Distal Displacement of Maxillary Sinus Anterior Wall Versus Conventional Sinus Lift with Lateral Access: A 3-Year Retrospective Computerized Tomography Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Inclusion Criteria
- sinus lifting, with either backward displacement of the anterior wall or with lateral access, and grafting with particulate bovine graft;
- dental implants placed in the augmented sinus very close to the native anterior wall (premolar area);
- preoperative and postoperative maxillary computerized tomographic scans.
- Patients were excluded if any of the following information was in their medical record:
- no loaded implant during the 3-year follow-up;
- lack of postoperative radiographic 3-dimensional (3D) data up to 3 years after augmentation;
- preoperative bone thickness between the sinus floor and the edentulous crest of less than 3 mm;
- patients without chronic systemic diseases;
- excessive smoking habits (>10 cigarettes a day);
- alcohol or drug abuse;
- patients unwilling or unable to cooperate in maintaining oral hygiene and following medical prescriptions.
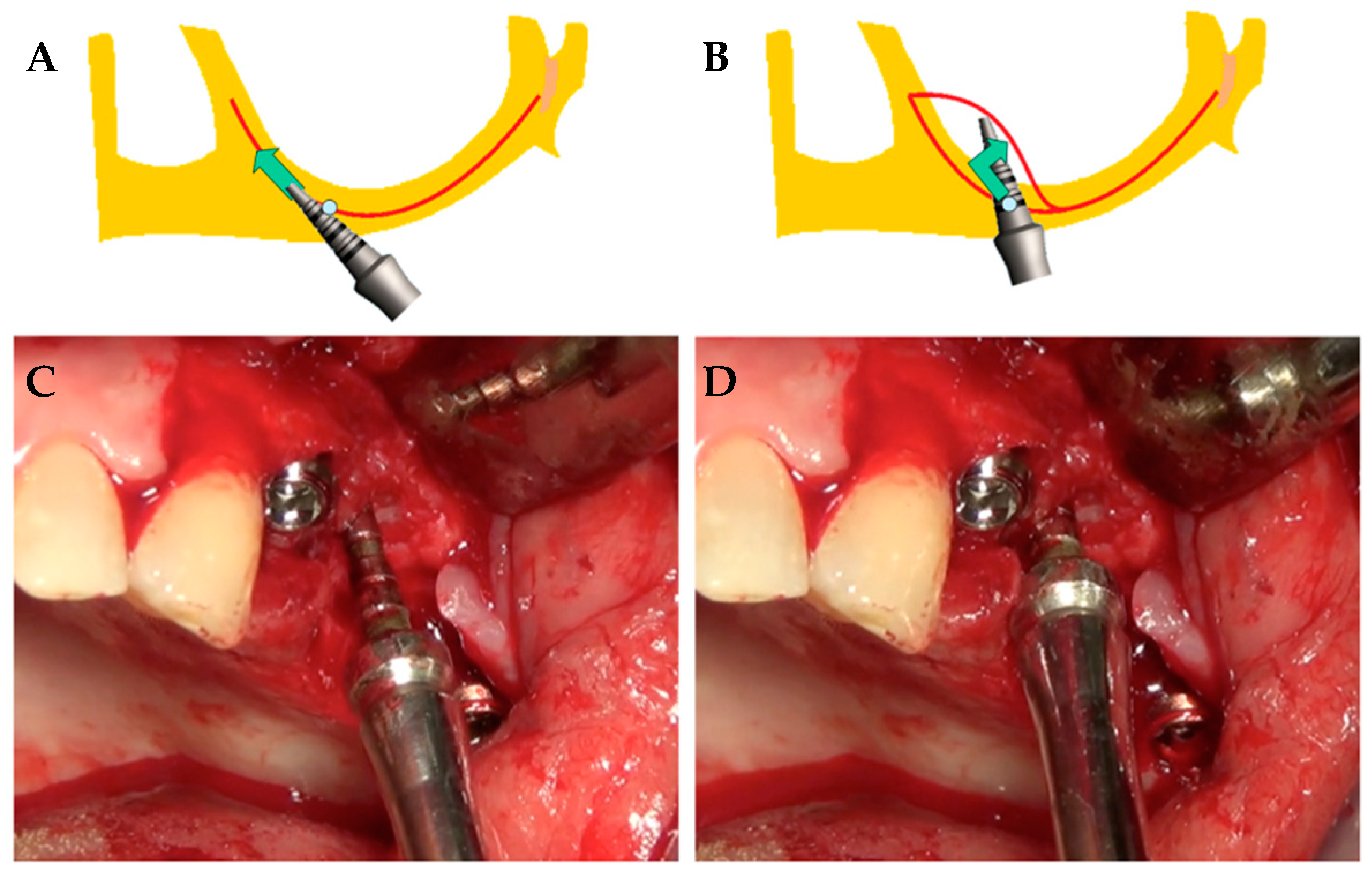
2.3. Surgical Procedures
2.4. Clinical Variables
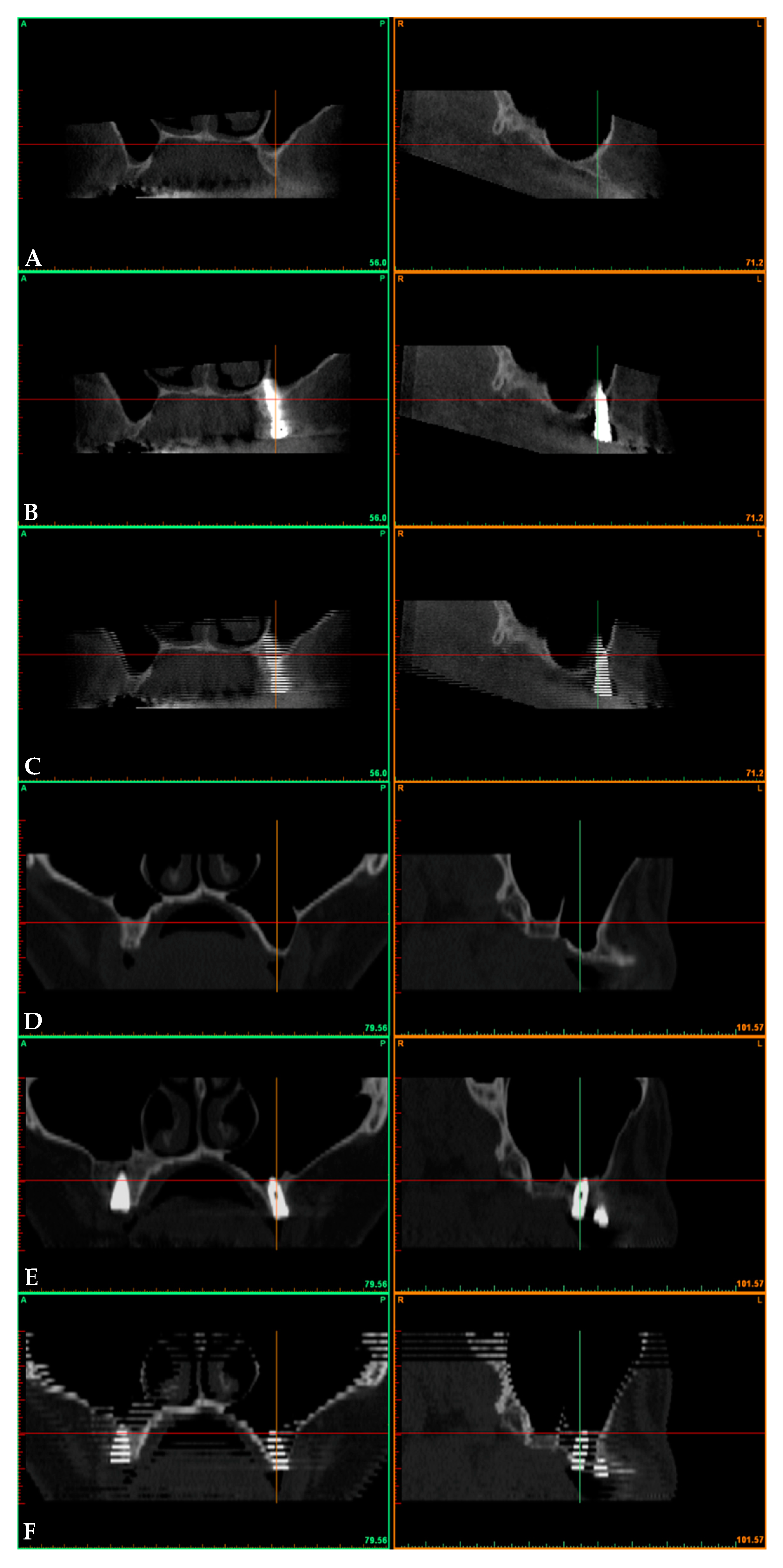
2.5. Radiographic Assessments
2.6. Statistical Analysis
3. Result
3.1. Results
3.2. Surgical and Prosthetic Findings
3.3. Radiological Evaluation
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Rancitelli, D.; Borgonovo, A.E.; Cicciù, M.; Re, D.; Rizza, F.; Frigo, A.C.; Maiorana, C. Maxillary Sinus Septa and Anatomic Correlation with the Schneiderian Membrane. J. Craniofac. Surg. 2015, 26, 1394–1398. [Google Scholar] [CrossRef] [PubMed]
- Listl, S.; Faggion, C.M., Jr. An economic evaluation of different sinus lift techniques. Comp. Study J. Clin. Periodontol. 2010, 37, 777–787. [Google Scholar] [CrossRef] [PubMed]
- Beretta, M.; Cicciù, M.; Bramanti, E.; Maiorana, C. Schneider membrane elevation in presence of sinus septa: Anatomic features and surgical management. Int. J. Dent. 2012, 2012, 261905. [Google Scholar] [CrossRef]
- Khoury, F. Augmentation of the sinus floor with mandibular bone block and simultaneous implantation: A 6-year clinical investigation. Int. J. Oral Maxillofac. Implant. 1999, 14, 557–564. [Google Scholar]
- Boyne, P.J.; James, R.A. Grafting of the maxillary sinus floor with autogenous marrow and bone. J. Oral Surg. 1980, 38, 613–616. [Google Scholar]
- Jensen, O.T.; Shulman, L.B.; Block, M.S.; Iacono, V.J. Report of the sinus consensus conference of 1996. Int. J. Oral Maxillofac. Implant. 1998, 13, 11–45. [Google Scholar]
- Pjetursson, B.E.; Tan, W.C.; Zwahlen, M.; Lang, N.P. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J. Clin. Periodontol. 2008, 35 (Suppl. 8), 216–240. [Google Scholar] [CrossRef]
- Tatum, H., Jr. Maxillary and sinus implant reconstructions. Dent. Clin. N. Am. 1986, 30, 207–229. [Google Scholar]
- Summers, R.B. A new concept in maxillary implant surgery: The osteotome technique. Compendium 1994, 15, 152–158. [Google Scholar]
- Summers, R.B. The osteotome technique: Part 3—Less invasive methods of elevating the sinus floor. Compendium 1994, 15, 698–704. [Google Scholar]
- Deporter, D.; Todescan, R.; Caudry, S. Simplifying management of the posterior maxilla using short, porous surfaced dental implants and simultaneous indirect sinus elevation. Int. J. Periodontics Restor. Dent. 2000, 20, 476–485. [Google Scholar]
- Bruschi, G.B.; Crespi, R.; Capparè, P.; Gherlone, E. Transcrestal Sinus Floor Elevation: A Retrospective Study of 46 Patients up to 16 Years. Clin. Implant Dent. Relat. Res. 2012, 14, 759–767. [Google Scholar] [CrossRef] [PubMed]
- Esposito, M.; Grusovin, M.G.; Rees, J.; Karasoulos, D.; Felice, P.; Alissa, R.; Worthington, H.; Coulthard, P. Effectiveness of sinus lift procedures for dental implant rehabilitation: A Cochrane systematic review. Eur. J. Oral Implantol. 2010, 3, 7–26. [Google Scholar]
- Langer, B.; Langer, L. Overlapped flap: A surgical modification for implant fixture installation. Int. J. Periodont. Restor. Dent. 1990, 10, 208–215. [Google Scholar]
- Crespi, R.; Capparè, P.; Gherlone, E. Electrical Mallet Provides Essential Advantages in Maxillary Bone Condensing. A Prospective Clinical Study. Clin. Implant Dent. Relat. Res. 2013, 15, 874–882. [Google Scholar] [CrossRef] [PubMed]
- Crespi, R.; Capparè, P.; Gherlone, E. Sinus Floor Elevation by Osteotome. Hand Mallet Versus Electrical Mallet: A Prospective Clinical Study. Int. J. Oral Maxillofac. Implant. 2012, 27, 1144–1450. [Google Scholar]
- Albrektsson, T.; Zarb, G.; Worthington, P.; Eriksson, A.R. The long term efficacy of currently used dental implants: A review and proposed criteria of success. Int. J. Oral Maxillofac. Implant. 1986, 1, 11–25. [Google Scholar]
- Smith, D.E.; Zarb, G.A. Criteria for success of osseointegrated endosseous implants. J. Prosthet. Dent. 1989, 62, 567–572. [Google Scholar] [CrossRef]
- Anusavice, K.J. Standardizing failure, success, and survival decisions in clinical studies of ceramic and metal-ceramic fixed dental prostheses. Dent. Mater. 2012, 28, 102–111. [Google Scholar] [CrossRef] [Green Version]
- Romeo, E.; Lops, D.; Margutti, E.; Ghisolfi, M.; Chiapasco, M.; Vogel, G. Long-term survival and success of oral implants in the treatment of full and partial arches: A 7-year prospective study with the ITI dental implant system. Int. J. Oral Maxillofac. Implant. 2012, 19, 247–259. [Google Scholar]
- Crespi, R.; Fabris, G.B.M.; Crespi, G.; Toti, P.; Marconcini, S.; Covani, U. Effects of different loading protocols on the bone remodeling volume of immediate maxillary single implants: A 2- to 3-year follow-up. Int. J. Oral Maxillofac. Implant. 2004, 34, 953–962. [Google Scholar] [CrossRef] [PubMed]
- Sbordone, C.; Toti, P.; Martuscelli, R.; Guidetti, F.; Porzio, M.; Sbordone, L. Evaluation of volumetric dimensional changes in posterior extraction sites with and without ARP using a novel imaging device. Clin. Implant Dent. Relat. Res. 2017, 19, 1044–1053. [Google Scholar] [CrossRef] [PubMed]
- Sbordone, C.; Toti, P.; Martuscelli, R.; Guidetti, F.; Ramaglia, L.; Sbordone, L. Retrospective volume analysis of bone remodeling after tooth extraction with and without deproteinized bovine bone mineral insertion. Clin. Oral Implant. Res. 2016, 27, 1152–1159. [Google Scholar] [CrossRef]
- Lombardo, G.; Pighi, J.; Marincola, M.; Corrocher, G.; Simancas-Pallares, M.; Nocini, P.F. Cumulative Success Rate of Short and Ultrashort Implants Supporting Single Crowns in the Posterior Maxilla: A 3-Year Retrospective Study. Int. J. Dent. 2017, 2017, 8434281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pal, U.S.; Sharma, N.K.; Singh, R.K.; Mahammad, S.; Mehrotra, D.; Singh, N.; Mandhyan, D. Direct vs. indirect sinus lift procedure: A comparison. Natl. J. Maxillofac. Surg. 2012, 3, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Maridati, P.; Stoffella, R.; Speroni, S.; Cicciu, M.; Maiorana, C. Alveolar antral artery isolation during sinus lift procedure with the double window technique. Open Dent. J. 2014, 8, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A. Maxillary Sinus Augmentation with Decellularized Bovine Compact Particles: A Radiological, Clinical, and Histologic Report of 4 Cases. Biomed. Res. Int. 2017, 2017, 2594670. [Google Scholar] [CrossRef]
- Sbordone, C.; Toti, P.; Guidetti, F.; Califano, L.; Bufo, P.; Sbordone, L. Volume changes of autogenous bone after sinus lifting and grafting procedures: A 6-year computerized tomographic follow-up. J. Craniomaxillofac. Surg. 2013, 41, 235–241. [Google Scholar] [CrossRef]
- Borges, F.L.; Dias, R.O.; Piattelli, A.; Borges, F.L.; Dias, R.O.; Piattelli, A.; Onuma, T.; Gouveia Cardoso, L.A.; Salomão, M.; Scarano, A.; et al. Simultaneous sinus membrane elevation and dental implant placement without bone graft: A 6-month follow-up study. J. Periodontol. 2011, 82, 403–412. [Google Scholar] [CrossRef]
- Cricchio, G.; Sennerby, L.; Lundgren, S. Sinus bone formation and implant survival after sinus membrane elevation and implant placement: A 1- to 6-year follow-up study. Clin. Oral Implant. Res. 2011, 22, 1200–1212. [Google Scholar] [CrossRef]
- Riben, C.; Thor, A. Follow-Up of the Sinus Membrane Elevation Technique for Maxillary Sinus Implants without the Use of Graft Material. Clin. Implant Dent. Relat. Res. 2016, 18, 895–905. [Google Scholar] [CrossRef] [PubMed]
- Leblebicioglu, B.; Ersanli, S.; Karabuda, C.; Tosun, T.; Gokdeniz, H. Radiographic evaluation of dental implants placed using an osteotome technique. J. Periodontol. 2005, 76, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Lai, H.C.; Zhuang, L.F.; Lv, X.F.; Zhang, Z.Y.; Zhang, Y.X.; Zhang, Z.Y. Osteotome sinus floor elevation with or without grafting: A preliminary clinical trial. Clin. Oral Implant. Res. 2010, 21, 520–526. [Google Scholar] [CrossRef] [PubMed]
- Fornell, J.; Johansson, L.A.; Bolin, A.; Isaksson, S.; Sennerby, L. Flapless, CBCT-guided osteotome sinus floor elevation with simultaneous implant installation. I: Radiographic examination and surgical technique. A prospective 1-year follow-up. Clin. Oral Implant. Res. 2012, 23, 28–34. [Google Scholar] [CrossRef]
- Brizuela, A.; Martín, N.; Fernández-Gonzalez, F.J.; Larrazábal, C.; Anta, A. Osteotome sinus floor elevation without grafting material: Results of a 2-year prospective study. J. Clin. Exp. Dent. 2014, 6, e479–e484. [Google Scholar] [CrossRef]
- Nedir, R.; Nurdin, N.; Vazquez, L.; Najm, S.A.; Bischof, M. Osteotome Sinus Floor Elevation without Grafting: A 10-Year Prospective Study. Clin. Implant Dent. Relat. Res. 2016, 18, 609–617. [Google Scholar] [CrossRef]
- Stacchi, C.; Lombardi, T.; Cusimano, P.; Berton, F.; Lauritano, F.; Cervino, G.; Di Lenarda, R.; Cicciù, M. Bone Scrapers Versus Piezoelectric Surgery in the Lateral Antrostomy for Sinus Floor Elevation. J. Craniofac. Surg. 2017, 28, 1191–1196. [Google Scholar] [CrossRef]
- Bortoluzzi, M.C.; Manfro, R.; Fabris, V.; Cecconello, R.; D’Agostini Derech, E. Comparative study of immediately inserted dental implants in sinus lift: 24 months of follow-up. Ann. Maxillofac. Surg. 2014, 4, 30–33. [Google Scholar] [CrossRef]
- Si, M.S.; Zhuang, L.F.; Gu, Y.X.; Mo, J.J.; Qiao, S.C.; Lai, H.C. Osteotome sinus floor elevation with or without grafting: A 3-year randomized controlled clinical trial. J. Clin. Periodontol. 2013, 40, 396–403. [Google Scholar] [CrossRef]
- Cricchio, G.; Imburgia, M.; Sennerby, L.; Lundgren, S. Immediate loading of implants placed simultaneously with sinus membrane elevation in the posterior atrophic maxilla: A two-year follow-up study on 10 patients. Clin. Implant Dent. Relat. Res. 2014, 16, 609–617. [Google Scholar] [CrossRef]


| Times | BVpreop | BV3yrs | Preop vs. 3Yrs | ||
|---|---|---|---|---|---|
| Variable | Normality Test | Variable | Normality Test | p-Value | |
| displacement (cc) n = 23 | 1.17 ± 0.34 | 0.8662 ^ | 1.53 ± 0.39 | 0.7716 ^ | 0.0017 * |
| filling (cc) n = 20 | 1.24 ± 0.41 | 0.4291 ^ | 1.94 ± 0.68 | 0.1907 ^ | <0.0001 * |
| displacement vs. filling (p-value) | 0.8076 ° | 0.0352 ° | |||
| sample size (power 80%, α 0.05, β 0.2) | 878 | 54 | |||
| Times | ΔBV (Preop→3 yrs) | %ΔBV (Preop→3yrs) | Angle of Displacement | ||
| Variable | Normality Test | Variable | Normality Test | (Degrees) | |
| displacement (cc) n = 23 | +0.36 ± 0.17 | 0.9983 ^ | +34 ± 21 | 0.0483 ^ | 31 ± 6 |
| filling (cc) n = 20 | +0.71 ± 0.31 | 0.0467 ^ | +57 ± 13 | 0.4135 ^ | - |
| distraction vs. grafting (p-value) | 0.0001 ° | 0.0001 ° | |||
| sample size (power 80%, α 0.05, β 0.2) | 14 | 20 | |||
| Times | MBL (Preop→3yrs) | Mesial vs. Distal | |||
| Variable (Mesial) | Variable (Distal) | Variable (Mean) | Normality Test | (p-Value) | |
| displacement (mm) n = 23 | 1.29 ± 0.63 | 1.66 ± 0.72 | 1.47 ± 0.38 | 0.9710 ^ | 0.1350 * |
| filling (mm) n = 20 | 1.35 ± 0.67 | 1.25 ± 0.78 | 1.30 ± 0.58 | 0.9248 ^ | 0.6980 * |
| displacement vs. filling (p-value) | 0.7977 ° | 0.0497 ° | 0.1026 ° | ||
| sample size (power 80%, α 0.05, β 0.2) | 3572 | 102 | 250 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Menchini-Fabris, G.B.; Toti, P.; Crespi, G.; Covani, U.; Crespi, R. Distal Displacement of Maxillary Sinus Anterior Wall Versus Conventional Sinus Lift with Lateral Access: A 3-Year Retrospective Computerized Tomography Study. Int. J. Environ. Res. Public Health 2020, 17, 7199. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17197199
Menchini-Fabris GB, Toti P, Crespi G, Covani U, Crespi R. Distal Displacement of Maxillary Sinus Anterior Wall Versus Conventional Sinus Lift with Lateral Access: A 3-Year Retrospective Computerized Tomography Study. International Journal of Environmental Research and Public Health. 2020; 17(19):7199. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17197199
Chicago/Turabian StyleMenchini-Fabris, Giovanni Battista, Paolo Toti, Giovanni Crespi, Ugo Covani, and Roberto Crespi. 2020. "Distal Displacement of Maxillary Sinus Anterior Wall Versus Conventional Sinus Lift with Lateral Access: A 3-Year Retrospective Computerized Tomography Study" International Journal of Environmental Research and Public Health 17, no. 19: 7199. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17197199




