The Effects of the Pilates Method on Pelvic Floor Injuries during Pregnancy and Childbirth: A Quasi-Experimental Study
Abstract
:1. Introduction
2. Materials and Methods
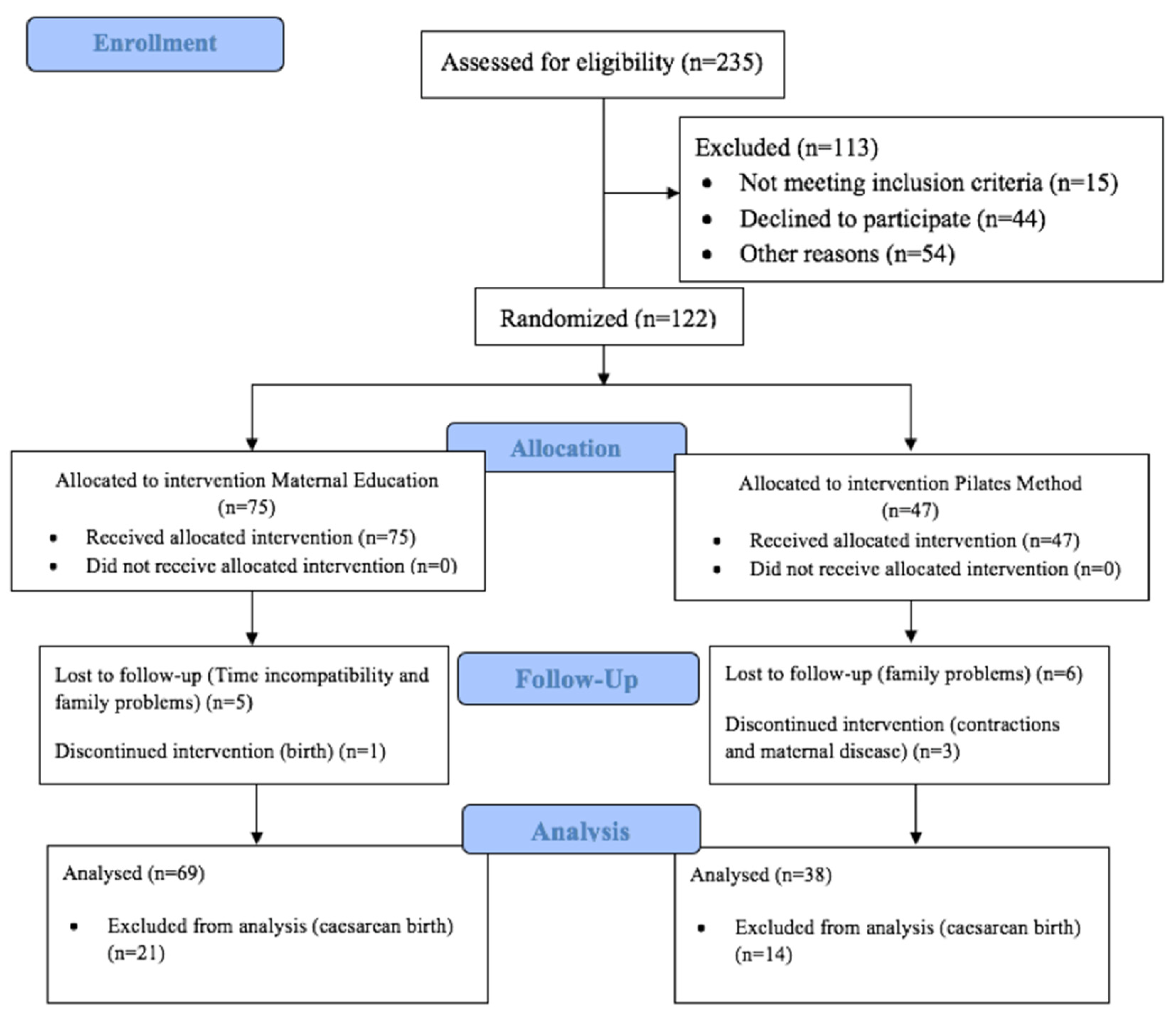
2.1. Study Design
2.2. Sample/Participants
2.2.1. Interventions
2.2.2. Experimental Group
2.2.3. Control Group
2.2.4. Sample Size
2.3. Data Collection
2.3.1. Outcomes
2.3.2. Validity and reliability/Rigor
2.3.3. Ethical Considerations
2.3.4. Data Analysis
3. Results
3.1. Characteristics of the Sample
3.2. Onset of Birth, Prevalence of Perineal Trauma and Predictive Variables
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Session 1 | Session 2 | Session 3 | Session 4 |
| Squats Pelvis tilt Quadrupled (arms only) The Cat The archer The mermaid Side leg lifts Clam Side kick Leg circle | Squats Pelvis tilt Quadrupled (legs only) Arm rotations The cat The archer The mermaid Side leg lifts Clam Side kick Leg circle | Squats Side leg lifts Quadrupled (arms and legs) Clam Side kick Leg circle Leg lifts Pelvic curl Roll-up/roll-down Tiger The mermaid | Squats Quadrupled (arms and legs) Push up on knees The Cat The archer The mermaid Side leg lifts botton leg Clam Side kick Pelvis tilt Leg lifts Roll-up/roll-down Leg circle Back support |
| Session 5 | Session 6 | Session 7 | Session 8 |
| Squats Quadrupled (arms and legs) Push up on knees The cat Saw The mermaid Side leg lifts botton leg Clam Side kick Leg lifts Roll-up/roll-down Leg circle Tiger Back support | Squats Working arms with tape Quadrupled (arms and legs) Push up on knees The cat Saw Pelvis tilt The mermaid Side two legs Clam Side kick Leg lifts Pelvic curl Roll-up/roll-down Leg circle Back support | Squats Working arms with tape Quadrupled (arms and legs) Push up on knees The Cat The archer Saw The mermaid Side two legs Clam Side kick Leg lifts Pelvic curl Roll-up/roll-down Back support Leg circle Tiger Hamstream extension | Squats Working arms with tape Quadrupled (arms and legs) Push up on knees The Cat The archer Saw The mermaid Side two legs Clam Side kick Leg lifts Pelvic curl Roll-up/roll-down Leg circle Hamstream extension Tiger Side kick kneeling Back support |
References
- Bozkurt, M.; Yumru, A.E.; Şahin, L. Pelvic floor dysfunction, and effects of pregnancy and mode of delivery on pelvic floor. Taiwan. J. Obstet. Gynecol. 2014, 53, 452–458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pierce, H.; Perry, L.; Gallagher, R.; Chiarelli, P. Pelvic floor health: A concept analysis. J. Adv. Nurs. 2015, 71, 991–1004. [Google Scholar] [CrossRef]
- Hyakutake, M.T.; Han, V.; Cundiff, G.W.; Baerg, L.; Koenig, N.A.; Lee, T.; Geoffrion, R. Pelvic Floor Health Education. Female Pelvic Med. Reconstr. Surg. 2016, 22, 336–339. [Google Scholar] [CrossRef]
- Neels, H.; Wyndaele, J.-J.; Tjalma, W.A.A.; De Wachter, S.; Wyndaele, M.; Vermandel, A. Knowledge of the pelvic floor in nulliparous women. J. Phys. Ther. Sci. 2016, 28, 1524–1533. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Howard, D.; Makhlouf, M. Can pelvic floor dysfunction after vaginal birth be prevented? Int. Urogynecol. J. 2016, 27, 1811–1815. [Google Scholar] [CrossRef]
- Leon-Larios, F.; Corrales-Gutierrez, I.; Casado-Mejía, R.; Suarez-Serrano, C. Influence of a pelvic floor training programme to prevent perineal trauma: A quasi-randomised controlled trial. Midwifery 2017, 50, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Bose, P.; Haxton, T.; Harding, C.; Lead, M.W. Episiotomy and Perineal Repair Guideline (GL836); Royal Berkshire NHS Foundation Trust: Reading, UK, 2017. [Google Scholar]
- Organización Mundial de la Salud. Cuidados en el parto normal: Una guía práctica. Rev. Hosp. Mat. Inf. Ramón Sardá. 1999, 18, 78–80. [Google Scholar]
- Escuriet, R.; Pueyo, M.J.; Perez-Botella, M.; Espada, X.; Salgado, I.; Gómez, A.; Biescas, H.; Espiga, I.; White, J.; Fernandez, R.; et al. Cross-sectional study comparing public and private hospitals in Catalonia: Is the practice of routine episiotomy changing? BMC Heal. Serv. Res. 2015, 15, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, L.A.; Price, N.; Simonite, V.; Burns, E.E. Incidence of and risk factors for perineal trauma: A prospective observational study. BMC Pregnancy Childbirth 2013, 13, 59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oblasser, C.; McCourt, C.; Hanzal, E.; Christie, J. Vibrating vaginal balls to improve pelvic floor muscle performance in women after childbirth: A protocol for a randomised controlled feasibility trial. J. Adv. Nurs. 2016, 72, 900–914. [Google Scholar] [CrossRef]
- Davidson, K.; Jacoby, S.; Brown, M.S. Prenatal Perineal Massage: Preventing Lacerations during Delivery. J. Obstet. Gynecol. Neonatal Nurs. 2000, 29, 474–479. [Google Scholar] [CrossRef] [PubMed]
- Kyvernitakis, I.; Köhler, C.; Schmidt, S.; Misselwitz, B.; Großmann, J.; Hadji, P.; Kalder, M. Impact of maternal body mass index on the cesarean delivery rate in Germany from 1990 to 2012. J. Périnat. Med. 2015, 43, 449–454. [Google Scholar] [CrossRef]
- Helen, L. The Effect of a Pilates Exercise Programme on Perceived Functional Disability and Pain Associated with Non-Specific Chronic Low Back Pain. MOJ Yoga Phys. Ther. 2017, 2. [Google Scholar] [CrossRef] [Green Version]
- Guzmán, P.; Díaz, A.M.; Gómez, D.; Guzmán RGuzmán, A. Actuación del fisioterapeuta en el tratamiento integral de la emba-razada. Nure Investig. 2013, 2, 1–8. [Google Scholar]
- Shaban, M.M.; Bassiouny, Y.A.; Elzahaby, I.M.; Hassan, A.A. Body mass index and labour outcome in Egyptian women. J. Obstet. Gynaecol. 2013, 34, 248–250. [Google Scholar] [CrossRef]
- Navarro, C.L.; Luján, M.I.S. Nuevos sistemas de comunicación del método Pilates en embarazo y puerperio = New communications systems of Pilates Method in pregnancy and postpartum period. Rev. Esp. Comun. Salud. 2017, 8, 20–28. [Google Scholar] [CrossRef] [Green Version]
- Almagiá, E. Influencia del estado emocional en la salud física. Terap. Psicol. 2003, 21, 38. [Google Scholar]
- Culligan, P.J.; Scherer, J.; Dyer, K.; Priestley, J.; Guingon-White, G.; DelVecchio, D.; Vangeli, M. A randomized clinical trial comparing pelvic floor muscle training to a Pilates exercise program for improving pelvic muscle strength. Int. Urogynecol. J. 2010, 21, 401–408. [Google Scholar] [CrossRef]
- Wells, C.; Kolt, G.; Bialocerkowski, A. Defining Pilates exercise: A systematic review. Complement. Ther. Med. 2012, 20, 253–262. [Google Scholar] [CrossRef]
- Oktaviani, I. Pilates workouts can reduce pain in pregnant women. Complement. Ther. Clin. Pract. 2018, 31, 349–351. [Google Scholar] [CrossRef] [PubMed]
- Dias, N.T.; Ferreira, L.R.; Fernandes, M.G.; Resende, A.P.M.; Pereira-Baldon, V.S. A Pilates exercise program with pelvic floor muscle contraction: Is it effective for pregnant women? A randomized controlled trial. Neurourol. Urodyn. 2018, 37, 379–384. [Google Scholar] [CrossRef] [PubMed]
- De Souza, L.M.; Pegorare, A.B.G.D.S.; Christofoletti, G.; Barbosa, S.R.M. Influence of a protocol of Pilates exercises on the contractility of the pelvic floor muscles of non-institutionalized elderly persons. Rev. Bras. Geriatr. Gerontol. 2017, 20, 484–492. [Google Scholar] [CrossRef] [Green Version]
- Aceituno, L.; Aguayo, J.; Arribas, L.; Caño, A.; Corona, I.; Martín, J.E.; Mora, M.A.; Ras, J.; Sánchez, T.; Sanz, R. Proceso Asistencial Integrado Embarazo, Parto y Puerperio, 3rd ed.; Consejería de Igualdad, Salud y Políticas Sociales: Sevilla, Spain, 2014; Available online: https://www.juntadeandalucia.es/export/drupaljda/salud_5af1956fa966b_embarazo_parto_puerperio_septiembre_2014.pdf (accessed on 17 June 2019).
- Rodríguez-Díaz, L.; Ruiz-Frutos, C.; Vázquez-Lara, J.M.; Ramírez-Rodrigo, J.; Villaverde-Gutiérrez, C.; Torres-Luque, G. Effectiveness of a physical activity programme based on the Pilates method in pregnancy and labour. Enfermería Clínica 2017, 27, 271–277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validi-ty. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aguiar, M.; Farley, A.; Hope, L.; Amin, A.; Shah, P.; Manaseki-Holland, S. Birth-Related Perineal Trauma in Low- and Middle-Income Countries: A Systematic Review and Meta-analysis. Matern. Child Health J. 2019, 23, 1048–1070. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Souza, J.C.; Monga, A.; Tincello, D.G. Risk factors for perineal trauma in the primiparous population during non-operative vaginal delivery. Int. Urogynecol. J. 2019, 31, 621–625. [Google Scholar] [CrossRef] [Green Version]
- Jiang, H.; Qian, X.; Carroli, G.; Garner, P. Selective versus routine use of episiotomy for vaginal birth. Cochrane Database Syst. Rev. 2017, 2, CD000081. [Google Scholar] [CrossRef] [Green Version]
- Jansson, M.H.; Nilsson, K.; Franzén, K. Development and validation of a protocol for documentation of obstetric perineal lacerations. Int. Urogynecol. J. 2019, 30, 2069–2076. [Google Scholar] [CrossRef] [Green Version]
- Uccella, S.; Manzoni, P.; Marconi, N.; Toscani, C.; Biasoli, S.; Cianci, S.; Franchi, M.; Sorice, P.; Bertoli, F.; Zorzato, P.C.; et al. Impact of Sport Activity and Physical Exercise on Obstetrical and Perineal Outcomes at Delivery: A Prospective Study. Am. J. Perinatol. 2019, 36, S83–S90. [Google Scholar] [CrossRef] [Green Version]
- Dieb, A.S.; Shoab, A.Y.; Nabil, H.; Gabr, A.; Abdallah, A.A.; Shaban, M.M.; Attia, A.H. Perineal massage and training reduce perineal trauma in pregnant women older than 35 years: A randomized controlled trial. Int. Urogynecol. J. 2019, 31, 613–619. [Google Scholar] [CrossRef]
- Rise, E.; Bø, K.; Nystad, W. Is there any association between abdominal strength training before and during pregnancy and delivery outcome? The Norwegian Mother and Child Cohort Study. Braz. J. Phys. Ther. 2019, 23, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Waddington, H.; Aloe, A.M.; Becker, B.J.; Djimeu, E.W.; Hombrados, J.G.; Tugwell, P.; Wells, G.; Reeves, B. Quasi-experimental study designs series—paper 6: Risk of bias assessment. J. Clin. Epidemiol. 2017, 89, 43–52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Latorre, G.F.S.; De Fraga, R.; Seleme, M.R.; Pt, C.V.M.; Berghmans, B. An ideal e-health system for pelvic floor muscle training adherence: Systematic review. Neurourol. Urodyn. 2019, 38, 63–80. [Google Scholar] [CrossRef] [PubMed]
| Class Number | Theme of the Session |
|---|---|
| Session 1 (Initial measurement) | Physiological changes during pregnancy |
| Session 2 | Childbirth |
| Session 3 (Intermediate measurement) | Care of the newborn |
| Session 4 | The postpartum period |
| Session 5 (Final measurement) | Breastfeeding |
| Variable | Total (n = 72) | Assistance to Regular Maternal Education (n = 48) | Assistance to Pilates Sessions (n = 24) | p-Value |
|---|---|---|---|---|
| Age, mean (SD) | 32.4 (5.2) | 32.4 (5.4) | 32.5 (4.8) | 0.80 |
| Height, mean (SD), m | 1.6 (0.0) | 1.6 (0.1) | 1.6 (0.1) | 0.40 |
| Weight 2, mean (SD), Kg | 67 (10.1) | 67.6 (10) | 65.7 (10.3) | 0.51 |
| BMI 3, mean (SD), Kg/m2 | 25.2 (3.8) | 25.2 (3.8) | 25.0 (4) | 0.45 |
| SBP, mean (SD), mmHg | 110.8 (10.5) | 110.5 (11) | 111.5 (10) | 0.40 |
| DBP, mean (SD), mmHg | 67.6 (8.5) | 67.6 (8.6) | 67.6 (8.6) | 0.28 |
| Weeks of Gestation, mean (SD) | 27.3 (3.7) | 27.3 (4.1) | 27.3 (2.6) | 0.69 |
| Physical Activity, n (%) | ||||
| Intense | 33 (11) | 4 (8.3) | 4 (16.7) | 0.42 |
| Moderate | 31 (43.1) | 23 (47.9) | 8 (33.3) | |
| Low | 8 (45.8) | 21 (43.8) | 12 (50) | |
| Smoking, n (%) | ||||
| Nonsmoker | 68 (94.4) | 45 (93.8) | 23 (95.8) | 0.72 |
| Smoker | 4 (5.6) | 3 (6.2) | 1 (4.2) | |
| Educational level, n (%) | ||||
| Primary–Secondary. | 26 (36.1) | 18 (37.5) | 8 (33.3) | 0.59 |
| Superior–Further. | 46 (63.9) | 30 (62.5) | 16 (66.7) | |
| Variable | Presence of Tearing (n = 30) | Absence of Tearing (n = 42) | OR Crude | IC 95% | p-Value |
|---|---|---|---|---|---|
| Age, mean (SD) | 33.4 (5.2) | 31.7 (5.1) | 1.07 | 0.97–1.18 | 0.58 |
| Weight, mean (SD), Kg | 72 (11.7) | 69.1 (10.3) | 1.02 | 0.98–1.07 | 0.58 |
| BMI, mean (SD), Kg/m2 | 26.8 (4.4) | 26.1 (3.7) | 1.04 | 0.93–1.17 | 0.53 |
| Weight gain during gestation, mean (SD) | 7.3 (6.7) | 7,05 (8,0) | 1.01 | 0.94–1.07 | 0.88 |
| SBP, mean (SD), mmHg | 111.9 (11.7) | 110.7 (10.4) | 1.01 | 0.97–1.05 | 0.50 |
| DBP, mean (SD), mmHg | 68.4 (7) | 67.6 (7) | 1.02 | 0.95–1.09 | 0.71 |
| Physical Activity, n (%) | |||||
| Low–Moderate | 27 (57.8) | 37 (42.2) | 1.22 | 0.27–5.53 | 0.59 |
| Intense | 3 (37.5) | 5 (62.5) | 1 | 1 | |
| Educational level, n (%) | |||||
| Primary–Secondary. | 9 (30) | 17 (40.5) | 0.63 | 0.22–1.7 | 0.17 |
| Superior–Further. | 21 (70) | 25 (59.5.6) | 1 | 1 | |
| Weeks of gestation at the end intervention, mean (SD) | 31.8 (4.7) | 32.6 (4) | 0.96 | 0.86–1.07 | 0.38 |
| Smoker, n (%) | |||||
| Nonsmoker | 2 (6.7) | 2 (4.8) | 1.43 | 0.2–10.75 | 0.89 |
| Smoker | 28 (93.3) | 40 (95.2) | 1 | 1 | |
| Assistance to Pilates, n (%) | |||||
| Yes | 4 (13.3) | 20 (47.6) | 0.17 | 0.05–0.57 | 0.007 |
| No | 26 (86.7) | 22 (52.4) | 1 | 1 | |
| Weeks of gestation at labor, mean (SD) | 39.2 (1.4) | 38.9 (1.5) | 1.18 | 0.82–1.6 | 0.70 |
| Type of childbirth, n (%) | |||||
| Eutocic | 5 (16.7) | 16 (38.1) | 0.32 | 0.10–1.02 | 0.19 |
| Dystocic | 25 (83.3) | 26 (61.9) | 1 | 1 | |
| Type of labor, n (%) | |||||
| Induced | 5 (16.7) | 9 (21.4) | 0.73 | 0.22–2.46 | 0.12 |
| Spontaneous | 25 (83.3) | 33 (78.6) | 1 | 1 | |
| Labor analgesia, n (%) | |||||
| Yes | 23 (76.7) | 37 (88.1) | 0.44 | 0.13–1.57 | 0.32 |
| No | 7 (23.3) | 5 (11.9) | 1 | 1 | |
| Episiotomy, n (%) | |||||
| Yes | 3 (10) | 28 (66.7) | 0.06 | 0.01–0.21 | 0.006 |
| No | 27 (90) | 14 (33.3) | 1 | 1 | |
| Weight of newborns, mean (SD), g | 3302.3 (347.5) | 3135.6 (373.1) | 1.00 | 1.000–1.003 | 0.006 |
| Pregnant women present at the end of Pilates (n = 24)/Pregnant women present at the end of education program (n = 48) All deliveries were cephalic, and there is no record of posterior cephalic position in any of the records. | |||||
| Variable | Total (n = 72) | Assistance to Regular Maternal Education (n = 48) | Assistance to Pilates Sessions (n = 24) | p-Value |
|---|---|---|---|---|
| Weight | ||||
| First trimester 1 | 63.3 (10.1) | 63.7 (10.4) | 62.5 (9.7) | 0.62 |
| Before the labor | 70.4 (10.8) | 70.6 (10.8) | 70.2 (11.0) | 0.88 |
| BMI | ||||
| First trimester 1 | 23.8 (3.7) | 23.8 (3.7) | 23.8 (3.7) | 0.97 |
| Before the labor | 26.4 (4.0) | 26.3 (4.0) | 26.5 (4.1) | 0.89 |
| Weight gain during gestation | 7.2 (7.4) | 6.9 (8.2) | 7.7 (5.8) | 0.63 |
| Variable | Coefficient | OR | IC 95% | p-Value |
|---|---|---|---|---|
| Educational Level | ||||
| Primary–Secondary | −1.41 | 0.24 | 0.06–0.98 | 0.047 |
| Superior–Further | 1 | 1 | ||
| Assistance to Pilates | ||||
| Yes | −1.76 | 0.17 | 0.04–0.78 | 0.022 |
| No | 1 | 1 | ||
| Episiotomy | ||||
| Yes | −3.2 | 0.04 | 0.09–0.2 | 0.001 |
| No | 1 | 1 | ||
| Log-2 likelihood: 62.94; R2 Cox–Snell: 0.38; R2 Nagelkerke: 0.52; Hosmer–Lemeshow: 0.81, 5 gl (p = 0.98). | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feria-Ramírez, C.; Gonzalez-Sanz, J.D.; Molina-Luque, R.; Molina-Recio, G. The Effects of the Pilates Method on Pelvic Floor Injuries during Pregnancy and Childbirth: A Quasi-Experimental Study. Int. J. Environ. Res. Public Health 2021, 18, 6995. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18136995
Feria-Ramírez C, Gonzalez-Sanz JD, Molina-Luque R, Molina-Recio G. The Effects of the Pilates Method on Pelvic Floor Injuries during Pregnancy and Childbirth: A Quasi-Experimental Study. International Journal of Environmental Research and Public Health. 2021; 18(13):6995. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18136995
Chicago/Turabian StyleFeria-Ramírez, Carmen, Juan D. Gonzalez-Sanz, Rafael Molina-Luque, and Guillermo Molina-Recio. 2021. "The Effects of the Pilates Method on Pelvic Floor Injuries during Pregnancy and Childbirth: A Quasi-Experimental Study" International Journal of Environmental Research and Public Health 18, no. 13: 6995. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18136995









