The Antecedents of Poor Doctor-Patient Relationship in Mobile Consultation: A Perspective from Computer-Mediated Communication
Abstract
:1. Introduction
2. Theoretical Background
2.1. Features of Computer-Mediated Communication
2.2. A Computer-Mediated Communication Perspective on Poor DPR
3. Research Method
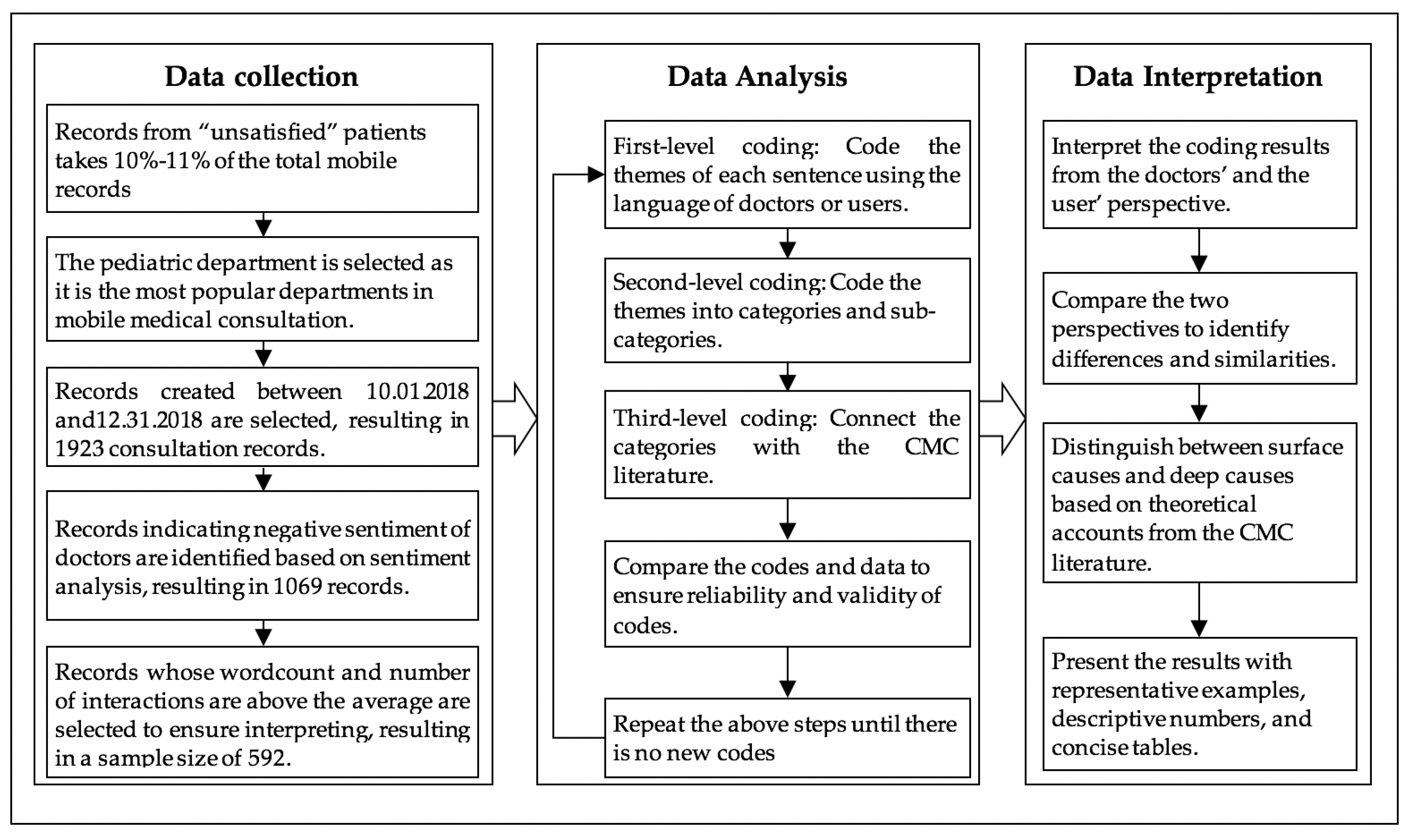
3.1. Data Collection
3.2. Data Analysis
4. Findings
4.1. The Users’ Perspective
4.1.1. Barriers for Doctors in Information Providing
4.1.2. Barriers for Doctors in Information Interpreting
4.1.3. Barriers for Doctors in Relationship Maintaining
4.2. The Doctors’ Perspective
4.2.1. Barriers for Users in Information Providing
4.2.2. Barriers for Users in Information Interpreting
4.2.3. Barriers for Users in Relationship maintaining
5. Discussion
5.1. Theoretical Implications
5.2. Practical Implications
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Liu, C.-F.; Tsai, Y.-C.; Jang, F.-L. Patients’ Acceptance towards a Web-Based Personal Health Record System: An Empirical Study in Taiwan. Int. J. Environ. Res. Public Health 2013, 10, 5191–5208. [Google Scholar] [CrossRef] [Green Version]
- Shaw, B.R.; Han, J.Y.; Hawkins, R.P.; James, S.; McTavish, F.; Gustafson, D.H. Doctor–patient relationship as motivation and outcome: Examining uses of an interactive cancer communication system. Int. J. Med. Inform. 2017, 76, 274–282. [Google Scholar] [CrossRef]
- Tang, Y.; Yang, Y.-T.; Shao, Y.-F. Acceptance of Online Medical Websites: An Empirical Study in China. Int J. Environ. Res. Public Health 2019, 16, 943. [Google Scholar] [CrossRef] [Green Version]
- Liang, C.; Gu, D.; Tao, F.; Jain, H.K.; Zhao, Y.; Ding, B. Influence of mechanism of patient-accessible hospital information system implementation on doctor–patient relationships: A service fairness perspective. Inf. Manag. 2017, 54, 57–72. [Google Scholar] [CrossRef]
- Zhang, X.; Guo, X.; Lai, K.H.; Yi, W. How does online interactional unfairness matter for patient–doctor relationship quality in online health consultation? The contingencies of professional seniority and disease severity. Eur. J. Inf. Syst. 2019, 28, 336–354. [Google Scholar] [CrossRef]
- iResearch. Report on the Demand of Doctors in China’s Online Medical Market. 2016. Available online: http://report.iresearch.cn/report/201609/2650.shtml (accessed on 29 September 2016).
- Hao, H.; Zhang, K. The voice of Chinese health consumers: A text mining approach to web-based physician reviews. J. Med. Internet Res. 2016, 18, 108–119. [Google Scholar] [CrossRef]
- Um, K.H.; Lau, A.K.W. Healthcare service failure: How dissatisfied patients respond to poor service quality. Int. J. Oper. Prod. Manag. 2018, 38, 1245–1270. [Google Scholar] [CrossRef]
- Zhou, M.; Zhao, L.; Campy, K.; Wang, S. Changing of China’s health policy and Doctor–Patient relationship. Health Policy Technol. 2017, 6, 358–367. [Google Scholar] [CrossRef]
- Gu, D.; Yang, X.; Li, X.; Jain, H.K.; Liang, C. Understanding the Role of Mobile Internet-Based Health Services on Patient Satisfaction and Word-of-Mouth. Int. J. Environ. Res. Public Health 2018, 15, 1972. [Google Scholar] [CrossRef] [Green Version]
- Mein Goh, J.; Gao, G.; Agarwal, R. The creation of social value: Can an online health community reduce rural–urban health disparities? MIS Q. 2016, 40, 1–22. [Google Scholar]
- Zhang, W.; Deng, Z.; Hong, Z.; Evans, R.D.; Ma, J.; Zhang, H. Unhappy Patients Are Not Alike: Content Analysis of the Negative Comments from China’s Good Doctor Website. J. Med. Internet Res. 2018, 20, 35–49. [Google Scholar] [CrossRef]
- Sewitch, M.J.; Abrahamowicz, M.; Dobkin, P.L.; Tamblyn, R. Measuring Differences Between Patients’ and Physicians’ Health Perceptions: The Patient–Physician Discordance Scale. J. Behav. Med. 2003, 26, 245–264. [Google Scholar] [CrossRef]
- Atanasova, S.; Kamin, T.; Petri, G. The benefits and challenges of online professional-patient interaction: Comparing views between users and health professional moderators in an online health community. Comput. Human Behav. 2018, 83, 106–118. [Google Scholar] [CrossRef]
- Akter, S.; D’Ambra, J.; Ray, P. Development and validation of an instrument to measure user perceived service quality of mHealth. Inf. Manag. 2013, 50, 181–195. [Google Scholar] [CrossRef] [Green Version]
- Deng, Z.; Liu, S.; Hinz, O. The health information seeking and usage behavior intention of Chinese consumers through mobile phones. Inf. Technol. People 2015, 28, 405–423. [Google Scholar] [CrossRef]
- Wu, T.; Deng, Z.; Zhang, D.; Buchanan, P.R.; Zha, D.; Wang, R. Seeking and using intention of health information from doctors in social media: The effect of doctor-consumer interaction. Int. J. Med. Inform. 2018, 105, 106–113. [Google Scholar] [CrossRef]
- Lee, S.A.; Zuercher, R.J. A current review of doctor–patient computer-mediated communication. J. Commun. Healthc. 2017, 10, 22–30. [Google Scholar] [CrossRef]
- Ang, C.S.; Talib, M.A.; Tan, K.A.; Tan, J.P.; Yaacob, S.N. Understanding computer-mediated communication attributes and life satisfaction from the perspectives of uses and gratifications and self-determination. Comput. Hum. Behav. 2015, 40, 20–29. [Google Scholar] [CrossRef]
- Lewandowski, J.; Rosenberg, B.D.; Parks, M.J.; Siegel, J.T. The effect of informal social support: Face-to-face versus computer-mediated communication. Comput. Hum. Behav. 2011, 27, 1806–1814. [Google Scholar] [CrossRef]
- Bae, M. The effects of anonymity on computer-mediated communication: The case of independent versus interdependent self-construal influence. Comput. Hum. Behav. 2016, 55, 300–309. [Google Scholar] [CrossRef]
- Rains, S.A. A meta-analysis of research on formal computer-mediated support groups: Examining group characteristics and health outcomes. Hum. Commun. Res. 2010, 35, 309–336. [Google Scholar] [CrossRef]
- Andreassen, H.K.; Trondsen, M.; Kummervold, P.E.; Gammon, D.; Hjortdahl, P. Patients who use e-mediated communication with their doctor: New constructions of trust in the patient-doctor relationship. Qual. Health Res. 2006, 16, 238–248. [Google Scholar] [CrossRef]
- Ho, S.M.; Lowry, P.B.; Warkentin, M.; Yang, Y.; Hollister, J.M. Gender deception in asynchronous online communication: A path analysis. Inf. Process. Manag. 2017, 53, 21–41. [Google Scholar] [CrossRef] [Green Version]
- Adrianson, L. Gender and computer-mediated communication: Group processes in problem solving. Comput. Hum. Behav. 2001, 17, 71–94. [Google Scholar] [CrossRef]
- Wright, K.B.; Bell, S.B. Health-related support groups on the Internet: Linking empirical findings to social support and computer-mediated communication theory. J. Health Psychol. 2003, 81, 39–54. [Google Scholar] [CrossRef]
- Borowitz, S.M.; Wyatt, J.C. The origin, content, and workload of e-mail consultations. JAMA 1998, 280, 1321–1324. [Google Scholar] [CrossRef] [Green Version]
- Colvin, J.; Chenoweth, L.; Bold, M.; Harding, C. Caregivers of older adults: Advantages and disadvantages of Internet-based social support. Fam. Relat. 2004, 53, 49–57. [Google Scholar] [CrossRef]
- Riordan, M.A.; Kreuz, R.J. Emotion encoding and interpretation in computer-mediated communication: Reasons for use. Comput. Hum. Behav. 2010, 26, 1667–1673. [Google Scholar] [CrossRef]
- Angeli, C.; Schwartz, N.H. Differences in electronic exchanges in synchronous and asynchronous computer-mediated communication: The effect of culture as a mediating variable. Interact. Learn. Environ. 2016, 24, 1109–1130. [Google Scholar] [CrossRef]
- Katz, S.J.; Moyer, C.A.; Cox, D.T.; Stern, D.T. Effect of a Triage-based E-mail System on Clinic Resource Use and Patient and Physician Satisfaction in Primary Care: A Randomized Controlled Trial. J. Gen. Intern. Med. 2003, 18, 736–744. [Google Scholar] [CrossRef] [Green Version]
- Joinson, A.N. Self-disclosure in computer-mediated communication: The role of self-awareness and visual anonymity. Eur. J. Soc. Psychol. 2001, 31, 177–192. [Google Scholar] [CrossRef]
- Patt, M.R.; Houston, T.K.; Jenckes, M.W.; Sands, D.Z.; Ford, D.E. Doctors who are using e-mail with their patients: A qualitative exploration. J. Med. Internet Res. 2003, 5, 1–23. [Google Scholar] [CrossRef]
- Tidwell, L.C.; Walther, J.B. Computer-mediated communication effects on disclosure, impressions, and interpersonal evaluations: Getting to know one another a bit at a time. Hum. Commun. Res. 2010, 28, 317–348. [Google Scholar] [CrossRef]
- Eveleigh, R.M.; Muskens, E.; van Ravesteijn, H.; van Dijk, I.; van Rijswijk, E.; Lucassen, P. An overview of 19 instruments assessing the doctor-patient relationship: Different models or concepts are used. J. Clin. Epidemiol. 2012, 65, 10–15. [Google Scholar] [CrossRef]
- Fuertes, J.N.; Anand, P.; Haggerty, G.; Kestenbaum, M.; Rosenblum, G.C. The Physician–Patient Working Alliance and Patient Psychological Attachment, Adherence, Outcome Expectations, and Satisfaction in a Sample of Rheumatology Patients. Behav. Med. 2015, 41, 60–68. [Google Scholar] [CrossRef]
- Teutsch, C. Patient-doctor communication. Med. Clin. North Am. 2003, 87, 1115–1145. [Google Scholar] [CrossRef]
- Ong, L.; De Haes, J.; Hoos, A.; Lammes, F. Doctor-patient communication: A review of the literature. Soc. Sci. Med. 1995, 40, 908–918. [Google Scholar] [CrossRef]
- Pian, W.; Song, S.; Zhang, Y. Consumer health information needs: A systematic review of measures. Inf. Process. Manag. 2020, 57, 102077. [Google Scholar] [CrossRef]
- Dennis, A.; Fuller, R.; Valacich, J. Media, tasks, and communication processes: A theory of media synchronicity. MIS Q. Manag. Inf. Syst. 2008, 32, 575–600. [Google Scholar] [CrossRef]
- Liang, B.; Scammon, D.L. E-Word-of-Mouth on health social networking sites: An opportunity for tailored health communication. J. Consum. Behav. 2011, 10, 322–331. [Google Scholar] [CrossRef]
- Motamarri, S.; Akter, S.; Ray, P.; Tseng, C.L. Distinguishing“ mHealth” from Other Healthcare Services in a Developing Country: A Study from the Service Quality Perspective. Commun. Assoc. Inf. Syst. 2014, 34, 669–692. [Google Scholar] [CrossRef]
- Zhang, X.; Yan, X.; Cao, X.; Sun, Y.; Chen, H.; She, J. The role of perceived e-health literacy in users’ continuance intention to use mobile healthcare applications: An exploratory empirical study in China. Inf. Technol. Dev. 2018, 24, 198–223. [Google Scholar] [CrossRef]
- Kozinets, R.V. The field behind the screen: Using netnography for marketing research in online communities. J. Mark. Res. 2002, 39, 61–72. [Google Scholar] [CrossRef] [Green Version]
- Murthy, D. Digital Ethnography: An Examination of the use of new technologies for social Research. Sociology 2008, 42, 837–855. [Google Scholar] [CrossRef] [Green Version]
- Analysys. Annual Comprehensive Analysis of Internet Healthcare in China 2018. 2018. Available online: https://www.analysys.cn/article/analysis/detail/20018737 (accessed on 1 December 2018).
- Burt, J.; Abel, G.; Elmore, N.; Lloyd, C.; Benson, J.; Sarson, L.; Carluccio, A.; Campbell, J.; Elliott, M.N.; Roland, M. Understanding negative feedback from South Asian patients: An experimental vignette study. BMJ Open 2016, 6, e011256. [Google Scholar] [CrossRef] [Green Version]
- Octacon. Chinese Sentiment Analysis. 2018. Available online: https://github.com/octacon/bixin (accessed on 10 June 2018).
- Montini, T.; Noble, A.A.; Stelfox, H.T. Content analysis of patient complaints. Int. J. Qual. Health Care 2008, 20, 412–420. [Google Scholar] [CrossRef]
- Liu, C.; Uffenheimer, M.; Nasseri, Y.; Cohen, J.; Ellenhorn, J. “But His Yelp Reviews Are Awful!”: Analysis of General Surgeons’ Yelp Reviews. J. Med. Internet Res. 2019, 21, e11646. [Google Scholar] [CrossRef]
- Saldana, J. The Coding Manual for Qualitative Researchers, 3rd ed.; SAGE Publications Ltd.: London, UK, 2009. [Google Scholar]
- Zhang, X.; Guo, X.; Lai, K.-h.; Yin, C.; Meng, F. From offline healthcare to online health service: The role of offline healthcare satisfaction and habits. J. Electron. Commer. Res. 2017, 18, 138–154. [Google Scholar]
- Derks, D.; Fischer, A.H.; Bos, A.E. The role of emotion in computer-mediated communication: A review. Comput. Hum. Behav. 2008, 24, 766–785. [Google Scholar] [CrossRef]
- Guo, S.; Guo, X.; Fang, Y.; Vogel, D. How Doctors Gain Social and Economic Returns in Online Health-Care Communities: A Professional Capital Perspective. J. Manag. Inf. Syst. 2017, 34, 487–519. [Google Scholar] [CrossRef]


| CMC Features | Potential Positive Impacts | Potential Negative Impacts |
|---|---|---|
| Connectivity | ||
| Text-based communication |
|
|
| Asynchronism |
| |
| Anonymity |
|
| Category | Subcategory | Percentage | Description |
|---|---|---|---|
| Barriers in information providing | Lack of etiology analysis | 6.42% | The doctor fails to explain the etiology for the user. |
| Lack of diagnostic evidence | 18.92% | The doctor fails to provide the user with sufficient evidence for diagnosis. | |
| Lack of operational advice | 16.22% | The doctor fails to give the user explicit operational instructions. | |
| Ambiguous answer | 25.00% | The doctor’s answer is ambiguous. | |
| Barriers in information interpreting | Ignoring information | 3.04% | The doctor ignores the information provided by the user, such as symptoms. |
| Irrelevant answer | 3.38% | The answer provided by the doctor cannot answer the question asked by the user. | |
| Barriers in relationship maintaining | Delayed reply | 26.69% | The doctor is not able to respond to the user in time. |
| Lack of initiative | 10.81% | The doctor fails to provide relevant information actively. | |
| Lack of emotional comport | 5.74% | The doctor lacks emotional comfort for the user. | |
| Unfriendly attitude | 13.18% | The doctor is impatient and unfriendly |
| Category | Subcategory | Percentage | Description |
|---|---|---|---|
| Barriers in information providing | Lack of diagnostic clues | 6.76% | The user fails to provide adequate or accurate diagnostic clues for the doctor |
| Barriers in information interpreting | Insufficient medical knowledge | 4.39% | The medical knowledge of the user is inadequate to interpret or understand the suggestions from the doctor |
| Conflicting opinions | 1.01% | The user has difficulty in understanding the doctor’s advice due to different opinions with their doctors. | |
| Barriers in relationship maintaining | Distrust towards the information | 13.51% | The user doubts the correctness and reliability of the information provided by the doctor. |
| Distrust towards the identity | 3.38% | The user doubts whether the doctor’s identity is real or authorized | |
| Personal remark | 11.82% | The user expresses dissatisfaction in a bad tone |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yan, M.; Tan, H.; Jia, L.; Akram, U. The Antecedents of Poor Doctor-Patient Relationship in Mobile Consultation: A Perspective from Computer-Mediated Communication. Int. J. Environ. Res. Public Health 2020, 17, 2579. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17072579
Yan M, Tan H, Jia L, Akram U. The Antecedents of Poor Doctor-Patient Relationship in Mobile Consultation: A Perspective from Computer-Mediated Communication. International Journal of Environmental Research and Public Health. 2020; 17(7):2579. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17072579
Chicago/Turabian StyleYan, Mengling, Hongying Tan, Luxue Jia, and Umair Akram. 2020. "The Antecedents of Poor Doctor-Patient Relationship in Mobile Consultation: A Perspective from Computer-Mediated Communication" International Journal of Environmental Research and Public Health 17, no. 7: 2579. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17072579





