Accessing Physical Activity and Health Disparities among Underserved Hispanic Children: The Role of Actual and Perceived Motor Competence
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Procedure
2.3. Measures
2.3.1. Actual Motor Competence
2.3.2. Perceived Motor Competence
2.3.3. Physical Activity
2.3.4. Health-Related Quality of Life (HRQoL)
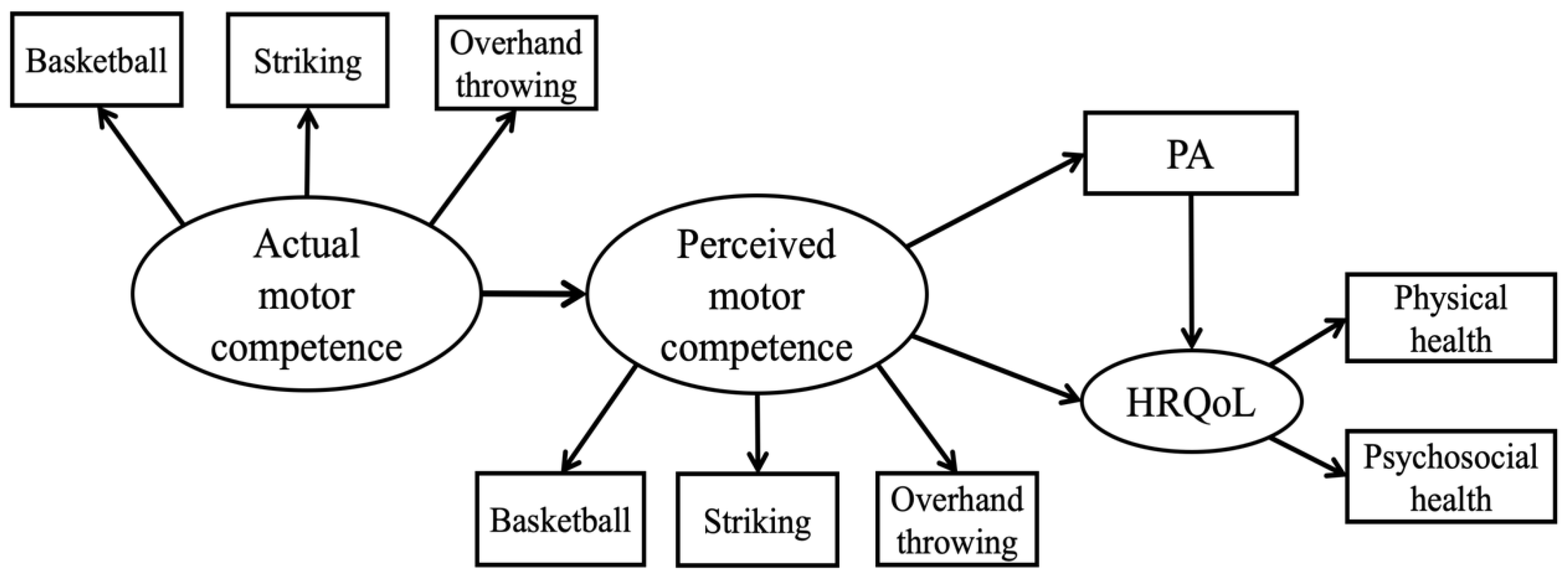
2.4. Data Analysis
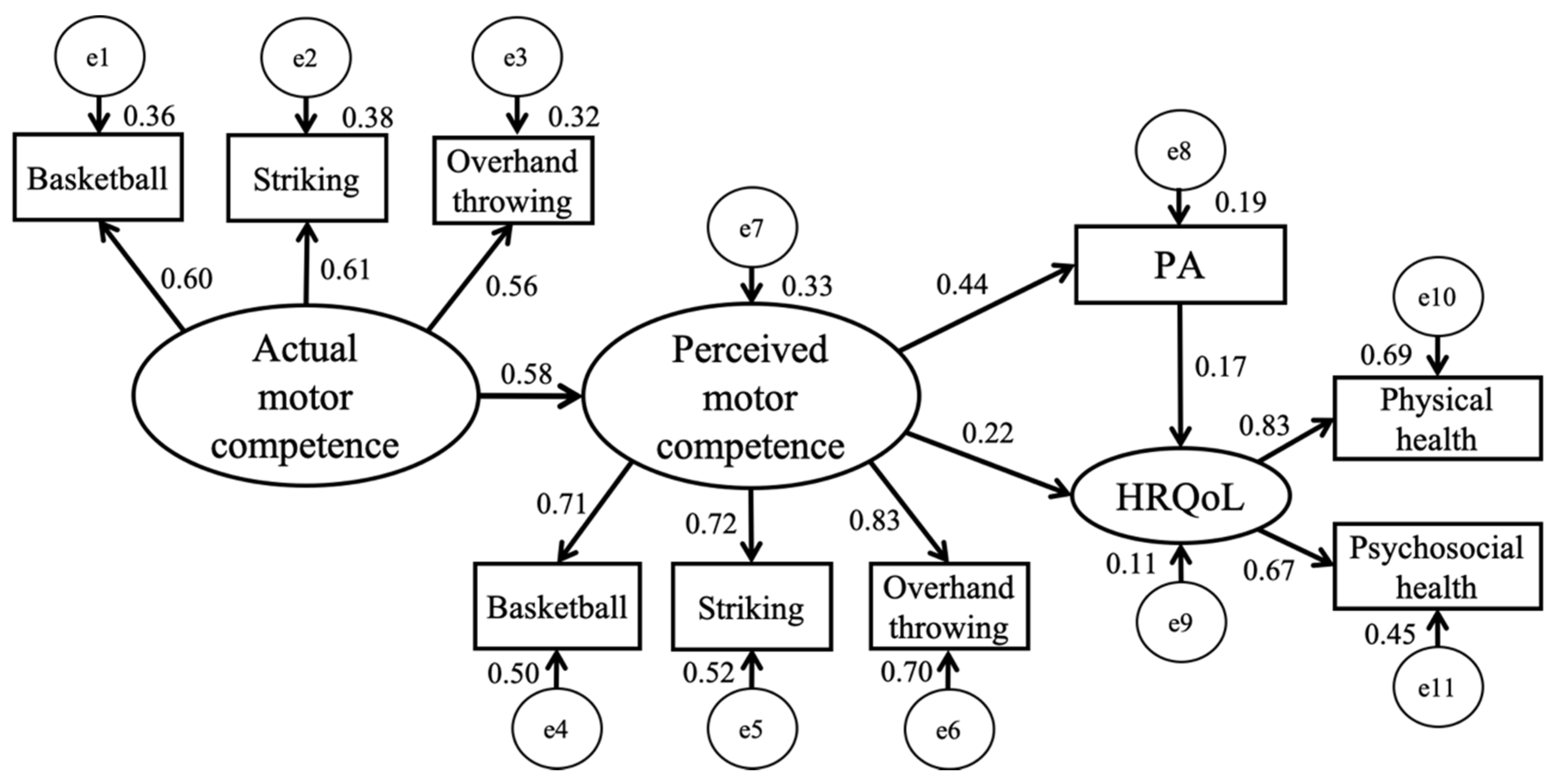
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- United States Department of Health and Human Services. Physical Activity Guidelines for Americans, 2nd ed.; United States Department of Health and Human Services: Washington, DC, USA, 2019. Available online: https://health.gov/paguidelines/second-edition/ (accessed on 1 December 2019).
- López-sánchez, G.F.; Gordon, D.; Hodgson, L.; Stubbs, B.; Smith, L. The Effect of the 2016 Rio de Janeiro Olympics on Spectators’ Physical Activity. Atena J. Sport. Sci. 2019, 1, 1–8. [Google Scholar]
- Powell, K.E.; Paluch, A.E.; Blair, S.N. Physical Activity for Health: What Kind? How Much? How Intense? On Top of What? Annu. Rev. Public Health 2011, 32, 349–365. [Google Scholar] [CrossRef] [Green Version]
- Varni, J.M.; Seid, M.; Kurtin, P. The PedsQLTM 4.0: Reliability and Validity of the Pediatric Quality of Life InventoryTM Version 4.0 Generic Core Scales in Healthy and Patient Populations. Med. Care 2001, 39, 800–812. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.; Chang, M.; Solmon, M.A. Physical Activity, Physical Fitness, and Health-Related Quality of Life in School-Aged Children. J. Teach. Phys. Educ. 2016, 35, 117–126. [Google Scholar] [CrossRef]
- Morrison, K.M.; Shin, S.; Tarnopolsky, M.; Taylor, V.H. Association of Depression & Health Related Quality of Life with Body Composition in Children and Youth with Obesity. J. Affect. Disord. 2015, 172, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Steele, R.G.; Gayes, L.A.; Dalton, W.T.; Smith, C.; Maphis, L.; Conway-Williams, E. Change in Health-Related Quality of Life in the Context of Pediatric Obesity Interventions: A Meta-Analytic Review. Health Psychol. 2016, 35, 1097–1109. [Google Scholar] [CrossRef] [Green Version]
- Quek, Y.H.; Tam, W.W.; Zhang, M.W.; Ho, R.C. Exploring the Association between Childhood and Adolescent Obesity and Depression: A Meta-analysis. Obes. Rev. 2017, 18, 742–754. [Google Scholar] [CrossRef]
- Breslin, G.; Gossrau-Breen, D.; McCay, N.; Gilmore, G.; MacDonald, L.; Hanna, D. Physical Activity, Gender, Weight Status, and Wellbeing in 9- to 11-Year-Old Children: A Cross-Sectional Survey. J. Phys. Act. Health 2012, 9, 394–401. [Google Scholar] [CrossRef]
- Chen, C.; Zhang, T.; Gu, X.; Lee, J.; Ren, S.; Wang, H. Understanding Adolescents’ Need Support, Need Satisfaction, and Health-Related Outcomes: A Self-Determination Health Behavior Perspective. Int. J. Environ. Res. Public Health 2019, 17, 104. [Google Scholar] [CrossRef] [Green Version]
- Centers for Disease Control and Prevention. Overweight and Obesity. Available online: https://www.cdc.gov/obesity/data/index.html/ (accessed on 1 December 2019).
- Ogden, C.L.; Carroll, M.D.; Kit, B.K.; Flegal, K.M. Prevalence of Childhood and Adult Obesity in the United States, 2011–2012. J. Am. Med. Assoc. 2014, 311, 806–814. [Google Scholar] [CrossRef] [Green Version]
- Butte, N.F.; Gregorich, S.E.; Tschann, J.M.; Penilla, C.; Pasch, L.A.; De Groat, C.L.; Flores, E.; Deardorff, J.; Greenspan, L.C.; Martinez, S.M. Longitudinal Effects of Parental, Child and Neighborhood Factors on Moderate-Vigorous Physical Activity and Sedentary Time in Latino Children. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Belcher, B.R.; Berrigan, D.; Dodd, K.W.; Emken, B.A.; Chou, C.P.; Spuijt-Metz, D. Physical Activity in US Youth: Impact of Race/Ethnicity, Age, Gender, & Weight Status. Med. Sci. Sport. Exerc. 2010, 42, 2211–2221. [Google Scholar] [CrossRef] [Green Version]
- Fakhouri, T.H.; Hughes, J.P.; Brody, D.J.; Kit, B.K.; Ogden, C.L. Physical Activity and Screen-Time Viewing among Elementary School-Aged Children in the United States from 2009 to 2010. JAMA Pediatr. 2013, 167, 223–229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chu, T.L.; Zhang, T.; Zhang, X.; Thomas, K.; Gu, X. School Environments Predict Hispanic Children’s Physical Education Related Outcomes through Basic Psychological Need Satisfaction. Learn. Individ. Differ. 2020, 80, 101844. [Google Scholar] [CrossRef]
- Tran, B.X.; Nghiem, S.; Afoakwah, C.; Latkin, C.A.; Ha, G.H.; Nguyen, T.P.; Doan, L.P.; Pham, H.Q.; Ho, C.S.H.; Ho, R.C.M. Characterizing Obesity Interventions and Treatment for Children and Youths during 1991–2018. Int. J. Environ. Res. Public Health 2019, 16, 4227. [Google Scholar] [CrossRef] [Green Version]
- Stodden, D.F.; Goodway, J.D.; Langendorfer, S.J.; Roberton, M.A.; Rudisill, M.E.; Garcia, C.; Garcia, L.E. A Developmental Perspective on the Role of Motor Skill Competence in Physical Activity: An Emergent Relationship. Quest 2008, 60, 290–306. [Google Scholar] [CrossRef]
- Cattuzzo, M.T.; dos Santos Henrique, R.; Ré, A.H.N.; de Oliveira, I.S.; Melo, B.M.; de Sousa Moura, M.; de Araújo, R.C.; Stodden, D. Motor Competence and Health Related Physical Fitness in Youth: A Systematic Review. J. Sci. Med. Sport 2016, 19, 123–129. [Google Scholar] [CrossRef]
- Lubans, D.R.; Morgan, P.J.; Cliff, D.P.; Barnett, L.M.; Okely, A.D. Fundamental Movement Skills in Children and Adolescents: Review of Associated Health Benefits. Sport. Med. 2010, 40, 1019–1035. [Google Scholar] [CrossRef] [Green Version]
- Gu, X.; Keller, J.; Weiller, K.; Zhang, T. The Roles of Physical Activity and Sedentary Behavior on Hispanic Children’s Mental Health: A Motor Skill Perspective. Qual. Life Res. 2018, 27, 185–193. [Google Scholar] [CrossRef]
- Robinson, L.E.; Stodden, D.F.; Barnett, L.M.; Lopes, V.P.; Logan, S.W. Rodrigues, Luis Paulo Luís D’Hondt, E. Motor Competence and Its Effect on Positive Developmental Trajectories of Health. Sport. Med. 2015, 45, 1273–1284. [Google Scholar] [CrossRef]
- Lee, J.; Zhang, T.; Chu, T.L.; Gu, X.; Zhu, P. Effects of a Fundamental Motor Skill-Based Afterschool Program on Children’s Physical and Cognitive Health Outcomes. Int. J. Environ. Res. Public Health 2020, 17, 733. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.; Zhang, T.; Chu, T.L.; Gu, X. Effects of a Need-Supportive Motor Skill Intervention on Children’s Motor Skill Competence and Physical Activity. Children 2020, 7, 21. [Google Scholar] [CrossRef] [Green Version]
- Barnett, L.M.; van Beurden, E.; Morgan, P.J.; Brooks, L.O.; Beard, J.R. Childhood Motor Skill Proficiency as a Predictor of Adolescent Physical Activity. J. Adolesc. Health 2009, 44, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Brian, A.; Goodway, J.D.; Logan, J.A.; Sutherland, S.; Brian, A.; Goodway, J.D.; Logan, J.A.; Sutherland, S.; Brian, A. SKIPing with Head Start Teachers: Influence of T-SKIP on Object-Control Skills. Res. Q. Exerc. Sport 2017, 88, 479–491. [Google Scholar] [CrossRef] [PubMed]
- Barnett, L.M.; Morgan, P.J.; van Beurden, E.; Ball, K.; Lubans, D.R. A Reverse Pathway? Actual and Perceived Skill Proficiency and Physical Activity. Med. Sci. Sport. Exerc. 2011, 43, 898–904. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- True, L.; Brian, A.; Goodway, J.; Stodden, D. Relationships between Productand Process-Oriented Measures of Motor Competence and Perceived Competence. J. Motor Learn. Dev. 2017, 5, 319–335. [Google Scholar] [CrossRef]
- Khodaverdi, Z.; Bahram, A.; Stodden, D.; Kazemnejad, A. The Relationship between Actual Motor Competence and Physical Activity in Children: Mediating Roles of Perceived Motor Competence and Health-Related Physical Fitness. J. Sport. Sci. 2016, 34, 1523–1529. [Google Scholar] [CrossRef]
- Gu, X.; Thomas, K.T.; Chen, Y.L. The Role of Perceived and Actual Motor Competency on Children’s Physical Activity and Cardiorespiratory Fitness during Middle Childhood. J. Teach. Phys. Educ. 2017, 36, 388–397. [Google Scholar] [CrossRef]
- Chu, T.L.; Zhang, T.; Thomas, K.T.; Zhang, X.; Gu, X. Predictive Strengths of Basic Psychological Needs in Physical Education among Hispanic Children: A Gender-Based Approach. J. Teach. Phys. Educ. 2019, 1–8. [Google Scholar] [CrossRef]
- Goodway, J.D.; Robinson, L.E.; Crowe, H.; Goodway, J.D.; Robinson, L.E.; Crowe, H. Gender Differences in Fundamental Motor Skill Development in Disadvantaged Preschoolers from Two Geographical Regions. Res. Q. Exerc. Sport 2010, 81, 17–24. [Google Scholar] [CrossRef]
- Gu, X. Fundamental Motor Skill, Physical Activity, and Sedentary Behavior in Socioeconomically Disadvantaged Kindergarteners. Psychol. Heath Med. 2016, 21, 871–881. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.; Chen, Y.L.; Jackson, A.W.; Zhang, T. Impact of a Pedometer-Based Goal-Setting Intervention on Children’s Motivation, Motor Competence, and Physical Activity in Physical Education. Phys. Educ. Sport Pedagog. 2018, 23, 54–65. [Google Scholar] [CrossRef]
- Chen, W.; Zhu, W.; Mason, S.; Hammond-Bennett, A.; Colombo-Dougovito, A.; HammondBennett, A.; ColomboDougovito, A. Effectiveness of Quality Physical Education in Improving Students’ Manipulative Skill Competency. J. Sport Health Sci. 2016, 5, 231–238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Association for Sport and Physical Education. PE Metrics: Assessing National Standards 1–6 in Elementary School; National Association for Sport and Physical Education: Reston, VA, USA, 2010. [Google Scholar]
- Thomas, J.; Nelson, J.; Silverman, S. Research Methods in Physical Activity; Human Kinetics: Champaign, IL, USA, 2015. [Google Scholar]
- Dyson, B.; Placek, J.H.; Graber, K.C.; Fisette, J.L.; Rink, J.; Zhu, W.; Avery, M.; Franck, M.; Fox, C.; Raynes, D.; et al. Development of PE Metrics Elementary Assessments for National Physical Education Standard 1. Meas. Phys. Educ. Exerc. Sci. 2011, 15, 100–118. [Google Scholar] [CrossRef]
- Williams, G.C.; Freedman, Z.R.; Deci, E.L. Supporting Autonomy to Motivate Glucose Control in Patients with Diabetes. Diabetes Care 1998, 21, 1644–1651. [Google Scholar] [CrossRef] [PubMed]
- Deci, E.L.; Ryan, R.M. Intrinsic Motivation and Self-Determination in Human Behavior; Plenum Press: New York, NY, USA, 1985. [Google Scholar]
- Kowalski, K.C.; Crocker, P.R.E.; Donen, R.M. The Physical Activity Questionnaire for Older Children (PAQ-C) and Adolescents (PAQ-A) Manual. Coll. Kinesiol. Univ. Saskatchewan 2004, 87, 1–38. [Google Scholar]
- Benítez-Porres, J.; López-Fernández, I.; Raya, J.F.; Álvarez Carnero, S.; Alvero-Cruz, J.R.; Álvarez Carnero, E. Reliability and Validity of the PAQ-C Questionnaire to Assess Physical Activity in Children. J. Sch. Health 2016, 86, 677–685. [Google Scholar] [CrossRef]
- Arbuckle, J. IBM SPSS AmosTM 25 User’s Guide; SPSS: Chicago, IL, USA, 2017. [Google Scholar]
- Hooper, D.; Coughlan, J.; Mullen, M.R. Structural Equation Modelling: Guidelines for Determining Model Fit. Electron. J. Bus. Res. Methods 2008, 6, 53–60. [Google Scholar] [CrossRef]
- Markus, K.A. Principles and Practice of Structural Equation Modeling by Rex B. Kline. Struct. Equ. Model. A Multidiscip. J. 2012, 19, 509–512. [Google Scholar] [CrossRef]
- Preacher, K.J.; Hayes, A.F. Asymptotic and Resampling Strategies for Assessing and Comparing Indirect Effects in Multiple Mediator Models. Behav. Res. Methods 2008, 40, 879–891. [Google Scholar] [CrossRef]
- Chou, C.P.; Bentler, P.M. Estimates and Tests in Structural Equation Modeling. In Structural Equation Modeling: Concepts, Issues, and Applications; Hoyle, R., Ed.; Sage: Newbury Park, CA, USA, 1995; pp. 37–55. [Google Scholar]
- Hu, L.T.; Bentler, P.M. Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria versus New Alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Kline, R.N. Principles and Practice of Structural Equation Modeling, 2nd ed.; Guilford Press: New York, NY, USA, 2005. [Google Scholar]
- Lubans, D.; Richards, J.; Hillman, C.; Faulkner, G.; Beauchamp, M.; Nilsson, M.; Kelly, P.; Smith, J.; Raine, L.; Biddle, S. Physical Activity for Cognitive and Mental Health in Youth: A Systematic Review of Mechanisms. Pediatrics 2016, 138, e20161642. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Meester, A.; Stodden, D.; Brian, A.; True, L.; Cardon, G.; Tallir, I.; Haerens, L. Associations among Elementary School Children’s Actual Motor Competence, Perceived Motor Competence, Physical Activity and BMI: A Cross-Sectional Study. PLoS ONE 2016, 11, e0164600. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goodway, J.D.; Rudisill, M.E. Perceived Physical Competence and Actual Motor Skill Competence of African American Preschool Children. Adapt. Phys. Act. Q. 1997, 14, 314–326. [Google Scholar] [CrossRef]
- Robinson, L.E. The Relationship between Perceived Physical Competence and Fundamental Motor Skills in Preschool Children. Child. Care Health Dev. 2011, 37, 589–596. [Google Scholar] [CrossRef]
- Famelia, R.; Goodway, J.D.; Tsuda, E.; Bakhtiar, S.; Goodway, J.D. Relationships among Perceived and Actual Motor Skill Competence and Physical Activity in Indonesian Preschoolers. J. Motor Learn. Dev. 2018, 6, S403–S423. [Google Scholar] [CrossRef]
- Bardid, F.; De Meester, A.; Tallir, I.; Cardon, G.; Lenoir, M.; Haerens, L. Configurations of Actual and Perceived Motor Competence among Children: Associations with Motivation for Sports and Global Self-Worth. Hum. Mov. Sci. 2016, 50, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Barnett, L.M.; Morgan, P.J.; van Beurden, E.; Beard, J.R. Perceived Sports Competence Mediates the Relationship between Childhood Motor Skill Proficiency and Adolescent Physical Activity and Fitness: A Longitudinal Assessment. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Southall, J.E.; Okely, A.D.; Steele, J.R. Actual and Perceived Physical Competence in Overweight and Nonoverweight Children. Pediatr. Exerc. Sci. 2004, 16, 15–24. [Google Scholar] [CrossRef]
- Lee, J.; Zhang, T.; Chu, T.L.; Zhang, X.; Weiller-abels, K.H.; Keller, J. Comprehensive School Physical Activity Program and Physical Literacy: Exploring Preservice Elementary Classroom Teachers’ Perspectives. Adv. Phys. Educ. 2019, 9, 314–330. [Google Scholar] [CrossRef] [Green Version]
- Estevan, I.; Barnett, L.M. Considerations Related to the Definition, Measurement and Analysis of Perceived Motor Competence. Sport. Med. 2018, 48, 2685–2694. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Solmon, M.A.; Gao, Z.; Kosma, M. Promoting School Students’ Physical Activity: A Social Ecological Perspective. J. Appl. Sport Psychol. 2012, 24, 92–105. [Google Scholar] [CrossRef]
- Zhang, T.; Gu, X.; Burgett, J.; Keller, J.; Zhang, X. The Role of Built Environments on Children’s Sedentary Behavior: A Social Ecological Perspective. World J. Prev. Med. 2017, 5, 33–42. [Google Scholar] [CrossRef] [Green Version]
| Performance | Criterion | Total Score |
|---|---|---|
| Basketball dribbling, passing, and receiving | Dribbling (0–4) Passing (0–4) Receiving (0–4) | 0–12 (9 = competent) |
| Striking with a paddle (one trial) | Form (0–4) Continuous strikes (0–4) | 0–8 (6 = competent) |
| Overhand throwing | Form (0–4; 1st, 2nd, 3rd) Accuracy to target (0–4; 1st, 2nd, 3rd) | 0–24 (18 = competent) |
| Variables | Range | M | SD | Skewness | Kurtosis |
|---|---|---|---|---|---|
| 1. Basketball | 3.5–12 | 9.35 | 1.92 | −0.66 | −0.02 |
| 2. Striking | 2–8 | 5.31 | 1.86 | −0.19 | −1.1 |
| 3. Overhand Throwing | 6–24 | 16.49 | 3.81 | −0.16 | −0.28 |
| 4. PMC-Basketball | 1–7 | 5.31 | 1.63 | −0.99 | 0.18 |
| 5. PMC-Striking | 1–7 | 4.43 | 1.59 | −0.25 | −0.64 |
| 6. PMC-Overhand Throwing | 1–7 | 5.22 | 1.44 | −0.58 | −0.44 |
| 7. Physical Activity | 1.52–4.86 | 3.15 | 0.66 | −0.15 | −0.10 |
| 8. Physical Health | 0–100 | 81.88 | 1.13 | −1.5 | 3.47 |
| 9. Psychosocial Health | 18.33–100 | 74.96 | 1.03 | −0.95 | 0.99 |
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Basketball | — | ||||||||
| 2. Striking | 0.36 ** | — | |||||||
| 3. Overhand Throwing | 0.34 ** | 0.34 ** | — | ||||||
| 4. PMC-Basketball | 0.26 ** | 0.21 ** | 0.22 ** | — | |||||
| 5. PMC-Striking | 0.28 ** | 0.39 ** | 0.26 ** | 0.46 ** | — | ||||
| 6. PMC-Overhand Throwing | 0.28 ** | 0.28 ** | 0.27 ** | 0.61 ** | 0.60 ** | — | |||
| 7. Physical Activity | 0.07 | 0.07 | 0.06 | 0.36 ** | 0.37 ** | 0.34 ** | — | ||
| 8. Physical Health | 0.04 | 0.01 | 0.16 * | 0.26 ** | 0.17 * | 0.18 ** | 0.21 ** | — | |
| 9. Psychosocial Health | −0.04 | 0.03 | 0.03 | 0.11 | 0.15 * | 0.15 * | 0.20 ** | 0.56 ** | — |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, T.; Lee, J.; Chu, T.L.; Chen, C.; Gu, X. Accessing Physical Activity and Health Disparities among Underserved Hispanic Children: The Role of Actual and Perceived Motor Competence. Int. J. Environ. Res. Public Health 2020, 17, 3013. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17093013
Zhang T, Lee J, Chu TL, Chen C, Gu X. Accessing Physical Activity and Health Disparities among Underserved Hispanic Children: The Role of Actual and Perceived Motor Competence. International Journal of Environmental Research and Public Health. 2020; 17(9):3013. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17093013
Chicago/Turabian StyleZhang, Tao, Joonyoung Lee, Tsz Lun (Alan) Chu, Changzhou Chen, and Xiangli Gu. 2020. "Accessing Physical Activity and Health Disparities among Underserved Hispanic Children: The Role of Actual and Perceived Motor Competence" International Journal of Environmental Research and Public Health 17, no. 9: 3013. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17093013






