Modeling the Research Landscapes of Artificial Intelligence Applications in Diabetes (GAPRESEARCH)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
- (a)
- Step 1: the publications related to AI in medicine and healthcare were extracted [3];
- (b)
- Step 2: among the papers in step 1, we used terms related to diabetes for identifying studies related to diabetes in AI in health and medicine.
2.2. Data Extraction
2.3. Data Analysis
2.4. Ethical Statement
3. Results
4. Discussion
4.1. Uses of AI in the Diagnosis of Diabetes
4.2. Risk Assessment of Diabetes and its Complications
4.3. Role of AI in Novel Treatments and Monitoring of Diabetes
4.4. Applications of Telehealth and Wearable Technology in the Daily Management of Diabetes
4.5. Robotic Surgery with Diabetes as a Co-Morbid
4.6. Challenges in the Use of AI
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- WHO.int. Diabetes. Available online: https://www.who.int/news-room/fact-sheets/detail/diabetes (accessed on 6 December 2019).
- Zhang, P.; Zhang, X.; Brown, J.; Vistisen, D.; Sicree, R.; Shaw, J.; Nichols, G. Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes Res. Clin. Pract. 2010, 87, 293–301. [Google Scholar] [CrossRef]
- Tran, B.X.; Vu, G.T.; Ha, G.H.; Vuong, Q.-H.; Ho, M.-T.; Vuong, T.-T.; La, V.-P.; Ho, M.-T.; Nghiem, K.-C.P.; Nguyen, H.L.T.; et al. Global Evolution of Research in Artificial Intelligence in Health and Medicine: A Bibliometric Study. J. Clin. Med. 2019, 8, 360. [Google Scholar] [CrossRef] [Green Version]
- Marateb, H.R.; Mansourian, M.; Faghihimani, E.; Amini, M.; Farina, D. A hybrid intelligent system for diagnosing microalbuminuria in Type II diabetes patients without having to measure urinary albumin. Comput. Biol. Med. 2014, 45, 34–42. [Google Scholar] [CrossRef]
- Hertroijs, D.F.L.; Elissen, A.M.J.; Brouwers, M.C.G.J.; Schaper, N.C.; Köhler, S.; Popa, M.C.; Asteriadis, S.; Hendriks, S.H.; Bilo, H.J.; Ruwaard, D. A risk score including body mass index, glycated haemoglobin and triglycerides predicts future glycaemic control in people with Type II diabetes. Diabetes Obes. Metab. 2018, 20, 681–688. [Google Scholar] [CrossRef]
- Web of Science Group. Web of Science Core Collection. Available online: https://clarivate.com/webofsciencegroup/solutions/web-of-science-core-collection/?fbclid=IwAR1YnyjGtbiE3cOizWZvlblrBhr86xZCOrbzDmFJ1pAFIDGBm5xdw5PU5qM (accessed on 25 January 2020).
- Chadegani, A.A.; Salehi, H.; Yunus, M.M.; Farhadi, H.; Fooladi, M.; Farhadi, M.; Ebrahim, N.A. A Comparison between Two Main Academic Literature Collections: Web of Science and Scopus Databases. ASS 2013, 9, 18. [Google Scholar] [CrossRef] [Green Version]
- Chen, C.; Zare, A.; Trinh, H.N.; Omotara, G.O.; Cobb, J.T.; Lagaunne, T.A. Partial Membership Latent Dirichlet Allocation for Soft Image Segmentation. IEEE Trans. Image Process. Publ. IEEE Signal Process. Soc. 2017, 26, 5590–5602. [Google Scholar] [CrossRef]
- Gross, A.; Murthy, D. Modeling virtual organizations with Latent Dirichlet Allocation: A case for natural language processing. Neural Netw. Off. J. Int. Neural Netw. Soc. 2014, 58, 38–49. [Google Scholar] [CrossRef]
- Li, Y.; Rapkin, B.; Atkinson, T.M.; Schofield, E.; Bochner, B.H. Leveraging Latent Dirichlet Allocation in processing free-text personal goals among patients undergoing bladder cancer surgery. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2019, 28, 1441–1455. [Google Scholar] [CrossRef]
- Lu, H.M.; Wei, C.P.; Hsiao, F.Y. Modeling healthcare data using multiple-channel latent Dirichlet allocation. J. Biomed. Inform. 2016, 60, 210–223. [Google Scholar] [CrossRef]
- Valle, D.; Albuquerque, P.; Zhao, Q.; Barberan, A.; Fletcher, R.J., Jr. Extending the Latent Dirichlet Allocation model to presence/absence data: A case study on North American breeding birds and biogeographical shifts expected from climate change. Glob. Chang. Biol. 2018, 24, 5560–5572. [Google Scholar] [CrossRef] [Green Version]
- Cobo, M.J.; López-Herrera, A.G.; Herrera-Viedma, E.; Herrera, F. Science mapping software tools: Review, analysis, and cooperative study among tools. J. Am. Soc. Inf. Sci. Technol. 2011, 62, 1382–1402. [Google Scholar] [CrossRef]
- Worldbank.org. Diabetes Prevalence (% of Population Ages 20 to 79) | Data. Available online: https://data.worldbank.org/indicator/SH.STA.DIAB.ZS?view=map&year_low_desc=false (accessed on 1 December 2019).
- Jong, G.-J.; Huang, C.-S.; Yu, G.-J.; Horng, G.-J. Artificial Neural Network Expert System for Integrated Heart Rate Variability. Wirel. Pers. Commun. 2014, 75, 483–509. [Google Scholar] [CrossRef]
- Liu, W.; Huang, C.; Cai, J.; Wang, X.; Zou, Z.; Sun, C. Household environmental exposures during gestation and birth outcomes: A cross-sectional study in Shanghai, China. Sci. Total Environ. 2018, 615, 1110–1118. [Google Scholar] [CrossRef]
- Ehteshami Bejnordi, B.; Veta, M.; Johannes van Diest, P.; van Ginneken, B.; Karssemeijer, N.; Litjens, G.; van der Laak, J.A.W.M.; The CAMELYON16 Consortium; Hermsen, M.; Manson, Q.F.; et al. Diagnostic Assessment of Deep Learning Algorithms for Detection of Lymph Node Metastases in Women With Breast CancerMachine Learning Detection of Breast Cancer Lymph Node MetastasesMachine Learning Detection of Breast Cancer Lymph Node Metastases. JAMA 2017, 318, 2199–2210. [Google Scholar] [CrossRef]
- McBrien, K.A.; Naugler, C.; Ivers, N.; Weaver, R.G.; Campbell, D.; Desveaux, L.; Hemmelgarn, B.R.; Edwards, A.L.; Saad, N.; Nicholas, D.; et al. Barriers to care in patients with diabetes and poor glycemic control—A cross-sectional survey. PLoS ONE 2017, 12, e0176135. [Google Scholar] [CrossRef]
- Borzouei, S.; Soltanian, A.R. Application of an artificial neural network model for diagnosing Type II diabetes mellitus and determining the relative importance of risk factors. Epidemiol. Health 2018, 40, e2018007. [Google Scholar] [CrossRef] [Green Version]
- Siegel, A.P.; Daneshkhah, A.; Hardin, D.S.; Shrestha, S.; Varahramyan, K.; Agarwal, M. Analyzing breath samples of hypoglycemic events in type 1 diabetes patients: Towards developing an alternative to diabetes alert dogs. J. Breath Res. 2017, 11, 026007. [Google Scholar] [CrossRef]
- Norouzi, S.; Kamel Ghalibaf, A.; Sistani, S.; Banazadeh, V.; Keykhaei, F.; Zareishargh, P.; Amiri, F.; Nematy, M.; Etminani, K. A Mobile Application for Managing Diabetic Patients’ Nutrition: A Food Recommender System. Arch. Iran. Med. 2018, 21, 466–472. [Google Scholar]
- Cvetkovic, B.; Janko, V.; Romero, A.E.; Kafali, O.; Stathis, K.; Lustrek, M. Activity Recognition for Diabetic Patients Using a Smartphone. J. Med. Syst. 2016, 40, 256. [Google Scholar] [CrossRef]
- Plotnikoff, R.C.; Wilczynska, M.; Cohen, K.E.; Smith, J.J.; Lubans, D.R. Integrating smartphone technology, social support and the outdoor physical environment to improve fitness among adults at risk of, or diagnosed with, Type II Diabetes: Findings from the ’eCoFit’ randomized controlled trial. Prev. Med. 2017, 105, 404–411. [Google Scholar] [CrossRef]
- Sullivan, A.N.; Lachman, M.E. Behavior Change with Fitness Technology in Sedentary Adults: A Review of the Evidence for Increasing Physical Activity. Front. Public Health 2016, 4, 289. [Google Scholar] [CrossRef] [Green Version]
- Bhat, V.; Tazari, M.; Watt, K.D.; Bhat, M. New-Onset Diabetes and Preexisting Diabetes Are Associated With Comparable Reduction in Long-Term Survival After Liver Transplant: A Machine Learning Approach. Mayo Clin. Proc. 2018, 93, 1794–1802. [Google Scholar] [CrossRef]
- Rigby, M.J. Ethical Dimensions of Using Artificial Intelligence in Health Care. AMA J. Ethics 2019, 21, 121–124. [Google Scholar] [CrossRef] [Green Version]


| Type of Data | Unit of Analysis | Analytical Methods | Presentations of Results |
|---|---|---|---|
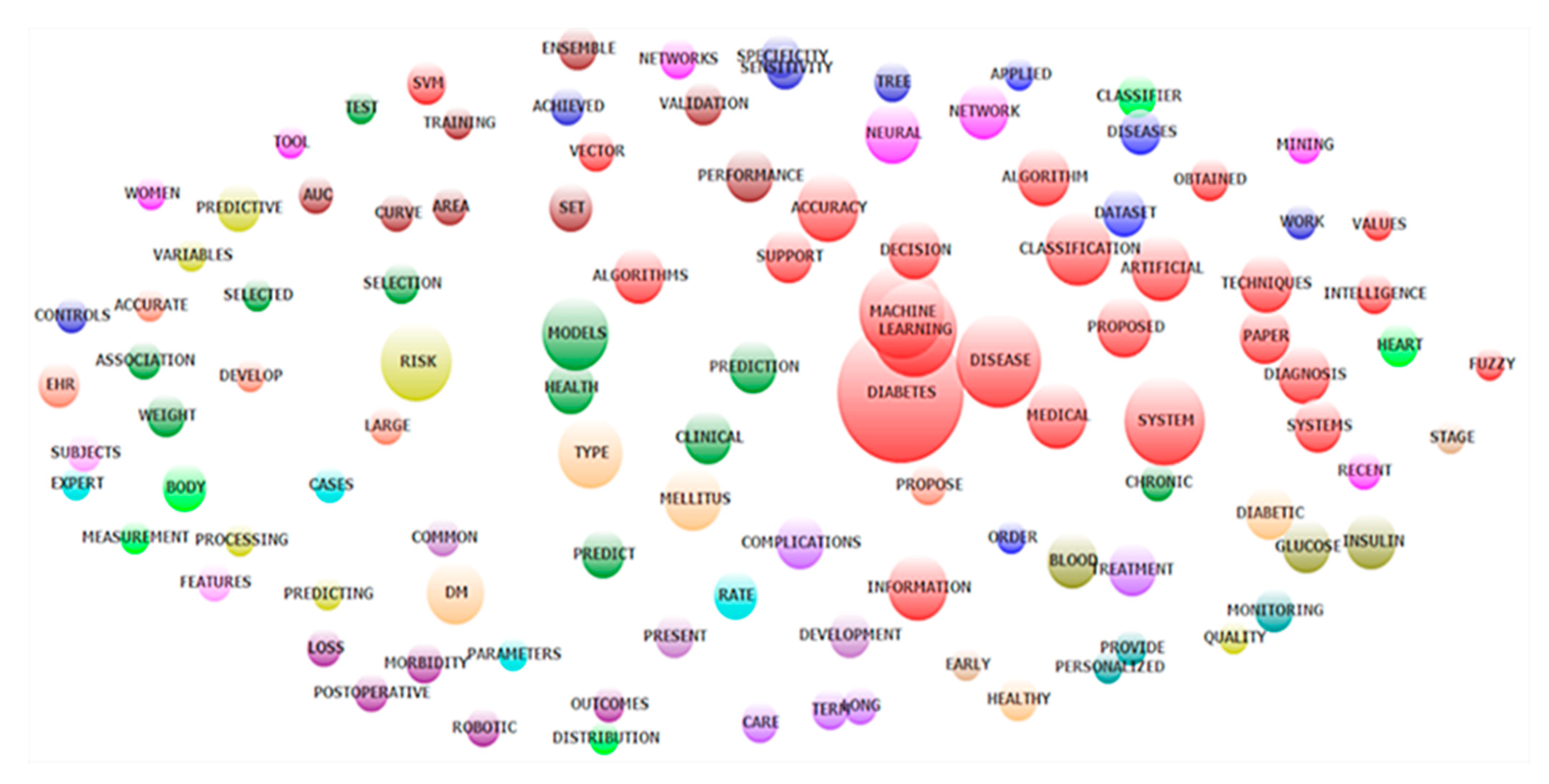
| Keywords, Countries | Words | Frequency of co-occurrence | Map of keywords clusters |
| Abstracts | Words | Exploratory factors analyses | Top 50 constructed research domains Clustering map of the landscapes constructed by these domains. |
| Abstracts | Papers | Latent Dirichlet Allocation | 10 classifications of research topics |
| WOS 1 classification of research areas | WOS research areas | Frequency of co-occurrence | Dendrogram of research disciplines |
| Year Published | Total Number of Papers | Total Citations | Mean Cite Rate per Year | Total Usage Last 6 Months 1 | Total Usage Last 5 Years 1 | Mean Use Rate Last 6 Months 2 | Mean Use Rate Last 5 Years 2 |
|---|---|---|---|---|---|---|---|
| 2018 | 74 | 60 | 0.8 | 405 | 739 | 5.5 | 2.0 |
| 2017 | 56 | 243 | 2.2 | 157 | 788 | 2.8 | 2.8 |
| 2016 | 57 | 400 | 2.3 | 61 | 656 | 1.1 | 2.3 |
| 2015 | 33 | 288 | 2.2 | 39 | 462 | 1.2 | 2.8 |
| 2014 | 22 | 196 | 1.8 | 29 | 403 | 1.3 | 3.7 |
| 2013 | 27 | 380 | 2.3 | 28 | 400 | 1.0 | 3.0 |
| 2012 | 17 | 135 | 1.1 | 9 | 117 | 0.5 | 1.4 |
| 2011 | 14 | 300 | 2.7 | 8 | 206 | 0.6 | 2.9 |
| 2010 | 12 | 343 | 3.2 | 8 | 107 | 0.7 | 1.8 |
| 2009 | 8 | 435 | 5.4 | 7 | 197 | 0.9 | 4.9 |
| 2008 | 8 | 291 | 3.3 | 8 | 75 | 1.0 | 1.9 |
| 2007 | 8 | 323 | 3.4 | 4 | 98 | 0.5 | 2.5 |
| 2006 | 8 | 213 | 2.0 | 9 | 130 | 1.1 | 3.3 |
| 2005 | 2 | 30 | 1.1 | 0 | 4 | 0.0 | 0.4 |
| 2004 | 5 | 321 | 4.3 | 3 | 56 | 0.6 | 2.2 |
| 2003 | 2 | 134 | 4.2 | 1 | 16 | 0.5 | 1.6 |
| 2002 | 5 | 177 | 2.1 | 0 | 21 | 0.0 | 0.8 |
| 2001 | 1 | 23 | 1.3 | 0 | 0 | 0.0 | 0.0 |
| 2000 | 4 | 44 | 0.6 | 0 | 10 | 0.0 | 0.5 |
| 1999 | 1 | 18 | 0.9 | 0 | 2 | 0.0 | 0.4 |
| 1998 | 2 | 48 | 1.1 | 0 | 5 | 0.0 | 0.5 |
| 1997 | 2 | 14 | 0.3 | 0 | 3 | 0.0 | 0.3 |
| 1996 | 1 | 22 | 1.0 | 0 | 4 | 0.0 | 0.8 |
| 1994 | 1 | 8 | 0.3 | 0 | 0 | 0.0 | 0.0 |
| 1993 | 1 | 2 | 0.1 | 0 | 0 | 0.0 | 0.0 |
| 1991 | 1 | 2 | 0.1 | 0 | 2 | 0.0 | 0.4 |
| No. | Country Settings | Frequency | % | No. | Country | Frequency | % |
|---|---|---|---|---|---|---|---|
| 1 | United States | 108 | 44.1% | 19 | Czech | 2 | 0.8% |
| 2 | Ireland | 25 | 10.2% | 20 | France | 2 | 0.8% |
| 3 | Italy | 15 | 6.1% | 21 | Netherlands | 2 | 0.8% |
| 4 | India | 14 | 5.7% | 22 | Singapore | 2 | 0.8% |
| 5 | Australia | 9 | 3.7% | 23 | United Arab Emirates | 2 | 0.8% |
| 6 | Japan | 8 | 3.3% | 24 | Antarctica | 1 | 0.4% |
| 7 | Taiwan | 6 | 2.4% | 25 | Brazil | 1 | 0.4% |
| 8 | Spain | 5 | 2.0% | 26 | Bulgaria | 1 | 0.4% |
| 9 | United Kingdom | 5 | 2.0% | 27 | Egypt | 1 | 0.4% |
| 10 | Germany | 4 | 1.6% | 28 | Greece | 1 | 0.4% |
| 11 | Israel | 4 | 1.6% | 29 | Jordan | 1 | 0.4% |
| 12 | Switzerland | 4 | 1.6% | 30 | Malaysia | 1 | 0.4% |
| 13 | Iran | 3 | 1.2% | 31 | Mexico | 1 | 0.4% |
| 14 | Poland | 3 | 1.2% | 32 | New Zealand | 1 | 0.4% |
| 15 | Saudi Arabia | 3 | 1.2% | 33 | Pakistan | 1 | 0.4% |
| 16 | Austria | 2 | 0.8% | 34 | Sweden | 1 | 0.4% |
| 17 | Canada | 2 | 0.8% | 35 | Tunisia | 1 | 0.4% |
| 18 | China | 2 | 0.8% | 36 | Turkey | 1 | 0.4% |
| No. | Name | Keywords | Eigenvalue | Frequency | % Cases |
| 1 | Predict; Predictors | Prediction; Predictors; Predict; Random; Models; Learning; Machine; Records | 2.89 | 173 | 74.39% |
| 2 | Events; Lead | Events; Lead; Developing; Detection; Potential; Treatment; Drug; Optimal; Medical; Work | 2.2 | 114 | 71.95% |
| 3 | UCI 1; Fuzzy | UCI; Fuzzy; Heart; Disease; Proposed; Obtained; Problems | 2.36 | 117 | 69.51% |
| 4 | Early; Rate | Early; Rate; Complications; Medical; Detection; Work | 1.88 | 89 | 65.85% |
| 5 | Technique; Cross | Technique; Cross; Applied; Validation; Machine; Metabolic; Learning | 2 | 132 | 64.63% |
| 6 | Support Vector Machine (SVM) | Vector; Support; SVM; Machine | 3.04 | 101 | 59.76% |
| 7 | Development; Present | Development; Present; Show; Conditions; Mellitus; Real | 2.33 | 75 | 58.54% |
| 8 | Classification | Classification; Predictive; Achieved | 2.1 | 57 | 54.88% |
| 9 | Monitoring; Blood Glucose | Monitoring; Glucose; Short; Insulin; Blood; Long; Treatment | 3.29 | 96 | 54.88% |
| 10 | Artificial Neural Network | Neural; Artificial; Network; Ann; Values; Parameters; DM 2; Obtained | 3.58 | 121 | 53.66% |
| 11 | Large; Physicians | Large; Physicians; Screening; Processing; Performance; Long; Set; AUC | 2.58 | 84 | 50.00% |
| 12 | Cost; Healthcare | Cost; Healthcare; Records; Predicting; Common; Risk | 2.68 | 71 | 48.78% |
| 13 | Body Mass; Index | Mass; Body; Index; Testing; Surgery; Rate; Complications; Robotic | 2.62 | 86 | 45.12% |
| 14 | Information; Develop | Information; Develop; Heart; Features; Long | 2.47 | 60 | 43.90% |
| 15 | Clinical Decision | Decision; Tree; Clinical; Major | 1.95 | 58 | 42.68% |
| 16 | Test; Neuropathy | Test; Neuropathy; Parameters; Component; Classifier; Accurate | 2.23 | 59 | 41.46% |
| 17 | Feature Selection; Features | Feature; Selection; Features; Proposed; Paper | 2.95 | 68 | 41.46% |
| 18 | Cohort; Hypertension | Cohort; Hypertension; Outcomes; Stage; Robotic; Surgery; Similar; Database; Complications | 15.05 | 73 | 41.46% |
| 19 | Area; Curve (AUC) 3 | Area; Curve; AUC; Identifying; Set; Evaluated | 3.82 | 79 | 39.02% |
| 20 | Sensitivity, Specificity | Specificity; Sensitivity; Develop | 1.85 | 42 | 26.83% |
| Year | Research areas | Frequency | % |
|---|---|---|---|
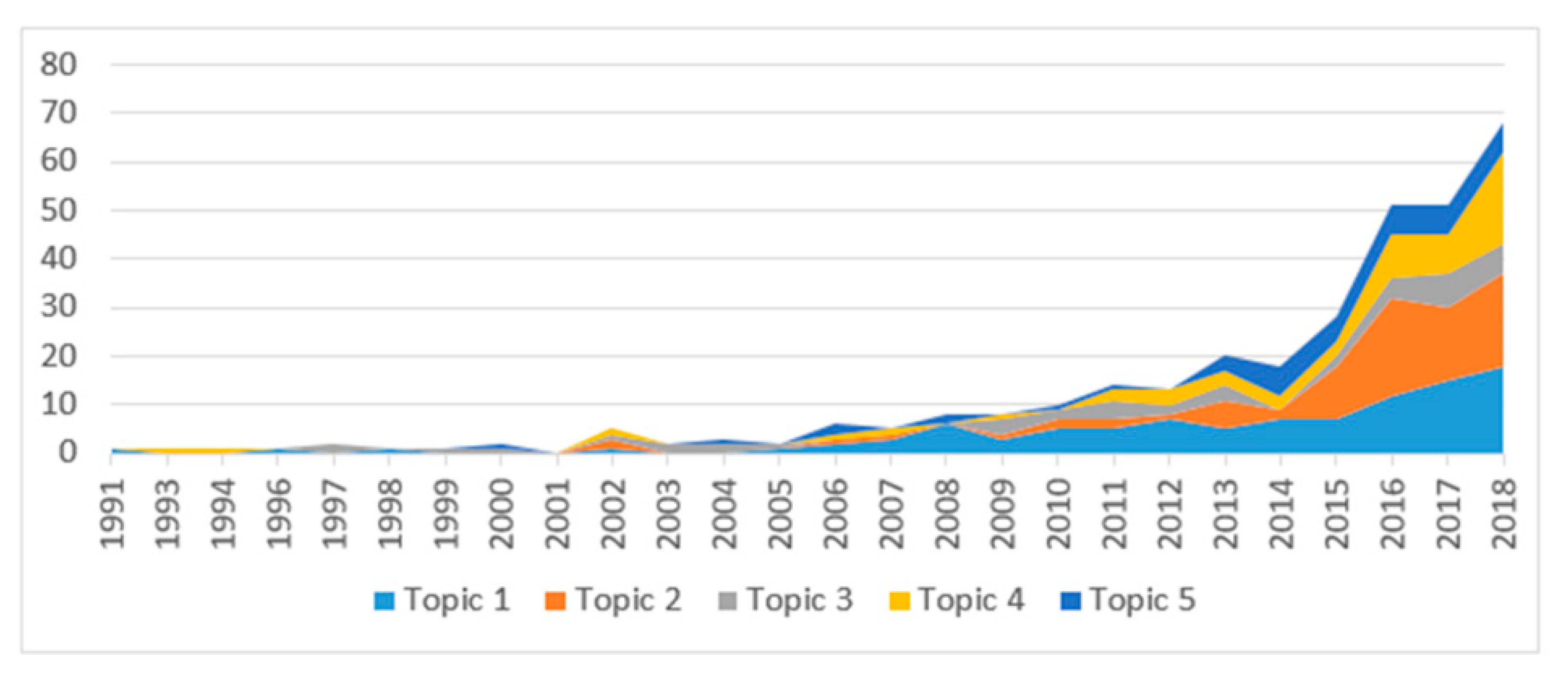
| Topic 1 | AI application in diabetes prediction and diagnosis | 100 | 31.1% |
| Topic 2 | Complications of diabetes prediction | 83 | 25.8% |
| Topic 3 | Biomedicine and molecular biology in diabetes | 43 | 13.4% |
| Topic 4 | E-health for diabetes care | 56 | 17.4% |
| Topic 5 | Robot-assisted surgery for patients with diabetes | 40 | 12.4% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vu, G.T.; Tran, B.X.; McIntyre, R.S.; Pham, H.Q.; Phan, H.T.; Ha, G.H.; Gwee, K.K.; Latkin, C.A.; Ho, R.C.M.; Ho, C.S.H. Modeling the Research Landscapes of Artificial Intelligence Applications in Diabetes (GAPRESEARCH). Int. J. Environ. Res. Public Health 2020, 17, 1982. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17061982
Vu GT, Tran BX, McIntyre RS, Pham HQ, Phan HT, Ha GH, Gwee KK, Latkin CA, Ho RCM, Ho CSH. Modeling the Research Landscapes of Artificial Intelligence Applications in Diabetes (GAPRESEARCH). International Journal of Environmental Research and Public Health. 2020; 17(6):1982. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17061982
Chicago/Turabian StyleVu, Giang Thu, Bach Xuan Tran, Roger S. McIntyre, Hai Quang Pham, Hai Thanh Phan, Giang Hai Ha, Kenneth K. Gwee, Carl A. Latkin, Roger C.M. Ho, and Cyrus S.H. Ho. 2020. "Modeling the Research Landscapes of Artificial Intelligence Applications in Diabetes (GAPRESEARCH)" International Journal of Environmental Research and Public Health 17, no. 6: 1982. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17061982






