Nurse-Coordinated Blood Pressure Telemonitoring for Urban Hypertensive Patients: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Literature Search and Identification of Eligible Studies
2.2. Inclusion and Exclusion Criteria
2.3. Study Selection
2.4. Outcomes
2.5. Data Extraction and Coding
2.6. Quality Assessment
2.7. Quantitative Data Synthesis
3. Results
3.1. Study Characteristics
3.2. Assessment of Risk of Bias
3.3. Primary Outcomes
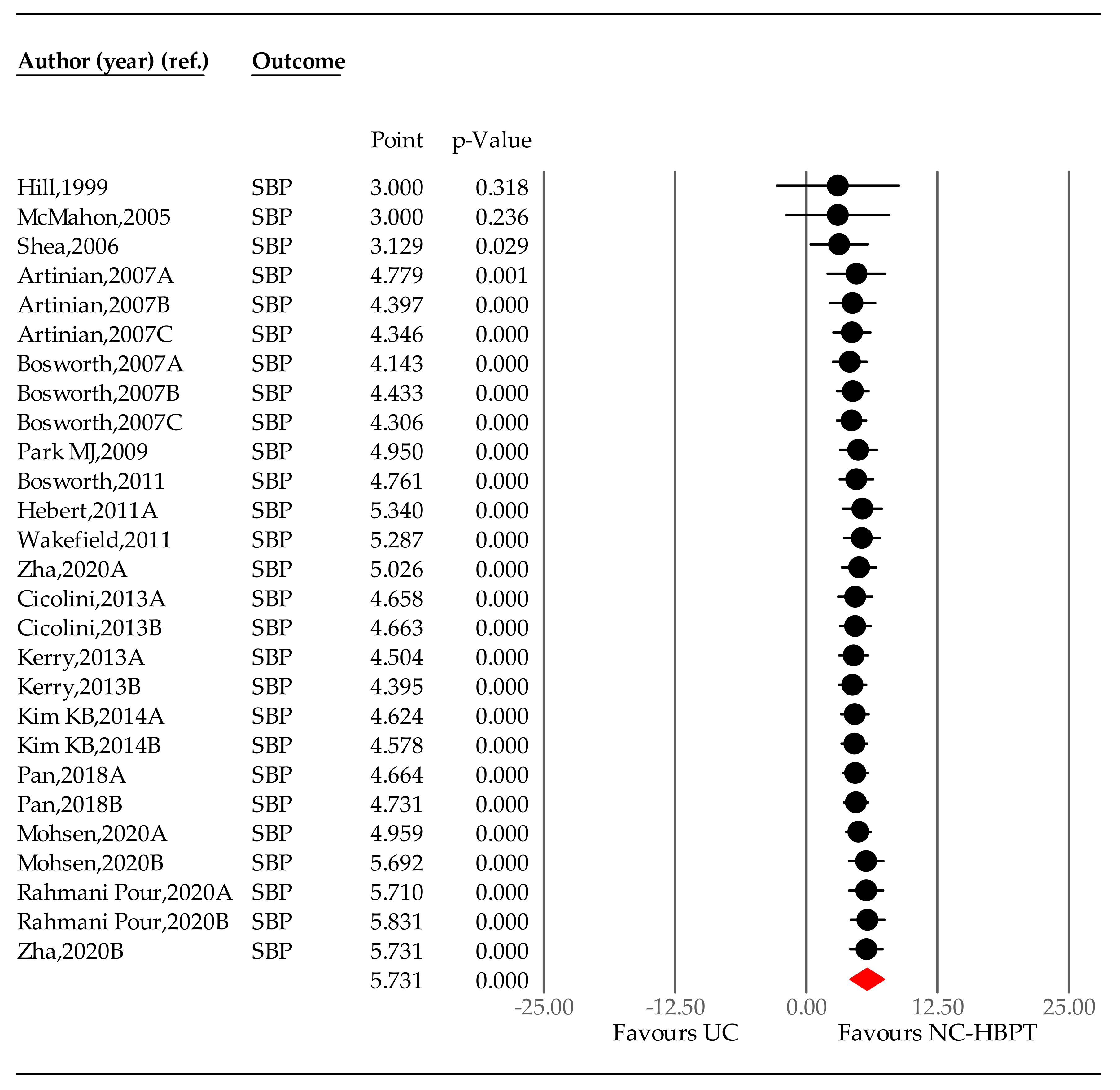
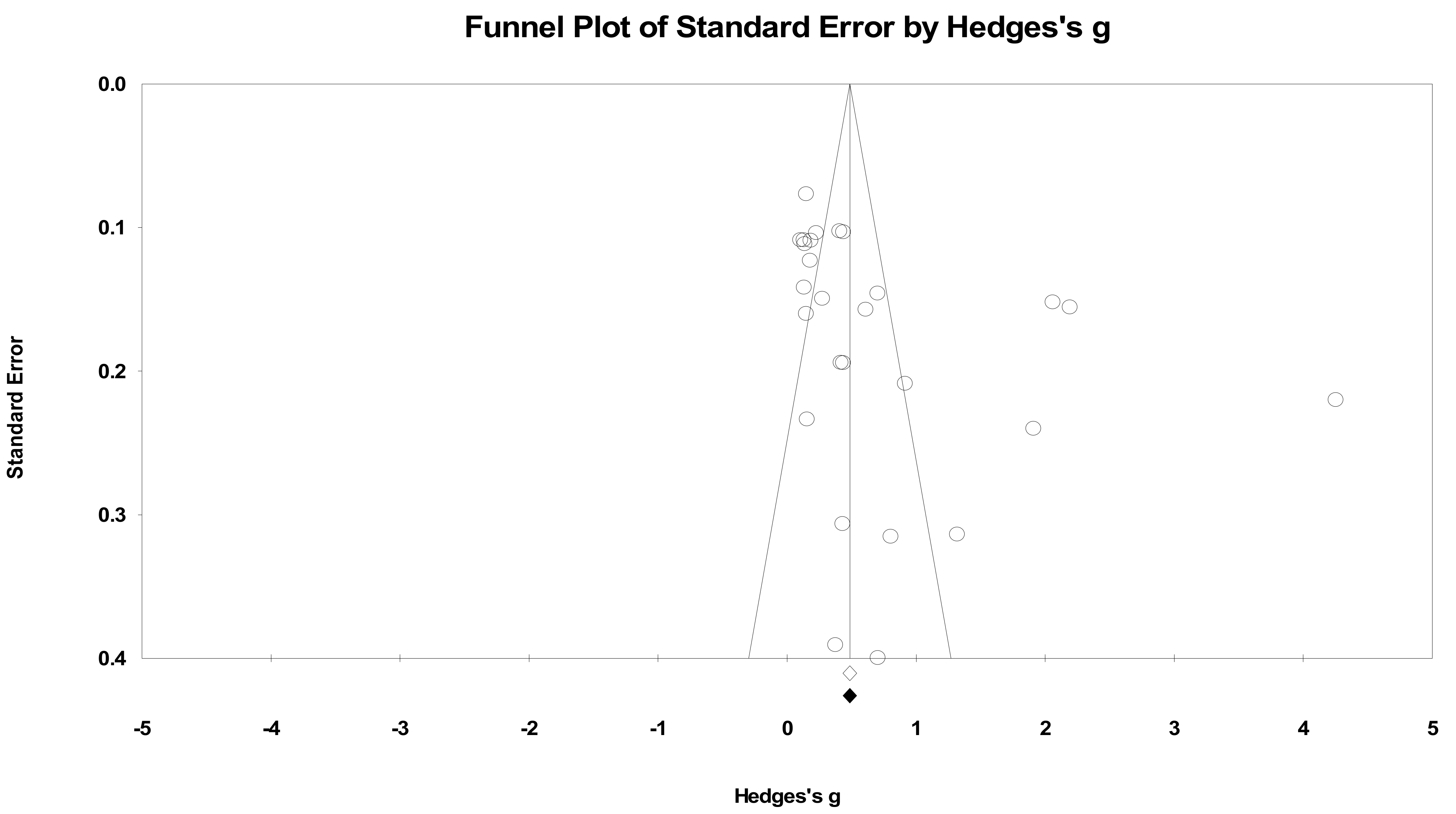
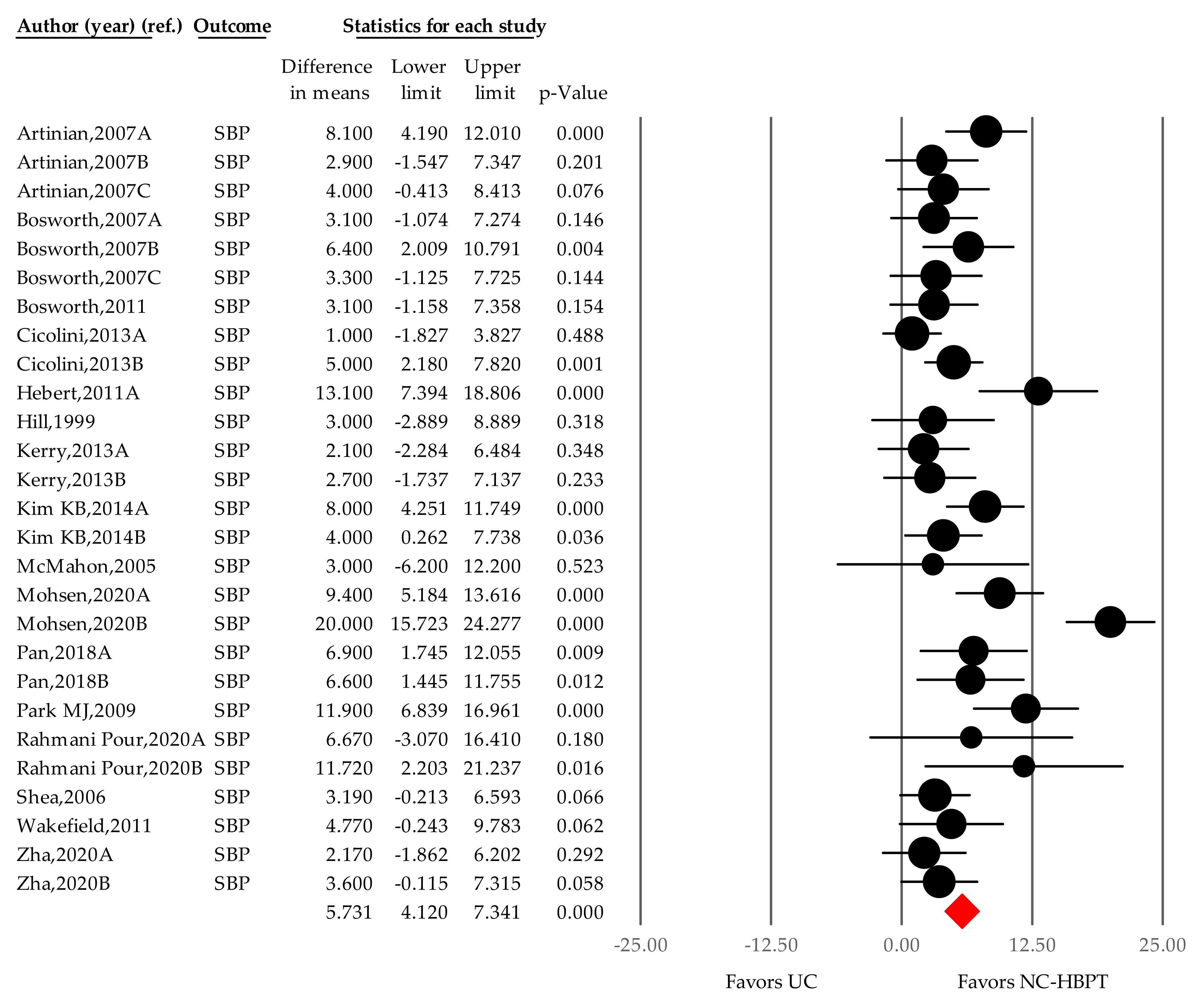
3.3.1. SBP Changes by Nurse-Coordinated HBPT
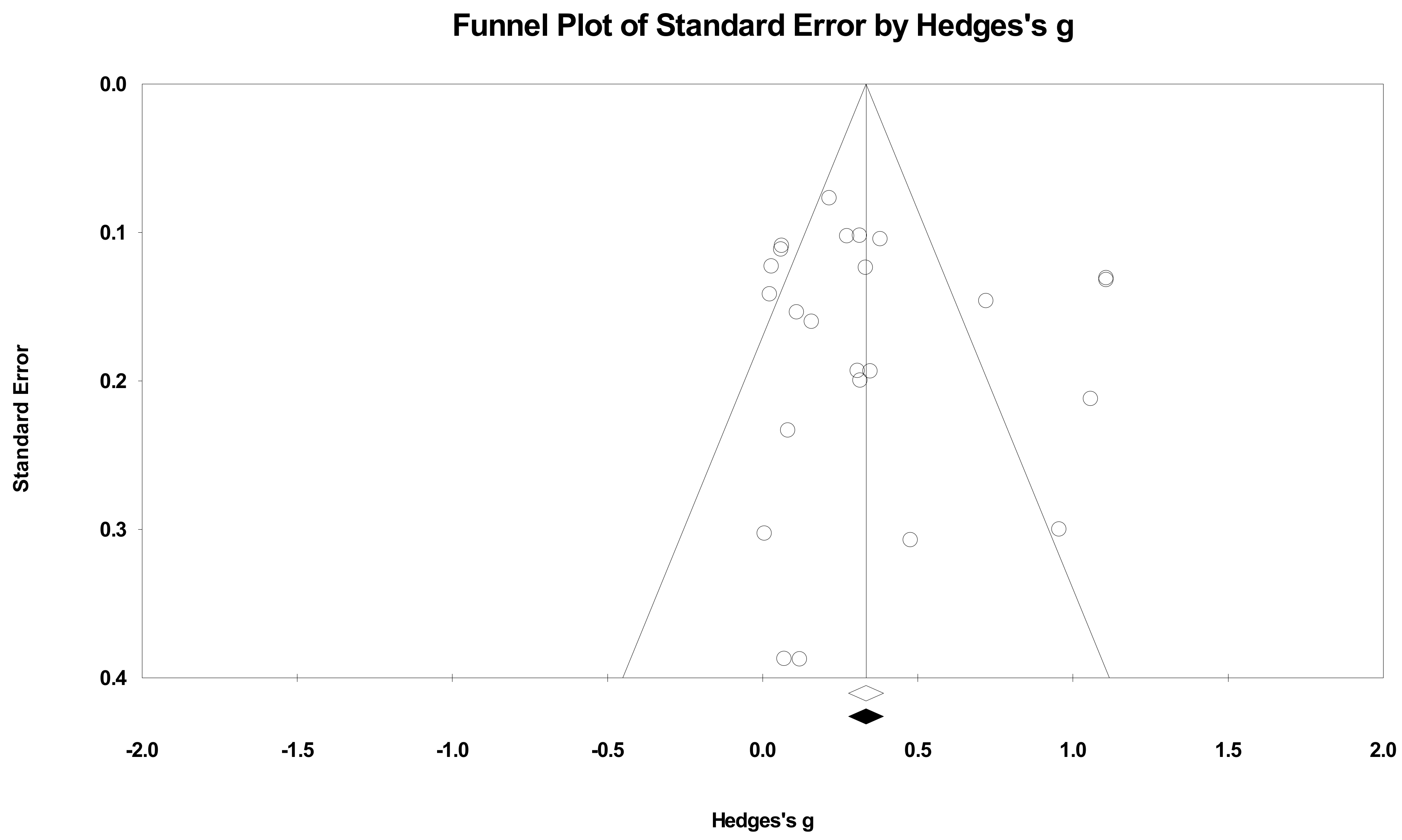
3.3.2. DBP Changes by Nurse-Led Coordination
3.4. Secondary Outcomes
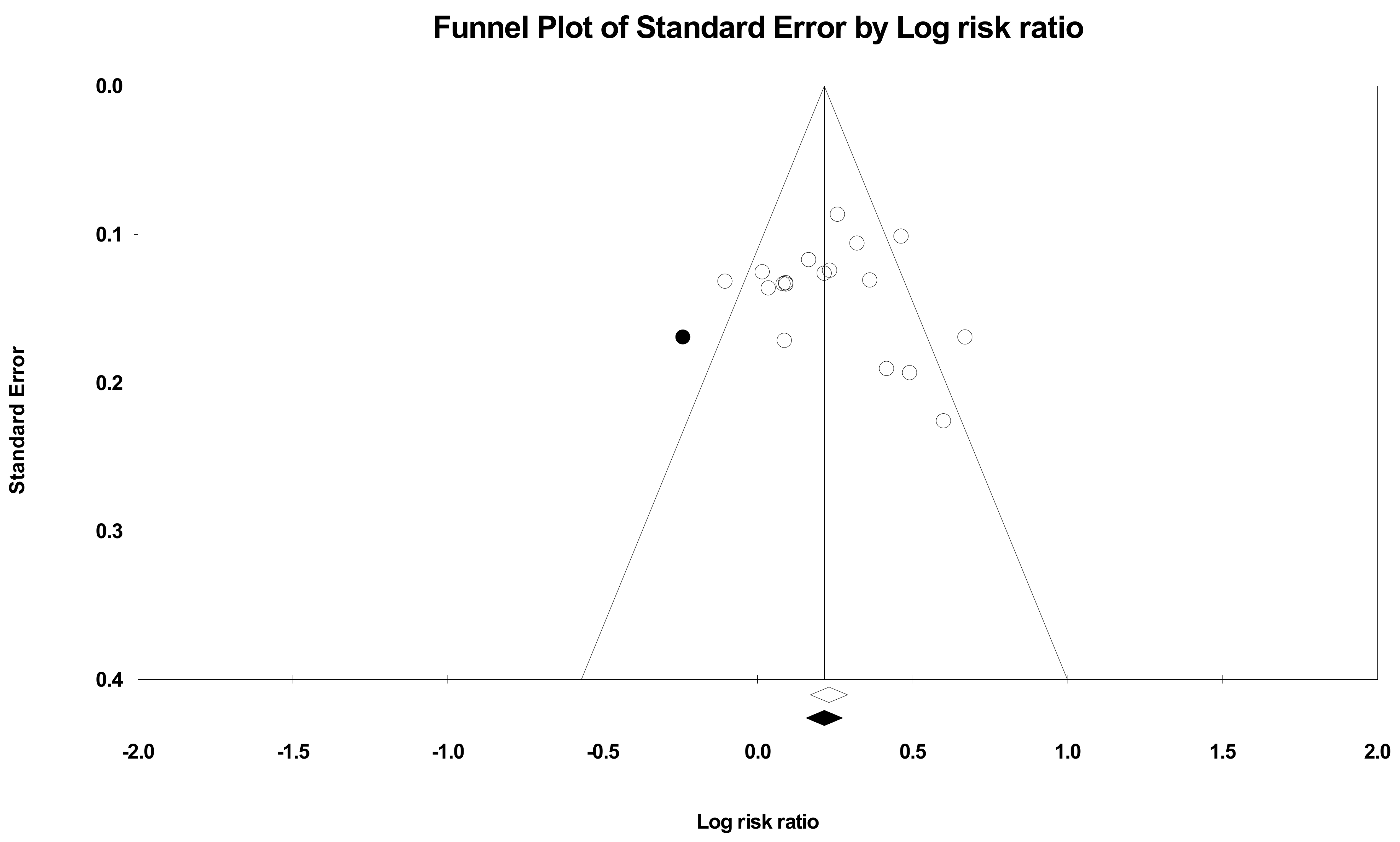
Rate of Reaching the Target Office Blood Pressure
3.5. Subgroup Analysis
3.5.1. Size of City
3.5.2. Setting
3.5.3. Duration
3.5.4. Coordinator’s Profession
3.5.5. Medically Underserved Area
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Appendix A. Searching Formula
Appendix B. Cumulative Meta-Analysis Presenting the Summative Effect at Each Time Point
Appendix C. Subgroup Analysis
| Category | Number of Studies | Summary WMD of SBP, mmHg (95% CI) | Heterogeneity, I2 (%) by FEM | p-Value of I2 |
|---|---|---|---|---|
| Overall | 27 | 5731 | 71.717 | p < 0.001 |
| City size (population) | ||||
| Under 1 million | 16 | 4.134 (2.275–5.992) | 7.934 | p = 0.063 |
| Over 1 million | 11 | 8.355 (5.937–10.773) | 82.533 | p < 0.001 |
| Setting | ||||
| Primary care clinic | 5 | 3.793 (0.450–7.136) | 0.000 | p = 0.086 |
| Community health center | 9 | 4.353 (1.877–6.829) | 34.921 | p = 0.039 |
| Hospital | 13 | 7.781 (5.483–10.079) | 79.627 | p < 0.001 |
| Duration (month) | ||||
| 3 or less | 8 | 6.694 (3.644–9.744) | 72.511 | p = 0.001 |
| 6 | 8 | 6.608 (3.771–9.444) | 85.761 | p < 0.001 |
| 12 | 9 | 3.573 (0.796–6.349) | 12.877 | P = 0.042 |
| Medically underserved area | ||||
| Not underserved | 17 | 6.150 (4.041–8.259) | 78.192 | p < 0.001 |
| Underserved | 10 | 4.424 (2.484–7.717) | 49.707 | p = 0.036 |
| Collaboration with other professionals | ||||
| No (Nurse-alone) | 20 | 6.132 | 78.074 | p < 0.001 |
| Yes | 7 | 4.465 | 75.373 | p = 0.633 |
References
- WHO. Hypertension. Available online: https://www.who.int/news-room/fact-sheets/detail/hypertension (accessed on 27 May 2021).
- Ostchega, Y.; Fryar, C.D.; Nwankwo, T.; Nguyen, D.T. Hypertension Prevalence Among Adults Aged 18 and Over: United States, 2017–2018. NCHS Data Brief, No 364; National Center for Health Statistics: Hyattsville, MD, USA, 2020. [Google Scholar]
- Clark, C.E.; Smith, L.F.P.; Taylor, R.S.; Campbell, J.L. Nurse-led interventions to improve control of blood pressure in people with hypertension: Systematic review and meta-analysis. BMJ 2010, 341. [Google Scholar] [CrossRef] [Green Version]
- Egan, B.M.; Li, J.; Hutchison, F.N.; Ferdinand, K.C. Hypertension in the United States, 1999 to 2012: Progress toward Healthy People 2020 goals. Circulation 2014, 130, 1692–1699. [Google Scholar] [CrossRef] [Green Version]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.L., Jr.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright, J.T., Jr.; et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003, 42, 1206–1252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task, F. Hypertension 2018, 71, 1269–1324. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Rosei, E.A.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Omboni, S.; McManus, R.J.; Bosworth, H.B.; Chappell, L.C.; Green, B.B.; Kario, K.; Logan, A.G.; Magid, D.J.; Mckinstry, B.; Margolis, K.L.; et al. Evidence and Recommendations on the Use of Telemedicine for the Management of Arterial Hypertension. Hypertension 2020, 76, 1368–1383. [Google Scholar] [CrossRef]
- Wilkins, A. Local response in health emergencies: Key considerations for addressing the COVID-19 pandemic in informal urban settlements. Env. Urban. 2020, 32, 503–522. [Google Scholar] [CrossRef]
- Sharma, A.; Ahmed, S.; Kaur, J.; Chawla, R.; Rejeeth, C. Exploring status of emergency drugs and vaccine development in Covid-19 pandemic: An update. VirusDisease 2021, 1–13. [Google Scholar] [CrossRef]
- World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. 2020. Available online: https://covid19.who.int/ (accessed on 27 May 2021).
- Bello, B.; Usehv, U. COVID-19: Are Non-Communicable Diseases Risk Factors for Its Severity? Am. J. Health Promot. 2021, 35, 720–729. [Google Scholar] [CrossRef]
- Miner, H.; Fatehi, A.; Ring, D.; Reichenberg, J.S. Clinician Telemedicine Perceptions During the COVID-19 Pandemic. Telemed. e-Health 2021, 27. [Google Scholar] [CrossRef] [PubMed]
- Ing, E.B.; Xu, Q.; Salimi, A.; Torun, N. Physician deaths from corona virus (COVID-19) disease. Occup. Med. 2020, 70, 370–374. [Google Scholar] [CrossRef]
- Phillips, L.S.; Branch, W.T.; Cook, C.B.; Doyle, J.P.; El Kebbi, I.M.; Gallina, D.L.; Miller, C.D.; Zeimer, D.C.; Barnes, C.S. Clinical inertia. Ann. Intern. Med. 2001, 135, 825–834. [Google Scholar] [CrossRef]
- Monahan, M.; Jowett, S.; Nickless, A.; Frassen, M.; Grant, S.; Greenfield, S.; Hobbs, F.D.R.; Hodgkinson, J.; Mant, J.; McManus, R. Cost-Effectiveness of Telemonitoring and Self-Monitoring of Blood Pressure for Antihypertensive Titration in Primary Care (TASMINH4). Hypertension 2019, 73, 1231–1239. [Google Scholar] [CrossRef] [PubMed]
- Omboni, S.; Guarda, A. Impact of Home Blood Pressure Telemonitoring and Blood Pressure Control: A Meta-Analysis of Randomized Controlled Studies. Am. J. Hypertens. 2011, 24, 989–998. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Filho, S.P.; Paffer, M.T.; Paffer, P.T.; Figeuiredo, M.C.; Veras, C.O.; Fonsêca, F.B. Home blood pressure monitoring: Report of a database of 1474 patients. J. Hypertens. 2021, 39, e121–e122. [Google Scholar] [CrossRef]
- Clark, C.E.; Horvath, I.A.; Taylor, R.S.; Campbell, J.L. Doctors record higher blood pressures than nurses: Systematic review and meta-analysis. Br. J. Gen. Pract. 2014, 64, e223–e232. [Google Scholar] [CrossRef] [Green Version]
- Cicolini, G.; Simonetti, V.; Comparcini, D.; Celiberti, I.; Nicola, M.D.; Capasso, L.M.; Flacco, M.E.; Bucci, M.; Mezzetti, A.; Manzoli, L. Efficacy of a nurse-led email reminder program for cardiovascular prevention risk reduction in hypertensive patients: A randomized controlled trial. Int J. Nurs. Stud. 2014, 51, 833–843. [Google Scholar] [CrossRef]
- Mohsen, M.M.; Riad, N.A.; Badawy, A.E.; Abd El Gafar, S.E.; Abd El-Hammed, B.M.; Eltomy, E.M. Tele-nursing versus Routine Outpatient Teaching for Improving Arterial Blood Pressure and Body Mass Index for Hypertensive Patients. Am. J. Nurs. Res. 2020, 8, 18–26. [Google Scholar]
- Hebert, P.; Sisk, J.E.; Tuzzio, L.; Casabianca, J.M.; Pogue, V.A.; Wang, J.J.; Chen, Y.; Cowles, C.; McLaughlin, M.A. Nurse-led disease management for hypertension control in a diverse urban community: A randomized trial. J. Gen. Intern. Med. 2012, 27, 630–639. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hill, M.N.; Bone, L.R.; Hilton, S.C.; Roary, M.C.; Kelen, G.D.; Levine, D.M. A clinical trial to improve high blood pressure care in young urban black men: Recruitment, follow-up, and outcomes. Am. J. Hypertens. 1999, 12, 548–554. [Google Scholar] [CrossRef] [Green Version]
- McMahon, G.T.; Gomes, H.E.; Hickson Hohne, S.; Hu, T.M.; Levine, B.A.; Conlin, P.R. Web-based care management in patients with poorly controlled diabetes. Diabetes Care 2005, 28, 1624–1629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Artinian, N.T.; Flack, J.M.; Nordstrom, C.K.; Hockman, E.M.; Washington, O.G.M.; Jen, K.C.; Fathy, M. Effects of nurse-managed telemonitoring on blood pressure at 12-month follow-up among urban African Americans. Nurs. Res. 2007, 56, 312–322. [Google Scholar] [CrossRef]
- Bosworth, H.B.; Olsen, M.K.; McCant, F.; Harrelson, M.; Gentry, P.; Rose, C.; Goldstein, M.K.; Hoffman, B.B.; Powers, B.; Oddone, E.Z. Hypertension Intervention Nurse Telemedicine Study (HINTS): Testing a multifactorial tailored behavioral/educational and a medication management intervention for blood pressure control. Am. Heart J. 2007, 153, 918–924. [Google Scholar]
- Laurant, M.; Reeves, D.; Hermens, R.; Braspenning, J.; Grol, R.; Sibbald, B. Substitution of doctors by nurses in primary care. Cochrane Database Syst. Rev. 2005, CD001271. [Google Scholar] [CrossRef]
- Fahey, T.; Schroeder, K.; Ebrahim, S.; Glynn, L. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst. Rev. 2010, CD005182. [Google Scholar] [CrossRef]
- McManus, R.; Mant, J.; Franssen, M.; Nickless, A.; Schwartz, C.; Hodgkinson, J.; Bradburn, P.; Farmer, A.; Grant, S.; Greenfield, S.; et al. Telemonitoring and/or self-monitoring of blood pressure in hypertension (TASMINH4): A randomised controlled trial. J. Hypertens. 2018, 36, e5. [Google Scholar] [CrossRef]
- Glynn, L.G.; Murphy, A.W.; Smith, S.M.; Schroeder, K.; Fahey, T. Self-monitoring and other non-pharmacological interventions to improve the management of hypertension in primary care: A systematic review. Br. J. Gen. Pract. 2010, 60, e476–e488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Omboni, S.; Gazzola, T.; Carabelli, G.; Parati, G. Clinical usefulness and cost effectiveness of home blood pressure telemonitoring: Meta-analysis of randomized controlled studies. J. Hypertens. 2013, 31, 455–468. [Google Scholar] [CrossRef]
- Duan, Y.; Xie, Z.; Dong, F.; Wu, Z.; Lin, Z.; Sun, N.; Xu, J. Effectiveness of home blood pressure telemonitoring: A systematic review and meta-analysis of randomised controlled studies. J. Hum. Hypertens. 2017, 31, 427–437. [Google Scholar] [CrossRef]
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.; Thomas, J. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, ED000142. [Google Scholar] [CrossRef] [Green Version]
- Choi, W.S.; Kim, N.S.; Kim, A.Y.; Woo, H. A Systematic Review and Meta-Analysis of Nurse-Coordinated Blood Pressure Telemonitoring for Urban Hypertensive Patients During the Covid-19 Era. PROSPERO. 2020, p. CRD42020222789. Available online: https://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42020222789 (accessed on 30 April 2020).
- Kerry, S.M.; Markus, H.S.; Khong, T.K.; Cloud, G.C.; Tulloch, J.; Coster, D.; Ibison, J.; Oakeshott, P. Home blood pressure monitoring with nurse-led telephone support among patients with hypertension and a history of stroke: A community-based randomized controlled trial. CMAJ 2013, 185, 23–31. [Google Scholar] [CrossRef] [Green Version]
- Kim, K.B.; Han, H.R.; Huh, B.; Nguyen, T.; Lee, H.; Kim, M.T. The effect of a community-based self-help multimodal behavioral intervention in Korean American seniors with high blood pressure. Am. J. Hypertens. 2014, 27, 1199–1208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pan, F.; Wu, H.; Liu, C.; Zhang, X.; Peng, W.; Wei, X.; Gao, W. Effects of home telemonitoring on the control of high blood pressure: A randomised control trial in the Fangzhuang Community Health Center, Beijing. Aust. J. Prim. Health 2018, 24, 398–403. [Google Scholar] [CrossRef] [PubMed]
- Pour, R.E.; Aliyari, S.; Farsi, Z.; Ghelich, Y. Comparing the effects of interactive and noninteractive education using short message service on treatment adherence and blood pressure among patients with hypertension. Nurs. Midwifery Stud. 2020, 9, 68–76. [Google Scholar]
- Zha, P.; Qureshi, R.; Porter, S.; Chao, Y.Y.; Pacquiao, D.; Chase, S.; O’Brien-Richardson, P. Utilizing a Mobile Health Intervention to Manage Hypertension in an Underserved Community. West. J. Nurs. Res. 2020, 42, 201–209. [Google Scholar] [CrossRef]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.; Rothstein, H.R. Introduction to Meta-Analysis; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Review Manager (RevMan) [Computer program]. Version 5.4. The Cochrane Collaboration, 2020.
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1988. [Google Scholar]
- Borenstein, M.; Hedges, L.; Higgins, J.; Rothstein, H. Comprehensive Meta-Analysis, Version 2; 104; Biostat: Englewood, NJ, USA, 2005. [Google Scholar]
- Bosworth, H.B.; Powers, B.J.; Olsen, M.K.; McCant, F.; Grubber, J.; Smith, V.; Gentry, P.W.; Rose, C.; Van Houtven, C.; Wang, V.; et al. Home blood pressure management and improved blood pressure control: Results from a randomized controlled trial. Arch. Intern. Med. 2011, 171, 1173–1180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, M.; Kim, H.; Kim, K. Cellular phone and Internet-based individual intervention on blood pressure and obesity in obese patients with hypertension. Int. J. Med. Inform. 2009, 78, 704–710. [Google Scholar] [CrossRef] [PubMed]
- Shea, S.; Weinstock, R.S.; Starren, J.; Teresi, J.; Palmas, W.; Field, L.; Morin, P.; Goland, R.; Izquierdo, R.E.; Wolff, T.; et al. A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus. J. Am. Med. Inform. Assoc. 2006, 13, 40–51. [Google Scholar] [CrossRef]
- Wakefield, B.J.; Holman, J.E.; Ray, A.; Scherubel, M.; Adams, M.R.; Hillis, S.L.; Rosenthal, G.E. Effectiveness of home telehealth in comorbid diabetes and hypertension: A randomized, controlled trial. Telemed. e-Health 2011, 17, 254–261. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G.; Sterne, J.A.C. Assessing risk of bias in included studies. In Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 (Updated March 2011); Higgins, J.P.T., Green, S., Eds.; The Cochrane Collaboration, John Wiley & Sons: Chichester, UK, 2011; Available online: http//www.handbook.cochrane.org (accessed on 31 July 2019).
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. A Health Telematics Policy in Support of WHO’s Health-For-All Strategy for Global Health Development. Report of the WHO Group Consultation on Health Telematics, December 11–16, 1997; World Health Organization: Geneva, Switzerland, 1998. [Google Scholar]
- Chu, D.K.; Akl, E.A.; Duda, S.; Solo, K.; Yaacoub, S.; Schünemann, H.J. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet 2020, 395, 1973–1987. [Google Scholar] [CrossRef]
- Blood Pressure Lowering Treatment Trialists’ Collaboration. Blood pressure-lowering treatment based on cardiovascular risk: A meta-analysis of individual patient data. Lancet 2014, 384, 591–598. [Google Scholar] [CrossRef]
- Choi, W.S.; Choi, J.H.; Oh, J.; Shin, I.; Yang, J. Effects of Remote Monitoring of Blood Pressure in Management of Urban Hypertensive Patients: A Systematic Review and Meta-Analysis. Telemed. e-Health 2020, 26, 744–759. [Google Scholar] [CrossRef] [PubMed]
- Aas, I.H.M. Telemedical work and cooperation. J. Telemed. Telecare 2001, 7, 212–218. [Google Scholar] [CrossRef]
- Jacob, C.; Sanchez-Vazquez, A.; Ivory, C. Social, Organizational, and Technological Factors Impacting Clinicians’ Adoption of Mobile Health Tools: Systematic Literature Review. JMIR mHealth uHealth 2020, 8, e15935. Available online: https://preprints.jmir.org/preprint/15935 (accessed on 10 April 2020). [CrossRef] [Green Version]
- Palmas, W.; Teresi, J.; Morin, P.; Wolff, L.T.; Field, L.; Eimicke, J.P.; Capps, L.; Prigollini, A.; Orbe, I.; Weinstock, R.S.; et al. Recruitment and enrollment of rural and urban medically underserved elderly into a randomized trial of telemedicine case management for diabetes care. Telemed. e-Health 2006, 12, 601–607. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.C.; Thomas, E.; Snoswell, C.L.; Haydon, H.; Mehrotra, A.; Clemensen, J.; Caffery, L.J. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J. Telemed. Telecare 2020, 26, 309–313. [Google Scholar] [CrossRef] [Green Version]




| Study | Number of Subjects (UC vs. HBPT Group) | Inclusion Criteria | The Profession of Coordinator | Name of City (Country) | Size of Urban Population (Over 1,000,000) | Description of Intervention Pathway | Additional Support | Main Outcome Measures |
|---|---|---|---|---|---|---|---|---|
| Artinian 2007A [26] | 193/194 | African-American hypertensive patients | Trained registered nurse | Detroit (USA) | No (916,952 in 2007) | Telephonic transmission | Telecounseling call and patient education | Changes in office BP |
| Artinian 2007B [26] | 157/164 | African-American hypertensive patients | Trained registered nurse | Detroit (USA) | No (916,952 in 2007) | Telephonic transmission | Telecounseling call and patient education | Changes in office BP |
| Artinian 2007C [26] | 169/167 | African-American hypertensive patients | Trained registered nurse | Detroit (USA) | No (916,952 in 2007) | Telephonic transmission | Telecounseling call and patient education | Office BP changes |
| Bosworth 2007A [27] | 150/150 | Hypertensive patients who are using a BP-lowering medication with poor (inadequate) BP control | Intervention nurses | Durham (USA) | No (217,847 in 2007) | Home BP monitoring + Behavioral intervention | Tailored behavioral intervention | Improved rates of BP control |
| Bosworth 2007B [27] | 150/150 | Hypertensive patients who are using a BP-lowering medication with poor (inadequate) BP control | Intervention nurses supervised with a physician | Durham (USA) | No (217,847 in 2007) | Home BP monitoring + Medication management | Medication management with a validated decision support system (DSS) | Improved rates of BP control |
| Bosworth 2007C [27] | 150/150 | Hypertensive patients who are using a BP-lowering medication with poor (inadequate) BP control | Intervention nurses | Durham (USA) | No (217,847 in 2007) | Home BP monitoring + Combined intervention | Combined behavioral and medication management | Improved rates of BP control |
| Bosworth 2011 [46] | 137/127 | Treated hypertensive patients | Registered nurse | Durham (USA) | No (228,354 in 2010) | Telephonic transmission | Behavioral management | Change in BP control, SBP, and DBP |
| Cicolini 2013A [21] | 98/100 | Treated and untreated hypertensive patients | Registered nurse | Chieti (Italy) | No (51,484 in 2011) | Web-based | Email reminder and phone call | 1. Changes in BP2. BMI, alcohol consumption, cigarette smoking, adherence to therapy |
| Cicolini 2013B [21] | 98/100 | Treated and untreated hypertensive patients | Registered nurse | Chieti (Italy) | No (51,484 in 2011) | Web-based | Email reminder and phone call | 1. Changes in BP2. BMI, alcohol consumption, cigarette smoking, adherence to therapy |
| Hebert 2011A [23] | 83/85 | Uncontrolled hypertensive patients | Registered nurse | New York (USA) | Yes (8,174,959 in 2010) | Telephonic transmission | Information on the use of home BP monitor | BP reduction |
| Hill 1999 [24] | 77/78 | Black or African-American hypertensive young male resident within the Johns-Hopkins Hospital catchment area | Nurse-community health worker team (registered nurse and health worker team) | Baltimore (USA) | No (763.014 in 1990) | Telephonic transmission | Individualized counseling, monthly telephone call, and a home visit (educational-behavioral intervention) | Changes in office BP |
| Kerry 2012A [36] | 169/168 | Hypertensive patients with history of stroke or transient ischemic attack | Nurse | London (UK) | Yes (8,135,667 in 2011) | Telephonic transmission | Nurse-led telephone support | Reduction of SBP |
| Kerry 2012B [36] | 169/168 | Hypertensive patients with history of stroke or transient ischemic attack | Nurse | London (UK) | Yes (8,135,667 in 2011) | Telephonic transmission | Nurse-led telephone support | Reduction of SBP |
| Kim KB 2014A [37] | 192/191 | Uncontrolled Korean-American hypertensive seniors | Bilingual RNs and nutritionist | Ellicott City (USA) | No (68,507 in 2014) | Web-based | 2 h weekly education and training for 6 weeks and monthly telephone counseling | Changes in SBP and DBP |
| Kim KB 2014B [37] | 187/185 | Uncontrolled Korean-American hypertensive seniors | Bilingual RNs and nutritionist | Ellicott City (USA) | No (68,507 in 2014) | Web-based | 2 h weekly education and training for 6 weeks and monthly telephone counseling | Changes in SBP and DBP |
| McMahon 2005 [25] | 35/37 | Poorly controlled diabetics and hypertensive patients | Advanced practice nurse and certified diabetes educator | Boston (USA) | No (559,034 in 2005) | Web-based | Telephone to encourage website usage | Changes in HbA1c, BP, lipid profiles |
| Mohsen 2019A [22] | 50/50 | Hypertensive patients who are on antihypertensive medication | Staff nurse | Shibin El Kom (Egypt) | No (249,611 in 2018) | Telenursing | Follow-up phone calls | Reducing arterial blood pressure and patients’ anthropometric measurement |
| Mohsen 2019B [22] | 50/50 | Hypertensive patients who are on antihypertensive medication | Staff nurse | Shibin El Kom (Egypt) | No (249,611 in 2018) | Telenursing | Follow-up phone calls | Reducing arterial blood pressure and patients’ anthropometric measurement |
| Pan 2018A [38] | 55/52 | Hypertensive patients with uncontrolled BP | GP, a hypertensionspecialist, a general nurse, an information manager | Beijing (China) | Yes (19,612,368 in 2010) | Smartphone application | Follow-up phone calls | The reduction in systolic blood pressure |
| Pan 2018B [38] | 55/52 | Hypertensive patients with uncontrolled BP | GP, a hypertensionspecialist, a general nurse, an information manager | Beijing (China) | Yes (19,612,368 in 2010) | Smartphone application | Follow-up phone calls | The reduction in systolic blood pressure |
| Park MJ 2009 [47] | 21/28 | Obese hypertensive patients | Registered nurse | Seoul (S. Korea) | Yes (10,208,302 in 2009) | Mobile or internet transmission | Short message service by cellular phone and internet recommendation | Changes in BP, body weight, waist circumference, and serum lipid profile |
| Rahmani Pour 2019A [39] | 21/21 | Hypertensive patients, use of antihypertensive medications | Instructors of a faculty of nursing and midwifery and several cardiologists | Tehran (Iran) | Yes (8,693,706 in 2016) | Short message service | Communicate with the first author | Improved treatment adherence, no significant differences among the groups with respect to the baseline SBP and DBP |
| Rahmani Pour 2019A [39] | 21/21 | Hypertensive patients, use of antihypertensive medications | Instructors of a faculty of nursing and midwifery and several cardiologists | Tehran (Iran) | Yes (8,693,706 in 2016) | Non-ISMS | Follow-up | No significant differences among the groups with respect to the baseline SBP and DBP |
| Shea 2006 [48] | 347/333 | Diabetic hypertensive patients | Nurse case manager | New York (USA) | Yes (8,143,197 in 2005) | Telephone-linked web-enabled computer system | Web-based messaging | Changes in HbA1c, BP, and cholesterol level |
| Wakefield 2011 [49] | 97/83 | Type 2 diabetics and hypertensive patients | Registered nurse | Iowa City (USA) | No (68,036 in 2010) | Telephonic transmission | Telephonic transmission and nurse care management | Changes in HbA1c and SBP |
| Zha 2020A [40] | 13/12 | Underserved and vulnerable urban population on HTN medication with diagnosed uncontrolled hypertension | Two nurses in the community health center | Newark (USA) | No (281,764 in 2016) | Mobile Health (Smart phone or tablet) | Three training sessions | No significant change in systolic BP, the potential to facilitate hypertension management |
| Zha 2020B [40] | 13/12 | Underserved and vulnerable urban population on HTN medication with diagnosed uncontrolled hypertension | Two nurses in the community health center | Newark (USA) | No (281,764 in 2016) | Mobile Health (Smart phone or tablet) | Three training sessions | No significant change in systolic BP, the potential to facilitate hypertension management |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, W.-S.; Kim, N.-S.; Kim, A.-Y.; Woo, H.-S. Nurse-Coordinated Blood Pressure Telemonitoring for Urban Hypertensive Patients: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 6892. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18136892
Choi W-S, Kim N-S, Kim A-Y, Woo H-S. Nurse-Coordinated Blood Pressure Telemonitoring for Urban Hypertensive Patients: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2021; 18(13):6892. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18136892
Chicago/Turabian StyleChoi, Woo-Seok, Nam-Suk Kim, Ah-Young Kim, and Hyung-Soo Woo. 2021. "Nurse-Coordinated Blood Pressure Telemonitoring for Urban Hypertensive Patients: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 18, no. 13: 6892. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18136892







