Shih, M.C.; De Moor, C.; Shrier, L. Reasons why adolescents and young adults have sex: Associations with psychological characteristics and sexual behavior. J. Sex Res. 2008, 45, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Kogan, S.M.; Brody, G.H.; Chen, Y.F.; Grange, C.M.; Slater, L.T.M.; DiClemente, R.J. Risk and protective factors for unprotected intercourse among rural African American young adults. Public Health Rep. 2010, 125, 709–717. [Google Scholar] [CrossRef] [Green Version]
- Tucker, J.S.; Ryan, G.W.; Golinelli, D.; Munjas, B.; Wenzel, S.L.; Kennedy, D.P.; Green, H.D.; Zhou, A.; Munjas, B. Substance Use and Other Risk Factors for Unprotected Sex: Results From An Event-Based Study of Homeless Youth. AIDS Behav. 2012, 16, 1699–1707. [Google Scholar] [CrossRef] [Green Version]
- Okafor, U.O.; Crutzen, R.; Aduak, Y.; Adebajo, S.; van den Borne, H.W. Behavioural interventions promoting condom use among female sex workers in sub-Saharan Africa: A systematic review. Afr. J. AIDS Res. 2017, 16, 257–268. [Google Scholar] [CrossRef] [Green Version]
- Wiyeh, A.B.; Mome, R.K.B.; Mahasha, P.W.; Kongnyuy, E.J.; Wiysonge, C.S. Effectiveness of the female condom in preventing HIV and sexually transmitted infections: A systematic review and meta-analysis. BMC Public Health 2020, 20, 1–17. [Google Scholar] [CrossRef]
- Liu, H.; Su, Y.; Zhu, L.; Xing, J.; Wu, J.; Wang, N. Effectiveness of ART and condom use for prevention of sexual HIV transmission in serodiscordant couples: A systematic review and meta-analysis. PLoS ONE 2014, 9, e111175. [Google Scholar] [CrossRef] [Green Version]
- Mubyazi, G.M.; Exavery, A.; Tenu, F.; Massaga, J.J.; Rugemalila, J.; Malebo, H.M.; Wiketye, V.; Makundi, E.A.; Ikingura, J.K.; Mushi, A.; et al. Determinants of demand for condoms to prevent HIV infections among barmaids and guesthouse workers in two districts, Tanzania. BMC Res. Notes 2015, 8, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Sarkar, N.N. Barriers to condom use. Eur. J. Contracept. Reprod. Health Care 2008, 13, 114–122. [Google Scholar] [CrossRef]
- Milhausen, R.R.; McKay, A.; Graham, C.A.; Sanders, S.A.; Crosby, R.A.; Yarber, W.L.; Wood, J.R. Do Associations Between Pleasure Ratings and Condom Use During Penile–Vaginal Intercourse Vary by Relationship Type?: A Study of Canadian University Students. J. Sex. Res. 2017, 55, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Randolph, M.E.; Pinkerton, S.D.; Bogart, L.M.; Cecil, H.; Abramson, P.R. Sexual pleasure and condom use. Arch. Sex. Behav. 2007, 36, 844–848. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Katikiro, E.; Njau, B. Motivating Factors and Psychosocial Barriers to Condom Use among out-of-School Youths in Dar es Salaam, Tanzania: A Cross Sectional Survey Using the Health Belief Model. ISRN AIDS 2012, 2012, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Hensel, D.J.; Stupiansky, N.W.; Herbenick, D.; Dodge, B.; Reece, M. Sexual Pleasure during Condom-Protected Vaginal Sex among Heterosexual Men. J. Sex. Med. 2012, 9, 1272–1276. [Google Scholar] [CrossRef] [PubMed]
- Swensen, C.H.; Eskew, R.W.; Kohlhepp, K.A. Five factors in long-term marriages. Lifestyles 1984, 7, 94–106. [Google Scholar] [CrossRef]
- Velten, J.; Margraf, J. Satisfaction guaranteed? How individual, partner, and relationship factors impact sexual satisfaction within partnerships. PLoS ONE 2017, 12, e0172855. [Google Scholar] [CrossRef]
- He, J.; Wang, Y.; Du, Z.; Liao, J.; He, N.; Hao, Y. Peer education for HIV prevention among high-risk groups: A systematic review and meta-analysis. BMC Infect. Dis. 2020, 20, 338. [Google Scholar] [CrossRef]
- Nall, A.; Chenneville, T.; Rodriguez, L.M.; O’Brien, J.L. Factors affecting hiv testing among youth in kenya. Int. J. Environ. Res. Public Health 2019, 16, 1450. [Google Scholar] [CrossRef] [Green Version]
- Djan, D. Factors Affecting the Attitude of Young People towards HIV Testing Uptake in Rural Ghana. J. HIV RetroVirus 2018, 4, 10–15. [Google Scholar] [CrossRef]
- MacPhail, C.; Pettifor, A.; Moyo, W.; Rees, H. Factors associated with HIV testing among sexually active South African youth aged 15–24 years. AIDS Care Psychol. Socio Med. Asp. AIDS/HIV 2009, 21, 456–467. [Google Scholar] [CrossRef]
- Evangeli, M.; Pady, K.; Wroe, A.L. Which Psychological Factors are Related to HIV Testing? A Quantitative Systematic Review of Global Studies. AIDS Behav. 2016, 20, 880–918. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thapinta, D.; Jenkins, R.A.; Celentino, D.D.; Nitayaphan, S.; Buapunh, P.; Triapon, A.; Morgan, P.A.; Khamboonruang, C.; Suwanarach, C.; Yutabootr, Y.; et al. Evaluation of Behavioural and Social Issues among Thai HIV vaccine trial volunteers. J. Acquir. Immune Defic. Sndromes Hum. Retrovirol. 1999, 20, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Milford, C.; Barsdorf, N.; Kafaar, Z. What should South African HIV vaccine trials do about social harms? AIDS Care Psychol. Socio Med. Asp. AIDS/HIV 2007, 19, 1110–1117. [Google Scholar] [CrossRef] [PubMed]
- Van Braeckel, E.; Koutsoukos, M.; Bourguignon, P.; Clement, F.; McNally, L.; Leroux-Roels, G. Vaccine-induced HIV seropositivity: A problem on the rise. J. Clin. Virol. 2011, 50, 334–337. [Google Scholar] [CrossRef] [Green Version]
- Traeger, M.W.; Schroeder, S.E.; Wright, E.J.; Hellard, M.E.; Cornelisse, V.J.; Doyle, J.S.; A Stoové, M. Effects of Pre-exposure Prophylaxis for the Prevention of Human Immunodeficiency Virus Infection on Sexual Risk Behavior in Men Who Have Sex with Men: A Systematic Review and Meta-analysis. Clin. Infect. Dis. 2018, 67, 676–686. [Google Scholar] [CrossRef]
- Guest, G.; McLellan-Lemal, E.; Matia, D.M.; Pickard, R.; Fuchs, J.; McKirnan, D.; Neidig, J.L. HIV vaccine efficacy trial participation: Men who have sex with men’s experiences of risk reduction counselling and perceptions of risk behaviour change. AIDS Care Psychol. Socio Med. Asp. AIDS/HIV 2005, 17, 46–57. [Google Scholar] [CrossRef]
- Motswaledi, M.S.; Kasvosve, I.; Oguntibeju, O.O. The role of red blood cells in enhancing or preventing HIV infection and other diseases. BioMed. Res. Int. 2013, 2013, 16–18. [Google Scholar] [CrossRef] [Green Version]
- Davison, G.M.; Hendrickse, H.L.; Matsha, T.E. Do Blood Group Antigens and the Red Cell Membrane Influence Human Immunodeficiency Virus Infection ? Cells 2020, 9, 845. [Google Scholar] [CrossRef] [Green Version]
- Motswaledi, M.S.; Kasvosve, I.; Oguntibeju, O.O. Blood Group antigens, C.; Lub and P1 may have a role in HIV infection in Africans. PLoS ONE 2016, 11, e0149883. [Google Scholar] [CrossRef] [Green Version]
- Gust, D.A.; Soud, F.; Hardnett, F.; Malotte, C.K.; Rose, C.; Kebaabetswe, P.; Makgekgenene, L.; Henderson, F.; Paxton, L.; Segolodi, T.; et al. Evaluation of sexual risk behavior among study participants in the TDF2 PrEP study among heterosexual adults in Botswana. J. Acquir. Immune Defic. Sndromes 2016, 73, 556–563. [Google Scholar] [CrossRef]
- UNAIDS. Good Participatory Practice: Guideline for Biomedical HIV Prevention Trials 2011; Global Advocacy for HIV Prevention: Geneva, Switzerland, 2011. [Google Scholar]
- Tarimo, E.A.M.; Ambikile, J.; Munseri, P.; Bakari, M. Perception of potential harm and benefits of HIV vaccine trial participation: A qualitative study from urban Tanzania. PLoS ONE 2019, 14, e0224831. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Swartz, L.; Kagee, A. Community participation in AIDS vaccine trials: Empowerment or science? Soc. Sci. Med. 2006, 63, 1143–1146. [Google Scholar] [CrossRef] [PubMed]
- Derlega, V.J.; Durham, B.; Gockel, B.; Sholis, D. Sex differences in self-disclosure: Effects of topic content, friendship, and partner’s sex. Sex Roles 1981, 7, 433–447. [Google Scholar] [CrossRef]
| Socio-Demographic Characteristics | Number (%) |
|---|---|
| Age: mean = 43.9 years, (SD = 6.6) at the time of this study | |
| Gender | |
| Male | 17(70.8) |
| Female | 7(29.2) |
| Marital status | |
| Single | 1(4.2) |
| Married | 18(75.0) |
| Divorced | 1(4.2) |
| Separated | 2(8.3) |
| Widowed | 2(8.3) |
| Level of education | |
| Primary | 11(45.8) |
| Secondary | 13(54.2) |
| Work Experience (Years) | |
| 10–19 | 14(58.3) |
| 20–29 | 7(29.2) |
| 30–39 | 2(8.3) |
| ≥40 | 1(4.2) |
| Themes | Category |
|---|---|
| Engaging in risky sexual behavior and practices before the HIV vaccine trial | Multiple sexual partners (11/24) |
| Unprotected sexual intercourse (14/24) | |
| Perceived barriers to the use of condoms (17/24) | |
| Compliance to safer sexual behavior and practices after HIV vaccine trial | Strengthened marital relationship (8/24) |
| Increased understanding of safer sex practice (13/24) | |
| Regular HIV testing with extramarital partners (17/24) | |
| Challenges after HIV vaccine trial | Experienced HIV vaccine-induced seropositivity (6/24) |
| Perceived protection after HIV vaccine trial (9/24) | |
| Opportunities towards safer sexual practices after HIV vaccine trial | Continuing safer sex educational intervention (15/24) |
| Involvement of the community in promoting safer sexual practices (10/24) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iseselo, M.K.; Tarimo, E.A.M.; Sandstrom, E.; Kulane, A. Sexual Behaviours and Practices before and after Phase I/II HIV Vaccine Trial: A Qualitative Study among Volunteers in Dar es Salaam Tanzania. Int. J. Environ. Res. Public Health 2020, 17, 7193. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17197193
Iseselo MK, Tarimo EAM, Sandstrom E, Kulane A. Sexual Behaviours and Practices before and after Phase I/II HIV Vaccine Trial: A Qualitative Study among Volunteers in Dar es Salaam Tanzania. International Journal of Environmental Research and Public Health. 2020; 17(19):7193. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17197193
Chicago/Turabian StyleIseselo, Masunga K., Edith A. M. Tarimo, Eric Sandstrom, and Asli Kulane. 2020. "Sexual Behaviours and Practices before and after Phase I/II HIV Vaccine Trial: A Qualitative Study among Volunteers in Dar es Salaam Tanzania" International Journal of Environmental Research and Public Health 17, no. 19: 7193. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17197193






