Global Mapping of Interventions to Improve Quality of Life of People with Diabetes in 1990–2018
Abstract
:1. Introduction
2. Materials and Methods
2.1. Searching Strategy
- -
- First, we produced a QOL dataset by employing topic search terms such as “quality of life” and “well-being” on the WOS. Among 441,617 records after searching, we excluded 114,212 documents (including: 4364 papers that were published in 2019; 25,543 documents that were non-English articles; 84,083 documents that were not articles/reviews; and 222 documents that had insufficient author information). A total of 327,405 quality of life-related papers were used for the next step.
- -
- Second, we filtered the papers regarding interventions in diabetes populations by using a set of title/abstract terms related to “diabetes” (AND “intervention” OR “trial”) and saved it as the final dataset. A total of 323,079 papers were excluded, resulting in 4326 papers that were included in the next phase.
- -
- Finally, we screened 4326 papers by reading their titles and abstracts and excluded 3626 papers that were not eligible according to the inclusion and exclusion criteria.
2.2. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Cho, N.H.; Shaw, J.E.; Karuranga, S.; Huang, Y.; da Rocha Fernandes, J.D.; Ohlrogge, A.W.; Malanda, B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 2018, 138, 271–281. [Google Scholar] [CrossRef]
- Smith-Palmer, J.; Bae, J.P.; Boye, K.S.; Norrbacka, K.; Hunt, B.; Valentine, W.J. Evaluating health-related quality of life in type 1 diabetes: A systematic literature review of utilities for adults with type 1 diabetes. Clin. Outcomes Res. Ceor 2016, 8, 559–571. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Diabetes: Fact Sheet. Available online: https://www.who.int/news-room/fact-sheets/detail/diabetes (accessed on 29 July 2019).
- Baena-Diez, J.M.; Penafiel, J.; Subirana, I.; Ramos, R.; Elosua, R.; Marin-Ibanez, A.; Guembe, M.J.; Rigo, F.; Tormo-Diaz, M.J.; Moreno-Iribas, C.; et al. Risk of Cause-Specific Death in Individuals With Diabetes: A Competing Risks Analysis. Diabetes Care 2016, 39, 1987–1995. [Google Scholar] [CrossRef] [Green Version]
- Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1859–1922. [CrossRef] [Green Version]
- Jing, X.; Chen, J.; Dong, Y.; Han, D.; Zhao, H.; Wang, X.; Gao, F.; Li, C.; Cui, Z.; Liu, Y.; et al. Related factors of quality of life of type 2 diabetes patients: A systematic review and meta-analysis. Health Qual. Life Outcomes 2018, 16, 189. [Google Scholar] [CrossRef]
- Saleh, F.; Ara, F.; Mumu, S.J.; Hafez, M.A. Assessment of health-related quality of life of Bangladeshi patients with type 2 diabetes using the EQ-5D: A cross-sectional study. BMC Res. Notes 2015, 8, 497. [Google Scholar] [CrossRef] [Green Version]
- Costanza, R.; Fisher, B.; Ali, S.; Beer, C.; Bond, L.; Boumans, R.; Danigelis, N.L.; Dickinson, J.; Elliott, C.; Farley, J.; et al. Quality of life: An approach integrating opportunities, human needs, and subjective well-being. Ecol. Econ. 2007, 61, 267–276. [Google Scholar] [CrossRef]
- Galloway, S.; Bell, D.; Hamilton, C.; Scullion, A. Quality of Life and Well-Being: Measuring the Benefits of Culture and Sport: Literature Review and Thinkpiece; 0755929071; Analytical Services Division, Scottish Executive Education Department: Edinburgh, UK, 2006.
- Cummins, R.A. Quality of Life Definition and Terminology: A Discussion Document from the International Society for Quality of Life Studies; International Society for Quality-of-Life Studies: Gilbert, AZ, USA, 1998. [Google Scholar]
- WHOQoL Group. Study protocol for the World Health Organization project to develop a Quality of Life assessment instrument (WHOQOL). Qual. Life Res. 1993, 2, 153–159. [Google Scholar] [CrossRef]
- Zhang, X.; Norris, S.L.; Chowdhury, F.M.; Gregg, E.W.; Zhang, P. The effects of interventions on health-related quality of life among persons with diabetes: A systematic review. Med. Care 2007, 45, 820–834. [Google Scholar] [CrossRef]
- Luscombe, F.A. Health-related quality of life measurement in type 2 diabetes. Value Health J. Int. Soc. Pharm. Outcomes Res. 2000, 3 (Suppl. 1), 15–28. [Google Scholar] [CrossRef] [Green Version]
- Watkins, K.; Connell, C.M. Measurement of health-related QOL in diabetes mellitus. Pharmacoeconomics 2004, 22, 1109–1126. [Google Scholar] [CrossRef] [PubMed]
- Cai, H.; Li, G.; Zhang, P.; Xu, D.; Chen, L. Effect of exercise on the quality of life in type 2 diabetes mellitus: A systematic review. Qual. Life Res. 2017, 26, 515–530. [Google Scholar] [CrossRef] [PubMed]
- Magwood, G.S.; Zapka, J.; Jenkins, C. A Review of Systematic Reviews Evaluating Diabetes Interventions. Diabetes Educ. 2008, 34, 242–265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ayadurai, S.; Hattingh, H.L.; Tee, L.B.G.; Md Said, S.N. A Narrative Review of Diabetes Intervention Studies to Explore Diabetes Care Opportunities for Pharmacists. J. Diabetes Res. 2016, 2016, 11. [Google Scholar] [CrossRef] [Green Version]
- Massey, C.N.; Feig, E.H.; Duque-Serrano, L.; Wexler, D.; Moskowitz, J.T.; Huffman, J.C. Well-being interventions for individuals with diabetes: A systematic review. Diabetes Res. Clin. Pract. 2019, 147, 118–133. [Google Scholar] [CrossRef]
- Emami, Z.; Hariri, N.; Khamseh, M.E.; Nooshinfard, F. Mapping diabetes research in Middle Eastern countries during 2007–2013: A scientometric analysis. Med. J. Islamic Repub. Iran 2018, 32, 84. [Google Scholar] [CrossRef]
- Rasolabadi, M.; Khaledi, S.; Ardalan, M.; Kalhor, M.M.; Penjvini, S.; Gharib, A. Diabetes Research in Iran: A Scientometric Analysis of Publications Output. Acta Inform. Med. 2015, 23, 160–164. [Google Scholar] [CrossRef] [Green Version]
- Bruggmann, D.; Richter, T.; Klingelhofer, D.; Gerber, A.; Bundschuh, M.; Jaque, J.; Groneberg, D.A. Global architecture of gestational diabetes research: Density-equalizing mapping studies and gender analysis. Nutr. J. 2016, 15, 36. [Google Scholar] [CrossRef] [Green Version]
- Ramin, S.; Gharebaghi, R.; Heidary, F. Scientometric Analysis and Mapping of Scientific Articles on Diabetic Retinopathy. Med. Hypothesisdiscov. Innov. Ophthalmol. J. 2015, 4, 81–100. [Google Scholar]
- Sweileh, W.M. Analysis of global research output on diabetes depression and suicide. Ann. Gen. Psychiatry 2018, 17, 44. [Google Scholar] [CrossRef] [Green Version]
- Tabatabaei-Malazy, O.; Ramezani, A.; Atlasi, R.; Larijani, B.; Abdollahi, M. Scientometric study of academic publications on antioxidative herbal medicines in type 2 diabetes mellitus. J. Diabetes Metab. Disord. 2016, 15, 48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martín-Martín, A.; Orduna-Malea, E.; Delgado López-Cózar, E. Coverage of highly-cited documents in Google Scholar, Web of Science, and Scopus: A multidisciplinary comparison. Scientometrics 2018, 116, 2175–2188. [Google Scholar] [CrossRef] [Green Version]
- Clarivate Analytics. Web of Science databases. Available online: https://clarivate.com/products/web-of-science/databases/ (accessed on 26 June 2019).
- Krzywinski, M.; Schein, J.; Birol, I.; Connors, J.; Gascoyne, R.; Horsman, D.; Jones, S.J.; Marra, M.A. Circos: An information aesthetic for comparative genomics. Genome Res. 2009, 19, 1639–1645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valle, D.; Albuquerque, P.; Zhao, Q.; Barberan, A.; Fletcher, R.J., Jr. Extending the Latent Dirichlet Allocation model to presence/absence data: A case study on North American breeding birds and biogeographical shifts expected from climate change. Glob. Chang. Biol. 2018, 24, 5560–5572. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, C.; Zare, A.; Trinh, H.N.; Omotara, G.O.; Cobb, J.T.; Lagaunne, T.A. Partial Membership Latent Dirichlet Allocation for Soft Image Segmentation. IEEE Trans. Image Process. 2017, 26, 5590–5602. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.M.; Wei, C.P.; Hsiao, F.Y. Modeling healthcare data using multiple-channel latent Dirichlet allocation. J. Biomed. Inf. 2016, 60, 210–223. [Google Scholar] [CrossRef]
- Gross, A.; Murthy, D. Modeling virtual organizations with Latent Dirichlet Allocation: A case for natural language processing. Neural. Netw. 2014, 58, 38–49. [Google Scholar] [CrossRef]
- Crowther, C.A.; Hiller, J.E.; Moss, J.R.; McPhee, A.J.; Jeffries, W.S.; Robinson, J.S. Effect of Treatment of Gestational Diabetes Mellitus on Pregnancy Outcomes. N. Engl. J. Med. 2005, 352, 2477–2486. [Google Scholar] [CrossRef] [Green Version]
- Backonja, M.; Beydoun, A.; Edwards, K.R.; Schwartz, S.L.; Fonseca, V.; Hes, M.; LaMoreaux, L.; Garofalo, E. Gabapentin for the symptomatic treatment of painful neuropathy in patients with diabetes mellitus: A randomized controlled trial. JAMA 1998, 280, 1831–1836. [Google Scholar] [CrossRef] [Green Version]
- Schauer, P.R.; Bhatt, D.L.; Kirwan, J.P.; Wolski, K.; Brethauer, S.A.; Navaneethan, S.D.; Aminian, A.; Pothier, C.E.; Kim, E.S.H.; Nissen, S.E.; et al. Bariatric Surgery versus Intensive Medical Therapy for Diabetes—3-Year Outcomes. N. Engl. J. Med. 2014, 370, 2002–2013. [Google Scholar] [CrossRef] [Green Version]
- Weinberger, M.; Oddone, E.Z.; Henderson, W.G. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. N. Engl. J. Med. 1996, 334, 1441–1447. [Google Scholar] [CrossRef]
- Davies, M.J.; Heller, S.; Skinner, T.C.; Campbell, M.J.; Carey, M.E.; Cradock, S.; Dallosso, H.M.; Daly, H.; Doherty, Y.; Eaton, S.; et al. Effectiveness of the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: Cluster randomised controlled trial. BMJ 2008, 336, 491–495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harati, Y.; Gooch, C.; Swenson, M.; Edelman, S.; Greene, D.; Raskin, P.; Donofrio, P.; Cornblath, D.; Sachdeo, R.; Siu, C.O.; et al. Double-blind randomized trial of tramadol for the treatment of the pain of diabetic neuropathy. Neurology 1998, 50, 1842–1846. [Google Scholar] [CrossRef] [PubMed]
- Watson, C.P.N.; Moulin, D.; Watt-Watson, J.; Gordon, A.; Eisenhoffer, J. Controlled-release oxycodone relieves neuropathic pain: A randomized controlled trial in painful diabetic neuropathy. Pain 2003, 105, 71–78. [Google Scholar] [CrossRef]
- O’Neil, P.M.; Smith, S.R.; Weissman, N.J.; Fidler, M.C.; Sanchez, M.; Zhang, J.; Raether, B.; Anderson, C.M.; Shanahan, W.R. Randomized Placebo-Controlled Clinical Trial of Lorcaserin for Weight Loss in Type 2 Diabetes Mellitus: The BLOOM-DM Study. Obesity 2012, 20, 1426–1436. [Google Scholar] [CrossRef]
- Schauer, P.R.; Bhatt, D.L.; Kirwan, J.P.; Wolski, K.; Aminian, A.; Brethauer, S.A.; Navaneethan, S.D.; Singh, R.P.; Pothier, C.E.; Nissen, S.E.; et al. Bariatric Surgery versus Intensive Medical Therapy for Diabetes—5-Year Outcomes. N. Engl. J. Med. 2017, 376, 641–651. [Google Scholar] [CrossRef] [Green Version]
- Mingrone, G.; Panunzi, S.; De Gaetano, A.; Guidone, C.; Iaconelli, A.; Nanni, G.; Castagneto, M.; Bornstein, S.; Rubino, F. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet 2015, 386, 964–973. [Google Scholar] [CrossRef]
- Satterfield, D.W.; Volansky, M.; Caspersen, C.J.; Engelgau, M.M.; Bowman, B.A.; Gregg, E.W.; Geiss, L.S.; Hosey, G.M.; May, J.; Vinicor, F. Community-Based Lifestyle Interventions to Prevent Type 2 Diabetes. Diabetes Care 2003, 26, 2643–2652. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shrestha, P.; Ghimire, L. A review about the effect of life style modification on diabetes and quality of life. Glob. J. Health Sci. 2012, 4, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Trikkalinou, A.; Papazafiropoulou, A.K.; Melidonis, A. Type 2 diabetes and quality of life. World J. Diabetes 2017, 8, 120–129. [Google Scholar] [CrossRef]
- Liu, L.; Jiao, J.H.; Chen, L. Bibliometric study of diabetic retinopathy during 2000–2010 by ISI. Int. J. Ophthalmol. 2011, 4, 333–336. [Google Scholar] [CrossRef] [PubMed]
- Somogyi, A.; Schubert, A.J.S. Correlation between national bibliometric and health indicators: The case of diabetes. Scientometrics 2005, 62, 285–292. [Google Scholar] [CrossRef]
- Khanal, P. Bringing all together for research capacity building in LMICs. Lancet Glob. Health 2017, 5, e868. [Google Scholar] [CrossRef] [Green Version]
- ESSENCE on Health Research. Seven Principle for Strengthening Research Capacity in Low-and-middle-income Countries: Simple Ideas in a Complex World; TDR/World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Ali, N.; Hill, C.; Kennedy, A.; IJsselmuiden, C. What Factors Influence National Health Research Agendas in Low and Middle Income Countries; Council on Health Research for Development (COHRED): Geneva, Switzerland, 2006. [Google Scholar]
- Baghaei Lakeh, A.; Ghaffarzadegan, N. Global Trends and Regional Variations in Studies of HIV/AIDS. Sci. Rep. 2017, 7, 4170. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Year Published | Total Number of Papers | Total Citations | Mean Cite Rate Per Year | Total Usage Last 6 Months 1 | Total Usage Last 5 Years 2 | Mean Use Rate Last 6 Months | Mean Use Rate Last 5 Years |
|---|---|---|---|---|---|---|---|
| 2018 | 63 | 158 | 2.5 | 218 | 405 | 3.5 | 1.3 |
| 2017 | 56 | 556 | 5.0 | 95 | 494 | 1.7 | 1.8 |
| 2016 | 57 | 455 | 2.7 | 51 | 601 | 0.9 | 2.1 |
| 2015 | 67 | 1009 | 3.8 | 77 | 1,135 | 1.1 | 3.4 |
| 2014 | 59 | 1845 | 6.3 | 67 | 927 | 1.1 | 3.1 |
| 2013 | 46 | 1205 | 4.4 | 25 | 808 | 0.5 | 3.5 |
| 2012 | 53 | 1342 | 3.6 | 28 | 871 | 0.5 | 3.3 |
| 2011 | 41 | 1127 | 3.4 | 16 | 501 | 0.4 | 2.4 |
| 2010 | 33 | 1020 | 3.4 | 24 | 380 | 0.7 | 2.2 |
| 2009 | 34 | 1590 | 4.7 | 23 | 370 | 0.7 | 2.2 |
| 2008 | 24 | 1372 | 5.2 | 10 | 297 | 0.4 | 2.5 |
| 2007 | 27 | 1244 | 3.8 | 18 | 308 | 0.7 | 2.3 |
| 2006 | 20 | 1038 | 4.0 | 8 | 156 | 0.4 | 1.6 |
| 2005 | 18 | 2438 | 9.7 | 18 | 335 | 1.0 | 3.7 |
| 2004 | 17 | 930 | 3.6 | 3 | 94 | 0.2 | 1.1 |
| 2003 | 9 | 870 | 6.0 | 3 | 79 | 0.3 | 1.8 |
| 2002 | 13 | 1233 | 5.6 | 1 | 79 | 0.1 | 1.2 |
| 2001 | 12 | 978 | 4.5 | 0 | 65 | 0.0 | 1.1 |
| 2000 | 13 | 1355 | 5.5 | 8 | 140 | 0.6 | 2.2 |
| 1999 | 3 | 202 | 3.4 | 1 | 9 | 0.3 | 0.6 |
| 1998 | 12 | 2265 | 9.0 | 1 | 98 | 0.1 | 1.6 |
| 1997 | 4 | 208 | 2.4 | 2 | 14 | 0.5 | 0.7 |
| 1996 | 8 | 1177 | 6.4 | 4 | 60 | 0.5 | 1.5 |
| 1995 | 2 | 202 | 4.2 | 2 | 13 | 1.0 | 1.3 |
| 1994 | 3 | 220 | 2.9 | 2 | 10 | 0.7 | 0.7 |
| 1993 | 2 | 13 | 0.3 | 0 | 0 | 0.0 | 0.0 |
| 1992 | 2 | 171 | 3.2 | 0 | 12 | 0.0 | 1.2 |
| 1990 | 1 | 37 | 1.3 | 0 | 0 | 0.0 | 0.0 |
| Title | Journal | Total Citations | Publication Year | Cite Rate | Study Design | Type of Diabetes | Type of Interventions | QOL Tool |
|---|---|---|---|---|---|---|---|---|
| Effect of treatment of gestational diabetes mellitus on pregnancy outcomes [32] | New England Journal of Medicine | 1,516 | 2005 | 108.3 | RCT | gestational diabetes mellitus | dietary advice, blood glucose monitoring, and insulin therapy | SF-36 |
| Gabapentin for the symptomatic treatment of painful neuropathy in patients with diabetes mellitus – A randomized controlled trial [33] | Journal of the American Medical Association | 981 | 1998 | 46.7 | RCT | Type 1 and type 2 | Gabapentin | SF-36 |
| Bariatric surgery versus intensive medical therapy for diabetes – 3-year outcomes [34] | New England Journal of Medicine | 798 | 2014 | 159.6 | RCT | Type 2 | Bariatric Surgery, Intensive Medical Therapy | RAND-36 |
| Does increased access to primary care reduce hospital readmissions? | New England Journal of Medicine | 504 | 1996 | 21.9 | RCT | General | Access to Primary Care | SF-36 |
| Effectiveness of the diabetes education and self-management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: Cluster randomized controlled trial [35] | British Medical Journal | 356 | 2008 | 32.4 | RCT | Type 2 | Group education programme | WHOQOL-BREF |
| Double-blind randomized trial of tramadol for the treatment of the pain of diabetic neuropathy [36] | Neurology | 351 | 1998 | 16.7 | RCT | Type 1 and type 2 | Tramadol | MOS |
| Controlled-release oxycodone relieves neuropathic pain: A randomized controlled trial in painful diabetic neuropathy [37] | Pain | 324 | 2003 | 20.3 | RCT | Type 1 and type 2 | Controlled-release oxycodone | SF-36 |
| Randomized placebo-controlled clinical trial of Lorcaserin for weight loss in Type 2 diabetes mellitus: The BLOOM-DM study [38] | Obesity | 294 | 2012 | 42.0 | RCT | Type 2 | Lorcaserin | IWQOL-LITE |
| Bariatric surgery versus intensive medical therapy for diabetes – 5-year outcomes [39] | New England Journal of Medicine | 293 | 2017 | 146.5 | RCT | Type 2 | Bariatric Surgery, Intensive Medical Therapy | RAND-36 |
| Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5-year follow-up of an open-label, single-centre, randomized controlled trial [40] | Lancet | 289 | 2015 | 72.3 | RCT | Type 2 | Bariatric-metabolic Surgery | RAND-36 |
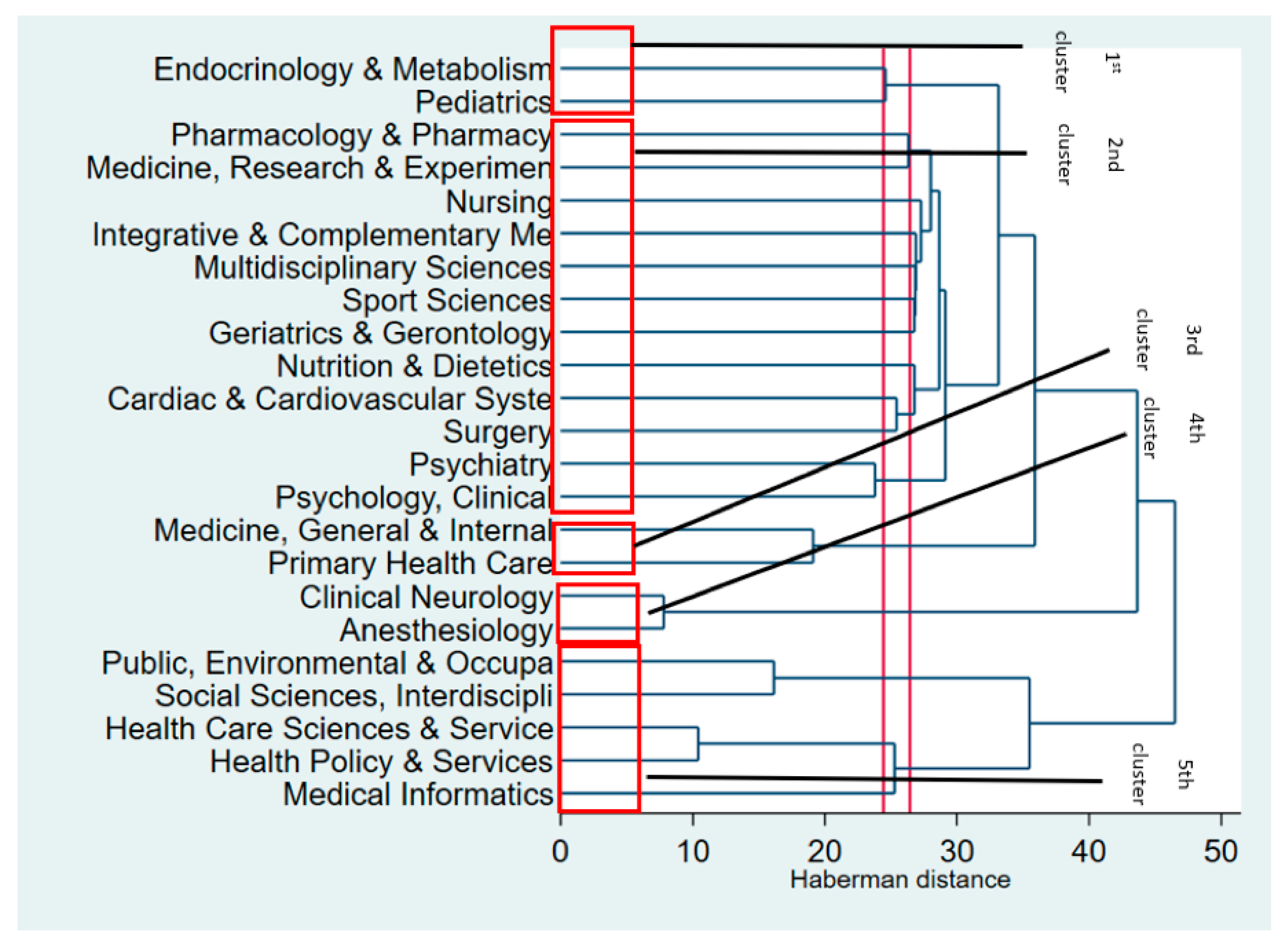
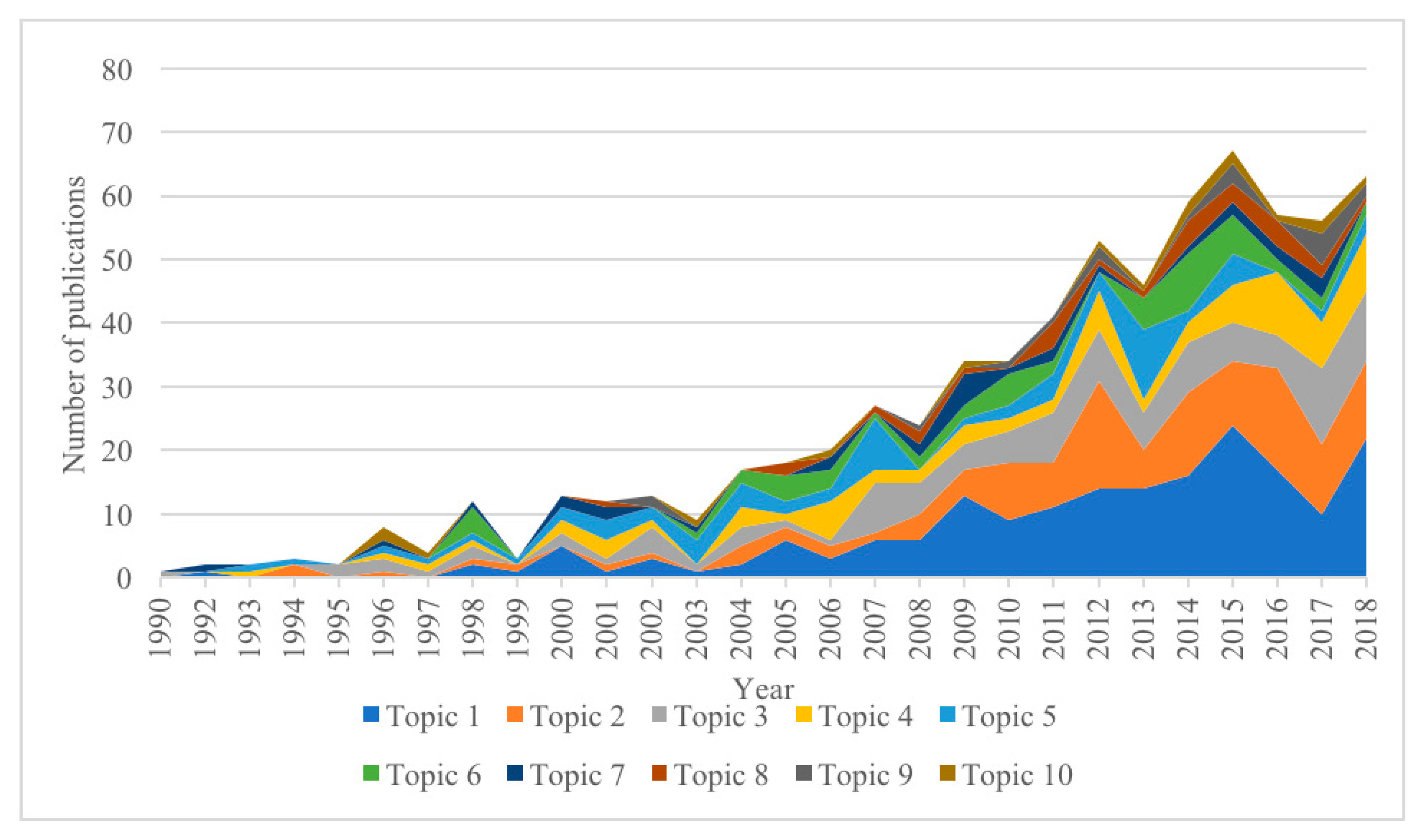
| Rank | Research Topics | n | Percent |
|---|---|---|---|
| Topic 1 | Community-, family-, and telehealth-based interventions to improve self-management and self-efficacy | 187 | 26.7% |
| Topic 2 | Lifestyle (e.g., physical activity and dietary) interventions in people with diabetes | 124 | 17.7% |
| Topic 3 | Interventions address comorbidities in people with diabetes | 107 | 15.3% |
| Topic 4 | Education-based interventions on different aspects of the disease | 74 | 10.6% |
| Topic 5 | Pharmacological treatment to control blood glucose levels | 66 | 9.4% |
| Topic 6 | Pharmacological treatment for diabetic neuropathic pain | 52 | 7.4% |
| Topic 7 | Functional complication interventions | 29 | 4.1% |
| Topic 8 | Interventions addressing mental disorders in people with diabetes | 27 | 3.9% |
| Topic 9 | Surgery and dietary interventions to promote weight loss | 18 | 2.6% |
| Topic 10 | Pharmacological and surgical interventions to address cardiovascular complications | 16 | 2.3% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tran, B.X.; Nguyen, L.H.; Pham, N.M.; Vu, H.T.T.; Nguyen, H.T.; Phan, D.H.; Ha, G.H.; Pham, H.Q.; Nguyen, T.P.; Latkin, C.A.; et al. Global Mapping of Interventions to Improve Quality of Life of People with Diabetes in 1990–2018. Int. J. Environ. Res. Public Health 2020, 17, 1597. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17051597
Tran BX, Nguyen LH, Pham NM, Vu HTT, Nguyen HT, Phan DH, Ha GH, Pham HQ, Nguyen TP, Latkin CA, et al. Global Mapping of Interventions to Improve Quality of Life of People with Diabetes in 1990–2018. International Journal of Environmental Research and Public Health. 2020; 17(5):1597. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17051597
Chicago/Turabian StyleTran, Bach Xuan, Long Hoang Nguyen, Ngoc Minh Pham, Huyen Thanh Thi Vu, Hung Trong Nguyen, Duong Huong Phan, Giang Hai Ha, Hai Quang Pham, Thao Phuong Nguyen, Carl A. Latkin, and et al. 2020. "Global Mapping of Interventions to Improve Quality of Life of People with Diabetes in 1990–2018" International Journal of Environmental Research and Public Health 17, no. 5: 1597. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17051597






