Water Management for Construction: Evidence for Risk Characterization in Community and Healthcare Settings: A Systematic Review
Abstract
:1. Introduction
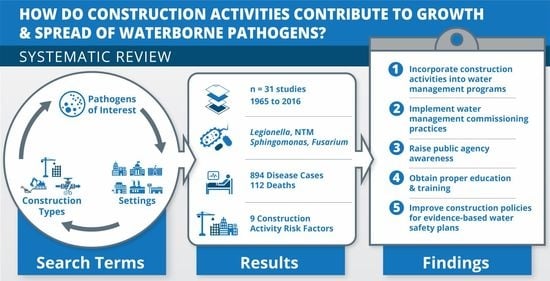
2. Materials and Methods
2.1. Review Process
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
2.4. Assessing Risk of Bias
2.5. Determining Risk Severity Using Confidence in the Body of Evidence
3. Results
3.1. Demographic Characteristics
3.2. Environmental Characteristics
3.2.1. Geographic Location
3.2.2. Seasonality and Weather Conditions
3.2.3. Building Types
3.2.4. Construction Types
3.2.5. Water Reservoirs
3.3. Construction Activity Risk Factors and Severity
Risk Severity
4. Discussion
4.1. Gap #1: Historical Significance of Construction Activities Impacting Waterborne Pathogens
4.2. Gap #2: Updating Water Management Standards with Construction Activity Risk Factors
4.3. Gap #3: Establish Water Management for Construction & Commissioning Plans
4.4. Gap #4: Moving Beyond Legionella
4.5. Gap #5 Education & Training Building Design and Construction Industries
4.6. Study Limitations
5. Conclusions
- (1)
- building owners maintain a water management program inclusive of developing a water management for construction (WMC) plan before construction activities begin;
- (2)
- building owners take responsibility to assure a proper building water management commissioning plan is implemented prior to occupancy of any building (e.g., newly constructed, renovated, unoccupied and re-opened, change of use or occupancy and building acquisition) with an emphasis on healthcare settings for acute patient care services;
- (3)
- public health agencies monitor cooling tower chemical treatment parameters in community settings, which can become overburdened with airborne soil and sediment from nearby construction activities;
- (4)
- building owners, public health officials, facility managers, facility construction managers, infectious disease physicians, infection prevention specialists and design and construction professionals obtain proper training, education and awareness of construction activity risk factors as described in the present study;
- (5)
- facility construction managers, architects, engineers and construction professionals develop and implement better evidenced-based construction policies and communication strategies to reduce the impact of the nine construction activity risk factors on building water distribution systems particularly in healthcare settings.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Gamage, S.D.; Ambrose, M.; Kralovic, S.M.; Roselle, G.A. Water safety and Legionella in health care. Infect. Dis. Clin. N. Am. 2016, 30, 689–712. [Google Scholar] [CrossRef] [PubMed]
- Water Safety in Buildings; Cunliffe, D.; Bartram, J.; Briand, E.; Chartier, Y.; Colbourne, J.; Drury, D.; Lee, J.; Schaefer, B.; Surman-Lee, S. (Eds.) World Health Organization. w/Ringgold Inc.: Portland, OR, USA, 2011. [Google Scholar]
- CDC. Toolkit: Developing a Water Management Program to Reduce Legionella Growth and Spread in Buildings; National Center for Immunization and Respiratory Diseases National Center for Environmental Health/Agency for Toxic Substance and Disease Registry, Ed.; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2017; pp. 1–31.
- Garrison, L.E.; Kunz, J.M.; Cooley, L.A.; Moore, M.R.; Lucas, C.; Schrag, S.; Sarisky, J.; Whitney, C.G. Vital signs: Deficiencies in environmental control identified in outbreaks of legionnaires’ disease—North America, 2000–2014. Am. J. Transplant. 2016, 16, 3049–3058. [Google Scholar] [CrossRef] [Green Version]
- CMS. Requirement to reduce Legionella risk in healthcare facility water systems to prevent cases and outbreaks of legionnaires’ disease. In Policy and Memos to States and Regions; Centers for Medicare and Medicaid Services, Ed.; CMS.gov: Baltimore, MD, USA, 2018. [Google Scholar]
- CDC. Federal Requirement to Reduce Legionella Risk. Available online: https://www.cdc.gov/legionella/wmp/healthcare-facilities/federal-requirement.html (accessed on 1 December 2019).
- ASHRAE. ANSI/ASHRAE Standard 188 Legionellosis: Risk Management for Building Water Systems; American Society of Heating Refrigeration and Air Conditioning Engineers: Atlanta, GA, USA, 2018; pp. 1–18. [Google Scholar]
- Bartley, J.M.; Olmsted, R.N.; Haas, J. Current views of health care design and construction: Practical implications for safer, cleaner environments. AJIC Am. J. Infect. Contol 2010, 38, S1–S12. [Google Scholar] [CrossRef] [PubMed]
- McCoy, W.F.; Rosenblatt, A.A.; LeChevallier, M.W. HACCP-based programs for preventing disease and injury from premise plumbing: A building consensus. Pathogens 2015, 4, 513–528. [Google Scholar] [CrossRef] [PubMed]
- Shabnam, V.; Steve, E.H.; Irina, D. Can public health risk assessment using risk matrices be misleading? Int. J. Environ. Res. Public Health 2015, 12, 9575–9588. [Google Scholar] [CrossRef] [Green Version]
- Donoghue, A.M. The design of hazard risk assessment matrices for ranking occupational health risks and their application in mining and minerals processing. Occup. Med. 2001, 51, 118–123. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Rooney, A.A.; Boyles, A.L.; Wolfe, M.S.; Bucher, J.R.; Thayer, K.A. Systematic review and evidence integration for literature-based environmental health science assessments. Environ. Health Perspect. 2014, 122, 711–718. [Google Scholar] [CrossRef] [Green Version]
- Monforte, R.; Cayla, J.; Sala, M.; Estruch, R.; Vidal, J.; Plasencia, A.; Urbano-Marquez, A. Community outbreak of Legionnaires’ disease in Barcelona. Lancet 1989, 1, 1011. [Google Scholar] [CrossRef]
- Garrard, J. Health Sciences Literature Review Made Easy the Matrix Method, 5th ed.; Jones & Bartlett Learning, LLC: Burlington, MA, USA, 2016. [Google Scholar]
- Abbas, Z.; Nolan, L.; Landry, L.; Galanis, E.; Egan, C. Investigation of an outbreak of Legionnaires’ disease in a hospital under construction: Ontario, September–October 2002. Can. Commun. Dis. Rep. 2003, 29, 145. [Google Scholar]
- Baker, A.W.; Lewis, S.S.; Alexander, B.D.; Chen, L.F.; Wallace, R.J.; Brown-Elliott, B.A.; Isaacs, P.J.; Pickett, L.C.; Patel, C.B.; Smith, P.K.; et al. Two-phase hospital-associated outbreak of Mycobacterium abscessus: Investigation and mitigation. Clin. Infect. Dis. 2017, 64, 902. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blatt, S.P.; Parkinson, M.D.; Pace, E.; Hoffman, P.; Dolan, D.; Lauderdale, P.; Zajac, R.A.; Melcher, G.P. Nosocomial legionnaires’ disease: Aspiration as a primary mode of disease acquisition. Am. J. Med. 1993, 95, 16–22. [Google Scholar] [CrossRef]
- Boivin, S.; Lacombe, M.-C.; Lalancette, L.; Allard, A.; Bordeleau, M.; Laverdure, G. Environmental factors associated with nosocomial legionellosis after anti-tumor necrosis factor therapy: Case study. Am. J. Infect. Control 2012, 40, 470. [Google Scholar] [CrossRef] [PubMed]
- Chafin, K.N.; Watts, M.D. Legionella—every infection preventionist’s dream—or is it? Crit. Care Nurs. Q. 2011, 34, 52. [Google Scholar] [CrossRef] [PubMed]
- Demirjian, A.; Lucas, C.E.; Garrison, L.E.; Kozak-Muiznieks, N.A.; States, S.; Brown, E.W.; Wortham, J.M.; Beaudoin, A.; Casey, M.L.; Marriott, C.; et al. The importance of clinical surveillance in detecting legionnaires’ disease outbreaks: A large outbreak in a hospital with a Legionella disinfection system-Pennsylvania, 2011–2012. Clin. Infect. Dis. 2015, 60, 1596–1602. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garbe, P.L.; Davis, B.J.; Weisfeld, J.S.; Markowitz, L.; Miner, P.; Garrity, F.; Barbaree, J.M.; Reingold, A.L. Nosocomial legionnaires’ disease: Epidemiologic demonstration of cooling towers as a source. JAMA 1985, 254, 521–524. [Google Scholar] [CrossRef]
- Grove, D.I.; Lawson, P.J.; Burgess, J.S.; Moran, J.L.; O’Fathartaigh, M.S.; Winslow, W.E. An outbreak of Legionella longbeachae infection in an intensive care unit? J. Hosp. Infect. 2002, 52, 250–258. [Google Scholar] [CrossRef] [Green Version]
- Guspiel, A.; Menk, J.; Streifel, A.; Messinger, K.; Wagner, J.; Ferrieri, P.; Kline, S. Management of risks from water and ice from ice machines for the very immunocompromised host: A process improvement project prompted by an outbreak of rapidly growing mycobacteria on a pediatric hematopoietic stem cell transplant (hsct) unit. Infect. Control Hosp. Epidemiol. 2017, 38, 792–800. [Google Scholar] [CrossRef]
- Haley, C.E.; Cohen, M.L.; Halter, J.; Meyer, R.D. Nosocomial Legionnaires’ disease: A continuing common-source epidemic at Wadsworth medical center. Ann. Intern. Med. 1979, 90, 583. [Google Scholar] [CrossRef]
- Helms, C.; Massanari, R.; Zeitler, R.; Streed, S.; Gilchrist, M.; Hall, N.; Hausler, W.; Sywassink, J.; Johnson, W.; At, E. Legionnaires’ disease associated with a hospital water system: A cluster of 24 nosocomial cases. Ann. Intern. Med. 1983, 99, 172–178. [Google Scholar] [CrossRef]
- Johnson, R.C.; Deming, C.; Conlan, S.; Zellmer, C.J.; Michelin, A.V.; Lee-Lin, S.; Thomas, P.J.; Park, M.; Weingarten, R.A.; Less, J.; et al. Investigation of a cluster of Sphingomonas koreensis infections. N. Engl. J. Med. 2018, 379, 2529–2539. [Google Scholar] [CrossRef] [PubMed]
- Kandiah, S.; Yassin, M.H.; Hariri, R.; Ferrelli, J.; Fabrizio, M.; Porter, L.; Duda, S.; Stout, J. Control of Legionella contamination with monochloramine disinfection in a large urban hospital hot water system. AJIC Am. J. Infect. Control 2012, 40, e84. [Google Scholar] [CrossRef]
- Marks, J.S.; Tsai, T.F.; Martone, W.J.; Baron, R.C.; Kennicott, J.; Holtzhauer, F.J.; Baird, I.; Fay, D.; Feeley, J.C.; Mallison, G.F.; et al. Nosocomial legionnaires’ disease in Columbus, Ohio. Ann. Intern. Med. 1979, 90, 565. [Google Scholar] [CrossRef]
- Martin, R.S.; Marrie, T.J.; Haase, D.; Sumarah, R.K. An environmental study of a nosocomial outbreak of Legionellosis in a city hospital. Can. J. Public Health 1988, 79, 440. [Google Scholar]
- Mermel, L.A.; Josephson, S.L.; Giorgio, C.H.; Dempsey, J.; Parenteau, S. Association of Legionnaires’ disease with construction: Contamination of potable water? Infect. Control Hosp. Epidemiol. 1995, 16, 76. [Google Scholar] [CrossRef] [PubMed]
- Parry, M.F.; Stampleman, L.; Hutchinson, J.H.; Folta, D.; Steinberg, M.G.; Krasnogor, L.J. Waterborne Legionella bozemanii and nosocomial pneumonia in immunosuppressed patients. Ann. Intern. Med. 1985, 103, 205. [Google Scholar] [CrossRef] [PubMed]
- Prabaker, K.; Muthiah, C.; Hayden, M.K.; Weinstein, R.A.; Cheerala, J.; Scorza, M.L.; Segreti, J.; Lavin, M.A.; Schmitt, B.A.; Welbel, S.F.; et al. Pseudo-outbreak of Mycobacterium gordonae following the opening of a newly constructed hospital at a Chicago Medical Center. Infect. Control Hosp. Epidemiol. 2015, 36, 198–203. [Google Scholar] [CrossRef]
- Sautour, M.; Edel-Hermann, V.; Steinberg, C.; Sixt, N.; Laurent, J.; Dalle, F.; Aho, S.; Hartemann, P.; L’ollivier, C.; Goyer, M.; et al. Fusarium species recovered from the water distribution system of a French university hospital. Int. J. Hyg. Environ. Health 2012, 215, 286–292. [Google Scholar] [CrossRef]
- Shands, K.N.; Ho, J.L.; Meyer, R.D.; Gorman, G.W. Potable water as a source of legionnaires’ disease. AJIC Am. J. Infect. Control 1985, 13, 286. [Google Scholar] [CrossRef]
- Srivastava, S.; Colville, A.; Odgers, M.; Laskey, L.; Mann, T. Controlling legionella risk in a newly commissioned hospital building. J. Infect. Prev. 2011, 12, 11–16. [Google Scholar] [CrossRef]
- Stout, J.E.; Brennen, C.; Muder, R.R. Legionnaires’ disease in a newly constructed long-term care facility. J. Am. Geriatr. Soc. 2000, 48, 1589. [Google Scholar] [CrossRef] [PubMed]
- Thacker, S.B.; Bennett, J.V.; Tsai, T.F.; Fraser, D.W.; McDade, J.E.; Shepard, C.C.; Williams, K.H.; Stuart, W.H.; Dull, H.B.; Eickhoff, T.C. An outbreak in 1965 of severe respiratory illness caused by the Legionnaires’ disease bacterium. J. Infect. Dis. 1978, 138, 512. [Google Scholar] [CrossRef] [PubMed]
- Francois Watkins, L.K.; Toews, K.-A.E.; Harris, A.M.; Davidson, S.; Ayers-Millsap, S.; Lucas, C.E.; Hubbard, B.C.; Kozak-Muiznieks, N.A.; Khan, E.; Kutty, P.K. Lessons from an outbreak of Legionnaires’ disease on a hematology-oncology unit. Infect. Control Hosp. Epidemiol. 2017, 38, 306–313. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castilla, J.; Barricarte, A.; Aldaz, J.; GarcÍA Cenoz, M.; Ferrer, T.; Pelaz, C.; Pineda, S.; BaladrÓN, B.; MartÍN, I.; GoÑI, B.; et al. A large Legionnaires’ disease outbreak in Pamplona, Spain: Early detection, rapid control and no case fatality. Epidemiol. Infect. 2008, 136, 823–832. [Google Scholar] [CrossRef]
- Caylà, J.A.; Sala, M.R.; Plasencia, A.; Beneyto, V.; Sureda, V.; Llorens, M.; Batalla, J. A community outbreak of Legionnaires’ disease in Barcelona: Epidemiologic and environmental study. Med. Clín. 1989, 93, 526. [Google Scholar]
- Coscollá, M.; Fenollar, J.; Escribano, I.; González-Candelas, F. Legionellosis outbreak associated with asphalt paving machine, Spain, 2009. Emerg. Infect. Dis. 2010, 16, 1381. [Google Scholar] [CrossRef] [Green Version]
- Knox, N.C.; Weedmark, K.A.; Conly, J.; Ensminger, A.W.; Hosein, F.S.; Drews, S.J. Unusual Legionnaires’ outbreak in cool, dry Western Canada: An investigation using genomic epidemiology. Epidemiol. Infect. 2017, 145, 254–265. [Google Scholar] [CrossRef] [Green Version]
- Miragliotta, G.; Del Prete, R.; Sabato, R.; Cassano, A.; Carnimeo, N. Legionellosis associated with artesian well excavation. Eur. J. Epidemiol. 1992, 8, 748–749. [Google Scholar] [CrossRef]
- Morton, S.; Bartlett, C.; Bibby, L.; Hutchinson, D.; Dyer, J.; Dennis, P. Outbreak of Legionnaires’ disease from a cooling water system in a power station. Occup. Environ. Med. 1986, 43, 630–635. [Google Scholar] [CrossRef] [Green Version]
- Redd, S.C.; Lin, F.Y.C.; Fields, B.S.; Biscoe, J.; Plikaytis, B.B. A rural outbreak of Legionnaires’ disease linked to visiting a retail store. Am. J. Public Health 1990, 80, 431. [Google Scholar] [CrossRef]
- Kamalbeik, S.; Talaie, H.; Mahdavinejad, A.; Karimi, A.; Salimi, A. Multidrug-resistant Acinetobacter baumannii infection in intensive care unit patients in a hospital with building construction: Is there an association? Korean J. Anesthesiol. 2014, 66, 295. [Google Scholar] [CrossRef] [PubMed]
- Fields, B.S.; Benson, R.F.; Besser, R.E. Legionella and Legionnaires’ disease: 25 years of investigation. Clin. Microbiol. Rev. 2002, 15, 506. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murphy, K.L. Water sampling for Legionella: Managing positive results. Biol. Blood Marrow Transplant. 2014, 20, S123. [Google Scholar] [CrossRef] [Green Version]
- Cunha, B.A.; Thekkel, V.; Schoch, P.E. Community-acquired versus nosocomial Legionella pneumonia: Lessons learned from an epidemiologic investigation. AJIC Am. J. Infect. Control 2011, 39, 901–903. [Google Scholar] [CrossRef] [PubMed]
- Scott, C.; Rafferty, M.; George, M.; Smith, R.; Stratton, S. Routine implementation of water restrictions to prevent Legionnaires’ disease. In Proceedings of the APIC 36th Annual Educational Conference & International Meeting, Fort Lauderdale, FL, USA, 7 June 2009; p. E66. [Google Scholar]
- Greub, G.; Raoult, D. Microorganisms resistant to free-living amoebae. Clin. Microbiol. Rev. 2004, 17, 413–433. [Google Scholar] [CrossRef] [Green Version]
- NASEM. Management of Legionella in Water Systems; The National Academies Press: Washington, DC, USA, 2019. [Google Scholar]
- Glick, T.H.; Gregg, M.B.; Berman, B.; Mallison, G.; Rhodes, W.W.; Kassanoff, I. Pontiac fever. An epidemic of unknown etiology in a health department: I. Clinical and epidemiologic aspects. Am. J. Epidemiol. 1978, 107, 149. [Google Scholar] [CrossRef]
- Falkinham, J.; Pruden, A.; Edwards, M. Opportunistic premise plumbing pathogens: Increasingly important pathogens in drinking water. Pathogens 2015, 4, 373–386. [Google Scholar] [CrossRef] [Green Version]
- AWWA. ANSI/AWWA Standard C651-14 Rev. C651-05: Disinfecting Water Mains; American Water Works Association: Denver, CO, USA, 2015; pp. 1–25. [Google Scholar] [CrossRef]
- ICC. 2018 International Plumbing Code. Chapter 6 Water Supply and Distribution; International Code Council, Inc.: Club Hills, IL, USA, 2017; pp. 41–58. [Google Scholar]
- Kunz, J.; Cooley, L. Preventing Legionnaires’ disease: Environmental health expertise is key. J. Environ. Health 2016, 79, 24–26. [Google Scholar]
- Rhoads, W.J.; Pruden, A.; Edwards, M.A. Survey of green building water systems reveals elevated water age and water quality concerns. Environ. Sci. Water Res. Technol. 2016, 2, 164–173. [Google Scholar] [CrossRef] [Green Version]
- Walsman, M.; Verma, R.; Muthulingam, S. The impact of LEED certification on hotel performance [Electronic article]. Cornell Hospitality Report 2014, 14, 6–13. [Google Scholar]

| Ref. | Authors | Year Pub. | Geographic Locations Country, Region | BOE Rating | Year Event Began | Event Duration (Months) | Pathogen of Interest | Total Disease Cases | Total Deaths | Construction Risk Factor(s) |
|---|---|---|---|---|---|---|---|---|---|---|
| Healthcare-associated | ||||||||||
| [14] | Abbas, et al. | 2003 | CAN, ON | 3 | 2002 | 2 | Legionella | 5 | 0 | Demolition, repressurization |
| [15] | Baker, et al. | 2017 | US, NC | 3 | 2013 | 29 | Mycobacterium | 116 | 26 | Commissioning at building opening, and water efficiency challenges |
| [16] | Blatt, et al. | 1993 | US, TX | 2 | 1989 | 12 | Legionella | 14 | 6 | Excavation, underground utility connections |
| [17] | Boivin, et al. | 2012 | CAN, QC | 1 | 2008 | 3 | Legionella | 2 | 0 | Excavation, vibration |
| [18] | Chafin, et al. | 2011 | US, TX | 2 | 2006 | 3 | Legionella | 10 | 0 | Water main, repressurization |
| [19] | Demirjian, et al. | 2015 | US, PA | 3 | 2011 | 24 | Legionella | 22 | 6 | Repressurization |
| [20] | Garbe, et al. | 1985 | US, RI | 3 | 1983 | 3 | Legionella | 15 | 10 | Repressurization |
| [21] | Grove, et al. | 2002 | AU, Adelaide | 3 | 2000 | 5 | Legionella | 7 | 2 | Demolition |
| [22] | Guspiel, et al. | 2017 | US, MN | 3 | 2011 | 10 | Mycobacterium | 15 | 0 | Commissioning at building opening, water efficiency challenges |
| [23] | Haley, et al. | 1979 | US, CA | 3 | 1977 | 15 | Legionella | 49 | 15 | Excavation, underground utility connections, commissioning at building opening |
| [24] | Helms, et al. | 1983 | US, IW | 3 | 1981 | 10 | Legionella | 24 | 11 | Commissioning at building opening |
| [25] | Johnson, et al. | 2018 | US, DC | 3 | 2005 | 144 | Shingomonas | 31 | 3 | Commissioning at building opening, water efficiency challenges |
| [26] | Kandiah, et al. | 2012 | US, PA | 2 | 2011 | 9 | Legionella | 0 | 0 | Repressurization |
| [27] | Marks, et al. | 1979 | US, OH | 1 | 1977 | 4 | Legionella | 9 | 0 | Excavation |
| [28] | Martin, et al. | 1988 | CAN, NS | 2 | 1984 | 2 | Legionella | 8 | 2 | Demolition, excavation |
| [29] | Mermel, et al. | 1995 | US, RI | 2 | 1992 | 3 | Legionella | 2 | 2 | Repressurization, vibration |
| [30] | Parry, et al. | 1985 | US, CT | 3 | 1983 | 5 | Legionella | 5 | 0 | Excavation, underground utility connections, demolition, repressurization |
| [31] | Prabaker, et al. | 2015 | US, IL | 3 | 2012 | 12 | Mycobacterium | 35 | 0 | Commissioning at building opening |
| [32] | Sautour, et al. | 2012 | FR, Dijon | 2 | 2009 | 9 | Fusarium | 0 | 0 | Repressurization, vibration |
| [33] | Shands, et al. | 1985 | US, CA | 3 | 1978 | 47 | Legionella | 171 | 0 | Commissioning at building opening, repressurization |
| [34] | Srivastava, et al. | 2011 | UK | 3 | 2007 | 22 | Legionella | 0 | 0 | Commissioning at building opening, water efficiency challenges |
| [35] | Stout, et al. | 2000 | US, PA | 3 | 1992 | 36 | Legionella | 6 | 3 | Commissioning at building opening, water efficiency challenges |
| [36] | Thacker, et al. | 1978 | US, DC | 3 | 1965 | 3 | Legionella | 81 | 16 | Excavation |
| [37] | Watkins, et al. | 2017 | US, AL | 3 | 2014 | 4 | Legionella | 10 | 0 | Commissioning at building opening |
| Community-acquired | ||||||||||
| [38] | Castilla, et al. | 2008 | ES, Pamplona | 3 | 2006 | 2 | Legionella | 146 | 0 | Demolition, excavation |
| [39] | Cayla, et al. | 1989 | ES, Barcelona | 3 | 1988 | 2 | Legionella | 56 | 7 | Demolition, excavation |
| [40] | Coscolla, et al. | 2010 | ES, Alcoi | 3 | 2009 | 3 | Legionella | 11 | 0 | Construction equipment w/water |
| [41] | Knox, et al. | 2017 | CAN, AB | 2 | 2012 | 2 | Legionella | 8 | 0 | Construction equipment w/water, excavation |
| [42] | Miragliotta, et al. | 1992 | IT, Apulia | 2 | 1990 | 1 | Legionella | 2 | 0 | Construction equipment w/water, excavation |
| [43] | Morton, et al. | 1986 | UK, Lancaster | 2 | 1981 | 2 | Legionella | 7 | 1 | Did not determine source |
| [44] | Redd, et al. | 1990 | US, MD | 3 | 1986 | 1 | Legionella | 27 | 2 | Excavation |
| Category | All | Community | Hospital |
|---|---|---|---|
| n = 31 | n = 7 | n = 24 | |
| Location | |||
| US | 19 | 1 | 18 |
| Other International | 6 | 4 | 2 |
| Canada | 4 | 1 | 3 |
| UK | 2 | 1 | 1 |
| Waterborne Pathogen of Interest | |||
| Legionella, pneumophila serogroup 1 | 19 | 6 | 13 |
| Legionella, other species | 2 | 0 | 2 |
| Legionella, no species listed | 5 | 1 | 4 |
| Nontubuculous Mycobacteria | 3 | 0 | 3 |
| Fusarium | 1 | 0 | 1 |
| Sphingomonas | 1 | 0 | 1 |
| Disease Cases & Deaths | |||
| Mean (cases per event) | 28.8 | 36.7 | 26.5 |
| Mean (deaths per event) | 3.6 | 1.4 | 4.3 |
| Total cases | 894 | 257 | 637 |
| Confirmed | 794 | 247 | 547 |
| Probable | 76 | 10 | 66 |
| Suspected | 24 | 0 | 24 |
| Deaths | 112 | 10 | 102 |
| Event Duration | |||
| Mean (months) | 13.8 | 1.9 | 17.3 |
| 0 to 6 months | 18 | 7 | 11 |
| >6 months to 12 months | 6 | 0 | 6 |
| >12 months to 18 months | 1 | 0 | 1 |
| >18 months to 24 months | 2 | 0 | 2 |
| >24 months | 4 | 0 | 4 |
| Category | All | Community | Hospital |
|---|---|---|---|
| n = 31 | n = 7 | n = 24 | |
| Total Population | 894 | 257 | 637 |
| Patients | 625 | 0 | 625 |
| Community residents | 248 | 248 | 0 |
| Construction workers | 13 | 9 | 4 |
| Healthcare staff | 4 | 0 | 4 |
| Visitors | 4 | 0 | 4 |
| Sex | (n = 19) | (n = 7) | (n = 11) |
| Males | 362 | 160 | 202 |
| Females | 193 | 97 | 96 |
| Age | (n = 20) | (n = 7) | (n = 13) |
| Range for low age | 10 yrs–71 yrs | 21 yrs–51 yrs | 10 yrs–71 yrs |
| Range for high age | 38 yrs–97 yrs | 38 yrs–97 yrs | 47 yrs–87 yrs |
| Age Mean | (n = 21) | (n = 7) | (n = 14) |
| 58.4 yrs | 55.3 yrs | 60.0 yrs | |
| ≥50% Population w/Underlying Disease | |||
| Yes | 15 | 1 | 14 |
| No | 3 | 2 | 1 |
| Did not report | 13 | 4 | 9 |
| ≥50% Population Smoked | |||
| Yes | 6 | 2 | 4 |
| No | 2 | 0 | 2 |
| Did not report | 23 | 5 | 18 |
| Category | All | Community | Hospital |
|---|---|---|---|
| n = 31 | n = 7 | n = 24 | |
| Building Type | |||
| Healthcare, acute care hospital | 22 | 0 | 22 |
| Open Land Development | 3 | 3 | 0 |
| Industrial | 2 | 2 | 0 |
| Healthcare, long term care | 1 | 0 | 1 |
| Healthcare, psych/behavioral | 1 | 0 | 1 |
| Medical school | 1 | 1 | 0 |
| Retail | 1 | 1 | 0 |
| Construction Type | |||
| Addition/Expansion on-site | 12 | 1 | 11 |
| Demolition only | 7 | 3 | 4 |
| New Construction off-site | 5 | 2 | 3 |
| Renovation within existing building | 3 | 0 | 3 |
| Renovation + New Construction | 3 | 0 | 3 |
| Season | |||
| Winter | 11 | 1 | 10 |
| Spring | 7 | 2 | 5 |
| Summer | 7 | 1 | 6 |
| Fall | 6 | 3 | 3 |
| Weather Impacts | |||
| Yes | 10 | 7 | 3 |
| No | 21 | 0 | 21 |
| Weather Factors | |||
| Prevailing winds | 8 | 5 | 3 |
| Temperature | 5 | 4 | 1 |
| Humidity | 3 | 3 | 0 |
| Rains/Storms | 2 | 1 | 1 |
| Building Water System Impacted | |||
| Potable water system | 15 | 0 | 15 |
| Utility (Cooling Towers) | 5 | 2 | 3 |
| Multiple systems impacted | 4 | 1 | 3 |
| Airborne with moisture source | 3 | 2 | 1 |
| Non-potable water system | 2 | 2 | 0 |
| Undetermined | 2 | 0 | 2 |
| Water Reservoir Impacted | |||
| Building water piping distribution system | 17 | 0 | 17 |
| Sink or shower fixture | 10 | 0 | 10 |
| Cooling dower | 7 | 2 | 5 |
| Dead-Leg or deadend piping condition | 4 | 0 | 4 |
| Construction equipment | 3 | 3 | 0 |
| Ice machine | 3 | 0 | 3 |
| AC Unit | 3 | 1 | 2 |
| Filtration system | 2 | 1 | 1 |
| Irrigation system | 2 | 0 | 2 |
| Recirculation pump | 2 | 0 | 2 |
| Standing water (ponding) | 1 | 0 | 1 |
| Did Not Report | 1 | 0 | 1 |
| Construction Activity Risk Factor | Frequency Mentioned | Total Disease Cases (S1) | Total Deaths (S2) | Severity Rank (S1) | Severity Rank (S2) |
|---|---|---|---|---|---|
| Commissioning @ Building Occup./Opening | 11 | 472 | 68 | 1 | 1 |
| Excavation | 12 | 407 | 48 | 2 | 2 |
| Re-pressurization (Shut-downs & Start-ups) | 9 | 230 | 18 | 3 | 5 |
| Demolition Activities | 6 | 227 | 11 | 4 | 6 |
| Efficiency Design Challenges | 5 | 168 | 32 | 5 | 3 |
| Underground Utility Connections | 3 | 68 | 21 | 6 | 4 |
| Construction Equipment Using Water | 3 | 21 | 0 | 7 | 8 |
| Water Main Challenges/Breaks | 1 | 10 | 0 | 8 | 8 |
| Vibration | 3 | 4 | 2 | 9 | 7 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scanlon, M.M.; Gordon, J.L.; McCoy, W.F.; Cain, M.F. Water Management for Construction: Evidence for Risk Characterization in Community and Healthcare Settings: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 2168. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17062168
Scanlon MM, Gordon JL, McCoy WF, Cain MF. Water Management for Construction: Evidence for Risk Characterization in Community and Healthcare Settings: A Systematic Review. International Journal of Environmental Research and Public Health. 2020; 17(6):2168. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17062168
Chicago/Turabian StyleScanlon, Molly M., James L. Gordon, William F. McCoy, and Melissa F. Cain. 2020. "Water Management for Construction: Evidence for Risk Characterization in Community and Healthcare Settings: A Systematic Review" International Journal of Environmental Research and Public Health 17, no. 6: 2168. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17062168