Association between Cardiovascular Mortality and Economic Development: A Spatio-Temporal Study for Prefectures in Japan
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources
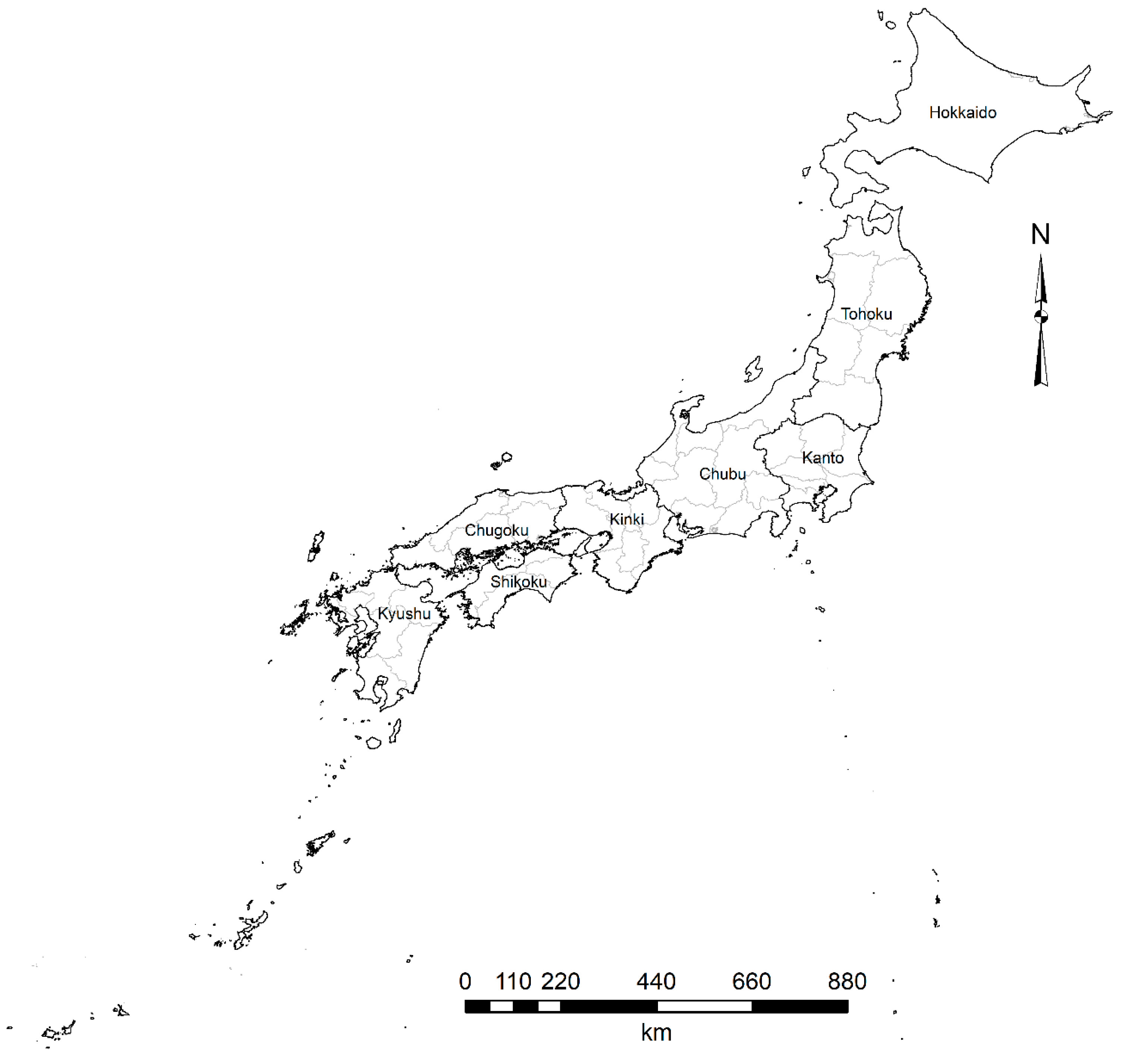
2.2. Level of Analysis
2.3. Bivariate Maps
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2017 (GBD 2017) Cause-Specific Mortality 1980–2017. Institute for Health Metrics and Evaluation (IHME): Seattle, DC, USA, 2018. Available online: http://ghdx.healthdata.org/gbd-results-tool (accessed on 10 September 2019).
- Roth, G.A.; Johnson, C.; Abajobir, A.; Abd-Allah, F.; Abera, S.F.; Abyu, G.; Ahmed, M.; Aksut, B.; Alam, T.; Alam, K.; et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017, 70, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Roth, G.A.; Dwyer-Lindgren, L.; Bertozzi-Villa, A.; Stubbs, R.W.; Morozoff, C.; Naghavi, M.; Mokdad, A.H.; Murray, C.J. Trends and patterns of geographic variation in cardiovascular mortality among US counties, 1980–2014. JAMA 2017, 317, 1976–1992. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Cardiovascular diseases (CVDs). 2017. Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 17 July 2019).
- Timaeus, I.M. Adult mortality. In Demographic Change in Sub-Saharan Africa; Foote, K.A., Hill, K.H., Martin, L.G., Eds.; National Academy Press: Washington, DC, USA, 1993; pp. 218–255. [Google Scholar]
- Lopez, A.D.; Caselli, G.; Valkonen, T. Adult Mortality in Developed Countries: From Description to Explanation; Oxford University Press: Oxford, UK, 1995. [Google Scholar]
- Lopez, A.D.; Mathers, C.D.; Ezzati, M.; Jamison, D.T.; Murray, C.J. Measuring the global burden of disease and risk factors, 1990–2001. Glob. Burd. Dis. Risk Factors 2006, 1, 1–14. [Google Scholar]
- Lopez, A.D.; Mathers, C.D.; Ezzati, M.; Jamison, D.T.; Murray, C.J. Global and regional burden of disease and risk factors, 2001: Systematic analysis of population health data. Lancet 2006, 367, 1747–1757. [Google Scholar] [CrossRef]
- Vallin, J.; Meslé, F. Convergences and divergences in mortality. A new approach to health transition. Demogr. Res. 2004, 2, 11–44. [Google Scholar] [CrossRef]
- Jerrett, M.; Burnett, R.T.; Ma, R.; Pope, C.A., III; Krewski, D.; Newbold, K.B.; Thurston, G.; Yuanli, S.; Finkelstein, N.; Calle, E.E.; et al. Spatial analysis of air pollution and mortality in Los Angeles. Epidemiology 2005, 16, 727–736. [Google Scholar] [CrossRef]
- Marmot, M. Fair society, healthy lives. In Strategic Review of Health Inequalities in England Post-2010; Marmot, M., Ed.; Department of Health: London, UK, 2010. [Google Scholar]
- World Health Organization. Noncommunicable Diseases (NCD) Country Profiles; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Roth, G.A.; Forouzanfar, M.H.; Moran, A.E.; Barber, R.; Nguyen, G.; Feigin, V.L.; Naghavi, M.; Mensah, G.A.; Murray, C.J. Demographic and epidemiologic drivers of global cardiovascular mortality. N. Engl. J. Med. 2015, 372, 1333–1341. [Google Scholar] [CrossRef] [Green Version]
- Baptista, E.A.; Queiroz, B.L. Spatial analysis of mortality by cardiovascular disease in the adult population: A study for Brazilian micro-regions between 1996 and 2015. Spat. Demogr. 2019, 7, 83–101. [Google Scholar] [CrossRef]
- Baptista, E.A.; Queiroz, B.L. The relation between cardiovascular mortality and development: Study for small areas in Brazil, 2001–2015. Demogr. Res. 2019, 41, 1437–1452. [Google Scholar] [CrossRef]
- Lopez, A.D.; Adair, T. Is the long-term decline in cardiovascular-disease mortality in high-income countries over? Evidence from national vital statistics. Int. J. Epidemiol. 2019, 48, 1815–1823. [Google Scholar] [CrossRef]
- Franco, M.; Cooper, R.S.; Bilal, U.; Fuster, V. Challenges and opportunities for cardiovascular disease prevention. Am. J. Med. 2011, 124, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, N.; Saito, E.; Kondo, N.; Inoue, M.; Ikeda, S.; Satoh, T.; Wada, K.; Stickley, A.; Katanoda, K.; Mizoue, T.; et al. What has made the population of Japan healthy? Lancet 2011, 378, 1094–1105. [Google Scholar] [CrossRef]
- Nomura, S.; Sakamoto, H.; Glenn, S.; Tsugawa, Y.; Abe, S.K.; Rahman, M.M.; Brown, J.C.; Ezoe, S.; Fitzmaurice, C.; Inokuchi, T.; et al. Population health and regional variations of disease burden in Japan, 1990–2015: A systematic subnational analysis for the Global Burden of Disease Study 2015. Lancet 2017, 390, 1521–1538. [Google Scholar] [CrossRef] [Green Version]
- Reddy, K.S.; Yusuf, S. Emerging epidemic of cardiovascular disease in developing countries. Circulation 1998, 97, 596–601. [Google Scholar] [CrossRef]
- Yusuf, S.; Reddy, S.; Ôunpuu, S.; Anand, S. Global burden of cardiovascular diseases: Part I: General considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 2001, 104, 2746–2753. [Google Scholar] [CrossRef] [Green Version]
- Yusuf, S.; Reddy, S.; Ôunpuu, S.; Anand, S. Global burden of cardiovascular diseases: Part II: Variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation 2001, 104, 2855–2864. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nowbar, A.N.; Howard, J.P.; Finegold, J.A.; Asaria, P.; Francis, D.P. Global geographic analysis of mortality from ischaemic heart disease by country, age and income: Statistics from World Health Organisation and United Nations. Int. J. Cardiol. 2014, 174, 293–298. [Google Scholar] [CrossRef] [Green Version]
- Preston, S.H. The changing relation between mortality and level of economic development. Popul. Stud. 1975, 29, 231–248. [Google Scholar] [CrossRef]
- Murray, C.J.; Lopez, A.D. Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. Lancet 1997, 349, 1498–1504. [Google Scholar] [CrossRef]
- Berger, M.C.; Messer, J. Public financing of health expenditures, insurance, and health outcomes. Appl. Econ. 2002, 34, 2105–2113. [Google Scholar] [CrossRef]
- Mackenbach, J.P.; Martikainen, P.; Looman, C.W.; Dalstra, J.A.; Kunst, A.E.; Lahelma, E. The shape of the relationship between income and self-assessed health: An international study. Int. J. Epidemiol. 2004, 34, 286–293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Subramanian, S.V.; Kawachi, I. Being well and doing well: On the importance of income for health. Int. J. Soc. Welf. 2006, 15, S13–S22. [Google Scholar] [CrossRef]
- James, S.L.; Gubbins, P.; Murray, C.J.; Gakidou, E. Developing a comprehensive time series of GDP per capita for 210 countries from 1950 to 2015. Popul. Health Metr. 2012, 10, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carstensen, L.W., Jr. Hypothesis testing using univariate and bivariate choropleth maps. Am. Cartogr. 1986, 13, 231–251. [Google Scholar] [CrossRef]
- Grossenbacher, T.; Zehr, A. Bivariate maps with ggplot2 and sf. Available online: https://github.com/grssnbchr/bivariate-maps-ggplot2-sf (accessed on 8 October 2019).
- Cockerham, W.C.; Hattori, H.; Yamori, Y. The social gradient in life expectancy: The contrary case of Okinawa in Japan. Soc. Sci. Med. 2000, 51, 11–122. [Google Scholar] [CrossRef]
- Rogers, R.G.; Wofford, S. Life expectancy in less developed countries: Socioeconomic development or public health? J. Biosoc. Sci. 1989, 21, 245–252. [Google Scholar] [CrossRef]
- Lin, R.T.; Chen, Y.M.; Chien, L.C.; Chan, C.C. Political and social determinants of life expectancy in less developed countries: A longitudinal study. BMC Public Health 2012, 12, 85. [Google Scholar] [CrossRef] [Green Version]
- Omran, A.R. The epidemiologic transition: A theory of the epidemiology of population change. Milbank Q. 2005, 83, 731–757. [Google Scholar] [CrossRef] [Green Version]
- Omran, A.R. The epidemiologic transition theory revisited thirty years later. World Health Stat. Q. 1998, 51, 99–119. [Google Scholar]
- Minagawa, Y.; Saito, Y. An analysis of factors related to disability-free life expectancy at 65 years of age across Japanese prefectures in 2010. Eur. J. Ageing 2018, 15, 15–22. [Google Scholar] [CrossRef]
- Gu, D.; Gerland, P.; Andreev, K.; Li, N.; Spoorenberg, T.; Heilig, G. Old age mortality in Eastern and South-Eastern Asia. Demogr. Res. 2013, 29, 999–1038. [Google Scholar] [CrossRef] [Green Version]
- Wada, K.; Kondo, N.; Gilmour, S.; Ichida, Y.; Fujino, Y.; Satoh, T.; Shibuya, K. Trends in cause specific mortality across occupations in Japanese men of working age during period of economic stagnation, 1980–2005: Retrospective cohort study. BMJ 2012, 344, e1191. [Google Scholar] [CrossRef] [Green Version]
- Suhrcke, M.; Urban, D. Are cardiovascular diseases bad for economic growth? Health Econ. 2010, 19, 1478–1496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suzuki, E.; Kashima, S.; Kawachi, I.; Subramanian, S.V. Geographic inequalities in all-cause mortality in Japan: Compositional or contextual? PLoS ONE 2012, 7, e39876. [Google Scholar] [CrossRef] [PubMed]
- Gilmour, S.; Liao, Y.; Bilano, V.; Shibuya, K. Burden of disease in Japan: Using national and subnational data to inform local health policy. J. Prev. Med. Public Health 2014, 47, 136–143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomoike, H.; Yokoyama, H.; Sumita, Y.; Hanai, S.; Kada, A.; Okamura, T.; Yoshikawa, J.; Doi, Y.; Hori, M.; Tei, C. Nationwide distribution of cardiovascular practice in Japan. Circ. J. 2015, 1058–1067. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakaya, T.; Dorling, D. Geographical inequalities of mortality by income in two developed island countries: A cross-national comparison of Britain and Japan. Soc. Sci. Med. 2005, 60, 2865–2875. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, E.; Kashima, S.; Kawachi, I.; Subramanian, S.V. Social and geographic inequalities in premature adult mortality in Japan: A multilevel observational study from 1970 to 2005. BMJ Open 2012, 2, e000425. [Google Scholar] [CrossRef]
- Tanaka, H.; Toyokawa, S.; Tamiya, N.; Takahashi, H.; Noguchi, H.; Kobayashi, Y. Changes in mortality inequalities across occupations in Japan: A national register based study of absolute and relative measures, 1980–2010. BMJ Open 2017, 7, e015764. [Google Scholar] [CrossRef]
- Anand, S.S.; Yusuf, S.; Jacobs, R.; Davis, A.D.; Yi, Q.; Gerstein, H.; Montague, P.A.; Lonn, E.; SHARE-AP Investigators. Risk factors, atherosclerosis, and cardiovascular disease among Aboriginal people in Canada: The Study of Health Assessment and Risk Evaluation in Aboriginal Peoples (SHARE-AP). Lancet 2001, 358, 1147–1153. [Google Scholar] [CrossRef]
- National Cancer Center. Cancer Registry and Statistics; Cancer Information Service, National Cancer Center: Tokyo, Japan, 2019.
- Uechi, K.; Asakura, K.; Masayasu, S.; Sasaki, S. Within-country variation of salt intake assessed via urinary excretion in Japan: A multilevel analysis in all 47 prefectures. Hypertens. Res. 2017, 40, 598. [Google Scholar] [CrossRef] [PubMed]
- Tomonari, T.; Fukuda, M.; Miura, T.; Mizuno, M.; Wakamatsu, T.Y.; Ichikawa, T.; Miyagi, S.; Shirasawa, Y.; Ito, A.; Yoshida, A.; et al. Is salt intake an independent risk factor of stroke mortality? Demographic analysis by regions in Japan. J. Am. Soc. Hypertens. 2011, 5, 456–462. [Google Scholar] [CrossRef]
- Fukuda, Y.; Nakao, H.; Yahata, Y.; Imai, H. Are health inequalities increasing in Japan? The trends of 1955 to 2000. Biosci. Trends 2007, 1, 38–42. [Google Scholar]
- Kondo, N.; Subramanian, S.V.; Kawachi, I.; Takeda, Y.; Yamagata, Z. Economic recession and health inequalities in Japan: Analysis with a national sample, 1986–2001. J. Epidemiol. Commun. Health 2008, 62, 869–875. [Google Scholar] [CrossRef] [Green Version]




| Region | Obs | (Mean; Std. Dev.) 1996–2000 | (Mean; Std. Dev.) 2001–2005 | (Mean; Std. Dev.) 2006–2010 | (Mean; Std. Dev.) 2011–2015 | t-Statistic | p-Value | 95% CI | |
|---|---|---|---|---|---|---|---|---|---|
| Crude mortality rate from cardiovascular disease (CMRCVD), Males | Hokkaido | 1 | 474.98; NA | 405.75; NA | 361.77; NA | 323.34; NA | |||
| Tohoku | 6 | 553.38; 38.80 | 469.05; 29.58 | 417.72; 27.17 | 369.21; 26.28 | ||||
| Kanto | 7 | 522.14; 31.05 | 437.72; 32.35 | 388.10; 29.35 | 351.49; 26.21 | ||||
| Chubu | 9 | 491.94; 15.14 | 408.23; 14.80 | 360.97; 8.39 | 323.44; 9.64 | ||||
| Kinki | 7 | 489.94; 27.61 | 405.59; 23.26 | 360.31; 29.62 | 324.72; 28.10 | ||||
| Chugoku | 5 | 474.98; 30.40 | 404.07; 27.11 | 356.34; 27.62 | 319.19; 32.51 | ||||
| Shikoku | 4 | 491.57; 22.52 | 415.69; 28.70 | 364.80; 27.21 | 323.15; 17.16 | ||||
| Kyushu | 8 | 465.92; 23.78 | 388.38; 18.15 | 342.84; 20.69 | 306.90; 22.13 | ||||
| Overall | 47 | 497.36; 37.22 | 416.75; 33.54 | 368.92; 32.05 | 330.36; 29.38 | ||||
| 1996–2000 vs. 2011–2015 | 46.11 | 2.47 × 10−5 *** | [156.94–173.91] | ||||||
| 2001–2005 vs. 2011–2015 | 37.83 | 7.91 × 10−6 *** | [81.21–92.04] | ||||||
| 2006–2010 vs. 2011–2015 | 25.55 | 1.63 × 10−6 *** | [35.32–42.53] | ||||||
| Crude mortality rate from cardiovascular disease (CMRCVD), Females | Hokkaido | 1 | 491.44; NA | 396.91; NA | 348.19; NA | 313.01; NA | |||
| Tohoku | 6 | 554.84; 11.11 | 445.27; 7.57 | 388.09; 8.72 | 354.28; 11.03 | ||||
| Kanto | 7 | 563.71; 27.40 | 451.81; 26.40 | 390.99; 27.68 | 355.13; 27.80 | ||||
| Chubu | 9 | 528.05; 27.66 | 416.58; 24.81 | 358.28; 18.34 | 325.33; 17.01 | ||||
| Kinki | 7 | 539.47; 27.84 | 422.29; 15.35 | 366.48; 15.05 | 331.99; 20.20 | ||||
| Chugoku | 5 | 497.84; 16.79 | 403.62; 15.93 | 352.20; 25.89 | 321.87; 20.46 | ||||
| Shikoku | 4 | 511.08; 11.44 | 410.81; 13.49 | 350.94; 9.57 | 318.57; 7.02 | ||||
| Kyushu | 8 | 482.74; 33.49 | 394.30; 23.89 | 338.93; 19.89 | 305.78; 17.80 | ||||
| Overall | 47 | 525.33; 36.86 | 420.26; 27.55 | 363.40; 25.67 | 329.92; 24.70 | ||||
| 1996–2000 vs. 2011–2015 | 39.10 | 0.00025 *** | [181.24–204.57] | ||||||
| 2001–2005 vs. 2011–2015 | 53.39 | 1.01 × 10−5 *** | [85.49–93.42] | ||||||
| 2006–2010 vs. 2011–2015 | 54.45 | 1.12 × 10−7 *** | [32.06–4.97] | ||||||
| Gross domestic product (GDP) per capita | Hokkaido | 1 | 3,576,523.69; NA | 3,445,865.77; NA | 3,262,695.18; NA | 3,325,173.73; NA | |||
| Tohoku | 6 | 3,433,025.80; 245,683.36 | 3,300,966.69; 226,786.18 | 3,239,177.83; 171,658.33 | 3,371,702.00; 170,078.19 | ||||
| Kanto | 7 | 4,136,858.70; 1,476,231.68 | 4,092,849.10; 1,650,936.63 | 4,030,843.22; 1,544,894.14 | 4,028,397.73; 1,374,579.74 | ||||
| Chubu | 9 | 4,027,838.09; 383,857.03 | 3,984,126.60; 399,028.09 | 3,897,409.85; 385,307.15 | 3,904,454.85; 383,350.29 | ||||
| Kinki | 7 | 3,722,355.37; 646,676.02 | 3,668,318.87; 581,919.85 | 3,664,780.70; 606,194.88 | 3,668,725.81; 582,640.94 | ||||
| Chugoku | 5 | 3,657,794.16; 263,055.59 | 3,620,914.78; 239,808.56 | 3,577,668.03; 354,972.07 | 3,579,774.87; 408,422.44 | ||||
| Shikoku | 4 | 3,364,701.83; 282,630.10 | 3,410,899.08; 255,786.70 | 3,348,105.72; 343,002.51 | 3,482,203.85; 344,634.99 | ||||
| Kyushu | 8 | 3,143,210.18; 336,695.29 | 3,127,890.12; 299,193.59 | 3,106,894.10; 282,077.80 | 3,152,639.24; 243,958.09 | ||||
| Overall | 47 | 3,666,663.39; 722,486.00 | 3,621,452.60; 758,963.03 | 3,569,781.58; 729,090.58 | 3,609,024.42; 664,783.23 | ||||
| 1996–2000 vs. 2011–2015 | 1.83 | 0.00031 *** | [−20,202.24–157,511.17] | ||||||
| 2001–2005 vs. 2011–2015 | 0.69 | 1.82 × 10−5 *** | [−41,816.68–76,506.40] | ||||||
| 2006–2010 vs. 2011–2015 | −2.38 | 2.48 × 10−5 *** | [−96,151.28–−223.09] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baptista, E.A.; Kakinuma, K.; Queiroz, B.L. Association between Cardiovascular Mortality and Economic Development: A Spatio-Temporal Study for Prefectures in Japan. Int. J. Environ. Res. Public Health 2020, 17, 1311. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17041311
Baptista EA, Kakinuma K, Queiroz BL. Association between Cardiovascular Mortality and Economic Development: A Spatio-Temporal Study for Prefectures in Japan. International Journal of Environmental Research and Public Health. 2020; 17(4):1311. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17041311
Chicago/Turabian StyleBaptista, Emerson Augusto, Kaoru Kakinuma, and Bernardo Lanza Queiroz. 2020. "Association between Cardiovascular Mortality and Economic Development: A Spatio-Temporal Study for Prefectures in Japan" International Journal of Environmental Research and Public Health 17, no. 4: 1311. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17041311





