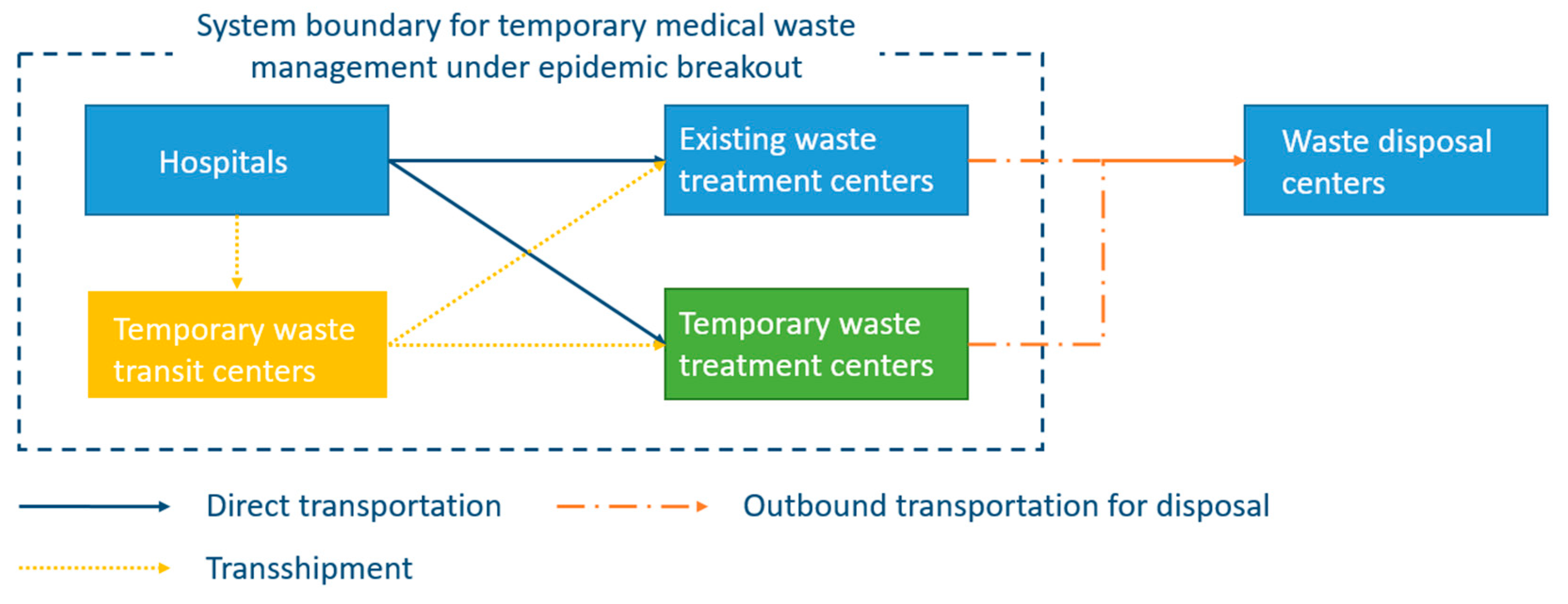
In order to show the application of the proposed mathematical model, a case study is presented in this section based on the outbreak of a novel coronavirus in China. Besides, general managerial implications are discussed from the analysis of the computational results.
4.1. Data Generation
Since December 2019, a novel coronavirus has spread rapidly across China and has resulted in a significant increase of infections within a very short period. The virus was first reported in Wuhan, which is the capital of Hubei Province and it has the highest number of infections [
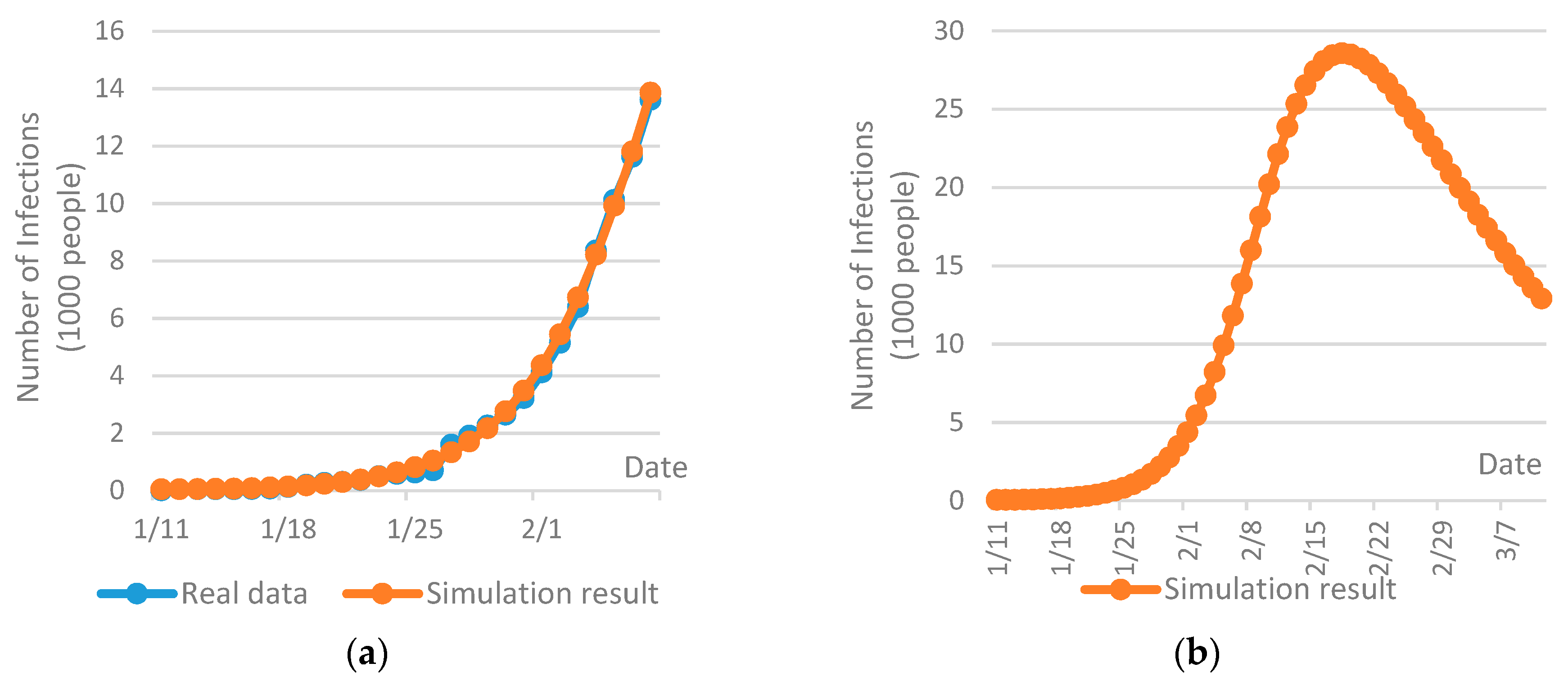
6]. At the time of the case study, the outbreak of the COVID-19 was still at the developing stage and the available knowledge and information were thus extremely limited. Based on the information published by the Health Commission of Hubei Province (web: wjw.hubei.gov.cn) and the Wuhan Municipal Health Commission (web: wjw.wuhan.gov.cn) until February 9th (19:30 h Norway time), the COVID-19 spread tendency in Wuhan was predicted with the SEIR method in AnyLogic simulation package. The SEIR method is based on a compartment theory and has been extensively used to predict epidemic spread [
68]. The SEIR method comprises of consecutive processes connecting four fundamental population groups: the susceptible population, the exposed population, the infected population, and the recovered population [
69]. The dynamics of the conversion of these four types of population is introduced by Liu et al. [
14] and Liu and Zhang [
16].
The AnyLogic simulation package is a powerful tool for the analysis of system dynamics [
70], which has been extensively used for analysis and prediction of epidemic spread [
71,
72]. In this research, a SEIR model was built up in AnyLogic. The model input was, to our best, the information collected at the time of the case study (February 9th). In addition, several assumptions were made in order to predict the future disease spread tendency in Wuhan. The initial infections were set to 41, which was the reported number until January 11th [
7]. The basic reproduction rate of the COVID-19, which depicts the average number of secondary infections caused by one patient to all susceptible population throughout the whole course of its infection [
14], was set to 2.68 in Wuhan [
6]. The incubation period of the COVID-19 was set to 7 days [
73]. The average length of stay in hospital was set to two to three weeks [
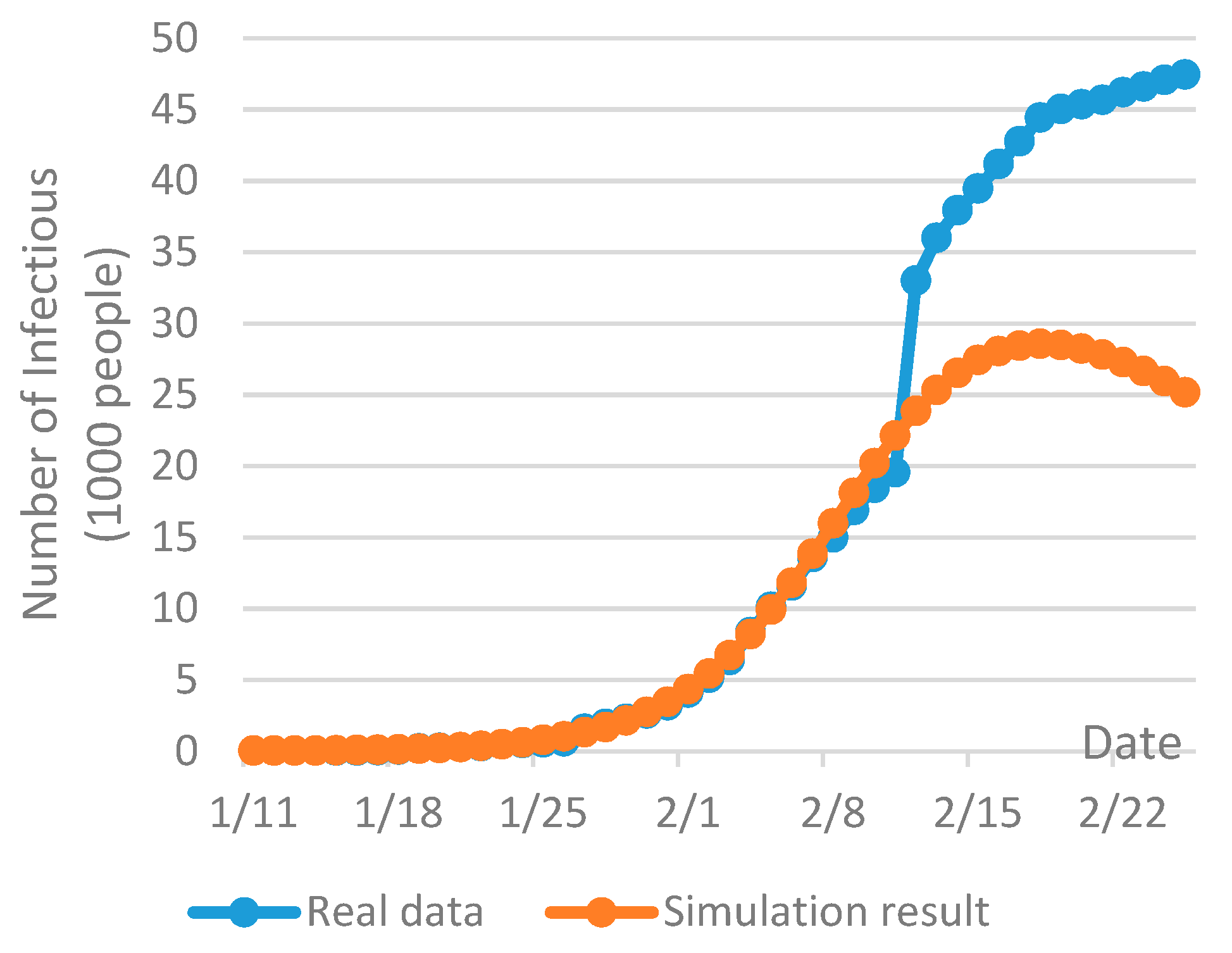
74] and the probability of contact infection was assumed to be 0.4. Taking into account the fact that Wuhan has been placed on effective lockdown since January 23th, 2020, the inbound and outbound transportation has been effectively cut off and the mobility of people within the city has been drastically restricted, so the disease may only be spread within a flexible domain of susceptible population. Due to this reason, the size of susceptible population was estimated with the best fit of the real data at the time of the case study, as shown in
Figure 2a. The repetition of the simulation was set to 20 times and the confidence level was set to be within 10%.
Figure 2b gives a prediction of the COVID-19 spread tendency in Wuhan from January 11th to March 11th, 2020, which indicates a significant increase of infections is expected at the end of February. Then, the number of infections may be reduced continuously from the beginning of March. Based on the prediction, the planning of six consecutive periods was performed with each period includes 10 days.
By February 8th, 28 hospitals had been opened for the patients infected by the COVID-19 and two temporary hospitals have been established at Huoshenshan and Leishenshan [
75]. Besides, another 11 temporary mobile cabin hospitals have been opened or planned at large public facilities, i.e., exhibition centers, sport stadiums and public schools, etc., for the treatment of mildly infections [
76]. The names and capacities of these hospitals, temporary hospitals and temporary mobile cabin hospitals are given in
Appendix A Table A1 and
Table A2. The construction of temporary hospitals and temporary mobile cabin hospitals were finished at the beginning of February, so the patients could not be allocated to them in the first two periods within the planning horizon. For the 27 hospitals opened for the COVID-19 infections, their existing capacities are estimated by the number of opened beds and their full capacities are estimated by the number of total beds. In order to allocate the patients to different hospitals, the following rules are assumed in this paper.
- (1)
In the first two periods, if the total existing capacity is not exceeded, patients are proportionally distributed to the existing 28 hospitals based on their existing capacities. Otherwise, patients are proportionally allocated based on their full capacities.
- (2)
In the other periods, if the total existing capacity is not exceeded, patients are proportionally allocated to all the 40 hospitals based on the existing capacities. Otherwise, patients are proportionally distributed based on the full capacities of these hospitals.
- (3)
If the full capacity is exceeded, the full capacity of all the hospitals are utilized. In this case, the patients who cannot get a hospital bed are assumed to be under home quarantine.
The amount of medical waste and healthcare hazards generated at different hospitals is proportional to the number of infections received and the average waste generation per bed. An early study reveals that the daily generation of medical waste in China is 0.68 kg/bed [
77]. In Wuhan, based on the total number of hospital beds, the average utilization rate and the total amount of healthcare waste generation given in the Wuhan Statistical Yearbook 2018 [
78], the daily generation of medical waste is approximately 0.6 kg/bed. However, the treatment of infectious diseases requires much more medical resources [
79], i.e., medical masks, protective glasses, and protective clothing, etc., so it leads to a higher rate of medical waste generation. Due to this reason, we assumed the daily generation rate of medical waste of the COVID-19 patients is 2.5 kg/bed. Then, the medical waste generation at different hospitals in each period was calculated by
kg.
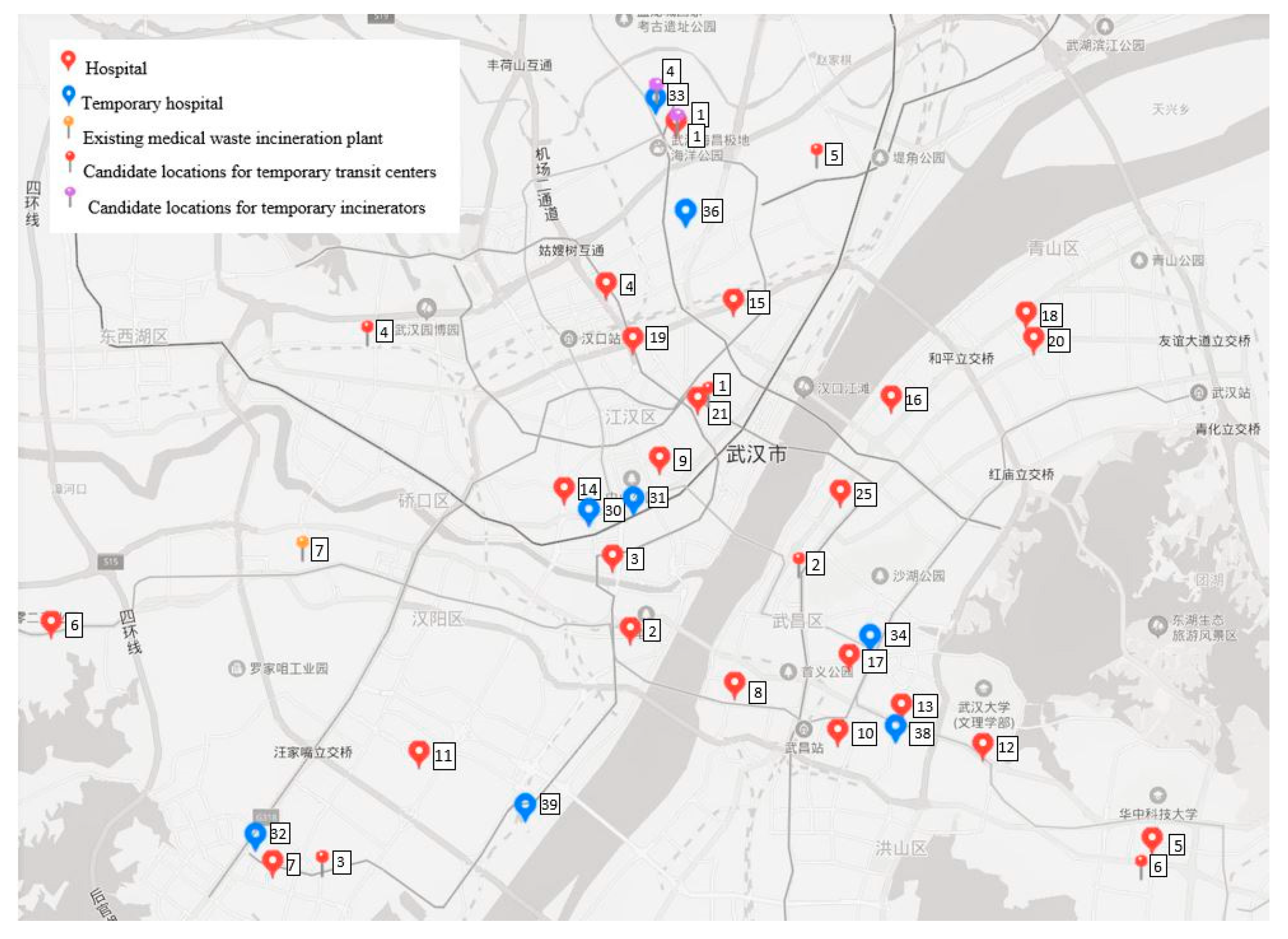
The medical waste in Wuhan is currently treated at a specialized facility located at the Guodingshan incineration plant, which has a capacity of approximately 18,000 ton/year [
80]. Apart from the ordinary medical waste, it is assumed 60% capacity of this plant can be used to deal with the highly infectious waste from the COVID-19 patients. Due to the sharp increase of medical waste generation, temporary incineration facilities have been planned and installed at several temporary healthcare centers, e.g., Jinyintan hospital, Huoshenshan hospital and Leishenshan hospital [
81]. In addition, considering the fairness to all the hospitals based on geographical distribution, we assumed another three temporary medical waste incinerators might be opened next to three temporary mobile cabin hospitals located at Wuhan Keting, China Optics Valley Convention & Exhibition Centre and Huangpi No. 1 middle school. Thus, in total, six candidate locations for establishing temporary treatment centers were selected. In order to better consolidate the transportation of medical waste, we assumed six existing transfer stations for municipal solid waste could be converted to processing medical waste with proper technological updates, so they were assumed the candidate locations for medical waste transit centers. The lists of the candidate locations for temporary facilities are given in
Appendix A Table A3 and
Table A4. With the help of Baidu Maps (
https://map.baidu.com/), the locations of respective nodes could be given and the distance between two nodes could be calculated.
Figure 3 shows the locations of hospitals, existing facilities, and candidate locations for temporary facilities in the city center of Wuhan.
In accordance with the level of hospitals and healthcare centers, based on expert opinions, we assumed three different probabilities of accidental risk at the sources: 0.003 for the third-level Grade-A hospitals, 0.004 for the other hospitals of the COVID-19 infections, and 0.007 for the temporary hospitals and the temporary mobile cabin hospitals, respectively. The basic reproduction rate of the COVID-19 was used for the value of
[
6]. The probability of transportation risk is determined by the probability of traffic accident and is proportional to the transport distance. For infectious healthcare hazards, it can be quantified by
[
65]. The consequence was assumed to be proportional to the population exposure within 500 m bandwidth along the transportation route [
82], which was estimated by the travel distance and the demographic distribution of Wuhan. To evaluate the risk related to facility operations, in accordance with Zhao and Huang [
65], the probability of accident was assumed to be 0.0001 for transit stations and 0.0006 treatment centers. The population exposure to medical waste transit and treatment facilities was considered as the main parameter for measuring the consequence of risk event. Herein, the facility risk was estimated by
[
83], where the affected radius was set to 1 km for transit stations and 3 km for treatment centers.
Table 1,
Table 2 and
Table 3 present the relevant cost parameters and capacities of both existing and temporary facilities. The size and cost parameters for setting up the same-type temporary facilities at different locations were set to identical value and were assumed based on Wang, Huang and He [
42], Zhao and Huang [
65] and Zhao et al. [
83]. The transportation cost is proportional to the travel distance. In this case study, the unit transportation cost was set to 35 yuan/ton/km [
83]. Then, the transportation cost of infectious medical waste on each link was calculated. It is noteworthy that the installation cost of temporary facilities is a fixed and non-recurring cost, which only applies at the beginning of the planning based on the facility location decisions. However, the other types of cost are variable and depend thus on the usage of facilities or transportation links.
4.2. Result and Discussion
The optimization problems were coded and solved in Lingo 18.0 optimization solver. First, the priority levels of the objective functions were given, based on which the optimal value, the nadir value and the range of each objective function were calculated in
Table 4. For analysis purpose, we set up the satisfaction levels of the risk of treatment and transportation and the total cost to 0.5 and 0.3, respectively. Then, the multi-objective optimization problem was converted to a single objective optimization and was solved.
Table 5 provides the computational information for solving the optimization problem. The objective values and the satisfaction levels are given in
Table 6.
In the optimal solution, the medical waste collected at hospitals is directly sent to treatment centers and the transshipment via intermediate transit centers is not selected. In addition to the existing Guodingshang medical waste incineration plant, another five candidate locations are chosen to establish temporary medical waste incinerators.
Table 7 shows the facility location decisions as well as the facility usage in different periods. Furthermore, the allocation of hospitals and the facility utilization rate are given in
Table 8 and
Table 9, respectively. Compared with the current plan in Wuhan, both Huoshenshan and Leishenshan hospitals are selected to open temporary treatment centers. However, instead of Jinyingtan hospital, another two candidate locations at Wuhan Keting and Huangpi No.1 Middle School are chosen to install the temporary incinerators. Besides, the optimal solution suggests the operations of the temporary medical waste incinerator at Leishenshan hospital should be started from the second period, while the operations of the other incinerators should be started from the third period. Due to the time requirement on the construction, installation and adjustment of these temporary incinerators, the advanced planning of their usage is thus of significant importance.
For the existing Guodingshang medical waste incineration plant, we assumed it would be used in all periods within the planning horizon. However, as shown in
Table 8 and
Table 9, the utilization rate of Guodingshang medical waste incineration plant is extremely low compared with the other temporary incinerators, which means the medical waste generated at hospitals is primary distributed to temporary incinerators instead of the existing facility. The reason of this could be explained by its location. Guodingshang medical waste incineration plant is located at Hanyang district, which is an urban district and is with high population density [
78]. Therefore, as argued in a previous research [
49], the operations of a medical waste incineration plant not only have negative environmental impact but also pose a significant risk on the nearby residents. The medical waste and healthcare hazards generated in epidemic outbreak are highly infectious and dangerous, the treatment of them at a centrally located incineration plant may dramatically increase the treatment risk on population exposure and is thus minimized in the optimal solution.
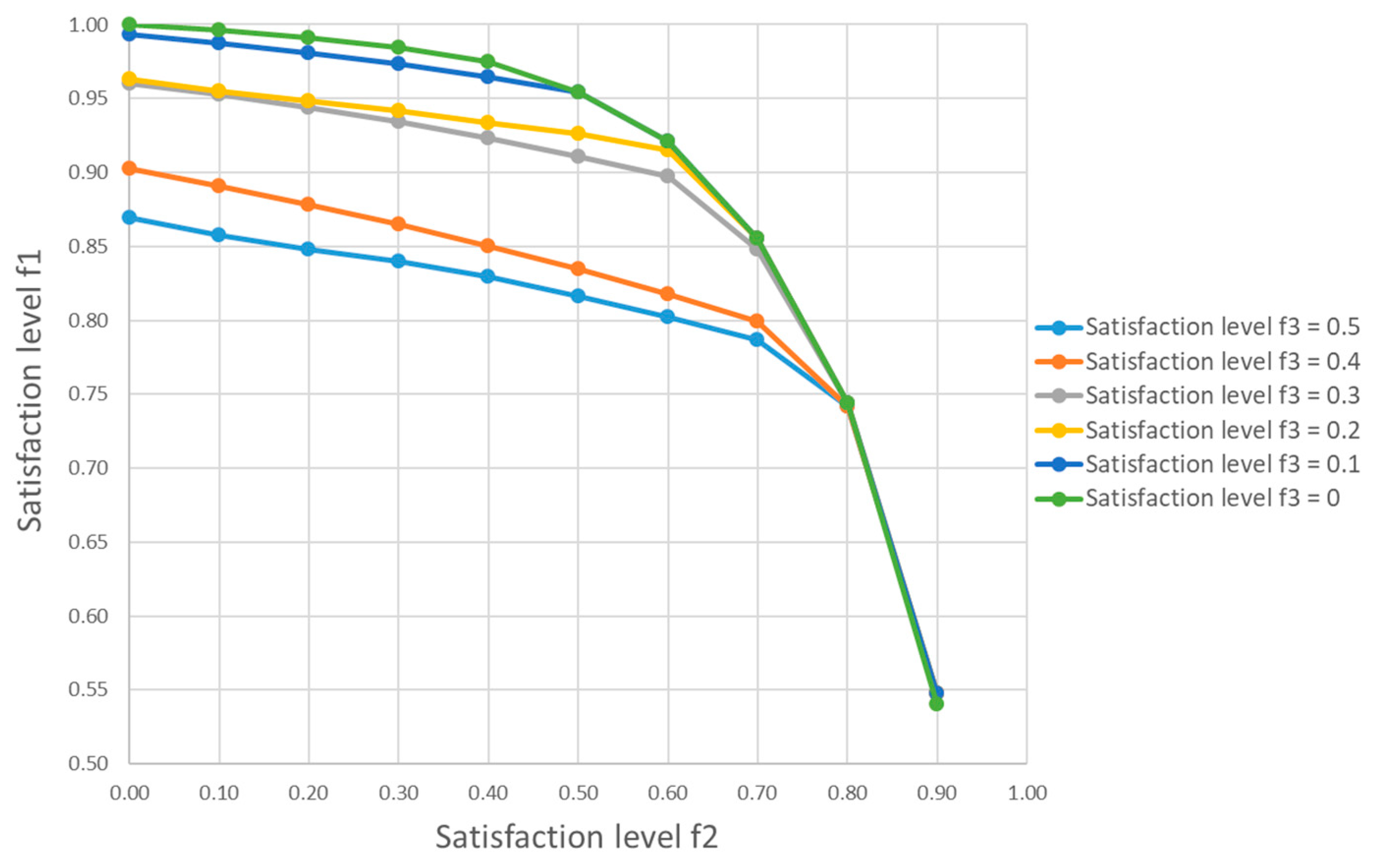
For comparison purpose, we considered another four scenarios with different combinations of the satisfaction levels
and
, as shown in
Table 10. When
increases from 0.5 to 0.7, the satisfaction level of the risk at sources is reduced by 6.6% and the treatment rate in the periods 3 to 6 decreases accordingly. On the other hand, when
decreases from 0.5 to 0.3, the optimal value of
is increased from 0.91 to 0.93 and more medical waste at the hospitals are collected and treated. Taking into account the change of satisfaction level of the cost objective, the satisfaction level
is decreased by 8.8% when
increases from 0.3 to 0.4. This reveals that, for a given satisfaction level
, a reduction on budget may lead to a higher risk at hospitals and other sources of medical waste. On the other hand, as illustrated in
Table 10, an increased investment may not lead to a significant reduction on the risk level of medical waste management.
Figure 4 gives a set of efficient Pareto optimal solutions with respect to the change of the satisfaction levels
from 0 to 0.9 and
from 0 to 0.5, respectively, which clearly shows the trade-off among these three objective functions. In general, the minimization of the risk at sources may require a compromise on the risk related to transportation and treatment of medical waste. Besides, the increase of budgetary limitation for medical waste management in epidemic outbreak may result in a better performance in risk control. However, the cost effectiveness may vary drastically in different situations. For instance, in this case study, the change of
from 0.4 to 0.3 is much more effective in the risk minimization than that of decreasing
from 0.3 to 0.2.
4.3. Policy Recommendations and Future Discussion
Even though the case study was conduced based on several assumptions and the computational result could be affected by the input from decision-makers, four policy recommendations can still be given considering the generality of the problem:
The establishment of an effective epidemic reverse logistics network with temporary facilities is of significance in dealing with the rapid increase of medical waste in epidemic outbreak.
The selection of facility locations is one of the most important decisions for both risk control and cost management of the temporary reverse logistics system.
Considering the time requirement for building, installation and adjustment of temporary facilities, advanced planning of the time of facility operation is of vital importance.
The increase of budgetary limitation may result in a better risk control, but the cost effectiveness may vary.
The outbreak of the COVID-19 is at the developing stage and the future disease spread tendency is still unclear at the time of this research and is with a high level of uncertainty. As shown in
Figure 5, the current infections of the COVID-19 on February 26th (08:30 h Norway time) in Wuhan have largely exceeded the prediction given by the SEIR model two weeks ago. The knowledge and information of the novel coronavirus are limited especially at the early phase of the outbreak in December 2019 [
84], so the reported infections at that time may be largely variated from the real infections. In addition, due to the lack of healthcare resources and the shortage of clinical beds before the completion of those temporary hospitals in early February, a large amount of suspected infections in Wuhan cannot be diagnosed and be received in hospital in a timely way [
85]. In order to provide enough clinical beds for the increased amount of the COVID-19 infections, more hospitals have been opened and more temporary mobile cabin hospitals have been planned [
86]. Meanwhile, this will lead to an increase on medical waste generation and hence the capacity for medical waste management needs to be increased accordingly.
China has suffered significantly from the outbreak of the novel coronavirus. The large mobility of people may further complicate the disease control and increase future uncertainty. In addition, it is also noteworthy that the number of the COVID-19 infections reported outside of China has been sharply increased [
10]. Research has revealed the risks of the COVID-19 outbreak in major cities around the globe [
6]. On March 3rd (11:30 h Norway time), the total number of new infections was reported at 1804, among which 1598 new infections were reported outside China [
87]. During the last one week, the rapid and significant increase on the new infections in the Republic of Korea, Italy, Japan and Iran has caused global concerns [
88].
The WHO’s risk assessment on the COVID-19 outbreak at both regional and global levels have been adjusted to the highest class [
87]. The keys to stop disease spread are the share of information and knowledge [
84], openness and transparency [
89], based on which early-stage preventive actions can be performed and rapid emergency response can be planned. As recently addressed by the Director-General of the WHO, “
with early, aggressive measures, countries can stop transmission and save lives [
88]”. Therefore, the infrastructural and resource preparedness should be done in order to effectively control a possible global outbreak of the COVID-19. Among other measures, the WHO has put focuses on providing logistics and supply chain supports for rapid response and effective control of the COVID-19 spread in many countries and areas [
87]. In this regard, the model proposed in this paper may be used, not only in Wuhan but also in other major cities exposed to the risk of the COVID-19 outbreak, for the decision-support of epidemic reverse logistics network design for effective management of increased medical waste generation.