Characteristics and Trends of the Hospital Standardized Readmission Ratios for Pneumonia: A Retrospective Observational Study Using Japanese Administrative Claims Data from 2010 to 2018
Abstract
:1. Introduction
2. Methods
2.1. Data Sources
2.2. Calculation of HSRRs
2.3. Relationship between Readmission and In-Hospital Mortality
2.4. Statistical Analysis
2.5. Patient and Public Involvement
3. Results
3.1. Characteristics of the Study Population
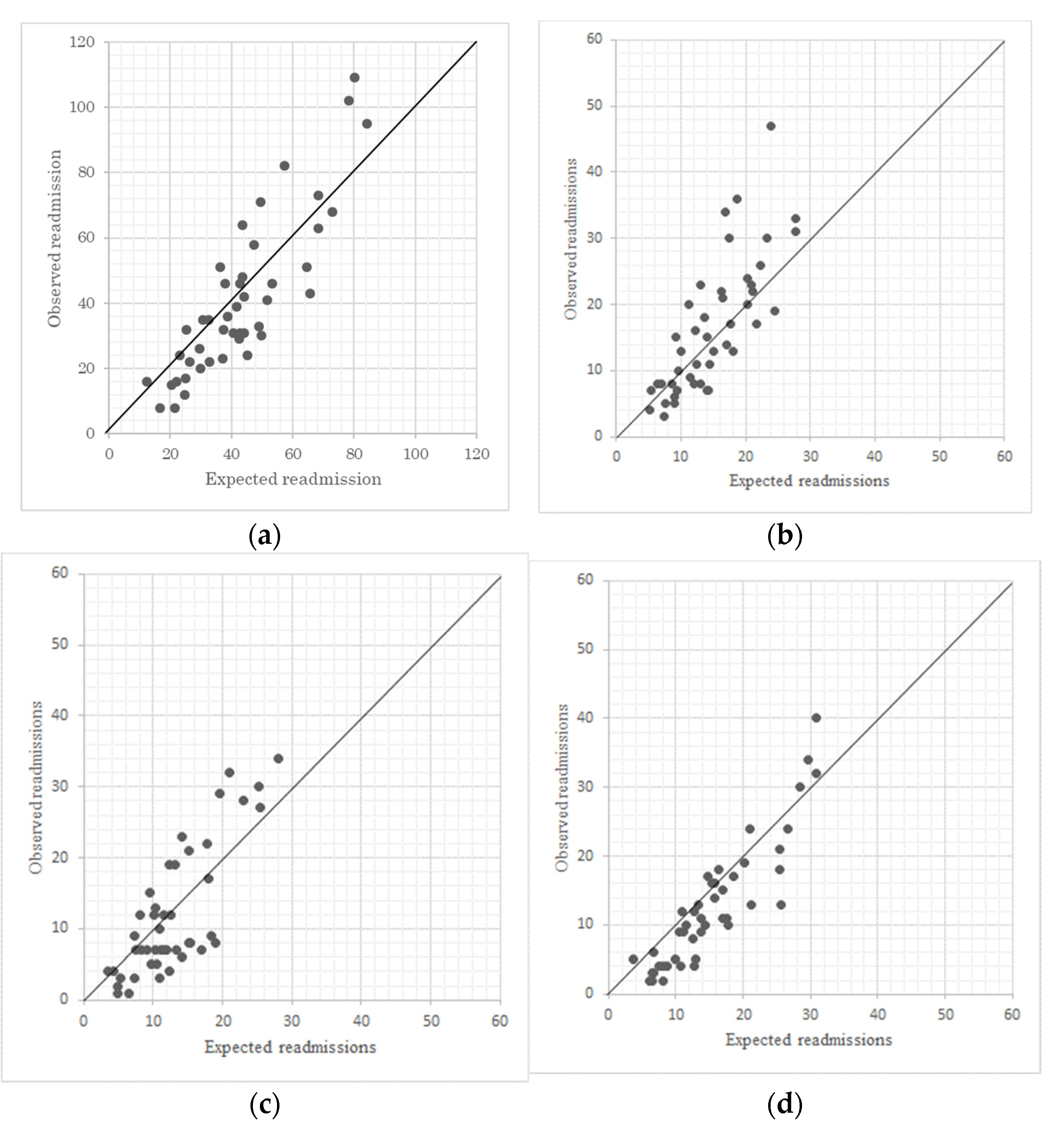
3.2. Characteristic of the HSRRs
3.3. Trends of the HSRRs
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Portal Site of Official Statistics of Japan, e-Stat. Available online: https://www.e-stat.go.jp/en/ (accessed on 5 March 2020).
- Nimptsch, U.; Mansky, T. Quality measurement combined with peer review improved German in-hospital mortality ratios for four diseases. Health Aff. 2013, 32, 1616–1623. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Institute for Health and Care Excellence. Pneumonia in Adults; National Institute for Health and Care Excellence: London, UK, 2016. [Google Scholar]
- Lingsma, H.F.; Bottle, A.; Middleton, S.; Kievit, J.; Steyerberg, E.W.; Marang-Van De Mheen, P.J. Evaluation of hospital outcomes: The relation between length-of-stay, readmission, and mortality in large international administrative database. BMC Health Serv. Res. 2018, 18, 116. [Google Scholar] [CrossRef] [Green Version]
- Dean, N.C.; Bateman, K.A.; Donnelly, S.M.; Silver, M.P.; Snow, G.L.; Hale, D. Improved clinical outcomes with utilization of a community-acquired pneumonia guideline. Chest 2006, 130, 794–799. [Google Scholar] [CrossRef]
- Gleason, P.P.; Meehan, T.P.; Fine, J.M.; Galusha, D.H.; Fine, M.J. Associations between initial antimicrobial therapy and medical outcomes for hospitalized elderly patients with pneumonia. Arch. Intern. Med. 1999, 159, 2562–2572. [Google Scholar] [CrossRef] [Green Version]
- Jarman, B.; Pieter, D.; Van Der Veen, A.A.; Kool, R.B.; Aylin, P.; Bottle, A.; Westert, G.P.; Jones, S. The hospital standardised mortality ratio: A powerful tool for Dutch hospitals to assess their quality of care? Qual. Saf. Health Care 2010, 19, 9–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scott, I.A.; Brand, C.A.; Phelps, G.E.; Barker, A.L.; Cameron, P.A. Using hospital standardised mortality ratios to assess quality of care--proceed with extreme caution. Med. J. Aust. 2011, 194, 645–648. [Google Scholar] [CrossRef] [PubMed]
- Desai, N.R.; Ross, J.S.; Kwon, J.Y.; Herrin, J.; Dharmarajan, K.; Bernheim, S.M.; Krumholz, H.M.; Horwitz, L.I. Association Between Hospital Penalty Status Under the Hospital Readmission Reduction Program and Readmission Ratios for Target and Non-Target Conditions. JAMA 2016, 316, 2647–2656. [Google Scholar] [CrossRef] [Green Version]
- Wadhera, R.K.; Maddox, K.E.J.; Wasfy, J.H.; Haneuse, S.; Shen, C.; Yeh, R.W. Association of the Hospital Readmission Reduction Program With Mortality During and After Hospitalization for Acute Myocardial Infarction, Heart Failure, and Pneumonia. JAMA Netw. Open 2018, 1, 2542–2552. [Google Scholar]
- Jason, H.; Corwin, M.Z.; Christinne, C. Readmission Ratios of the Hospital Readmissions Reduction Program. Ann. Intern. Med. 2017, 166, 324–332. [Google Scholar]
- McCarthy, C.P.; Vaduganathan, M.; Patel, K.V.; Lalani, H.S.; Ayers, C.; Bhatt, D.L.; Januzzi, J.L.; de Lemos, J.A.; Yancy, C.; Fonarow, G.C.; et al. Association of the New Peer Group-Stratified Method With the Reclassification of Penalty Status in the Hospital Readmission Reduction Program. JAMA Netw. Open 2019, 2, e192987. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caracciolo, C.M.; Parker, D.M.; Marshall, E.; Brown, J.R. Excess Readmission vs Excess Penalties as a Function of Socioeconomics and Geography. J. Hosp. Med. 2017, 12, 610. [Google Scholar] [CrossRef] [Green Version]
- Zuckerman, R.B.; Sheingold, S.H.; Orav, E.J.; Ruhter, J.; Epstein, A.M. Readmissions, Observation, and the Hospital Readmissions Reduction Program. N. Engl. J. Med. 2016, 374, 1543–1551. [Google Scholar] [CrossRef]
- Yunwei, G.; Dessislava, P. Impact of the Medicare hospital readmissions reduction program on vulnerable populations. BMC Health Serv. Res. 2019, 19, 1–15. [Google Scholar]
- Salerno, A.M.; Horwitz, L.I.; Kwon, J.Y.; Herrin, J.; Grady, J.N.; Lin, Z.; Ross, J.S.; Bernheim, S.M. Trends in readmission ratios for safety net hospitals and non-safety net hospitals in the era of the US Hospital Readmission Reduction Program: A retrospective time series analysis using Medicare administrative claims data from 2008 to 2015. BMJ Open 2017, 7, e016149. [Google Scholar] [CrossRef]
- Wadhera, R.K.; Maddox, K.E.J.; Kazi, D.S.; Shen, C.; Yeh, R.W. Hospital revisits within 30 days after discharge for medical conditions targeted by the Hospital Readmissions Reduction Program in the United States: National retrospective analysis. BMJ 2019, 366, 14563. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aswani, M.S.; Kilgore, M.L.; Becker, D.J.; Redden, D.T.; Sen, B.; Blackburn, J. Differential Impact of Hospital and Community Factors on Medicare Readmission Penalties. Health Serv. Res. 2018, 53, 4416–4436. [Google Scholar] [CrossRef]
- Zuckerman, R.B.; Joynt Maddox, K.E.; Sheingold, S.H.; Chen, L.M.; Epstein, A.M. Effect of a Hospital-wide Measure on the Readmissions Reduction Program. N. Engl. J. Med. 2017, 337, 1551–1558. [Google Scholar] [CrossRef] [PubMed]
- Centers for Medicare & Medicaid Services. MEASURE INFORMATION FORM. Available online: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeedbackProgram/Downloads/2015-ACR-MIF.pdf (accessed on 5 March 2020).
- Thompson, M.P.; Kaplan, C.M.; Cao, Y.; Bazzoli, G.J.; Waters, T.M. Reliability of 30-Day Readmission Measures Used in the Hospital Readmission Reduction Program. Health Serv. Res. 2016, 51, 2095–2114. [Google Scholar] [CrossRef] [Green Version]
- Borza, T.; Oerline, M.K.; Skolarus, T.A.; Norton, E.C.; Ryan, A.M.; Ellimoottil, C.; Dimick, J.B.; Shahinian, V.B.; Hollenbeck, B.K. Association of the Hospital Readmissions Reduction Program With Surgical Readmissions. JAMA Surg. 2018, 153, 243–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kitazawa, T.; Matsumoto, K.; Fujita, S.; Yoshida, A.; Iida, S.; Nishizawa, H.; Hasegawa, T. Perioperative patient safety indicators and hospital surgical volumes. BMC Res. Notes 2014, 7, 117. [Google Scholar] [CrossRef] [Green Version]
- Matsuda, S.; Fujimori, K.; Kuwabara, K.; Ishikawa, K.B.; Fushimi, K. Diagnosis procedure combination as an infrastructure for the clinical study. Asian Pac. J. Dis. Manag. 2011, 5, 81–87. [Google Scholar] [CrossRef]
- Uematsu, H.; Kunisawa, S.; Yamashita, K.; Fushimi, K.; Imanaka, Y. Impact of weekend admission on in-hospital mortality in severe community-acquired pneumonia patients in Japan. Respirology 2016, 21, 905–910. [Google Scholar] [CrossRef] [Green Version]
- Amin, R.; Hatakeyama, Y.; Kitazawa, T.; Matsumoto, K.; Fujita, S.; Seto, K.; Hasegawa, T. Capturing the trends in hospital standardized mortality ratios for pneumonia: A retrospective observational study in Japan (2010 to 2018). BMC Health Serv. Res. 2020, 25, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Friebel, R.; Hauck, K.; Aylin, P.; Steventon, A. National trends in emergency readmission ratios: A longitudinal analysis of administrative data for England between 2006 and 2016. BMJ Open 2018, 8, e020325. [Google Scholar] [CrossRef] [Green Version]
- Aylin, P.; Bottle, A.; Majeed, A. Use of administrative data or clinical databases as predictors of risk of death in hospital: Comparison of models. BMJ 2007, 334, 1044. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Institute for Health and Care Excellence. CCG Outcome Indicator Set; National Institute for Health and Care Excellence: London, UK, 2019. [Google Scholar]
- Shindo, Y.; Sato, S.; Maruyama, E.; Ohashi, T.; Ogawa, M.; Imaizumi, K.; Hasegawa, Y. Comparison of severity scoring systems A-DROP and CURB-65 for community-acquired pneumonia. Respirology 2008, 13, 731–735. [Google Scholar] [CrossRef] [PubMed]
- The committee for the Japanese Respiratory Society guidelines for the management of respiratory infections. Severity classification of pneumonia. Respirology 2006, 11, S84–S85. [Google Scholar] [CrossRef]
- Naoyuki, M.; Toshiharu, M.; Mikio, O.; Japanese Respiratory Society. The JRS guidelines for the management of community-acquired pneumonia in adults: An update and new recommendations. Intern. Med. 2006, 45, 419–428. [Google Scholar]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.M.; Sundararajan, V. Updating and Validation the Charlson Comorbidity Index and Score for Risk Adjustment in Hospital Discharge Abstract Using Data From 6 Countries. Am. J. Epidemiol. 2011, 173, 676–682. [Google Scholar] [CrossRef] [Green Version]
- Ethical Guidelines for Epidemiological Research. Available online: http://www.lifescience.mext.go.jp/files/pdf/n796_01.pdf (accessed on 19 January 2020).
- Zhou, H.; Della, P.R.; Roberts, P.; Goh, L.; Dhaliwal, S.S. Utility of analyses to predict 28-day or 30-day unplanned hospital readmissions: An updated systematic review. BMJ Open 2016, 6, e0110. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | 2010–2018 (n = 54,756) | |||
|---|---|---|---|---|
| Readmission | Non-Readmission | p | ||
| Demographic features | ||||
| Age 15–64 year (reference) | 168 (0.3) | 8137 (14.9) | <0.001 †† | |
| Age 65–74 year | 301 (0.5) | 8394 (15.3) | ||
| Age 75 year+ | 1377 (2.5) | 36,379 (66.4) | ||
| Sex (% of male) | 1173 (2.1) | 28,944 (50.1) | <0.001 †† | |
| Comorbidity | ||||
| CCI score 0 (reference) | 758 (1.4) | 25,307 (46.2) | <0.001 †† | |
| CCI score 1–2 | 799 (1.5) | 21,376 (39.0) | ||
| CCI score 3–4 | 250 (0.5) | 5415 (9.9) | ||
| CCI score 5+ | 39 (0.1) | 812 (1.5) | ||
| Urgency of admission (% of Emergency admission) | 1546 (2.8) | 46,218 (84.4) | <0.001 †† | |
| Severity status | ||||
| ADROP score 0 (reference) | 155 (0.3) | 7956 (14.5) | <0.001 †† | |
| ADROP score 1–2 (moderate) | 1255 (2.3) | 34,100 (62.3) | ||
| ADROP score 3 (severe) | 322 (0.6) | 8186 (14.9) | ||
| ADROP score 4–5 (extremely severe) | 114 (0.2) | 2668 (4.9) | ||
| LOS (days) | mean ± SD | 24.8 ± 24.7 | 20.2 ± 24.2 | <0.001 † |
| Discharge destination (home) | 1157 (2.1) | 36,192 (66.1) | <0.001 †† | |
| Coefficient | p | Odds Ratio | (95% CI) | |
|---|---|---|---|---|
| Age 15–64 year (reference) | ||||
| Age 65–74 year | 0.318 | 0.003 | 1.375 | (1.117–1.692) |
| Age 75 year+ | 0.303 | 0.004 | 1.354 | (1.103–1.663) |
| Sex (male) | 0.357 | <0.001 | 1.429 | (1.295–1.577) |
| CCI score 0 (reference) | ||||
| CCI score 1–2 | 0.313 | 0.003 | 1.169 | (1.055–1.294) |
| CCI score 3–4 | 0.315 | <0.001 | 1.371 | (1.182–1.589) |
| CCI score 5+ | 0.367 | 0.029 | 1.444 | (1.038–2.010) |
| Urgency of admission (Emergency admission) | −0.324 | <0.001 | 0.723 | (0.637–0.821) |
| ADROP score 0 (reference) | ||||
| ADROP score 1–2 (moderate) | 0.364 | 0.001 | 1.439 | (1.163–1.781) |
| ADROP score 3 (severe) | 0.361 | 0.003 | 1.435 | (1.126–1.829) |
| ADROP score 4–5 (extremely severe) | 0.424 | 0.004 | 1.528 | (1.146–2.035) |
| LOS (days) | 0.003 | <0.001 | 1.003 | (1.002–1.004) |
| Discharge destination (home) | −0.214 | <0.001 | 0.807 | (0.730–0.893) |
| Period | n | r | p |
|---|---|---|---|
| 2010–2012—2013–2015 | 99 | 0.255 | 0.010 |
| 2013–2015—2016–2018 | 80 | 0.603 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Onishi, R.; Hatakeyama, Y.; Matsumoto, K.; Seto, K.; Hirata, K.; Hasegawa, T. Characteristics and Trends of the Hospital Standardized Readmission Ratios for Pneumonia: A Retrospective Observational Study Using Japanese Administrative Claims Data from 2010 to 2018. Int. J. Environ. Res. Public Health 2021, 18, 7624. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18147624
Onishi R, Hatakeyama Y, Matsumoto K, Seto K, Hirata K, Hasegawa T. Characteristics and Trends of the Hospital Standardized Readmission Ratios for Pneumonia: A Retrospective Observational Study Using Japanese Administrative Claims Data from 2010 to 2018. International Journal of Environmental Research and Public Health. 2021; 18(14):7624. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18147624
Chicago/Turabian StyleOnishi, Ryo, Yosuke Hatakeyama, Kunichika Matsumoto, Kanako Seto, Koki Hirata, and Tomonori Hasegawa. 2021. "Characteristics and Trends of the Hospital Standardized Readmission Ratios for Pneumonia: A Retrospective Observational Study Using Japanese Administrative Claims Data from 2010 to 2018" International Journal of Environmental Research and Public Health 18, no. 14: 7624. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18147624






