Effectiveness of a Flexible and Continuous Case Management Program for Suicide Attempters
Abstract
:1. Introduction
2. Material and Methods
2.1. Methods
2.1.1. Subjects
2.1.2. Procedures and Intervention
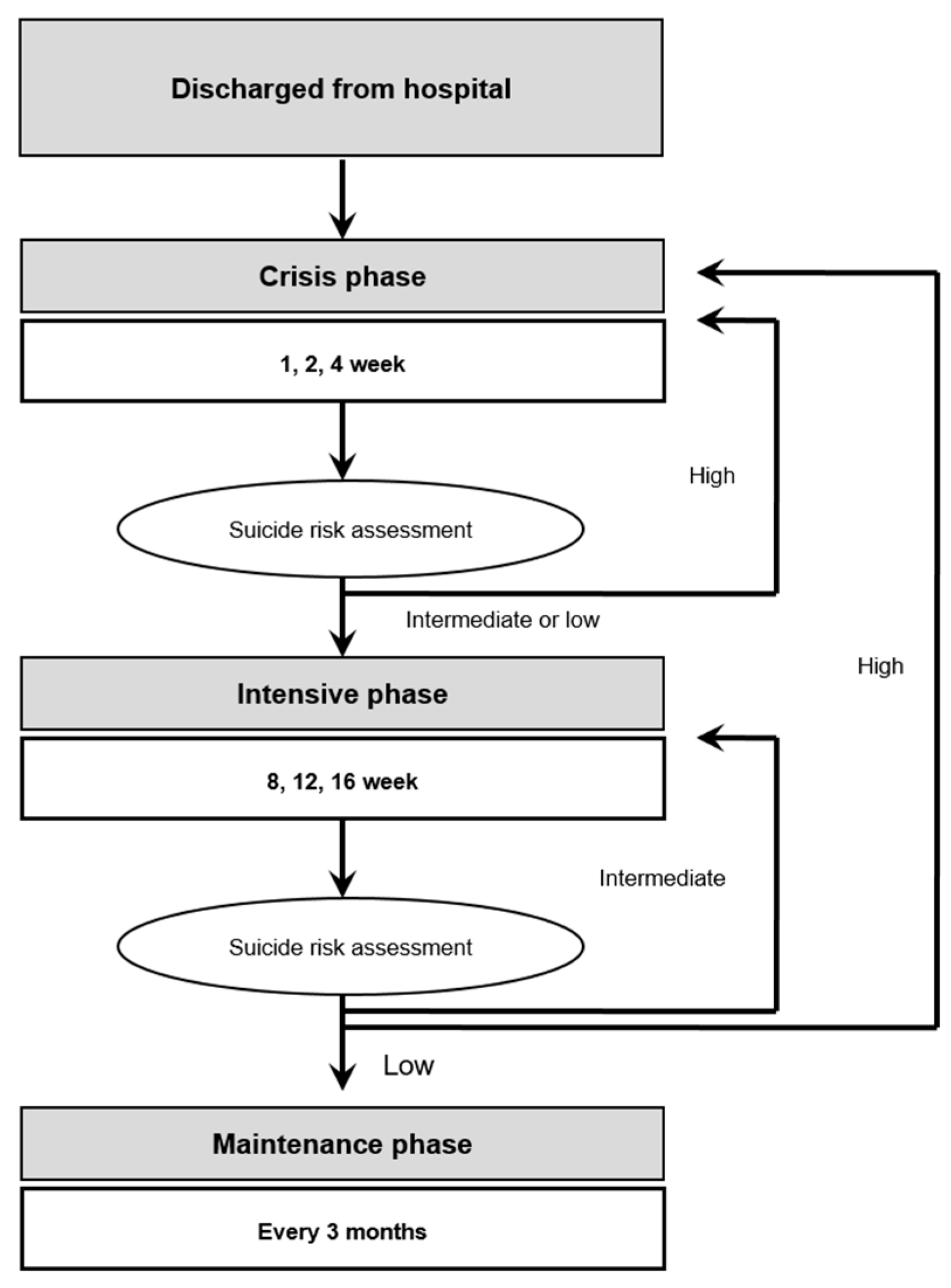
- Crisis management and suicide risk were conducted in weeks 1, 2, and 4. If the suicide risk was high, the attempters underwent crisis management again, but if the risk was low, the attempters went through intensive management until week 6.
- Intensive management constituted case management conducted in weeks 8, 12, and 16, and suicide risk was assessed along with intensive management. If the suicide risk was high, the attempters went back to crisis management; if the risk was moderate, they went back to intensive management; and if the risk was low, they went to the maintenance phase, in which case management was conducted every three months.
- Maintenance was conducted continuously unless the patients refused. The shift between case management phases was carried out after the risk through the most recently conducted systematic suicide risk assessment was verified. If the patients seemed stable after one year and eight months, the frequency of contact was reduced to once every six months, and mail correspondence was sent continuously.
2.2. Measures
2.2.1. Socio-Demographic Characteristics and Suicide-Related Factors
2.2.2. Systematic Suicide Risk Assessment
2.2.3. Identification of Death by Suicide
2.2.4. Statistical Analysis
3. Results
3.1. Characteristics of Participants in the Case Management Program
3.2. Effectiveness of the Case Management Program on Death by Suicide Reattempt
4. Discussion
4.1. Effectiveness of a Flexible, Continuous Case Management Program
- Case management programs can be flexible depending on the patient’s needs [16].
4.2. Death by Suicide
4.3. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Mental Health: Suicide Prevention. Available online: http://www.who.int/mental_health/suicide-prevention/en/ (accessed on 20 March 2020).
- Korea National Statistical Office. Death and Cause of Death in Korea. Available online: https://kosis.kr (accessed on 20 March 2020).
- Mrazek, P.J.; Haggerty, R.J. Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research; National Academies Press: Washington, DC, USA, 1994. [Google Scholar]
- Bertolote, J.M. Suicide prevention: At what level does it work? World Psychiatry 2004, 3, 147–151. [Google Scholar] [PubMed]
- Owens, D.; Horrocks, J.; House, A. Fatal and non-fatal repetition of self-harm. Systematic review. Br. J. Psychiatry 2002, 181, 193–199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hawton, K.; Zahl, D.; Weatherall, R. Suicide following deliberate self-harm: Long-term follow-up of patients who presented to a general hospital. Br. J. Psychiatry 2003, 182, 537–542. [Google Scholar] [CrossRef] [Green Version]
- Suominen, K.; Isometsa, E.; Suokas, J.; Haukka, J.; Achte, K.; Lonnqvist, J. Completed suicide after a suicide attempt: A 37-year follow-up study. Am. J. Psychiatry 2004, 161, 562–563. [Google Scholar] [CrossRef] [Green Version]
- Bostwick, J.M.; Pabbati, C.; Geske, J.R.; McKean, A.J. Suicide attempt as a risk factor for completed suicide: Even more lethal than we knew. Am. J. Psychiatry 2016, 173, 1094–1100. [Google Scholar] [CrossRef] [Green Version]
- Carroll, R.; Metcalfe, C.; Gunnell, D. Hospital presenting self-harm and risk of fatal and non-fatal repetition: Systematic review and meta-analysis. PLoS ONE 2014, 9, e89944. [Google Scholar] [CrossRef]
- Gibb, S.J.; Beautrais, A.L.; Fergusson, D.M. Mortality and further suicidal behaviour after an index suicide attempt: A 10-year study. Aust. N. Z. J. Psychiatry 2005, 39, 95–100. [Google Scholar] [CrossRef]
- Carter, G.L.; Clover, K.; Whyte, I.M.; Dawson, A.H.; Este, C.D. Postcards from the edge project: Randomised controlled trial of an intervention using postcards to reduce repetition of hospital treated deliberate self poisoning. BMJ 2005, 331, 805. [Google Scholar] [CrossRef] [Green Version]
- Cebria, A.I.; Parra, I.; Pamias, M.; Escayola, A.; Garcia-Pares, G.; Punti, J.; Laredo, A.; Valles, V.; Cavero, M.; Oliva, J.C.; et al. Effectiveness of a telephone management programme for patients discharged from an emergency department after a suicide attempt: Controlled study in a spanish population. J. Affect. Disord. 2013, 147, 269–276. [Google Scholar] [CrossRef] [Green Version]
- De Leo, D.; Heller, T. Intensive case management in suicide attempters following discharge from psychiatric care. Aust. J. Prim. Health 2007, 13, 49–58. [Google Scholar] [CrossRef]
- Fleischmann, A.; Bertolote, J.M.; Wasserman, D.; De Leo, D.; Bolhari, J.; Botega, N.J.; De Silva, D.; Phillips, M.; Vijayakumar, L.; Varnik, A.; et al. Effectiveness of brief intervention and contact for suicide attempters: A randomized controlled trial in five countries. Bull. World Health Organ. 2008, 86, 703–709. [Google Scholar] [CrossRef] [PubMed]
- Hassanian-Moghaddam, H.; Sarjami, S.; Kolahi, A.A.; Carter, G.L. Postcards in persia: Randomised controlled trial to reduce suicidal behaviours 12 months after hospital-treated self-poisoning. Br. J. Psychiatry 2011, 198, 309–316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hvid, M.; Wang, A.G. Preventing repetition of attempted suicide—I. Feasibility (acceptability, adherence, and effectiveness) of a baerum-model like aftercare. Nord. J. Psychiatry 2009, 63, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Kawanishi, C.; Aruga, T.; Ishizuka, N.; Yonemoto, N.; Otsuka, K.; Kamijo, Y.; Okubo, Y.; Ikeshita, K.; Sakai, A.; Miyaoka, H.; et al. Assertive case management versus enhanced usual care for people with mental health problems who had attempted suicide and were admitted to hospital emergency departments in japan (action-j): A multicentre, randomised controlled trial. Lancet Psychiatry 2014, 1, 193–201. [Google Scholar] [CrossRef]
- Morthorst, B.; Krogh, J.; Erlangsen, A.; Alberdi, F.; Nordentoft, M. Effect of assertive outreach after suicide attempt in the aid (assertive intervention for deliberate self harm) trial: Randomised controlled trial. BMJ 2012, 345, e4972. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Motto, J.A.; Bostrom, A.G. A randomized controlled trial of postcrisis suicide prevention. Psychiatr. Serv. 2001, 52, 828–833. [Google Scholar] [CrossRef] [PubMed]
- Beautrais, A.L.; Gibb, S.J.; Faulkner, A.; Fergusson, D.M.; Mulder, R.T. Postcard intervention for repeat self-harm: Randomised controlled trial. Br. J. Psychiatry 2010, 197, 55–60. [Google Scholar] [CrossRef] [Green Version]
- Pan, Y.J.; Chang, W.H.; Lee, M.B.; Chen, C.H.; Liao, S.C.; Caine, E.D. Effectiveness of a nationwide aftercare program for suicide attempters. Psychol. Med. 2013, 43, 1447–1454. [Google Scholar] [CrossRef]
- Chen, W.J.; Chen, C.C.; Ho, C.K.; Lee, M.B.; Lin, G.G.; Chou, F.H. Community-based case management for the prevention of suicide reattempts in kaohsiung, taiwan. Commun. Ment. Health J. 2012, 48, 786–791. [Google Scholar] [CrossRef]
- Hawton, K.; Witt, K.G.; Salisbury, T.L.T.; Arensman, E.; Gunnell, D.; Hazell, P.; Townsend, E.; van Heeringen, K. Psychosocial interventions following self-harm in adults: A systematic review and meta-analysis. Lancet Psychiatry 2016, 3, 740–750. [Google Scholar] [CrossRef] [Green Version]
- Simon, R.I.; Hales, R.E. The American Psychiatric Publishing Textbook of Suicide Assessment and Management; American Psychiatric Publishing: Washington, DC, USA, 2006. [Google Scholar]
- Park, S.; Choi, J.W.; Kyoung Yi, K.; Hong, J.P. Suicide mortality and risk factors in the 12 months after discharge from psychiatric inpatient care in korea: 1989–2006. Psychiatry Res. 2013, 208, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.; Lee, J.; Kim, E.; Kim, S.H.; Ha, K.; Kim, Y.S.; Leventhal, B.L.; Ahn, Y.M. Sex difference in risk period for completed suicide following prior attempts: Korea national suicide survey (knss). J. Affect. Disord. 2018, 227, 861–868. [Google Scholar] [CrossRef] [PubMed]


| Variables | Case Management | No-Case Management | χ2 | p-Value |
|---|---|---|---|---|
| (n = 353) | (n = 136) | |||
| Age | 1.576 | 0.665 | ||
| >24 | 52 (14.7%) | 16 (11.8%) | ||
| 25–44 | 127 (36.0%) | 56 (41.2%) | ||
| 45–59 | 93 (26.3%) | 36 (26.5%) | ||
| 60+ | 81 (22.9%) | 28 (20.6%) | ||
| Gender | 0.200 | 0.655 | ||
| Male | 135 (38.2%) | 55 (40.4) | ||
| Female | 218 (61.8%) | 81 (29.6) | ||
| Education (20) a | 1.573 | 0.455 | ||
| Elementary school | 106 (30.5%) | 32 (26.2%) | ||
| Middle/High school | 200 (57.6%) | 71 (58.2%) | ||
| College | 41 (11.8%) | 19 (15.9%) | ||
| Marital status (4) a | 4.110 | 0.128 | ||
| Single or never married | 84 (23.8%) | 31 (23.5%) | ||
| Married/Cohabitation | 204 (57.8%) | 66 (50.0%) | ||
| Separated/Divorced/Widowed | 65 (18.4%) | 35 (26.5%) | ||
| Religion (21) a | 0.245 | 0.620 | ||
| No | 179 (52.2%) | 62 (49.6%) | ||
| Yes | 164 (47.8%) | 63 (50.4%) | ||
| Somatic illness (186) a | 0.276 | 0.600 | ||
| No | 158 (65.3%) | 42 (68.9%) | ||
| Yes | 84 (34.7%) | 19 (31.1%) |
| Variables | Case Management | No-Case Management | χ2 | p-Value |
|---|---|---|---|---|
| (n = 353) | (n = 136) | |||
| Previous suicide attempts (5) a | 1.395 | 0.237 | ||
| No | 259 (73.4%) | 89 (67.9%) | ||
| Yes | 94 (26.6%) | 42 (32.1%) | ||
| Family history of suicide (17) a | 6.592 | 0.010 | ||
| No | 316 (90.3%) | 119 (97.5%) | ||
| Yes | 34 (9.7%) | 3 (2.5%) | ||
| Family history of psychiatric disorders (21) a | 1.514 | 0.219 | ||
| No | 309 (89.8%) | 116 (93.5%) | ||
| Yes | 35 (10.2%) | 8 (6.5%) | ||
| History of psychiatric treatment (22) a | 11.117 | 0.001 | ||
| No | 194 (56.9%) | 93 (73.8%) | ||
| Yes | 147 (43.1%) | 33 (26.2%) | ||
| Ongoing psychiatric treatment (22) a | 5.335 | 0.021 | ||
| No | 249 (73%) | 105 (83.3%) | ||
| Yes | 92 (27.0%) | 21 (16.7%) | ||
| Use of alcohol before the index attempts (6) a | 3.765 | 0.052 | ||
| No | 174 (49.7%) | 53 (39.8%) | ||
| Yes | 176 (50.3%) | 80 (60.2%) | ||
| Psychiatric evaluation at ER | 2.603 | 0.107 | ||
| No | 108 (30.6%) | 52 (38.2%) | ||
| Yes | 245 (69.4%) | 84 (61.8%) | ||
| Current suicidal idea (133) a | 0.958 | 0.328 | ||
| No | 142 (54.6%) | 58 (60.4%) | ||
| Yes | 118 (45.4%) | 38 (39.6%) | ||
| Planned suicide attempts (198) a | 1.296 | 0.255 | ||
| No | 192 (82.4%) | 44 (75.9%) | ||
| Yes | 41 (17.6%) | 14 (24.1%) | ||
| Psychiatric diagnosis (31) a | 7.696 | 0.103 | ||
| Mood disorder | 157 (45.9%) | 45 (38.8%) | ||
| Psychotic disorder | 10 (2.9%) | 1 (0.9%) | ||
| Substance use disorder | 53 (15.5%) | 19 (16.4%) | ||
| Others | 99 (28.9%) | 35 (30.2%) | ||
| No axis I disorder | 23 ((6.7%) | 16 (13.8%) | ||
| Motivation for suicide attempt | ||||
| Interpersonal problem | 236 (66.9%) | 82 (60.3%) | 1.859 | 0.204 |
| Economic or job problem | 46 (13.0%) | 17 (12.5%) | 0.025 | 0.875 |
| Separation problem b | 8 (2.3%) | 3 (2.2%) | 1.000 | |
| Mistreatment or violence problem | 62 (17.6%) | 28 (20.6%) | 0.598 | 0.439 |
| Psychiatric problem b | 8 (2.3%) | 5 (3.7%) | 0.346 | |
| Method of attempt (2) a | 19.122 | 0.008 | ||
| Poisoning | 293 (83.0%) | 102 (76.1%) | ||
| Cutting | 11 (3.1%) | 15 (11.2%) | ||
| Stabbing | 5 (1.4%) | 3 (2.2%) | ||
| Drowning | 1 (0.3%) | 1 (0.7%) | ||
| Hanging | 19 (5.4%) | 3 (2.2%) | ||
| Asphyxia | 16 (4.5%) | 4 (3.0%) | ||
| Falling from a height | 3 (0.8%) | 4 (3.0%) | ||
| Others | 5 (1.4%) | 2 (1.5%) | ||
| Psychiatric Treatment within three months following index attempt | 1.349 | 0.245 | ||
| No | 271 (76.6%) | 111 (81.6%) | ||
| Yes | 82 (23.2%) | 25 (18.4%) | ||
| Duration of case management | - | |||
| Median (IQR) | 364 (210–587) | - | ||
| Mean (SD) | 397.99 (262) | - |
| HR | 95% CI | aHR1 | 95% CI | aHR2 | 95% CI | |
|---|---|---|---|---|---|---|
| Case management | 0.341 | 0.133–0.872 | 0.306 | 0.118–0.790 | 0.266 | 0.085–0.834 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, M.-H.; Lee, J.; Noh, H.; Hong, J.-P.; Kim, H.; Cha, Y.S.; Ahn, J.-S.; Chang, S.-J.; Min, S. Effectiveness of a Flexible and Continuous Case Management Program for Suicide Attempters. Int. J. Environ. Res. Public Health 2020, 17, 2599. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17072599
Kim M-H, Lee J, Noh H, Hong J-P, Kim H, Cha YS, Ahn J-S, Chang S-J, Min S. Effectiveness of a Flexible and Continuous Case Management Program for Suicide Attempters. International Journal of Environmental Research and Public Health. 2020; 17(7):2599. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17072599
Chicago/Turabian StyleKim, Min-Hyuk, Jinhee Lee, Hyunjean Noh, Jin-Pyo Hong, Hyun Kim, Yong Sung Cha, Joung-Sook Ahn, Sei-Jin Chang, and Seongho Min. 2020. "Effectiveness of a Flexible and Continuous Case Management Program for Suicide Attempters" International Journal of Environmental Research and Public Health 17, no. 7: 2599. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17072599





