Health Literacy as Communicative Action—A Qualitative Study among Persons at Risk in the Context of Predictive and Preventive Medicine
Abstract
:1. Introduction
1.1. Being at Risk
1.2. Health Literacy
1.3. The Value of Communication
1.4. Aims and Research Questions
2. Materials and Methods
2.1. Sampling and Recruiting Procedure
2.2. Data Collection
2.2.1. Narrative Interviews
2.2.2. Embodied Perceptions of Risk and Illness
2.2.3. Ethnographic Data Concerning the Research-Relationship
2.3. Data Analysis
2.3.1. Analysis of the Narratives, Body-Maps and Ethnographic Data for Each Clinical Field Using a Field-specific Coding System
2.3.2. Interpretative Analysis of the Findings of All Four Clinical Fields, By Developing a New Integrated Coding System
2.3.3. Interdisciplinary Data Validation and Cross-Check Analysis
3. Results
3.1. Database
3.2. Main Categories

3.2.1. Key Situations
Genesis
“That’s a little strange because, um … that was for me, well breast cancer has always been an issue for me.”(FBOCP06)
“Yeah, I kind of want to know what that is and why. [...] Just to have the certainty.”(ADP08)
“And it’s nothing that has uh just been there for three months, it has always been there. Well, it didn’t just appear like three months ago, it has always been there.”(PSYP10)
Time of Cognisance
“Um, and then, as really the most relevant moment was when I was at the North Cape and the big turquoise wide sea was in front of me, the people around me were all happy, there were some plants around me you can’t find anywhere else, and I just didn’t feel anything.”(PSYP01)
“I was still young and thin and thought: ‘How could that be, diabetes type two, you get that at seventy or eighty or so and if you get it before then, it’s because you’re a rather chubby person!’ I was really shocked. Because I expected everything, but not that I would become diabetic at the age of fifty or in my early fifties.”(CHDP01)
Impact
3.2.2. Risk Understanding
Definition – Describing Risk
Interpretation – Appraising Risk
Entanglements
Warning System
“That’s why I’m glad I was able to deal with my problems now. [...] And I’m just glad that this bang fortunately caused the discernment that I have to let people help me.”(PSYP07)
“That was just another piece of the puzzle for me. It was absolutely out of question. Either you want to know or you don’t. I already said before I knew for certain: Just take my breast off!”(FBOCP04)
“We have decided to downsize a little with respect to our living. Age-appropriate. That as well has to do with my dementia.”(ADP06)
3.2.3. Agency
Dealing with Information and Knowledge
Attitude and Identity
“I am a risk factor.”(ADP05)
“And then you go like: ‘Oh shit – this is like a tattoo!’ That’s gonna stay for now.”(PSYP10)
Strategies
Role of Health Care Professionals
“But on the other hand, it’s actually very important, well it happened now already, um, twice, that something important just showed up in the results .., about which my doctor didn’t talk to me.”(ADP05)
“I just don’t trust doctors anymore. Oh God, I have experienced so much that I prefer using my own head. […] Things you experience are not always that enjoyable, you know?”(FBOCP01)
“A trusted relationship with my doctor is essential to me. Now I ended up with a doctor I don’t have any connection to. And in that case… well, with her, I would rather not talk about sensitive stuff.”(CHDP03)
“Where it actually kicked in for me were my therapy sessions. […] Because of them, I was able to see things more clearly.”(PSYP10)
4. Discussion
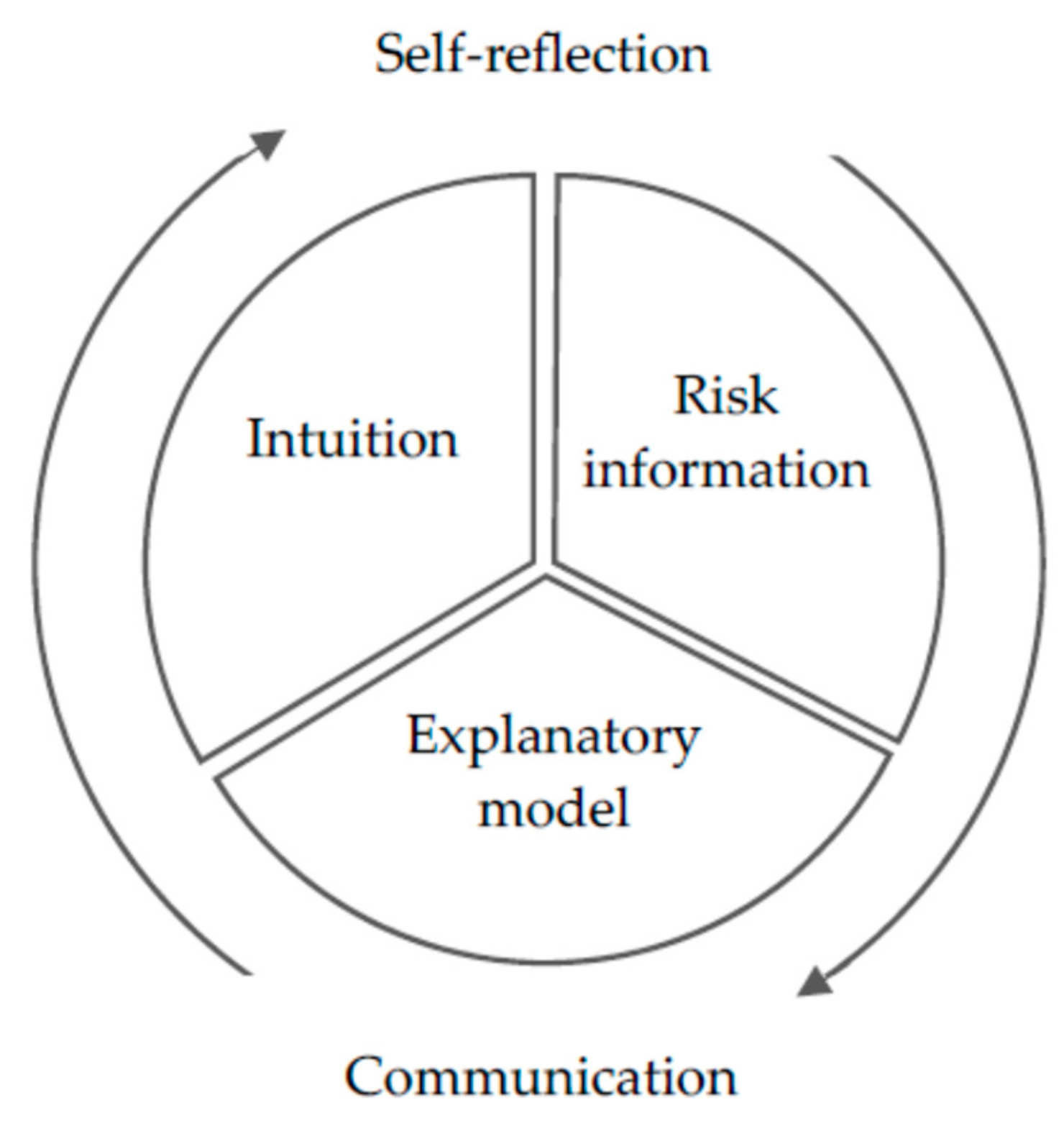
4.1. Defining HL from a Bottom-Up Perspective: Jumping the Frame of Dealing with Health Information and Opening up a Space for a More Holistic Approach
4.2. HL as Communicative Action?
4.2.1. Lifeworld and System
4.2.2. Communicative and Strategic Action
4.3. Intervention-Oriented Theory on HL as Communicative Action – Draft and First Ideas
4.3.1. Interaction as a Target
4.3.2. (Self-)Reflection as a Tool
4.3.3. Individual and Organisational HL at Once
5. Limitations and Reflection
5.1. Methods and Setting
5.2. Recruitment and Sample
5.3. Analysis
5.4. Research Environment
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Familial Breast and Ovarian Cancer: Zentrum Familiärer Brust- und Eierstockkrebs, Rita Schmutzler und Kerstin Riehm | Alzheimer’s Disease: Zentrum für Neurologie und Psychiatrie, Klinik für Psychiatrie und Psychotherapie, Frank Jessen und Ayda Rostamzadeh |
| Coronary Heart Disease: Schwerpunkt Allgemeinmedizin, August-Wilhelm Bödecker und Jörg Robertz | Psychosis: Früherkennungs-und Therapiezentrum für psychische Krisen, Klinik und Poliklinik für Psychiatrie und Psychotherapie, Theresa Haidl und Mauro Seves |
Appendix B
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Coronary Heart Disease | |
| Adults (a) with an increased risk of developing coronary heart disease (CHD) or (b) those suffering from clinically manifest CHD (according to the cardiovascular disease risk charts of the European Society of Cardiology [49]). | - Age < 35 years - Severe physical disease (except CHD and diabetes mellitus) - Mental illness (e.g., dementia, substance dependence, psychosis) |
| (a) adults without known CHD | |
| Age: women > 60 years; men > 50 years | |
| Hypertension (blood pressure > 140/95 mmHg) and/or total cholesterol > 200 mg/dl and/or smoking and/or diabetes mellitus | |
| (b) adults with known CHD | |
| Women and men with known KHK, smoking and/or blood pressure > 140/95 mmHg and/or LDL cholesterol > 100 mg/dl and/or diabetes with HbA1c > 7.5%. | |
| Written declaration of consent | |
| German language skills that allow the interview conduction | |
| Psychosis | |
| - Adults who fulfill the clinical high-risk criteria for psychosis (basic symptom criteria (SPI-A) and/or the ultra-high risk criteria (SIPS)) | - Age < 18 years - Increased risk based only on instruments of self-assessment - Known presence of a traumatic event - Current clinically relevant depressive episode, anxiety symptoms or suicidal tendencies |
| - Written declaration of consent | |
| - German language skills that allow the interview conduction | |
| Alzheimer’s Disease | |
| - Written declaration of consent German language skills that allow the interview conduction | - Dementia Indications of a non-AD neurodegenerative disease such as: Parkinson’s disease, Lewy’s body dementia, frontotemporal lobar degeneration, very rapid cognitive deterioration within a few weeks or months (classically indicative of a prion disease, neoplasia or metabolic disorder) or brain tumour |
| Clinical Criteria for the Diagnosis of an MCI (According to NIA-AA Criteria): Cognitive impairment (self or foreign medical history reported) Objective impairment in one or more cognitive domains Maintain daily life activities (ATLs) No dementia | |
| Clinical Criteria for the Diagnosis of an SCD (According to the Criteria of Jessen et al. 2014): Subjective and persistent (not acute) deterioration of cognitive performance compared to the original starting level Neuropsychological test battery, which is used for MCI or prodromal AD, shows a positive response within the age range, gender- and education-adjusted norm group lying findings | - Current clinically relevant depressive episode (GDS >11), other serious psychiatric disorders or suicidal tendencies - MCI, prodromal AD or dementia - impairments caused by a psychiatric* or neurological disease (excluding AD), somatic disease, medication or substance abuse can be explained * mild subsyndromal depressive symptoms or anxiety symptoms are not considered an exclusion criterion |
| Familial Breast and Ovarian Cancer | |
| - Group 1: Carrier of a BRCA1 or BRCA2 mutation | - Age < 18 years mild cognitive disorders or Alzheimer’s dementia - Current clinically relevant depressive episode, anxiety symptoms or suicidal tendencies |
| - Group 2: Carrier of a mutation in a moderate risk gene (e.g., CHEK2) | |
| - Group 3: No mutation detection in one of the known risk genes, but increased mathematical risk of disease due to own and family anamnesis | |
| - Written declaration of consent | |
| - German language skills that allow the interview conduction | |
Appendix C
| FBOC (n = 10) | PSY (n = 10) | AD (n = 10) | CHD (n = 3) | TOTAL (n = 33) | ||
|---|---|---|---|---|---|---|
| Gender | Female | 10 | 4 | 3 | 1 | 18 |
| Male | - | 6 | 7 | 2 | 15 | |
| Other | - | - | - | - | ||
| Age | 18–30 | 1 | 9 | - | - | 10 |
| 31–40 | 5 | 1 | - | - | 6 | |
| 41–50 | 3 | - | - | 1 | 4 | |
| 51–60 | - | - | 1 | 1 | 2 | |
| 61–70 | - | - | 8 | 1 | 9 | |
| ≥ 71 | - | - | 1 | - | 1 | |
| Marital Status | Not specified | - | - | 1 | 1 | 2 |
| Single | 3 | 9 | 1 | 2 | 15 | |
| Married | 6 | 1 | 5 | - | 12 | |
| Widowed | - | - | 1 | - | 1 | |
| Divorced | 1 | - | 2 | - | 3 | |
| Separated | - | - | - | - | - | |
| Living Conditions | Alone | 1 | 2 | 2 | 1 | 6 |
| Shared apartment | - | 4 | - | - | 4 | |
| With partner | 5 | 1 | 5 | 2 | 13 | |
| With relative | 1 | 2 | 2 | - | 5 | |
| With partner and relative | 3 | - | 1 | - | 4 | |
| Other | - | - | - | - | - | |
| Cultural Background | German | 7 | 7 | 9 | 3 | 26 |
| Bi-cultural | 2 | 3 | 1 | - | 6 | |
| Other | 1 | - | - | - | 1 | |
| Mother Tongue | German | 7 | 8 | 9 | 3 | 27 |
| Bi-lingual | 2 | 2 | 1 | - | 5 | |
| Other | 1 | - | - | - | 1 | |
| Education | Abitur 1 | 8 | 8 | 4 | 2 | 22 |
| Fachhochschulreife 2 | - | - | 3 | 1 | 4 | |
| Mittlere Reife 3 | 2 | 2 | 1 | - | 5 | |
| Polytechnische Oberschule 4 | - | - | - | - | - | |
| Haupt-/Volksschulabschluss5 | - | - | 2 | - | 2 | |
| No school certificate | - | - | - | - | - | |
| Other | - | - | - | - | - | |
| Employment Status | Full-time | 5 | 6 | 1 | - | 12 |
| Part-time | 4 | - | 2 | 2 | 8 | |
| In training/study | - | 3 | - | - | 3 | |
| Homemaking | - | - | - | - | - | |
| Retirement | - | - | 5 | - | 5 | |
| Jobseeker | - | - | 1 | - | 1 | |
| Unemployed | - | - | 1 | 1 | 2 | |
| Work disability | 1 | 1 | - | - | 2 |
| Clinical Field | Sex | Age | Marital Status | Living Conditions | Cultural Background | Mother Tongue | Religious? | Highest School Leaving Certificate | Branch/Profession-al Activity/Education | Employment Relationship | Long-Term Med. Treatment | Chronic Disease |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FBOCP01 | Female | 41 to 50 | Divorced | With rel. | German | German | No | Abitur 1 | Social area | Fulltime | Yes | No |
| FBOCP02 | Female | 31 to 40 | Unmarried | With partner | German | German | Yes | MR 3 | Economics | Part-time | Yes | Yes |
| FBOCP03 | Female | 31 to 40 | Married | Partner & rel. | Bi-cultural | G. & others | Yes | Abitur 1 | Social area | Part-time | No | No |
| FBOCP04 | Female | 18 to 30 | Unmarried | With partner | German | German | No | Abitur 1 | Art & culture | Disabled | No | No |
| FBOCP05 | Female | 41 to 50 | Married | Alone | Bi-cultural | G. & others | n.a. | Abitur 1 | IT | Fulltime | Yes | Yes |
| FBOCP06 | Female | 31 to 40 | Married | With partner | German | German | Yes | MR 3 | Health area | Fulltime | Yes | No |
| FBOCP07 | Female | 41 to 50 | Married | With partner | German | German | Yes | Abitur 1 | Other | Fulltime | Yes | Yes |
| FBOCP08 | Female | 51 to 60 | Married | Partner & rel. | German | German | Yes | Abitur 1 | Health area | Part-time | Yes | Yes |
| FBOCP09 | Female | 18 to 30 | Unmarried | With partner | Other | Other | Yes | Abitur 1 | Health area | Part-time | No | No |
| FBOCP10 | Female | 31 to 40 | Married | Partner & rel. | German | German | Yes | Abitur 1 | Health area | Fulltime | Yes | No |
| ADP01 | Female | 61 to 70 | Divorced | Alone | German | German | Yes | FH-Reife 2 | Health area | In pension | Yes | Yes |
| ADP02 | Female | 61 to 70 | Married | With partner | German | German | No | Abitur 1 | Social area | In pension | Yes | Yes |
| ADP03 | Male | 61 to 70 | Married | Alone | Other | Other | No | Abitur 1 | Other | In pension | Yes | Yes |
| ADP04 | Male | 61 to 70 | Married | Partner & rel. | German | German | Yes | FH-Reife 2 | Health area | Fulltime | Yes | Yes |
| ADP05 | Female | 61 to 70 | n.a. | With partner | German | German | No | MR | Admin. | Part-time | Yes | Yes |
| ADP06 | Male | 61 to 70 | Married | With partner | German | German | Yes | Abitur 1 | Science | In pension | No | Yes |
| ADP07 | Female | 61 to 70 | Widowed | With partner | German | German | Yes | HS 5 | Other | Unemployed | No | No |
| ADP08 | Female | 61 to 70 | Married | With partner | German | German | No | Abitur 1 | Admin. | Seeking work | Yes | Yes |
| ADP09 | Female | 51 to 60 | Single | With rel. | German | German | Yes | FH-Reife 2 | Social area | Part-time | Yes | No |
| ADP10 | Female | 71 or older | Divorced | With rel.tives | German | German | Yes | HS 5 | Health area | In pension | No | No |
| PSYP01 | Male | 18 to 30 | Unmarried | Alone | Bi-cultural | G. & others | No | Abitur 1 | IT | In training | Yes | Yes |
| PSYP02 | Female | 31 to 40 | Married | Partner & rel. | German | German | No | Abitur 1 | Social area | Fulltime | No | No |
| PSYP03 | Female | 18 to 30 | Unmarried | With rel. | German | German | No | Abitur 1 | Social area | In training | Yes | No |
| PSYP04 | Female | 18 to 30 | Unmarried | Shared app. | German | German | No | Abitur 1 | Social area | Fulltime | No | No |
| PSYP05 | Male | 18 to 30 | Unmarried | With partner | German | German | No | Abitur 1 | Social area | Fulltime | Yes | Yes |
| PSYP06 | Female | 18 to 30 | Unmarried | Shared app. | German | German | Yes | MR 3 | Other | Disabled | Yes | Yes |
| PSYP07 | Male | 18 to 30 | Unmarried Unmarried | With rel. | German | German | Yes | Abitur 1 | Other | Fulltime | Yes | No |
| PSYP08 | Male | 18 to 30 | Unmarried | Shared app. | German | German | No | Abitur 1 | Social area | In training | No | Yes |
| PSYP09 | Male | 18 to 30 | Unmarried | Shared app. | Bi-cultural | G. & others | Yes | Abitur 1 | Art & culture | Fulltime | Yes | Yes |
| PSYP10 | Male | 18 to 30 | Alone | Bi-cultural | German | No | MR 3 | Social area | Fulltime | No | No | |
| CHDP01 | Male | 51 to 60 | Unmarried | Alone | German | German | n.a. | Abitur 1 | Trade | Unemployed | Yes | Yes |
| CHDP02 | Female | 61 to 70 | n.a. | With partner | German | German | Yes | FH-Reife 2 | Economics | Part-time | Yes | Yes |
| CHDP03 | Male | 41 to 50 | Unmarried | With partner | German | German | Yes | Abitur 1 | Other | Part-time | No | No |
Appendix D
| Audio Material | Transcripts | Questionnaires | Body Maps | |
|---|---|---|---|---|
| FBOC | 10:00 h | 351 pages | 10 | 10 |
| AD | 09:20 h | 325 pages | 10 | 8 |
| CHD | 04:10 h | 60 pages | 3 | 3 |
| PSY | 10:20 h | 300 pages | 10 | 10 |
| Total | ~34:00 h | 1036 pages | 33 | 31 |
References
- Kickbusch, I. Health Governance: The Health Society. In Health and Modernity; Springer: New York, NY, USA, 2007; pp. 144–161. [Google Scholar] [CrossRef]
- Sørensen, K.; van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health Literacy and Public Health: A Systematic Review and Integration of Definitions and Models. BMC Public Health 2012, 80. [Google Scholar] [CrossRef] [Green Version]
- Kickbusch, I.; Pelikan, J.M.; Apfel, F.; Tsouros, A.D. Health Literacy. The solid facts. WHO Regional Office for Europe 2013. Available online: https://apps.who.int/iris/bitstream/handle/10665/128703/e96854.pdf (accessed on 10 September 2019).
- Oliveira, G.S.d.; Errea, M.; Bialek, J.; Kendall, M.C.; McCarthy, R.J. The impact of health literacy on shared decision making before elective surgery. A propensity matched case control analysis. BMC Health Serv. Res. 2018, 18, 958. [Google Scholar] [CrossRef] [PubMed]
- Muhanga, M.I.; Malungo, J.R.S. The what, why and how of health literacy: A systematic review of literature. Int. J. Health 2017, 5, 107–114. [Google Scholar] [CrossRef] [Green Version]
- Abel, T.; Sommerhalder, K. Gesundheitskompetenz/Health Literacy. Das Konzept und seine Operationalisierung. Bundesgesundheitsblatt Gesundh. Gesundh. 2015, 58, 923–929. [Google Scholar] [CrossRef] [PubMed]
- Samerski, S. Health literacy as a social practice. Social and empirical dimensions of knowledge on health and healthcare. Soc. Sci. Med. 2019, 226, 1–8. [Google Scholar] [CrossRef]
- Smith, S.K.; Dixon, A.; Trevena, L.; Nutbeam, D.; McCaffery, K.J. Exploring patient involvement in healthcare decision making across different education and functional health literacy groups. Soc. Sci. Med. 2009, 69, 1805–1812. [Google Scholar] [CrossRef]
- Altin, S.V.; Stock, S. The impact of health literacy, patient-centered communication and shared decision-making on patients’ satisfaction with care received in German primary care practices. BMC Health Serv. Res. 2016, 16, 450. [Google Scholar] [CrossRef] [Green Version]
- Joseph-Williams, N.; Williams, D.; Wood, F.; Lloyd, A.; Brain, K.; Thomas, N.; Prichard, A.; Goodland, A.; McGarrigle, H.; Sweetland, H.; et al. A descriptive model of shared decision making derived from routine implementation in clinical practice (‘Implement-SDM’): Qualitative study. Patient Educ. Couns. 2019, 102, 1774–1785. [Google Scholar] [CrossRef]
- Shen, H.-N.; Lin, C.-C.; Hoffmann, T.; Tsai, C.-Y.; Hou, W.-H.; Kuo, K.N. The relationship between health literacy and perceived shared decision making in patients with breast cancer. Patient Educ. Couns. 2019, 102, 360–366. [Google Scholar] [CrossRef]
- Hauser, K.; Koerfer, A.; Kuhr, K.; Albus, C.; Herzig, S.; Matthes, J. Outcome-Relevant Effects of Shared Decision Making. Dtsch. Ärzteblatt Int. 2015, 112, 665–671. [Google Scholar] [CrossRef] [Green Version]
- Stiggelbout, A.M.; Pieterse, A.H.; de Haes, J.C.J.M. Shared decision making. Concepts, evidence, and practice. Patient Educ. Couns. 2015, 98, 1172–1179. [Google Scholar] [CrossRef] [PubMed]
- Koch, K. Informationen über Krebsfrüherkennung. Was wollen die Patienten? Med. Klin. 2003, 98, 400–403. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, H.; Kiuchi, T. Health literacy and health communication. Biopsychosoc. Med. 2010, 4, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schaefer, C.; Bitzer, E.M.; Dierks, M.L. für den Vorstandes DNGK. Mehr Organisationale Gesundheitskompetenz in die Gesundheitsversorgung bringen! Ein Positionspapier des DNGK. Köln, 15.11.2019. Available online: https://dngk.de/gesundheitskompetenz/or-ganisationale-gesundheitskompetenz-positionspapier-2019/ (accessed on 13 December 2019).
- Chinn, D. Critical health literacy: A review and critical analysis. Soc. Sci. Med. 2011, 73, 60–67. [Google Scholar] [CrossRef]
- Nutbeam, D. Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promot. Int. 2000, 15, 259–267. [Google Scholar] [CrossRef] [Green Version]
- Sørensen, K.; Pelikan, J.M.; Röthlin, F.; Ganahl, K.; Slonska, Z.; Doyle, G.; Fullam, J.; Kondilis, B.; Agrafiotis, D.; Uiters, E.; et al. Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU). Eur. J. Public Health 2015, 25, 1053–1058. [Google Scholar] [CrossRef] [Green Version]
- Alper, J. A Proposed Framework for Integration of Quality Performance Measures for Health Literacy, Cultural Competence, and Language Access Services: Proceedings of a Workshop. Roundtable on Health Literacy; Board on Population Health and Public Health Practice; Health and Medicine Division; National Academies of Sciences, Engineering, and Medicine: Washington, DC, USA, 2018. [Google Scholar]
- Haidl, T.K.; Seves, M.; Eggers, S.; Rostamzadeh, A.; Genske, A.; Jünger, S.; Woopen, C.; Jessen, F.; Ruhrmann, S.; Vogeley, K. Health literacy in clinical high-risk individuals for psychosis: A systematic mixed-methods review. Early Interv. Psychiatry 2019, 13, 1293–1309. [Google Scholar] [CrossRef]
- Rostamzadeh, A.; Stapels, J.; Genske, A.; Haidl, T.; Jünger, S.; Seves, M.; Woopen, C.; Jessen, F. Health Literacy in Individuals at Risk for Alzheimer’s Dementia: A Systematic Review. J. Prev. Alzheimer’s Dis. 2019, 6, 1–9. [Google Scholar] [CrossRef]
- Hellstern, M.; Peltzer, S.; Genske, A.; Jünger, S.; Woopen, C.; Albus, C. Health literacy in persons at risk of and patients with coronary heart disease: A systematic review. Soc. Sci. Med. 2020, 245, 112711. [Google Scholar]
- Patton, M. Qualitative Evaluation and Research Methods; Beverly Hills: Sage, CA, USA, 1990. [Google Scholar]
- Guest, G.; Bunce, A.; Johnson, L. How Many Interviews Are Enough? Field Methods 2016, 18, 59–82. [Google Scholar] [CrossRef]
- Schütze, F. Biographieforschung und narratives Interview. Neue Prax. 1983, 13, 283–293. [Google Scholar]
- Nohl, A.-M. Interview und Dokumentarische Methode. Anleitungen für die Forschungspraxis, 5th ed.; Springer VS: Wiesbaden, Germany, 2017. [Google Scholar] [CrossRef]
- Lorke, M.; Schwegler, C.; Jünger, S. Re-claiming the power of definition—The value of reflexivity in research on mental health at risk. In Qualitative Research Methods in Mental Health: Innovative and Collaborative Approaches Borcsa; Willig, M.C., Ed.; Springer Nature: Cham, Germany, In press.
- VERBI Software. MAXQDA 2018; VERBI Software: Berlin, Germany, 2019.
- Gastaldo, D.; Rivas-Quarneti, N.; Magalhaes, L. Body-Map Storytelling as a Health Research Methodology. Blurred Lines Creating Clear Pictures. FQS 2018, 19, 1–26. [Google Scholar]
- Merleau-Ponty, M. Phänomenologie der Wahrnehmung, 6th ed.; de Gruyter: Berlin, Germany, 1966. [Google Scholar]
- Stamer, M.; Güthlin, C.; Holmberg, C.; Karbach, U.; Patzelt, C.; Meyer, T. Qualitative Studien in der Versorgungsforschung - Diskussionspapier, Teil 3. Qualität qualitativer Studien. Gesundheitswesen 2015, 77, 966–975. [Google Scholar] [CrossRef] [PubMed]
- Lincoln, Y.S.; Guba, E. Naturalistic Inquiry; Sage: London, UK, 1985. [Google Scholar]
- Breuer, F.; Muckel, P.; Dieris, B. Reflexive Grounded Theory. Eine Einführung für die Forschungspraxis, 4th ed.; Springer VS: Wiesbaden, Germany, 2019. [Google Scholar]
- Saunders, B.; Sim, J.; Kingstone, T.; Baker, S.; Waterfield, J.; Bartlam, B.; Burroughs, H.; Jinks, C. Saturation in qualitative research: Exploring its conceptualization and operationalization. Q. Quant 2018, 52, 1893–1907. [Google Scholar] [CrossRef] [PubMed]
- Strübing, J.; Hirschauer, S.; Ayaß, R.; Krähnke, U.; Scheffer, T. Gütekriterien qualitativer Sozialforschung. Ein Diskuss. Z. Für Soziologie 2018, 47, 83–100. [Google Scholar]
- Denzin, N. The Research Act in Sociology; Butterworth: London, UK, 1970. [Google Scholar]
- Park, C.L.; Folkman, S. Meaning in the Context of Stress and Coping. Rev. Gen. Psychol. 1997, 1, 115–144. [Google Scholar] [CrossRef]
- Slovic, P.; Finuncane, M.L.; Peters, E.; MacGregor, D.G. Risk as Analysis and Risk as Feelings: Some Thoughts about Affect, Reason, Risk and Rationality. Risk Anal. 2004, 24, 311–322. [Google Scholar] [CrossRef]
- Nutbeam, D. The evolving concept of health literacy. Soc. Sci. Med. 2008, 67, 2072–2078. [Google Scholar] [CrossRef]
- Kleinman, A. The Illness Narratives: Suffering, Healing, and the Human Condition; Basic Books: New York, NY, USA, 1988; p. 304. [Google Scholar]
- Greenhalgh, T.; Robb, N.; Scambler, G. Communicative and strategic action in interpreted consultations in primary health care: A Habermasian perspective. Soc. Sci. Med. 2006, 63, 1170–1187. [Google Scholar] [CrossRef]
- Papen, U. Informal, incidental and ad hoc: The information-seeking and learning strategies of health care patients. Lang. Educ. 2012, 26, 105–119. [Google Scholar] [CrossRef]
- Fairbrother, H.; Curtis, P.; Doyder, E. Making health information meaningful: Children’s health literacy practices. Ssm Popul. Health 2016, 2, 476–484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Habermas, J. Theorie des Kommunikativen Handelns; Suhrkamp: Frankfurt, Germany, 1981. [Google Scholar]
- Carel, H.; Kidd, I.J. Epistemic injustice in healthcare: A philosophical analysis. Med. Health Care Philos. 2014, 17, 529–540. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DasGupta, S.; Charon, R. Personal Illness Narratives: Using Refelctive Writing to Teach Empathy. Acad. Med. 2004, 79, 351–356. [Google Scholar] [CrossRef] [PubMed]
- Dierks, M.-L. Brustkrebs-Früherkennung: Einstellungen und Motive von Frauen zur Mammographie. In Die Kontroverse um die Brustkrebs-Früherkennung; Koppelin, F., Müller, R., Keil, A., Hauffe, U., Eds.; Huber: Bern, Switzerland, 2001; pp. 109–116. [Google Scholar]
- Piepolii, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.-T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts). Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [CrossRef]
| 1. | When using the term bottom-up approach in this article, we refer to the attempt to take the perspective of those being studied (the so-called persons at risk) without imposing specialist-driven definitions of health, risk, and HL (top-down approach). Instead of empirically testing existing pre-defined scientific concepts, we put the emphasis on health, risk and HL as understood and enacted by our interviewees. |
| 2. | The systematic review in the field of familial breast and ovarian cancer is under revision and will be published in 2020. |
| 3. | The collaborating partners were involved in the different phases of the project as follows: sampling and recruiting (clinical staff and the authors), data collection in terms of conducting interviews and taking field notes (LH, ML and SJ), data analysis for each clinical field (LH, ML and SJ), and interpretative analysis across the four clinical fields (LH, ML and SJ). |
| 4. | Before the interview, all potential study participants were provided with information concerning the aims, methods (including details on the interview procedure, possible harms and benefits, and the continuing opportunity to withdraw from study participation), the exploitation of the research results, and data protection. At the outset of the interview, all participants signed a written consent form. |
| 5. | More detailed information on strategies to minimise potential distress for participants, including a reflection on methodological and ethical issues in qualitative research on health risks, can be found in [28]. |
| 6. | An appropriate description of the body-maps would be beyond the scope of this article. To avoid an oversimplified presentation, we will therefore refrain from providing examples. The in-depth analysis of the body-maps and their role in the process of theory generation will be thematised in a separate article. |
| 7. |
| FBOC | AD | CHD | PSY | In Total | |
|---|---|---|---|---|---|
| Planned | 10 | 10 | 10 | 10 | 40 |
| Conducted | 10 | 11 | 3 | 10 | 34 |
| Included | 10 | 10 | 3 | 10 | 33 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harzheim, L.; Lorke, M.; Woopen, C.; Jünger, S. Health Literacy as Communicative Action—A Qualitative Study among Persons at Risk in the Context of Predictive and Preventive Medicine. Int. J. Environ. Res. Public Health 2020, 17, 1718. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17051718
Harzheim L, Lorke M, Woopen C, Jünger S. Health Literacy as Communicative Action—A Qualitative Study among Persons at Risk in the Context of Predictive and Preventive Medicine. International Journal of Environmental Research and Public Health. 2020; 17(5):1718. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17051718
Chicago/Turabian StyleHarzheim, Laura, Mariya Lorke, Christiane Woopen, and Saskia Jünger. 2020. "Health Literacy as Communicative Action—A Qualitative Study among Persons at Risk in the Context of Predictive and Preventive Medicine" International Journal of Environmental Research and Public Health 17, no. 5: 1718. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17051718





