Reality Check 2: The Cost-Effectiveness of Policy Disallowing Body Checking in Non-Elite 13- to 14-Year-Old Ice Hockey Players
Abstract
:1. Introduction
2. Materials and Methods
2.1. Effectiveness
2.2. Healthcare Resource Use and Costs
2.3. Unit Costs
2.4. Cost-Effectiveness Analysis
2.5. Provincial and National Projection
2.6. Statistical Analysis
3. Results
3.1. Cost-Effectiveness Analysis Results
3.2. Provincial and National Projection Results
4. Discussion
4.1. Interpretation
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Annual Report 2018–2019. Hockey Canada. 2019. Available online: https://cdn.agilitycms.com/hockey-canada/Corporate/About/Downloads/2018-19-hockey-canada-annual-report-e.pdf (accessed on 13 November 2019).
- Taliaferro, L.A.; Rienzo, B.A.; Miller, M.D.; Pigg, R.M.; Dodd, V.J. High School Youth and Suicide Risk: Exploring Protection Afforded Through Physical Activity and Sport Participation. J. Sch. Health 2008, 78, 545–553. [Google Scholar] [CrossRef] [PubMed]
- Slutzky, C.B.; Simpkins, S.D. The link between children’s sport participation and self-esteem: Exploring the mediating role of sport self-concept. Psychol. Sport Exerc. 2009, 10, 381–389. [Google Scholar] [CrossRef]
- Fox, C.K.; Barranderson, D.J.; Neumark-Sztainer, D.; Wall, M. Physical Activity and Sports Team Participation: Associations with Academic Outcomes in Middle School and High School Students. J. Sch. Health 2010, 80, 31–37. [Google Scholar] [CrossRef]
- Daneshvar, D.H.; Riley, D.O.; Nowinski, C.J.; McKee, A.C.; Stern, R.A.; Cantu, R.C. Long-term consequences: Effects on normal development profile after concussion. Phys. Med. Rehabil. Clin. N. Am. 2011, 22, 683–700. [Google Scholar] [CrossRef]
- Fridman, L.; Fraser-Thomas, J.L.; McFaull, S.R.; MacPherson, A.K. Epidemiology of sports-related injuries in children and youth presenting to Canadian emergency departments from 2007–2010. Sports Med. Arthrosc. Rehabil. Technol. 2013, 5, 30. [Google Scholar] [CrossRef]
- Buckwalter, J.A.; Lane, N.E. Athletics and Osteoarthritis. Am. J. Sports Med. 1997, 25, 873–881. [Google Scholar] [CrossRef] [PubMed]
- Kujala, U.M.; Kettunen, J.; Paananen, H.; Aalto, T.; Battié, M.; Impivaara, O.; Videman, T.; Sarna, S. Knee osteoarthritis in former runners, soccer players, weight lifters, and shooters. Arthritis Rheum. 1995, 38, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Saxon, L.; Finch, C.; Bass, S. Sports Participation, Sports Injuries and Osteoarthritis. Sports Med. 1999, 28, 123–135. [Google Scholar] [CrossRef] [PubMed]
- Babcock, L.; Byczkowski, T.; Wade, S.L.; Ho, M.; Mookerjee, S.; Bazarian, J.J. Predicting Postconcussion Syndrome After Mild Traumatic Brain Injury in Children and Adolescents Who Present to the Emergency Department. JAMA Pediatr. 2013, 167, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Barlow, K.M.; Crawford, S.; Stevenson, A.; Sandhu, S.S.; Belanger, F.; Dewey, D. Epidemiology of Postconcussion Syndrome in Pediatric Mild Traumatic Brain Injury. Pediatrics 2010, 126, e374–e381. [Google Scholar] [CrossRef] [PubMed]
- Emery, C.A.; Kang, J.; Shrier, I.; Goulet, C.; Hagel, B.E.; Benson, B.W.; Nettel-Aguirre, A.; McAllister, J.R.; Hamilton, G.M.; Meeuwisse, W.H. Risk of Injury Associated With Body Checking Among Youth Ice Hockey Players. JAMA 2010, 303, 2265–2272. [Google Scholar] [CrossRef] [PubMed]
- Hockey Canada. Teaching Checking: Body Checking. Checking Resource Guide. Available online: https://cdn.hockeycanada.ca/hockey-canada/Hockey-Programs/Coaching/Checking/Downloads/teaching_checking_progression_body_checking.pdf (accessed on 30 April 2021).
- Black, A.M.; Hagel, B.E.; Palacios-Derflingher, L.; Schneider, K.J.; Emery, C.A. The risk of injury associated with body checking among Pee Wee ice hockey players: An evaluation of Hockey Canada’s national body checking policy change. Br. J. Sports Med. 2017, 51, 1767–1772. [Google Scholar] [CrossRef] [PubMed]
- SportMed, B.C. Hockey Canada Announces Ban on Body-Checking in Peewee Hockey. 2013. Available online: https://sportmedbc.com/news/hockey-canada-announces-ban-body-checking-peewee-hockey (accessed on 16 April 2018).
- Lacny, S.; Marshall, D.A.; Currie, G.; Kulin, N.A.; Meeuwisse, W.H.; Kang, J.; Emery, C.A. Reality check: The cost–effectiveness of removing body checking from youth ice hockey. Br. J. Sports Med. 2014, 48, 1299–1305. [Google Scholar] [CrossRef] [PubMed]
- Emery, C.; Palacios-Derflingher, L.; Black, A.M.; Eliason, P.; Krolikowski, M.; Spencer, N.; Kozak, S.; Schneider, K.J.; Babul, S.; Mrazik, M.; et al. Does disallowing body checking in non-elite 13- to 14-year-old ice hockey leagues reduce rates of injury and concussion? A cohort study in two Canadian provinces. Br. J. Sports Med. 2020, 54, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Kumar, B.; Vijayaraghavan, T.; Willaert, X.; Cuthbertson, B. Cost-effectiveness analysis should be mandatory in clinical-effectiveness research. Can. Med. Assoc. J. 2019, 191, E1140. [Google Scholar]
- Krahn, M.; Bryan, S.; Lee, K.; Neumann, P.J. Embracing the science of value in health. Can. Med. Assoc. J. 2019, 191, E733–E736. [Google Scholar] [CrossRef] [PubMed]
- Husereau, D.; Drummond, M.; Petrou, S.; Carswell, C.; Moher, D.; Greenberg, D.; Augustovski, F.; Briggs, A.H.; Mauskopf, J.; Loder, E.; et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMJ 2013, 346, f1049. [Google Scholar] [CrossRef] [PubMed]
- Alberta Health, Medical Price List as of 1 April 2017. Available online: https://www.alberta.ca/fees-health-professionals.aspx#jumplinks-0 (accessed on 25 April 2018).
- Alberta Health, Interactive Health Data Application, Health Costing, Hospital Ambulatory Care Case Costs. Available online: http://www.ahw.gov.ab.ca/IHDA_Retrieval/selectCategory.do (accessed on 25 April 2018).
- Alberta Health, Interactive Drug Benefit List. 2018. Available online: https://www.ab.bluecross.ca/dbl/idbl_main1.php (accessed on 25 April 2018).
- Canadian Institute for Health Research, National Expediture Trends. Available online: https://www.cihi.ca/en/national-health-expenditure-trends (accessed on 21 May 2021).
- Currie, G.R.; Lee, R.; Black, A.M.; Palacios-Derflingher, L.; Hagel, B.E.; Emery, C.A.; Marshall, D.A. What is the impact of a national policy disallowing body checking in 11-12 year old ice hockey leagues? An economic evaluation alongside an Alberta cohort study. Sports Health 2021. [Google Scholar] [CrossRef] [PubMed]
| Perspective | Healthcare Resource Types |
|---|---|
| Public healthcare costs | General practitioner/family physician visits, paediatrician visits, sports medicine visits, orthopaedic surgeon visits, emergency department visits (physician billing and technical fees), neurologist, MRI, CT Scan, Ultrasounds, X-rays |
| Private healthcare costs | Chiropractor visits, physiotherapist visits, massage therapist visits, athletic therapist visits, casts, braces, splints, crutches, over-the-counter and prescribed medication |
| Total healthcare costs | public healthcare system + private healthcare costs |
| Outcome | No Body Checking | Body Checking |
|---|---|---|
| Number of Teams | 33 | 49 |
| Number of players | 396 | 608 |
| Game participation hours | 12,393 | 23,374 |
| Number of injuries | 31 | 129 |
| No Body Checking | Body Checking | ||
|---|---|---|---|
| n = 396 | n = 608 | ||
| Sex, n (%) | Male | 390 (98) | 597 (98) |
| Female | 6 (2) | 11 (2) | |
| Missing data | 0 (0) | 0 (0) | |
| Height, mean (SD) cm | 165.7 (10) | 164.90 (10) | |
| Missing data, n (%) | 86 (22) | 109 (18) | |
| Weight, mean (SD) kg | 55.6 (14) | 54.2 (12) | |
| Missing data, n (%) | 108 (27) | 129 (21) | |
| Year of play, n (%) | First | 195 (49) | 329 (54) |
| Second | 169 (43) | 254 (43) | |
| Missing data | 32 (8) | 25 (3) | |
| Position, n (%) | Forward | 195 (49) | 325 (54) |
| Defence | 103 (26) | 176 (29) | |
| Goalie | 28 (7) | 50 (8) | |
| Missing data | 70 (18) | 57 (9) | |
| Previous injury, n (%) * | No | 276 (70) | 432 (71) |
| Yes | 72 (18) | 139 (23) | |
| Missing data | 48 (12) | 37 (6) | |
| Previous concussion n (%) ° | No | 252 (64) | 403 (66) |
| Yes | 129 (33) | 190 (31) | |
| Missing data | 15 (4) | 15 (2) | |
| No Body Checking (n = 396) | Body Checking (n = 608) | |
|---|---|---|
| Public healthcare | Costs (2017, $C °) | Costs (2017, $C °) |
| Visits | $5278 | $25,041 |
| Imaging | $2665 | $14,188 |
| Casting | $0 | $655 |
| Total public healthcare costs | $7943 | $39,884 |
| Private healthcare | ||
| Visits | $1015 | $2968 |
| Treatments | $240 | $435 |
| Medication | $5 | $51 |
| Ambulance out-of-pocket fee | $385 | |
| Total private healthcare costs | $1645 | $3454 |
| Total public and private healthcare costs | $9588 | $43,338 |
| No Body Checking | Body Checking | Difference (No Body Checking Minus Body Checking) | |
|---|---|---|---|
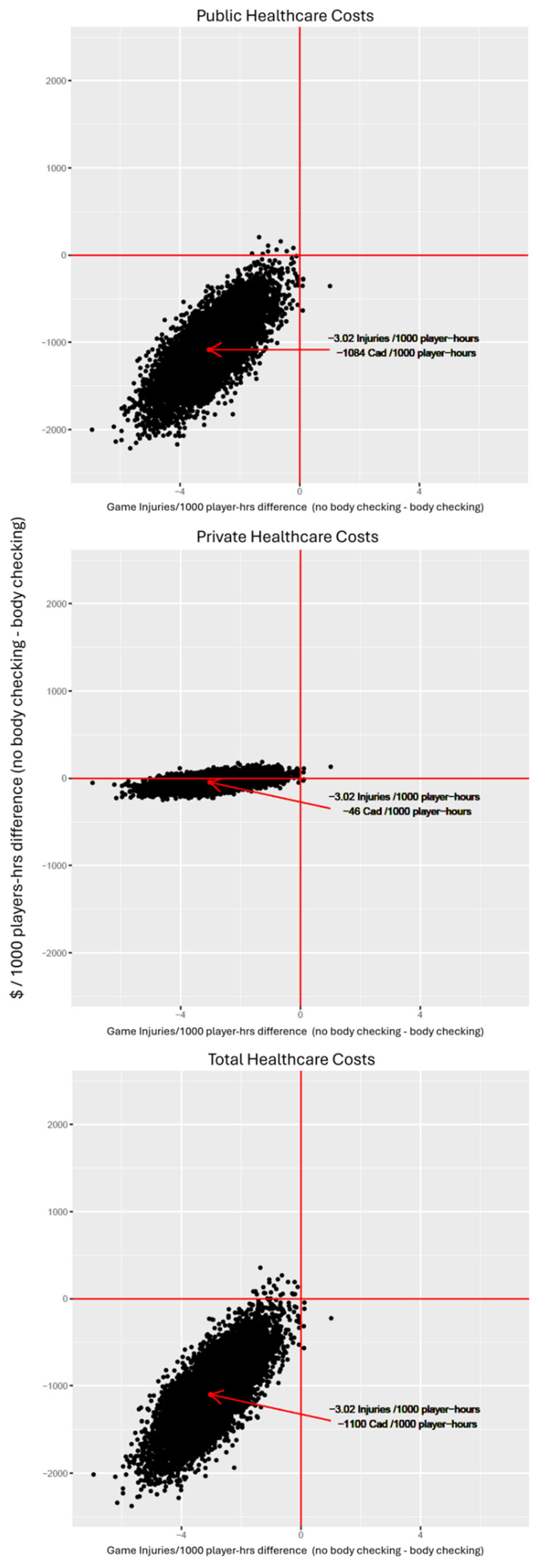
| Injury rate (per 1000 player hours) [95% CI] * | 2.50 [0.20, 4.80] | 5.52 [3.03, 8.01] | −3.02 [−4.01, −1.35] |
| Base Case: Public Healthcare Perspective | |||
| Cost (per 1000 player-hours) [95% CI] | $641 [$ 266, $ 1095] | $ 1725 [$ 1207, $ 2201] | $ −1084 [$ −1716, $ −416] |
| Scenario Analysis: Private Healthcare Perspective | |||
| Cost (per 1000 player hours) [95% CI] | $ 102 [$ 25, $ 190] | $ 148 [$ 75, $ 224] | $ −46 [$ −156, $ 70] |
| Scenario Analysis: Public and Private Healthcare Perspective | |||
| Cost (per 1000 player hours) [95% CI] | $ 774 [$ 332, $ 1308] | $ 1874 [$ 1324, $ 2412] | −$ 1100 [$ −1804, $ −346] |
| Alberta Projection * | |
|---|---|
| Public healthcare costs | $ −187,364 (95% CI $ −296,617, $ −71,903) |
| Private healthcare costs | $ −7972 (95% CI $ −26,965, $12,037) |
| Total healthcare costs | $ −190,188 (95% CI $ −311,798, $ −59,761) |
| Canadian Projection * | |
| Public healthcare costs | $ −1,602,397 (95% CI $ −2,536,769, $ −614,936) |
| Private healthcare costs | $ −68,183 (95% CI $ −230,614, $102,940) |
| Total healthcare costs | $ −1,626,554 (95% CI $ −2,666,602, $ −511,084) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Currie, G.R.; Lee, R.; Palacios-Derflingher, L.; Hagel, B.; Black, A.M.; Babul, S.; Mrazik, M.; Marshall, D.A.; Emery, C.A. Reality Check 2: The Cost-Effectiveness of Policy Disallowing Body Checking in Non-Elite 13- to 14-Year-Old Ice Hockey Players. Int. J. Environ. Res. Public Health 2021, 18, 6322. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18126322
Currie GR, Lee R, Palacios-Derflingher L, Hagel B, Black AM, Babul S, Mrazik M, Marshall DA, Emery CA. Reality Check 2: The Cost-Effectiveness of Policy Disallowing Body Checking in Non-Elite 13- to 14-Year-Old Ice Hockey Players. International Journal of Environmental Research and Public Health. 2021; 18(12):6322. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18126322
Chicago/Turabian StyleCurrie, Gillian R., Raymond Lee, Luz Palacios-Derflingher, Brent Hagel, Amanda M. Black, Shelina Babul, Martin Mrazik, Deborah A. Marshall, and Carolyn A. Emery. 2021. "Reality Check 2: The Cost-Effectiveness of Policy Disallowing Body Checking in Non-Elite 13- to 14-Year-Old Ice Hockey Players" International Journal of Environmental Research and Public Health 18, no. 12: 6322. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18126322





