COVID-19 Policy Differences across US States: Shutdowns, Reopening, and Mask Mandates
Abstract
:1. Introduction
Literature Review
2. Methods
2.1. Data
2.1.1. Outcome Variable: Daily Infection Growth Rate
2.1.2. Independent Variables
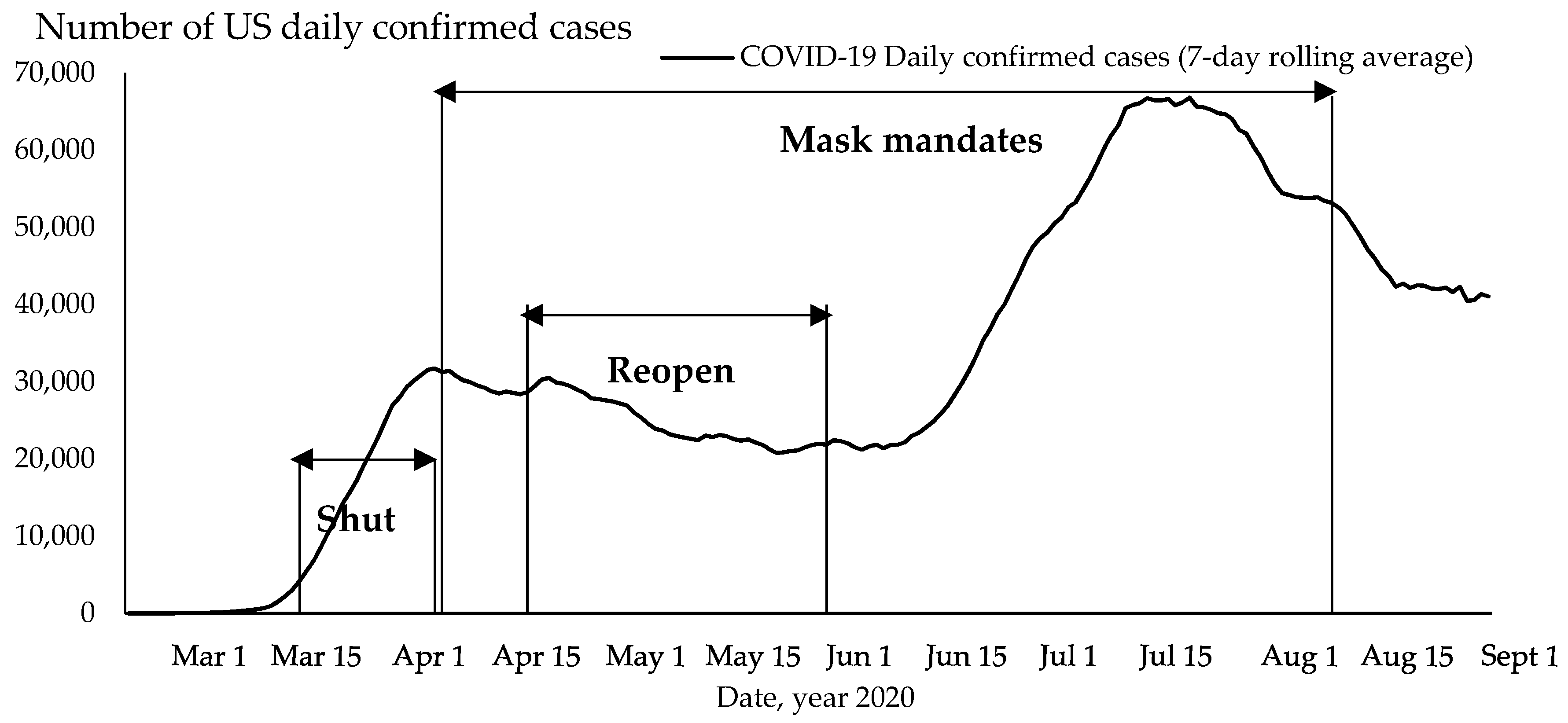
Policy Implementation
Other Independent Variables
2.2. Methodology
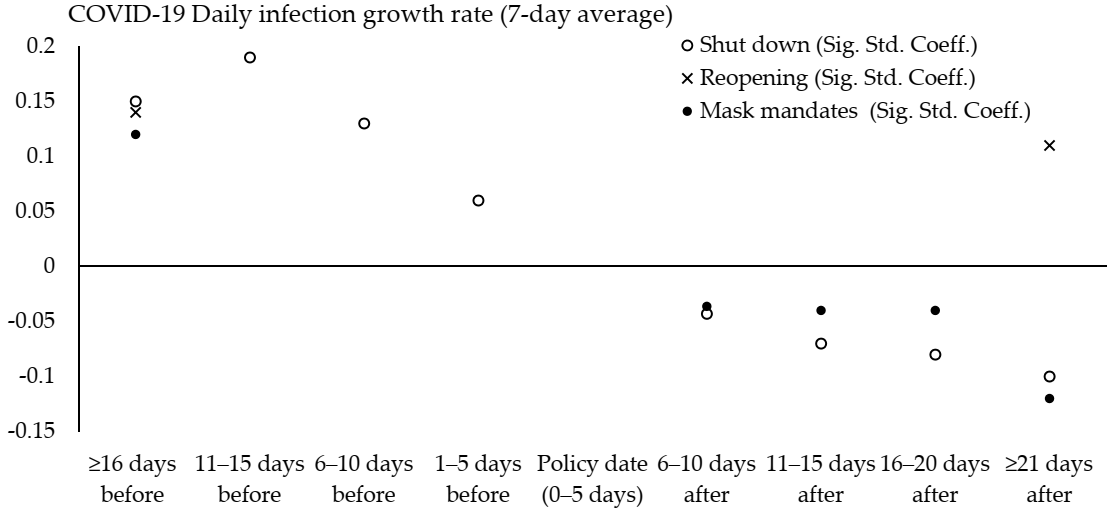
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
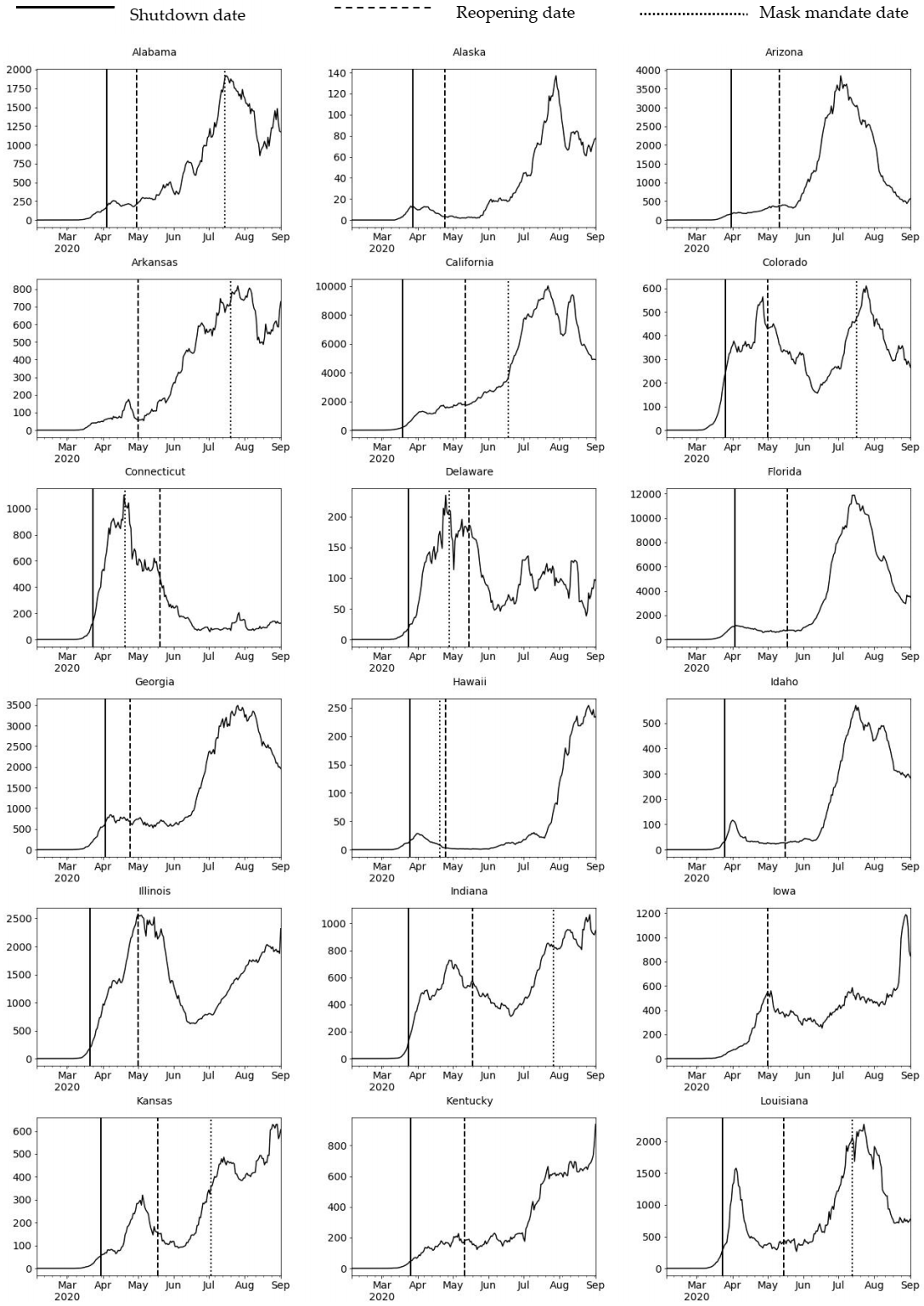
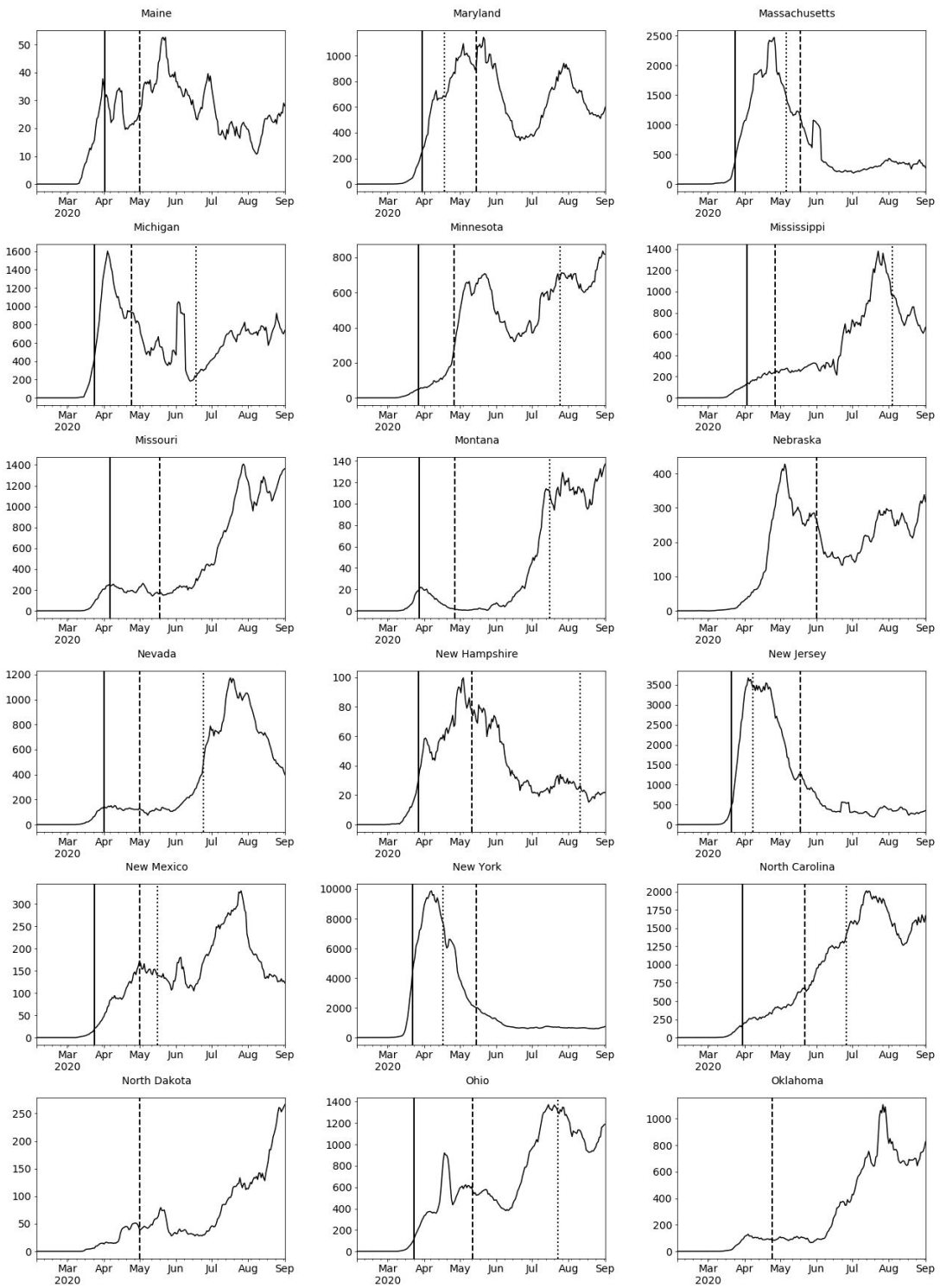
Appendix A. COVID-19 Daily Confirmed Cases (7-Day Rolling Average), US States
Appendix B
| Daily Infection Growth Rate 1 (%) | ||
|---|---|---|
| Std. Coeff. | p Value | |
| Daily test growth rate 1 (%) | 0.07 ** | (0.00) |
| Reopening implementation (1 = yes) 2 | ||
| Pre-policy period | ||
| ≥16 days before | 0.33 ** | (0.00) |
| 11–15 days before | 0.00 | (0.76) |
| 6–10 days before | −0.00 | (0.95) |
| 1–5 days before | −0.00 | (0.77) |
| Reopening date (reference, 0–5 days) | ||
| Post-policy period | ||
| 6–10 days after | 0.00 | (0.88) |
| 11–15 days after | 0.01 | (0.66) |
| 16–20 days after | 0.01 | (0.29) |
| ≥21 days after | 0.11 ** | (0.00) |
| Mask mandate implementation (1 = yes) 3 | ||
| Pre-policy period | ||
| ≥16 days before | 0.05 ** | (0.00) |
| 11–15 days before | −0.01 | (0.59) |
| 6–10 days before | −0.02 | (0.08) |
| 1–5 days before | −0.01 | (0.21) |
| Mask mandate date (reference, 0–5 days) | ||
| Post-policy period | ||
| 6–10 days after | −0.03 * | (0.01) |
| 11–15 days after | −0.03 * | (0.01) |
| 16–20 days after | −0.02 * | (0.03) |
| ≥21 days after | −0.06 ** | (0.00) |
| Medicaid expansion 4 (1 = yes) | −0.01 | (0.44) |
| Percentage essential workers 5,6 | 0.03 * | (0.03) |
| Percentage minorities 6 | 0.02 * | (0.04) |
| N | 8450 | |
| Log likelihood | −1249.20 | |
| Pseudo R | 0.11 | |
References
- New York Times. The COVID Tracking Project. Social Explorer. 2020. Available online: https://www.socialexplorer.com/ (accessed on 1 September 2020).
- Selden, T.M.; Berdahl, T.A. COVID-19 and Racial/Ethnic Disparities in Health Risk, Employment, and Household Composition. Health Aff. 2020, 39, 1624–1632. [Google Scholar] [CrossRef]
- Kraemer, M.; Yang, C.-H.; Gutiérrez, B.; Wu, C.-H.; Klein, B.; Pigott, D.M.; Du Plessis, L.; Faria, N.R.D.C.; Li, R.; Hanage, W.P.; et al. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science 2020, 368, 493–497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shim, E.; Tariq, A.; Choi, W.; Lee, Y.; Chowell, G. Transmission potential and severity of COVID-19 in South Korea. Int. J. Infect. Dis. 2020, 93, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Wee, L.E.; Conceicao, E.P.; Sim, X.Y.J.; Aung, M.K.; Tan, K.Y.; Wong, H.M.; Wijaya, L.; Tan, B.H.; Ling, M.L.; Venkatachalam, I. Minimizing intra-hospital transmission of COVID-19: The role of social distancing. J. Hosp. Infect. 2020, 105, 113–115. [Google Scholar] [CrossRef] [PubMed]
- Jarvis, C.I.; Van Zandvoort, K.; Gimma, A.; Prem, K.; Klepac, P.; Rubin, G.J.; Edmunds, W.J. Quantifying the impact of physical distance measures on the transmission of COVID-19 in the UK. BMC Med. 2020, 18, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Casares, M.; Khan, H. The Timing and Intensity of Social Distancing to Flatten the COVID-19 Curve: The Case of Spain. Int. J. Environ. Res. Public Health 2020, 17, 7283. [Google Scholar] [CrossRef]
- Goniewicz, K.; Khorram-Manesh, A.; Hertelendy, A.J.; Goniewicz, M.; Naylor, K.A.; Burkle, F.M. Current Response and Management Decisions of the European Union to the COVID-19 Outbreak: A Review. Sustainability 2020, 12, 3838. [Google Scholar] [CrossRef]
- Kim, Y.; Warner, M.E. Shrinking local autonomy: Corporate coalitions and the subnational state. Camb. J. Reg. Econ. Soc. 2018, 11, 427–441. [Google Scholar] [CrossRef]
- Warner, M.E.; Zhang, X. Social Safety Nets and COVID-19 Stay Home Orders across US States: A Comparative Policy Analysis; Cornell Health Equity Seminar: New York, NY, USA, 2020; Available online: http://cms.mildredwarner.org/p/309 (accessed on 10 October 2020).
- Kettl, D.F. States Divided: The Implications of American Federalism for COVID-19. Public Adm. Rev. 2020, 80, 595–602. [Google Scholar] [CrossRef]
- Bowman, A.O.; McKenzie, J.H. Managing a Pandemic at a Less Than Global Scale: Governors Take the Lead. Am. Rev. Public Adm. 2020, 50, 551–559. [Google Scholar] [CrossRef]
- Michener, J. Fragmented Democracy: Medicaid, Federalism, and Unequal Politics; Cambridge University Press: New York, NY, USA, 2018. [Google Scholar]
- Kaiser Family Foundation. Status of State Medicaid Expansion Decisions: Interactive Map. 2020. Available online: https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/ (accessed on 2 November 2020).
- Artiga, S.; Orgera, K.; Damico, A. Changes in Health Coverage by Race and Ethnicity since the ACA, 2010–2018. Kaiser Family Foundation 2020. Available online: https://www.kff.org/racial-equity-and-health-policy/issue-brief/changes-in-health-coverage-by-race-and-ethnicity-since-the-aca-2010-2018/ (accessed on 23 November 2020).
- Azar, K.M.; Shen, Z.; Romanelli, R.J.; Lockhart, S.H.; Smits, K.; Robinson, S.; Brown, S.; Pressman, A.R. Disparities In Outcomes Among COVID-19 Patients In A Large Health Care System in California. Health Aff. 2020, 39, 1253–1262. [Google Scholar] [CrossRef] [PubMed]
- Hsiang, S.; Allen, D.; Annan-Phan, S.; Bell, K.; Bolliger, I.; Chong, T.; Druckenmiller, H.; Huang, L.Y.; Hultgren, A.; Krasovich, E.; et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nat. Cell Biol. 2020, 584, 262–267. [Google Scholar] [CrossRef]
- Lai, S.; Ruktanonchai, N.W.; Zhou, L.; Prosper, O.F.; Luo, W.; Floyd, J.R.; Wesolowski, A.; Santillana, M.; Zhang, C.; Du, X.; et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nat. Cell Biol. 2020, 585, 410–413. [Google Scholar] [CrossRef] [PubMed]
- Pei, S.; Kandula, S.; Shaman, J. Differential effects of intervention timing on COVID-19 spread in the United States. Sci. Adv. 2020, 6, eabd6370. [Google Scholar] [CrossRef] [PubMed]
- Al-Zobbi, M.; Alsinglawi, B.; Mubin, O.; Alnajjar, F. Measurement Method for Evaluating the Lockdown Policies during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 5574. [Google Scholar] [CrossRef] [PubMed]
- Palomino, J.C.; Rodriguez, J.G.; Sebastian, R. Wage inequality and poverty effects of lockdown and social distancing in Europe. Eur. Econ. Rev. 2020, 129, 103564. [Google Scholar] [CrossRef]
- U.S. Bureau of Labor Statistics. Unemployment Statistics, 2020; Prepared by Social Explorer. 2020; US Census: Washington, DC, USA, 2020.
- Brown, S. How COVID-19 Is Affecting Black and Latino Families’ Employment and Financial Well-Being; Urban Institute: Washington, DC, USA, 2020; Available online: https://www.urban.org/urban-wire/how-covid-19-affecting-black-and-latino-families-employment-and-financial-well-being (accessed on 20 June 2020).
- Thunström, L.; Newbold, S.C.; Finnoff, D.; Ashworth, M.; Shogren, J.F. The Benefits and Costs of Using Social Distancing to Flatten the Curve for COVID-19. J. Benefit-Cost Anal. 2020, 11, 179–195. [Google Scholar] [CrossRef]
- Hodge, J.G. Federal vs. State Powers in Rush to Reopen Amid the Coronavirus Pandemic. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
- New York Times. See Coronavirus Restrictions and Mask Mandates for All 50 States. 2020. Available online: https://www.nytimes.com/interactive/2020/us/states-reopen-map-coronavirus.html (accessed on 22 June 2020).
- Lyu, W.; Wehby, G.L. Community Use of Face Masks and COVID-19: Evidence from a Natural Experiment of State Mandates in the US. Health Aff. 2020, 39, 1419–1425. [Google Scholar] [CrossRef]
- Eikenberry, S.E.; Mancuso, M.; Iboi, E.; Phan, T.; Eikenberry, K.; Kuang, Y.; Kostelich, E.; Gumel, A.B. To mask or not to mask: Modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect. Dis. Model. 2020, 5, 293–308. [Google Scholar] [CrossRef]
- Kheirallah, K.A.; Alsinglawi, B.; Alzoubi, A.; Saidan, M.N.; Mubin, O.; Alorjani, M.S.; Mzayek, F. The Effect of Strict State Measures on the Epidemiologic Curve of COVID-19 Infection in the Context of a Developing Country: A Simulation from Jordan. Int. J. Environ. Res. Public Health 2020, 17, 6530. [Google Scholar] [CrossRef] [PubMed]
- Khalifa, S.; Mohamed, B.S.; Elashal, M.H.; Du, M.; Guo, Z.; Zhao, C.; Musharraf, S.G.; Boskabady, M.H.; El-Seedi, H.H.R.; Efferth, T.; et al. Comprehensive Overview on Multiple Strategies Fighting COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 5813. [Google Scholar] [CrossRef] [PubMed]
- CNN. These Are the States Requiring People to Wear Masks When Out in Public. 2020. Available online: https://www.cnn.com/2020/06/19/us/states-face-mask-coronavirus-trnd/index.html (accessed on 31 October 2020).
- United Nations High Commission on Human Rights. COVID-19 and Minority Rights: Overview and Promising Practices. 2020. Available online: https://www.ohchr.org/Documents/Issues/Minorities/OHCHRGuidance_COVID19_MinoritiesRights.pdf (accessed on 20 November 2020).
- Zhang, X.; Warner, M.; Wethington, E. Can Age-Friendly Planning Promote Equity in Community Health Across the Rural-Urban Divide in the US? Int. J. Environ. Res. Public Health 2020, 17, 1275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pirtle, W.N.L. Racial Capitalism: A Fundamental Cause of Novel Coronavirus (COVID-19) Pandemic Inequities in the United States. Health Educ. Behav. 2020, 47, 504–508. [Google Scholar] [CrossRef] [PubMed]
- CDC. Health Equity Considerations and Racial and Ethnic Minority Groups; CDC: Atlanta, GA, USA, 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html (accessed on 20 November 2020).
- Haffajee, R.L.; Mello, M.M. Thinking Globally, Acting Locally—The U.S. Response to Covid-19. N. Engl. J. Med. 2020, 382, e75. [Google Scholar] [CrossRef] [PubMed]
- Courtemanche, C.; Garuccio, J.; Le, A.; Pinkston, J.; Yelowitz, A. Strong Social Distancing Measures in the United States Reduced the COVID-19 Growth Rate. Health Aff. 2020, 39, 1237–1246. [Google Scholar] [CrossRef]
- Lyu, W.; Wehby, G.L. Shelter-In-Place Orders Reduced COVID-19 Mortality and Reduced the Rate of Growth in Hospitalizations. Health Aff. 2020, 39, 1615–1623. [Google Scholar] [CrossRef]
- US News. Governor Unveils Plan to Get South Dakota ‘Back to Normal’. 2020. Available online: https://www.usnews.com/news/best-states/south-dakota/articles/2020-04-28/south-dakota-governor-to-unveil-plan-to-reopen-state (accessed on 22 June 2020).
- Center on Budget and Policy Priorities. 5 Million Essential and Front-line Workers Get Health Coverage through Medicaid; CBPP: Washington, DC, USA, 2020; Available online: https://www.cbpp.org/blog/5-million-essential-and-front-line-workers-get-health-coverage-through-medicaid (accessed on 16 August 2020).
- American Community Survey (2014–2018), 2020. Prepared by Social Explorer. 2020. Available online: https://www.socialexplorer.com/ (accessed on 10 June 2020).
- Chowdhury, R.; Heng, K.; Shawon, S.R.; Goh, G.; Okonofua, D.; Ochoa-Rosales, C.; Gonzalez-Jaramillo, V.; Bhuiya, A.; Reidpath, D.; Prathapan, S.; et al. Dynamic interventions to control COVID-19 pandemic: A multivariate prediction modelling study comparing 16 worldwide countries. Eur. J. Epidemiol. 2020, 35, 389–399. [Google Scholar] [CrossRef]
- Tuite, A.R.; Fisman, D.N.; Greer, A.L. Mathematical modelling of COVID-19 transmission and mitigation strategies in the population of Ontario, Canada. Can. Med Assoc. J. 2020, 192, E497–E505. [Google Scholar] [CrossRef] [Green Version]
- Prem, K.; Liu, Y.; Russell, T.W.; Kucharski, A.J.; Eggo, R.M.; Davies, N.; Jit, M.; Klepac, P.; Flasche, S.; Clifford, S.; et al. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: A modelling study. Lancet Public Health 2020, 5, e261–e270. [Google Scholar] [CrossRef] [Green Version]
- Raine, S.; Liu, A.; Mintz, J.; Wahood, W.; Huntley, K.; Haffizulla, F. Racial and Ethnic Disparities in COVID-19 Outcomes: Social Determination of Health. Int. J. Environ. Res. Public Health 2020, 17, 8115. [Google Scholar] [CrossRef] [PubMed]
- Warner, M.; Zhang, X. Serving an ageing population: Collaboration is key. Local Gov. Stud. 2020, 1–20. [Google Scholar] [CrossRef]
- Warner, M.E.; Xu, Y.; Morken, L.J. What Explains Differences in Availability of Community Health-Related Services for Seniors in the United States? J. Aging Health 2016, 29, 1160–1181. [Google Scholar] [CrossRef] [Green Version]
- Warner, M.; Zhang, X. Healthy Places for Children: The Critical Role of Engagement, Common Vision, and Collaboration. Int. J. Environ. Res. Public Health 2020, 17, 9277. [Google Scholar] [CrossRef]
| Shutdown | Reopening | Mask Mandates | |
|---|---|---|---|
| Outcome variable | |||
| Daily COVID-19 infection growth rate (7-day rolling average, %) 1 | 14.35 | 1.38 | 2.74 |
| Independent variables | |||
| Policy implementation | |||
| Number of states imposing the order 2,3 | 42 | 50 | 36 |
| Earliest policy implementation date 2,3 | 19 March 2020 | 20 April 2020 | 8 April 2020 |
| Latest policy implementation date 2,3 | 7 April 2020 | 1 June 2020 | 11 August 2020 |
| Study period (21 days before to 21 days after policy implementation) | 27 February 2020– 28 April 2020 | 30 March 2020– 22 June 2020 | 18 March 2020– 1 September 2020 |
| Number of days | 62 | 86 | 169 |
| Other independent variables | |||
| Daily test growth rate (7-day rolling average, %) 1 | 30.16 | 4.39 | 5.70 |
| Medicaid expansion (1 = yes) 4 | 0.72 | 0.72 | 0.72 |
| Percentage essential workers 5,6 | 32.90 | 32.90 | 32.90 |
| Percentage minorities 6 | 30.89 | 30.89 | 30.89 |
| Number of observations (number of days ×50 states) | 3100 | 4300 | 8450 |
| Policy Implementation Variables | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Dates Before | Pre-Policy Variables | Policy Enactment Date, 0–5 Days | Dates After | Post-Policy Variables | ||||||
| ≥16 Days | 11–15 Days | 6–10 Days | 1–5 Days | 6–10 Days | 11–15 Days | 16–20 Days | ≥21 Days | |||
| 22 March 2020–27 March 2020 | ||||||||||
| 27 February 2020 | 1 | 0 | 0 | 0 | 28 March 2020 | 1 | 0 | 0 | 0 | |
| … | … | |||||||||
| 6 March 2020 | 1 April 2020 | |||||||||
| 7 March 2020 | 0 | 1 | 0 | 0 | 2 April 2020 | 0 | 1 | 0 | 0 | |
| … | … | |||||||||
| 11 March 2020 | 6 April 2020 | |||||||||
| 12 March 2020 | 0 | 0 | 1 | 0 | 7 April 2020 | 0 | 0 | 1 | 0 | |
| … | … | |||||||||
| 16 March 2020 | 11 April 2020 | |||||||||
| 17 March 2020 | 0 | 0 | 0 | 1 | 12 April 2020 | 0 | 0 | 0 | 1 | |
| … | … | |||||||||
| 21 March 2020 | 28 April 2020 | |||||||||
| Shutdown 2 | Reopening 2 | Mask Mandates 3 | ||||
|---|---|---|---|---|---|---|
| Daily Infection Growth Rate 1 (%) | Daily Infection Growth Rate 1 (%) | Daily Infection Growth Rate 1 (%) | ||||
| Std. Coeff. | p Value | Std. Coeff. | p Value | Std. Coeff. | p Value | |
| Daily test growth rate 1 (%) | 0.03 | (0.06) | 0.04 ** | (0.00) | 0.08 ** | (0.00) |
| Policy implementation | ||||||
| Pre-policy period | ||||||
| ≥16 days before | 0.15 ** | (0.00) | 0.14 ** | (0.00) | 0.12 ** | (0.00) |
| 11–15 days before | 0.19 ** | (0.00) | 0.01 | (0.69) | −0.00 | (0.91) |
| 6–10 days before | 0.13 ** | (0.00) | −0.00 | (0.94) | −0.02 | (0.10) |
| 1–5 days before | 0.06 ** | (0.00) | −0.01 | (0.75) | −0.02 | (0.13) |
| Policy date (reference, 0–5 days) | ||||||
| Post-policy period | ||||||
| 6–10 days after | −0.04 * | (0.02) | −0.00 | (0.95) | −0.04 ** | (0.00) |
| 11–15 days after | −0.07 ** | (0.00) | 0.00 | (0.81) | −0.04 ** | (0.00) |
| 16–20 days after | −0.08 ** | (0.00) | 0.02 | (0.30) | −0.04 ** | (0.00) |
| ≥21 days after | −0.10 ** | (0.00) | 0.11 ** | (0.00) | −0.12 ** | (0.00) |
| Medicaid expansion 4 (1 = yes) | 0.02 | (0.29) | −0.04 * | (0.01) | 0.02 | (0.33) |
| Percentage essential workers 5,6 | −0.01 | (0.63) | 0.03 * | (0.04) | 0.02 | (0.18) |
| Percentage minorities 6 | 0.00 | (0.87) | 0.02 | (0.34) | 0.04 * | (0.01) |
| N | 3100 | 4300 | 8450 | |||
| Log likelihood | −1249.20 | 3567.05 | 6444.67 | |||
| Pseudo R | 0.11 | 0.02 | 0.04 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, X.; Warner, M.E. COVID-19 Policy Differences across US States: Shutdowns, Reopening, and Mask Mandates. Int. J. Environ. Res. Public Health 2020, 17, 9520. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17249520
Zhang X, Warner ME. COVID-19 Policy Differences across US States: Shutdowns, Reopening, and Mask Mandates. International Journal of Environmental Research and Public Health. 2020; 17(24):9520. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17249520
Chicago/Turabian StyleZhang, Xue, and Mildred E. Warner. 2020. "COVID-19 Policy Differences across US States: Shutdowns, Reopening, and Mask Mandates" International Journal of Environmental Research and Public Health 17, no. 24: 9520. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17249520