Epidemiology of Paediatric Shoulder Dislocation: A Nationwide Study in Italy from 2001 to 2014
Abstract
:1. Introduction
2. Materials and Methods
2.1. Population
2.2. Regions of Italy
2.3. Surgical Hospitalization Rates
2.4. Statistics
3. Results
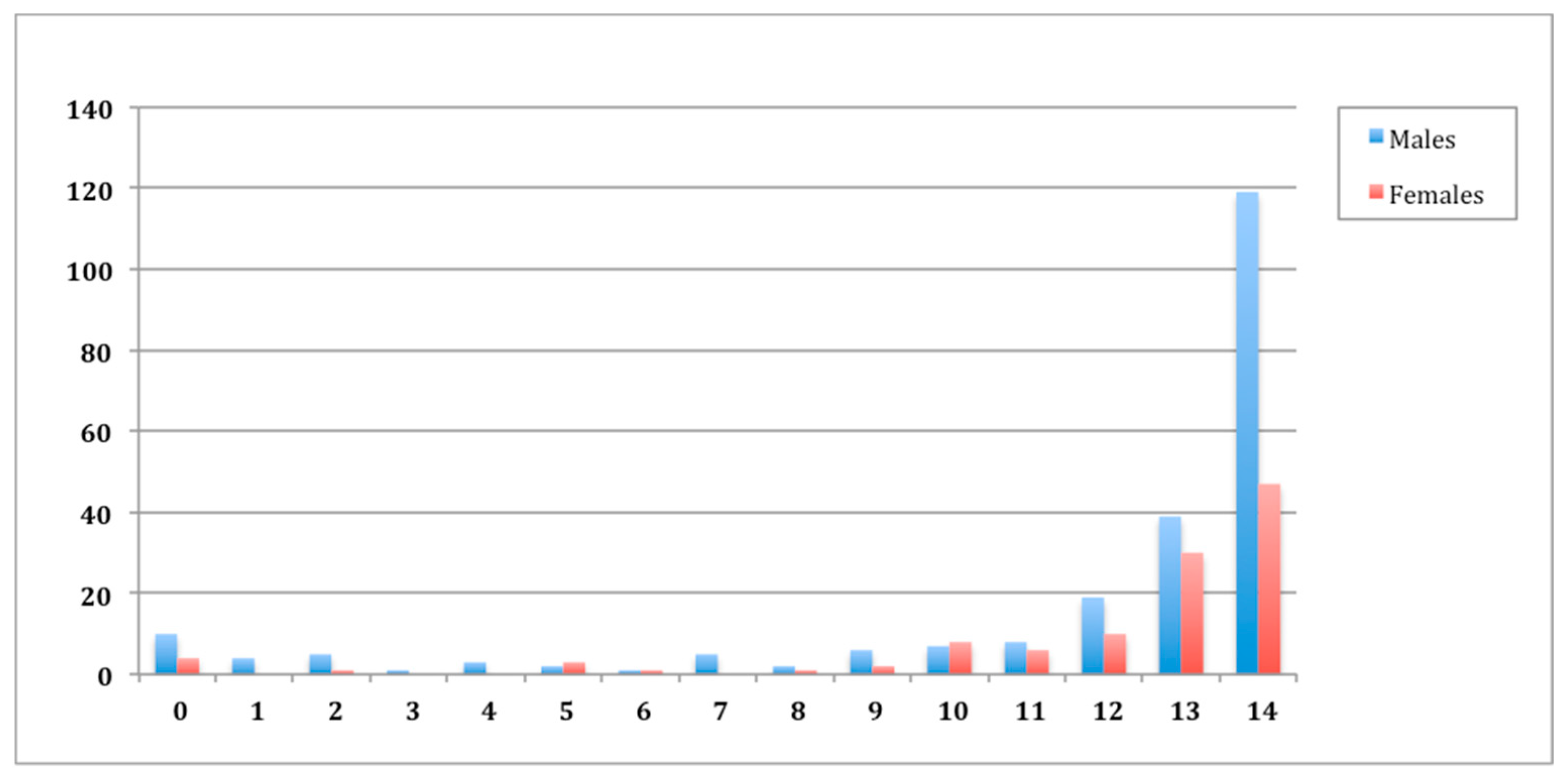
3.1. Demographics
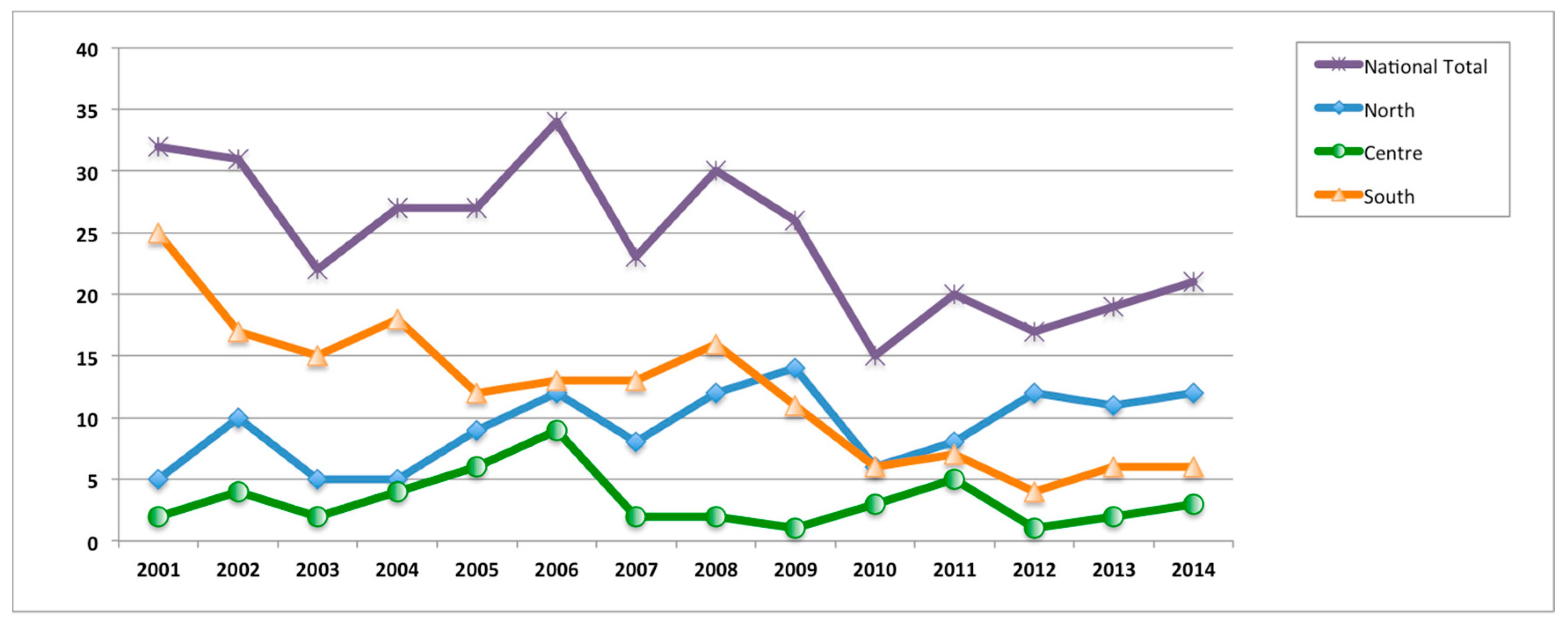
3.2. Region of Hospitalization
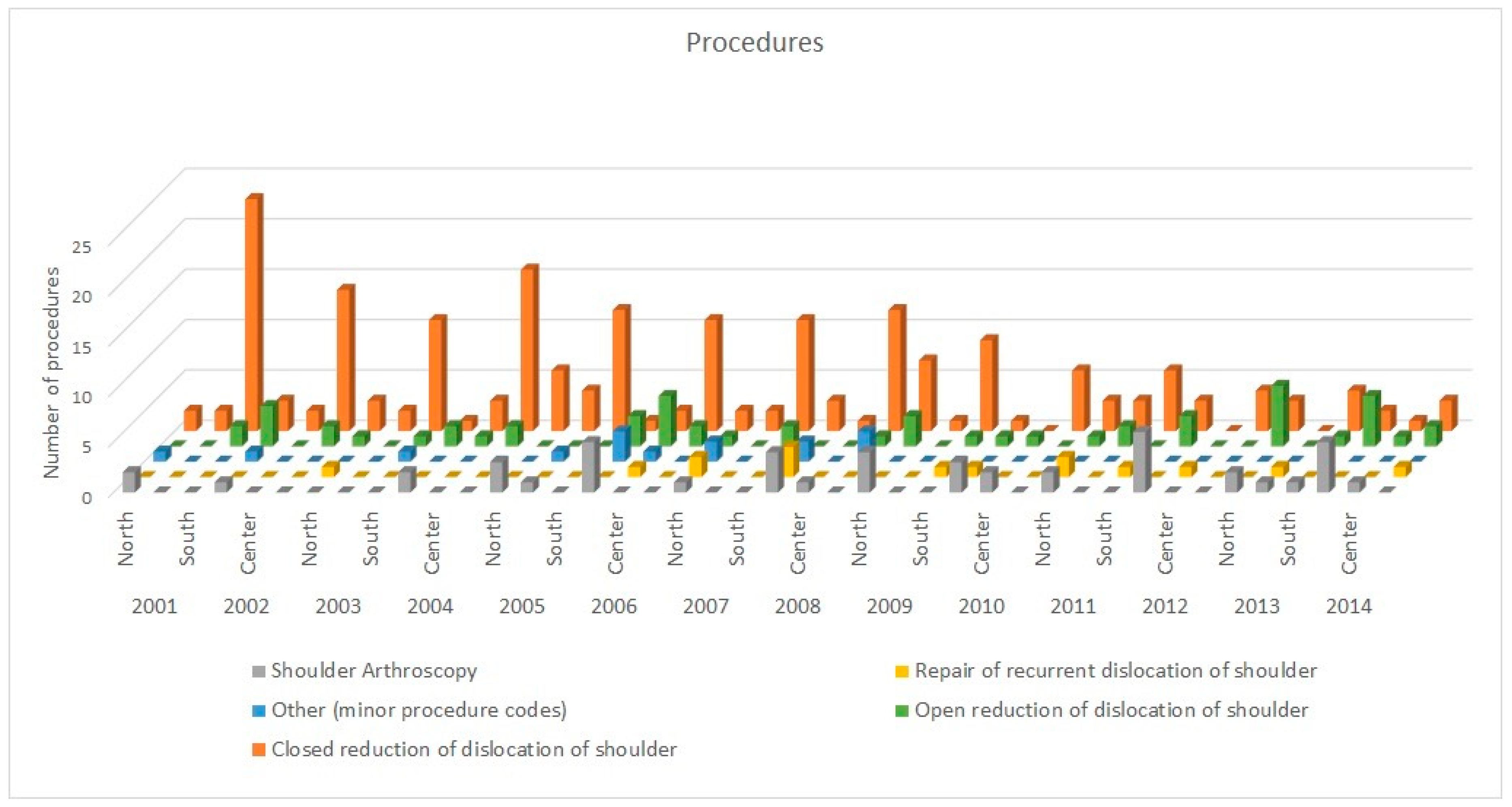
3.3. Admission Diagnosis and Procedure Performed
3.4. Surgical Hospitalization Rates
3.5. Public or Private Hospitalization
3.6. Length of the hospitalization
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Zacchilli, M.A.; Owens, B.D. Epidemiology of shoulder dislocations presenting to emergency departments in the united states. J. Bone Jt. Surg. 2010, 92, 542–549. [Google Scholar] [CrossRef] [PubMed]
- Leroux, T.; Wasserstein, D.; Veillette, C.; Khoshbin, A.; Henry, P.; Chahal, J.; Austin, P.; Mahomed, N.; Ogilvie-Harris, D. Epidemiology of primary anterior shoulder dislocation requiring closed reduction in ontario, canada. Am. J. Sports Med. 2014, 42, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, L.D.; Flanigan, D.C.; Norwig, J.; Jost, P.; Bradley, J. Prevalence and variance of shoulder injuries in elite collegiate football players. Am. J. Sports Med. 2005, 33, 1142–1146. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Forriol, F.; Campi, S.; Maffulli, N.; Denaro, V. Animal models for translational research on shoulder pathologies: From bench to bedside. Sports Med. Arthrosc. Rev. 2011, 19, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Ma, R.; Nielsen, N.M.; Gulotta, L.V.; Dines, J.S.; Owens, B.D. Management of shoulder instability in the skeletally immature patient. J. Am. Acad. Orthop. Surg. 2013, 21, 529–537. [Google Scholar] [PubMed]
- Longo, U.G. Editorial commentary: Unsolved problems in shoulder instability-the dilemma of bone loss! Arthroscopy 2019, 35, 1267–1268. [Google Scholar] [CrossRef] [Green Version]
- Castricini, R.; Longo, U.G.; Petrillo, S.; Candela, V.; De Benedetto, M.; Maffulli, N.; Denaro, V. Arthroscopic latarjet for recurrent shoulder instability. Medicine 2019, 55, 582. [Google Scholar] [CrossRef] [Green Version]
- Longo, U.G.; Buchmann, S.; Berton, A.; Maffulli, N.; Denaro, V. Arthroscopic knots and strength sutures for rotator cuff repair. Sports Med. Arthrosc. Rev. 2011, 19, 251–265. [Google Scholar] [CrossRef]
- Maffulli, N.; Longo, U.G. Conservative management for tendinopathy: Is there enough scientific evidence? Rheumatology 2008, 47, 390–391. [Google Scholar] [CrossRef] [Green Version]
- Longo, U.G.; Loppini, M.; Rizzello, G.; Ciuffreda, M.; Maffulli, N.; Denaro, V. Management of primary acute anterior shoulder dislocation: Systematic review and quantitative synthesis of the literature. Arthrosc. J. Arthrosc. Relat. Surg. 2014, 30, 506–522. [Google Scholar] [CrossRef]
- Longo, U.G.; Loppini, M.; Rizzello, G.; Ciuffreda, M.; Maffulli, N.; Denaro, V. Latarjet, bristow, and eden-hybinette procedures for anterior shoulder dislocation: Systematic review and quantitative synthesis of the literature. Arthrosc. J. Arthrosc. Relat. Surg. 2014, 30, 1184–1211. [Google Scholar] [CrossRef] [PubMed]
- Leroux, T.; Ogilvie-Harris, D.; Veillette, C.; Chahal, J.; Dwyer, T.; Khoshbin, A.; Henry, P.; Mahomed, N.; Wasserstein, D. The epidemiology of primary anterior shoulder dislocations in patients aged 10 to 16 years. Am. J. Sports Med. 2015, 43, 2111–2117. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Rizzello, G.; Locher, J.; Salvatore, G.; Florio, P.; Maffulli, N.; Denaro, V. Bone loss in patients with posterior gleno-humeral instability: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 612–617. [Google Scholar] [CrossRef] [PubMed]
- Southgate, D.F.; Bokor, D.J.; Longo, U.G.; Wallace, A.L.; Bull, A.M. The effect of humeral avulsion of the glenohumeral ligaments and humeral repair site on joint laxity: A biomechanical study. Arthroscopy 2013, 29, 990–997. [Google Scholar] [CrossRef] [PubMed]
- Cleeman, E.; Flatow, E.L. Shoulder dislocations in the young patient. Orthop. Clin. N. Am. 2000, 31, 217–229. [Google Scholar] [CrossRef]
- Hovelius, L. Shoulder dislocation in swedish ice hockey players. Am. J. Sports Med. 1978, 6, 373–377. [Google Scholar] [CrossRef]
- Longo, U.G.; Forriol, F.; Loppini, M.; Lanotte, A.; Salvatore, G.; Maffulli, N.; Denaro, V. The safe zone for avoiding suprascapular nerve injury in bone block procedures for shoulder instability. A cadaveric study. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 1506–1510. [Google Scholar] [CrossRef]
- Longo, U.G.; Rizzello, G.; Loppini, M.; Locher, J.; Buchmann, S.; Maffulli, N.; Denaro, V. Multidirectional instability of the shoulder: A systematic review. Arthrosc. J. Arthrosc. Relat. Surg. 2015, 31, 2431–2443. [Google Scholar] [CrossRef]
- Paulino Pereira, N.R.; van der Linde, J.A.; Alkaduhimi, H.; Longo, U.G.; van den Bekerom, M.P.J. Are collision athletes at a higher risk of re-dislocation after an open bristow-latarjet procedure? A systematic review and meta-analysis. Shoulder Elb. 2018, 10, 75–86. [Google Scholar] [CrossRef]
- Franceschi, F.; Longo, U.G.; Ruzzini, L.; Rizzello, G.; Maffulli, N.; Denaro, V. The Roman Bridge: A “double pulley-suture bridges” technique for rotator cuff repair. BMC Musculoskelet. Disord. 2007, 8, 123. [Google Scholar] [CrossRef] [Green Version]
- Postacchini, F.; Gumina, S.; Cinotti, G. Anterior shoulder dislocation in adolescents. J. Shoulder Elb. Surg. 2000, 9, 470–474. [Google Scholar] [CrossRef] [PubMed]
- Marans, H.; Angel, K.; Schemitsch, E.; Wedge, J. The fate of traumatic anterior dislocation of the shoulder in children. J Bone Jt. Surg Am 1992, 74, 1242–1244. [Google Scholar] [CrossRef]
- Bottoni, C.R.; Wilckens, J.H.; DeBerardino, T.M.; D’Alleyrand, J.-C.G.; Rooney, R.C.; Harpstrite, J.K.; Arciero, R.A. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am. J. Sports Med. 2002, 30, 576–580. [Google Scholar] [CrossRef]
- Hovelius, L.; Olofsson, A.; Sandström, B.; Augustini, B.-G.; Krantz, L.; Fredin, H.; Tillander, B.; Skoglund, U.; Salomonsson, B.; Nowak, J. Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger. J. Bone Jt. Surg. 2008, 90, 945–952. [Google Scholar] [CrossRef]
- Hoelen, M.; Burgers, A.; Rozing, P. Prognosis of primary anterior shoulder dislocation in young adults. Arch. Orthop. Trauma Surg. 1990, 110, 51–54. [Google Scholar] [CrossRef]
- Gigis, I.; Heikenfeld, R.; Kapinas, A.; Listringhaus, R.; Godolias, G. Arthroscopic versus conservative treatment of first anterior dislocation of the shoulder in adolescents. J. Pediatr. Orthop. 2014, 34, 421–425. [Google Scholar] [CrossRef]
- Whelan, D.B.; Litchfield, R.; Wambolt, E.; Dainty, K.N. External rotation immobilization for primary shoulder dislocation: A randomized controlled trial. Clin. Orthop. Relat. Res. 2014, 472, 2380–2386. [Google Scholar] [CrossRef] [Green Version]
- Murray, J.; Leclerc, A.; Pelet, S. Immobilisation in external rotation after primary shoulder dislocation reduces the risk of recurrence in young patients: A randomised controlled trial. Bone Jt. J. 2016, 98, 77. [Google Scholar]
- Uhring, J.; Rey, P.-B.; Rochet, S.; Obert, L. Interest of emergency arthroscopic stabilization in primary shoulder dislocation in young athletes. Orthop. Traumatol. Surg. Res. 2014, 100, S401–S408. [Google Scholar] [CrossRef] [Green Version]
- Blomquist, J.; Solheim, E.; Liavaag, S.; Schroder, C.P.; Espehaug, B.; Havelin, L.I. Shoulder instability surgery in norway: The first report from a multicenter register, with 1-year follow-up. Acta Orthop. 2012, 83, 165–170. [Google Scholar] [CrossRef] [Green Version]
- Cil, A.; Kocher, M.S. Treatment of pediatric shoulder instability. J. Pediatr. Orthop. 2010, 30, S3–S6. [Google Scholar] [CrossRef]
- Locher, J.; Wilken, F.; Beitzel, K.; Buchmann, S.; Longo, U.G.; Denaro, V.; Imhoff, A.B. Hill-sachs off-track lesions as risk factor for recurrence of instability after arthroscopic bankart repair. Arthroscopy 2016, 32, 1993–1999. [Google Scholar] [CrossRef]
- Weber, A.E.; Nathani, A.; Dines, J.S.; Allen, A.A.; Shubin-Stein, B.E.; Arendt, E.A.; Bedi, A. An algorithmic approach to the management of recurrent lateral patellar dislocation. J. Bone Jt. Surg. Am. Vol. 2016, 98, 417–427. [Google Scholar] [CrossRef] [Green Version]
- Kitayama, S.; Sugaya, H.; Takahashi, N.; Matsuki, K.; Kawai, N.; Tokai, M.; Ohnishi, K.; Ueda, Y.; Hoshika, S.; Kitamura, N.; et al. Clinical outcome and glenoid morphology after arthroscopic repair of chronic osseous bankart lesions: A five to eight-year follow-up study. J. Bone Jt. Surg. Am. Vol. 2015, 97, 1833–1843. [Google Scholar] [CrossRef]
- Longo, U.G.; Huijsmans, P.E.; Maffulli, N.; Denaro, V.; De Beer, J.F. Video analysis of the mechanisms of shoulder dislocation in four elite rugby players. J. Orthop. Sci. 2011, 16, 389–397. [Google Scholar] [CrossRef]
- Longo, U.G.; Loppini, M.; Rizzello, G.; Romeo, G.; Huijsmans, P.E.; Denaro, V. Glenoid and humeral head bone loss in traumatic anterior glenohumeral instability: A systematic review. Knee Surg. Sports Traumatol. Arthrosc 2014, 22, 392–414. [Google Scholar] [CrossRef]
- Longo, U.G.; Rizzello, G.; Ciuffreda, M.; Locher, J.; Berton, A.; Salvatore, G.; Denaro, V. Humeral avulsion of the glenohumeral ligaments: A systematic review. Arthroscopy 2016, 32, 1868–1876. [Google Scholar] [CrossRef]
- Longo, U.G.; Loppini, M.; Rizzello, G.; Ciuffreda, M.; Berton, A.; Maffulli, N.; Denaro, V. Remplissage, humeral osteochondral grafts, weber osteotomy, and shoulder arthroplasty for the management of humeral bone defects in shoulder instability: Systematic review and quantitative synthesis of the literature. Arthroscopy 2014, 30, 1650–1666. [Google Scholar] [CrossRef]
- Longo, U.G.; van der Linde, J.A.; Loppini, M.; Coco, V.; Poolman, R.W.; Denaro, V. Surgical versus nonoperative treatment in patients up to 18 years old with traumatic shoulder instability: A systematic review and quantitative synthesis of the literature. Arthrosc. J. Arthrosc. Relat. Surg. 2016, 32, 944–952. [Google Scholar] [CrossRef]
- Ferré, F.; de Belvis, A.G.; Valerio, L.; Longhi, S.; Lazzari, A.; Fattore, G.; Ricciardi, W.; Maresso, A. Health System Review; WHO European Centre for Health Policy: Brussels, Belgium, 2014. [Google Scholar]
- Ventura, M.; Fusco, D.; Bontempi, K.; Colais, P.; Davoli, M. Regional outcome evaluation program (p. Re. Val. E.): Reduction of inequality in access to effective health care in the lazio region of italy (2012–2015). PLoS ONE 2018, 13, e0194972. [Google Scholar] [CrossRef] [Green Version]
- Mangano, A. An analysis of the regional differences in health care utilization in italy. Health Place 2010, 16, 301–308. [Google Scholar] [CrossRef]
- Giannoni, M.; Hitiris, T. The regional impact of health care expenditure: The case of italy. Appl. Econ. 2002, 34, 1829–1836. [Google Scholar] [CrossRef]
- McLAUGHLIN, H.L.; MacLELLAN, D.I. Recurrent anterior dislocation of the shoulder ii. A comparative study. J. Trauma Acute Care Surg. 1967, 7, 191–201. [Google Scholar] [CrossRef]
- Davis, G.; Kline, D.G.; Spinner, R.J.; Zager, E.L.; Garberina, M.J.; Williams, G.R.; McCrory, P. Clinics in neurology and neurosurgery of sport: Peripheral nerve injury. Br. J. Sports Med. 2009, 43, 537–540. [Google Scholar] [CrossRef]
- Calandra, J.J.; Baker, C.L.; Uribe, J. The incidence of hill-sachs lesions in initial anterior shoulder dislocations. Arthrosc. J. Arthrosc. Relat. Surg. 1989, 5, 254–257. [Google Scholar] [CrossRef]
- Hovelius, L. Anterior dislocation of the shoulder in teen-agers and young adults. Five-year prognosis. J. Bone Jt. Surg. Am. Vol. 1987, 69, 393–399. [Google Scholar]
- Simonet, W.T.; Cofield, R.H. Prognosis in anterior shoulder dislocation. Am. J. Sports Med. 1984, 12, 19–24. [Google Scholar] [CrossRef]
- Henry, J.H.; Genung, J.A. Natural history of glenohumeral dislocation—Revisited. Am. J. Sports Med. 1982, 10, 135–137. [Google Scholar] [CrossRef]
- Vellios, E.E.; Trivellas, M.; Arshi, A.; Beck, J.J. Recurrent patellofemoral instability in the pediatric patient: Management and pitfalls. Curr. Rev. Musculoskelet. Med. 2020, 13, 58–68. [Google Scholar] [CrossRef]
- Cordischi, K.; Li, X.; Busconi, B. Intermediate outcomes after primary traumatic anterior shoulder dislocation in skeletally immature patients aged 10 to 13 years. Orthopedics 2009, 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shanley, E.; Thigpen, C.; Brooks, J.; Hawkins, R.J.; Momaya, A.; Kwapisz, A.; Kissenberth, M.J.; Tokish, J.M. Return to sport as an outcome measure for shoulder instability: Surprising findings in nonoperative management in a high school athlete population. Am. J. Sports Med. 2019, 47, 1062–1067. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rockwood, C.A. The Shoulder; Elsevier Health Sciences: Amsterdam, The Netherlands, 2009; Volume 1. [Google Scholar]
- Deitch, J.; Mehlman, C.T.; Foad, S.L.; Obbehat, A.; Mallory, M. Traumatic anterior shoulder dislocation in adolescents. Am. J. Sports Med. 2003, 31, 758–763. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, G.; Slongo, T.; Kohler, G.; Horst, M.; Lampert, C. Traumatic shoulder dislocation in children and adolescents. Eur. J. Trauma 2003, 29, 375–378. [Google Scholar] [CrossRef]
- Rowe, C.R. Prognosis in dislocations of the shoulder. JBJS 1956, 38, 957–977. [Google Scholar] [CrossRef]




| N° of HOSPITALIZATIONS PER YEAR—NATIONAL POPULATION | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Total (ABS) | Total (%) | |
| Male | 24 | 21 | 16 | 18 | 18 | 25 | 16 | 17 | 18 | 9 | 15 | 12 | 10 | 12 | 231 | 67.15% |
| Female | 8 | 10 | 6 | 9 | 9 | 9 | 7 | 13 | 8 | 6 | 5 | 5 | 9 | 9 | 113 | 32.85% |
| Total | 32 | 31 | 22 | 27 | 27 | 34 | 23 | 30 | 26 | 15 | 20 | 17 | 19 | 21 | 344 | 100.00% |
| Avg | ||||||||||||||||
| Male/Female Ratio | 3 | 2.1 | 2.67 | 2 | 2 | 2.78 | 2.29 | 1.31 | 2.25 | 1.5 | 3 | 2.4 | 1.11 | 1.33 | 2.12 | |
| N° OF PROCEDURES PER 100.000 INHABITANTS (0–15 YEARS OLD) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Avg | |
| 0–15 years old Population (ISTAT) | 8,109,389 | 8,148,138 | 8,190,349 | 8,255,712 | 8,283,936 | 8,321,900 | 8,367,043 | 8,428,708 | 8,477,937 | 8,513,222 | 8,325,217 | 8,348,338 | 8,448,133 | 8,383,122 | |
| N° Hospitalizations per 100.000 inh (0–15 y old) | 0.39 | 0.38 | 0.27 | 0.33 | 0.33 | 0.41 | 0.27 | 0.36 | 0.31 | 0.18 | 0.24 | 0.2 | 0.22 | 0.25 | 0.3 |
| HOSPITALIZATION LENGTH (Days)—NATIONAL POPULATION | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Avg | |
| Hospitalization Lenght (days) | 2.4 | 1.1 | 1.2 | 1 | 1.1 | 1.2 | 1.1 | 1 | 1 | 1.1 | 1.1 | 1.1 | 1.1 | 1 | 1.2 |
| N° of HOSPITALIZATIONS PER YEAR—MACROAREA (North-Center-South) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Total (ABS) | Total (%) | |
| North | 5 | 10 | 5 | 5 | 9 | 12 | 8 | 12 | 14 | 6 | 8 | 12 | 11 | 12 | 129 | 37.50% |
| Centre | 2 | 4 | 2 | 4 | 6 | 9 | 2 | 2 | 1 | 3 | 5 | 1 | 2 | 3 | 46 | 13.40% |
| South | 25 | 17 | 15 | 18 | 12 | 13 | 13 | 16 | 11 | 6 | 7 | 4 | 6 | 6 | 169 | 49.10% |
| Total National | 32 | 31 | 22 | 27 | 27 | 34 | 23 | 30 | 26 | 15 | 20 | 17 | 19 | 21 | 344 | 100.00% |
| Migration | Piedmont | Aosta Valley | Lombardy | A.P. of Bolzano | A.P. of Trento | Veneto | Friuli - Venezia Giulia | Liguria | Emilia Romagna | Tuscany | Umbria | Marche | Lazio | Abruzzo | Molise | Campania | Apulia | Basilicata | Calabria | Sicily | Sardinia | Total Hospitalization performed | Extra-Regional Hospitalization (ABS) | Extra-Regional Hospitalization (%) | Regional Hospitalization (ABS) | Regional Hospitalization (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Piedmont | 18 | 0 | 2 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 23 | 5 | 21.74% | 18 | 78.26% |
| Aosta Valley | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 100.00% | 0 | 0.00% |
| Lombardy | 0 | 0 | 32 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 33 | 1 | 3.03% | 32 | 96.97% |
| A.P. of Bolzano | 0 | 0 | 0 | 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6 | 0 | 0.00% | 6 | 100.00% |
| A.P. of Trento | 0 | 0 | 0 | 0 | 1 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 3 | 75.00% | 1 | 25.00% |
| Veneto | 0 | 0 | 1 | 2 | 0 | 13 | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 20 | 7 | 35.00% | 13 | 65.00% |
| Friuli - Venezia Giulia | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 0.00% | 4 | 100.00% |
| Liguria | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 9 | 5 | 55.56% | 4 | 44.44% |
| Emilia Romagna | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 11 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 14 | 3 | 21.43% | 11 | 78.57% |
| Tuscany | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 13 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 15 | 2 | 13.33% | 13 | 86.67% |
| Umbria | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 3 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6 | 5 | 83.33% | 1 | 16.67% |
| Marche | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 1 | 25.00% | 3 | 75.00% |
| Lazio | 0 | 0 | 2 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 18 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 25 | 7 | 28.00% | 18 | 72.00% |
| Abruzzo | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 1 | 25.00% | 3 | 75.00% |
| Molise | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 3 | 2 | 66.67% | 1 | 33.33% |
| Campania | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 46 | 1 | 1 | 0 | 0 | 0 | 50 | 4 | 8.00% | 46 | 92.00% |
| Apulia | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 35 | 0 | 0 | 0 | 0 | 40 | 5 | 12.50% | 35 | 87.50% |
| Basilicata | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 2 | 0 | 0.00% | 2 | 100.00% |
| Calabria | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 10 | 0 | 0 | 11 | 1 | 9.09% | 10 | 90.91% |
| Sicily | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 49 | 0 | 53 | 4 | 7.55% | 49 | 92.45% |
| Sardinia | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 9 | 10 | 1 | 10.00% | 9 | 90.00% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Longo, U.G.; Salvatore, G.; Locher, J.; Ruzzini, L.; Candela, V.; Berton, A.; Stelitano, G.; Schena, E.; Denaro, V. Epidemiology of Paediatric Shoulder Dislocation: A Nationwide Study in Italy from 2001 to 2014. Int. J. Environ. Res. Public Health 2020, 17, 2834. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17082834
Longo UG, Salvatore G, Locher J, Ruzzini L, Candela V, Berton A, Stelitano G, Schena E, Denaro V. Epidemiology of Paediatric Shoulder Dislocation: A Nationwide Study in Italy from 2001 to 2014. International Journal of Environmental Research and Public Health. 2020; 17(8):2834. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17082834
Chicago/Turabian StyleLongo, Umile Giuseppe, Giuseppe Salvatore, Joel Locher, Laura Ruzzini, Vincenzo Candela, Alessandra Berton, Giovanna Stelitano, Emiliano Schena, and Vincenzo Denaro. 2020. "Epidemiology of Paediatric Shoulder Dislocation: A Nationwide Study in Italy from 2001 to 2014" International Journal of Environmental Research and Public Health 17, no. 8: 2834. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17082834





