Changes in Clinical Characteristics and Outcomes of Patients Admitted to Inpatient Cardiac Rehabilitation
Abstract
:1. Introduction
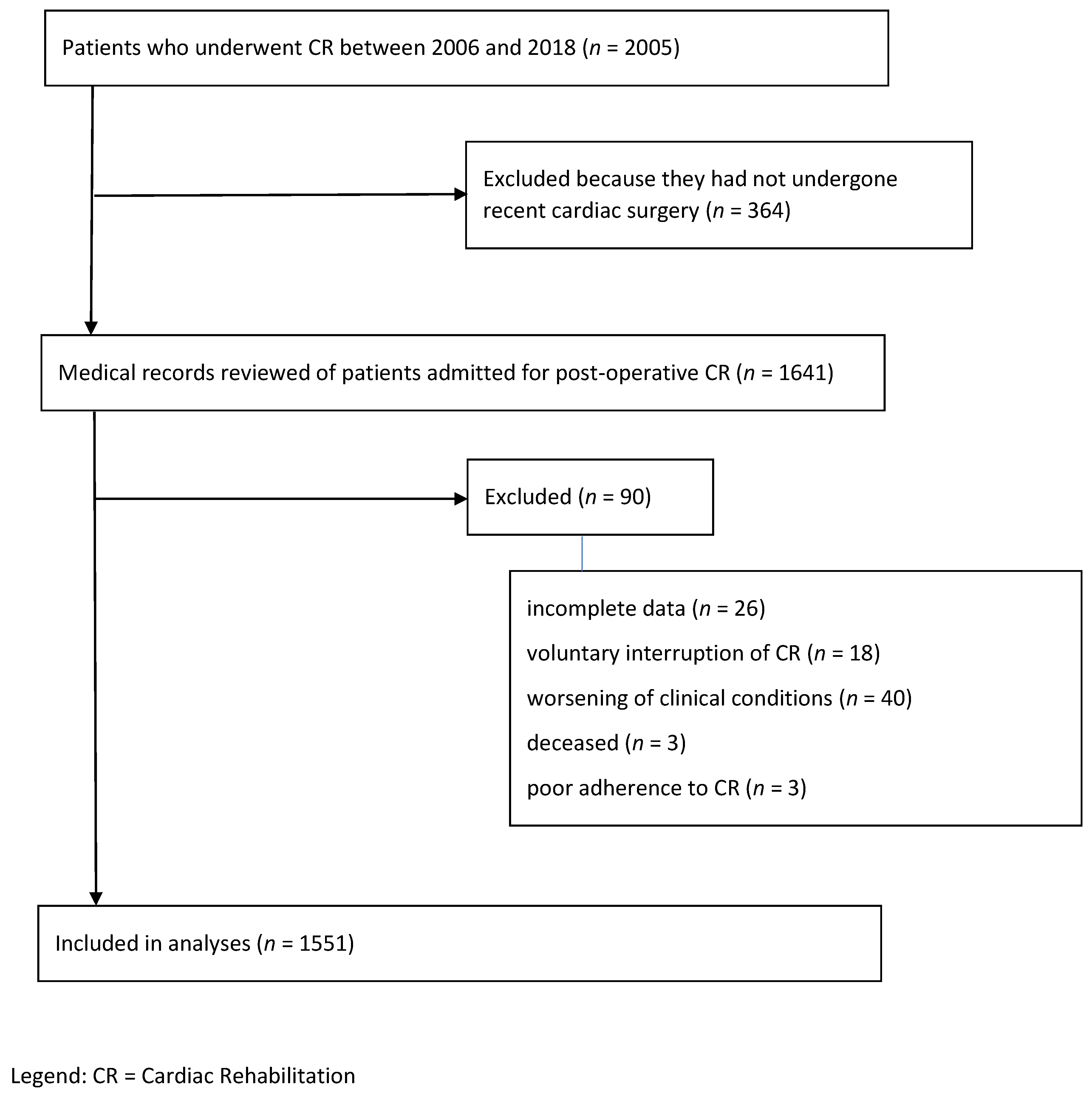
2. Methods
2.1. Study Design and Data Sources
2.2. Cardiac Rehabilitation Program
2.3. Data Collection and Outcome Assessment
2.4. Data Analysis
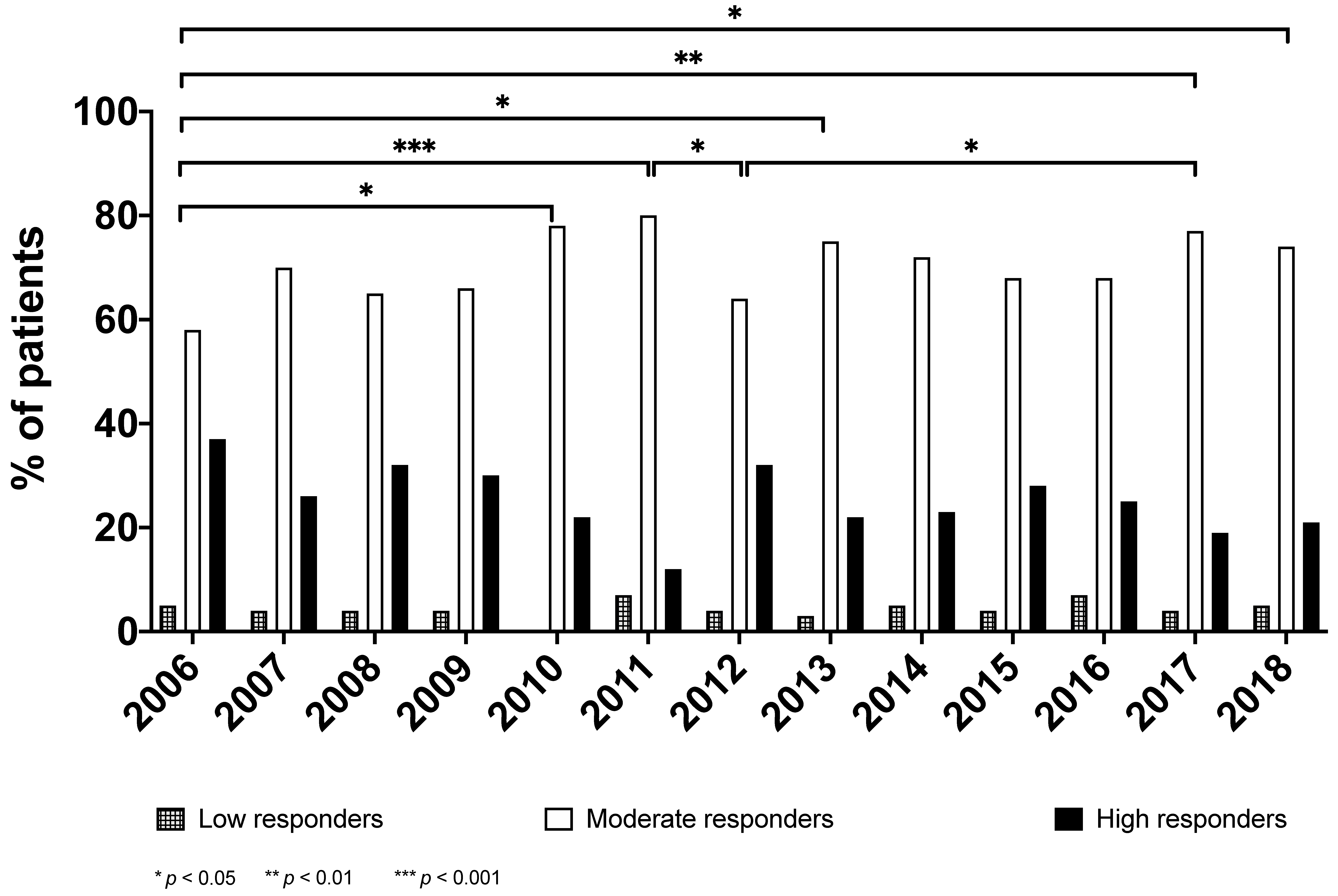
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Piepoli, M.F.; Corrà, U.; Adamopoulos, S.; Benzer, W.; Bjarnason-Wehrens, B.; Cupples, M.; Dendale, P.; Doherty, P.; Gaita, D.; Höfer, S.; et al. Secondary prevention in the clinical management of patients with cardiovascular diseases. Core components, standards and outcome measures for referral and delivery: A policy statement from the cardiac rehabilitation section of the European Association for Cardiovascular Prevention & Rehabilitation. Endorsed by the Committee for Practice Guidelines of the European Society of Cardiology. Eur. J. Prev. Cardiol. 2014, 21, 664–681. [Google Scholar] [CrossRef]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.-T.; Corra, U.; Cosyns, B.; Deaton, C.; et al. Linee guida europee 2016 sulla prevenzione delle malattie cardiovascolari nella pratica clinica. Sesta Task Force congiunta della Società Europea di Cardiologia e di altre Società sulla Prevenzione delle Malattie Cardiovascolari nella Pratica Clinica (costituita da rappresentanti di 10 società e da esperti invitati). Redatte con il contributo straordinario dell’Associazione Europea per la Prevenzione e Riabilitazione Cardiovascolare (EACPR) [2016 European guidelines on cardiovascular disease prevention in clinical practice. The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts. Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation]. G. Ital. Cardiol. 2017, 18, 547–612. [Google Scholar] [CrossRef]
- Schopfer, D.; Forman, D.E. Cardiac Rehabilitation in Older Adults. Can. J. Cardiol. 2016, 32, 1088–1096. [Google Scholar] [CrossRef]
- Suaya, J.A.; Shepard, D.S.; Normand, S.-L.T.; Ades, P.A.; Prottas, J.; Stason, W.B. Use of Cardiac Rehabilitation by Medicare Beneficiaries After Myocardial Infarction or Coronary Bypass Surgery. Circulation 2007, 116, 1653–1662. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khadanga, S.; Savage, P.D.; Gaalema, D.E.; Ades, P.A. Predictors of Cardiac Rehabilitation Participation: OPPORTUNITIES TO INCREASE ENROLLMENT. J. Cardiopulm. Rehabil. Prev. 2021. [Google Scholar] [CrossRef]
- Kirk, H.; Kersten, P.; Crawford, P.; Keens, A.; Ashburn, A.; Conway, J. The cardiac model of rehabilitation for reducing cardiovascular risk factors post transient ischaemic attack and stroke: A randomized controlled trial. Clin. Rehabil. 2014, 28, 339–349. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.J.; Balady, G.; Banka, G.; Beckie, T.M.; Chiu, J.; Gokak, S.; Ho, P.M.; Keteyian, S.J.; King, M.; Lui, K.; et al. 2018 ACC/AHA Clinical Performance and Quality Measures for Cardiac Rehabilitation: A Report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. J. Am. Coll. Cardiol. 2018, 71, 1814–1837. [Google Scholar] [CrossRef] [PubMed]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef]
- Jones, C.J.; Rikli, R.E.; Beam, W.C. A 30-s Chair-Stand Test as a Measure of Lower Body Strength in Community-Residing Older Adults. Res. Q. Exerc. Sport 1999, 70, 113–119. [Google Scholar] [CrossRef]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS Statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117, Erratum in 2016, 193, 1185. [Google Scholar] [CrossRef]
- Samsa, G.; Edelman, D.; Rothman, M.L.; Williams, G.R.; Lipscomb, J.; Matchar, D. Determining clinically important differences in health status measures: A general approach with illustration to the Health Utilities Index Mark II. Pharmacoeconomics. PharmacoEconomics 1999, 15, 141–155. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Ozalevli, S.; Ozden, A.; Itil, O.; Akkoclu, A. Comparison of the Sit-to-Stand Test with 6 min walk test in patients with chronic obstructive pulmonary disease. Respir. Med. 2007, 101, 286–293. [Google Scholar] [CrossRef] [Green Version]
- Wright, A.A.; Cook, C.E.; Baxter, D.; Dockerty, J.D.; Abbott, J.H. A Comparison of 3 Methodological Approaches to Defining Major Clinically Important Improvement of 4 Performance Measures in Patients With Hip Osteoarthritis. J. Orthop. Sports Phys. Ther. 2011, 41, 319–327. [Google Scholar] [CrossRef]
- Singh, S.J.; Puhan, M.; Andrianopoulos, V.; Hernandes, N.A.; Mitchell, K.E.; Hill, C.J.; Lee, A.L.; Camillo, C.A.; Troosters, T.; Spruit, M.A.; et al. An official systematic review of the European Respiratory Society/American Thoracic Society: Measurement properties of field walking tests in chronic respiratory disease. Eur. Respir. J. 2014, 44, 1447–1478. [Google Scholar] [CrossRef] [PubMed]
- Ries, A.L. Minimally Clinically Important Difference for the UCSD Shortness of Breath Questionnaire, Borg Scale, and Visual Analog Scale. COPD J. Chronic Obstr. Pulm. Dis. 2005, 2, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Khair, R.M.; Nwaneri, C.; Damico, R.L.; Kolb, T.; Hassoun, P.M.; Mathai, S.C. The Minimal Important Difference in Borg Dyspnea Score in Pulmonary Arterial Hypertension. Ann. Am. Thorac. Soc. 2016, 13, 842–849. [Google Scholar] [CrossRef] [Green Version]
- IBM Corp. IBM SPSS Statistics for Windows, Version 25.0; IBM Corp: Armonk, NY, USA, 2017. [Google Scholar]
- GraphPad Prism Version 8.0.0 for Windows, GraphPad Software. Available online: https://www.graphpad.com (accessed on 14 June 2021).
- The Jamovi Project. Jamovi. (Version 1.2) [Computer Software]. 2020. Available online: https://www.jamovi.org (accessed on 14 June 2021).
- Sartini, C.; Lomivorotov, V.; Pisano, A.; Riha, H.; Redaelli, M.B.; Lopez-Delgado, J.C.; Pieri, M.; Hajjar, L.; Fominskiy, E.; Likhvantsev, V.; et al. A Systematic Review and International Web-Based Survey of Randomized Controlled Trials in the Perioperative and Critical Care Setting: Interventions Increasing Mortality. J. Cardiothorac. Vasc. Anesth. 2019, 33, 2685–2694. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; von Segesser, L.K.; Berdajs, D.; Ferrari, E. Endovascular treatment of the dissected proximal aortic arch: A systematic review. Interact. Cardiovasc. Thorac. Surg. 2021, ivab161. [Google Scholar] [CrossRef] [PubMed]
- Tonelli, R.; Crisafulli, E.; Costi, S.; Clini, E. The multimorbidity patient. In Pulmonary Rehabilitation; Donner, C., Ambrosino, N., Goldstein, R., Eds.; Taylor & Francis Group: London, UK, 2020; pp. 349–357. [Google Scholar]
- Abraham, L.N.; Sibilitz, K.L.; Berg, S.K.; Tang, L.H.; Risom, S.S.; Lindschou, J.; Taylor, R.S.; Borregaard, B.; Zwisler, A.-D. Exercise-based cardiac rehabilitation for adults after heart valve surgery. Cochrane Database Syst. Rev. 2021, 5, CD010876. [Google Scholar] [CrossRef]
- Baker, N.; Lawn, S.; Gordon, S.J.; George, S. Older Adults’ Experiences of Goals in Health: A Systematic Review and Metasynthesis. J. Appl. Gerontol. 2021, 40, 818–827. [Google Scholar] [CrossRef]
- Hulzebos, E.H.; Smit, Y.; Helders, P.P.; van Meeteren, N.L. Preoperative physical therapy for elective cardiac surgery patients. Cochrane Database Syst. Rev. 2012, 11, CD010118. [Google Scholar] [CrossRef] [PubMed]
- Snowdon, D.; Haines, T.; Skinner, E.H. Preoperative intervention reduces postoperative pulmonary complications but not length of stay in cardiac surgical patients: A systematic review. J. Physiother. 2014, 60, 66–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mölken, M.R.-V.; Leijten, F.; Hoedemakers, M.; Tsiachristas, A.; Verbeek, N.; Karimi, M.; Bal, R.; De Bont, A.; Islam, K.; Askildsen, J.E.; et al. Strengthening the evidence-base of integrated care for people with multi-morbidity in Europe using Multi-Criteria Decision Analysis (MCDA). BMC Health Serv. Res. 2018, 18, 576. [Google Scholar] [CrossRef] [Green Version]
- Ambrosino, N.; Clini, E. Response to pulmonary rehabilitation: Toward personalised programmes? Eur. Respir. J. 2015, 46, 1538–1540. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Year | Pt. | F | M | Age | Main Diagnosis | Comorbid. | Complic. | CR Sessions | Hospital Stay |
|---|---|---|---|---|---|---|---|---|---|
| n | n (%) | n (%) | Mean ± SD | Freq. (%) | Median IQR (25;75) | Median IQR (25;75) | Mean ± SD | Mean ± SD | |
| 2006 | 65 | 22 (34) | 43 (66) | 69.7 ± 10.1 | CABG (54%) | 1 (1;3) | 0 (0;1) | 13.8 ± 2.9 | 16.5 ± 3.3 |
| 2007 | 94 | 24 (26) | 70 (75) | 68.0 ± 10.1 | CABG (44%) | 2 (1;3) | 0 (0;1) | 14.1 ± 3.3 | 17.0 ± 4.0 |
| 2008 | 79 | 24 (30) | 55 (70) | 68.6 ± 9.3 | CABG (41%) | 1 (0;3) | 0 (0;1) | 14.8 ± 3.2 | 18.1 ± 4.6 |
| 2009 | 112 | 38 (34) | 74 (66) | 69.5 ± 10.1 | CABG (47%) | 2 (1;3) | 0 (0;1) | 13.4 ± 3.5 | 16.5 ± 4.4 |
| 2010 | 83 | 30 (36) | 53 (64) | 70.2 ± 9.7 | CABG (46%) | 2 (1;3) | 1 (0;1) | 13.6 ± 3.6 | 16.5 ± 4.8 |
| 2011 | 121 | 38 (31) | 83 (69) | 70.0 ± 10.5 | CVS (38%) | 2 (1;4) | 0 (0;1) | 13.3 ± 2.8 | 16.3 ± 3.9 |
| 2012 | 168 | 67 (40) | 101 (60) | 70.0 ± 9.5 | CVS (41%) | 2 (1;4) | 0 (0;1) | 12.8 ± 2.7 | 15.9 ± 3.7 |
| 2013 | 193 | 60 (31) | 133 (69) | 70.9 ± 10.2 | CVS (40%) | 2 (1;3) | 0 (0;1) | 12.7 ± 2.1 | 15.4 ± 2.9 |
| 2014 | 87 | 40 (46) | 47 (54) | 69.8 ± 11.6 | CVS (45%) | 3 (2;4) | 1 (0;1) | 12.9 ± 2.4 | 15.9 ± 2.9 |
| 2015 | 100 | 33 (33) | 67 (67) | 69.6 ± 9.5 | CABG (41%) | 2 (1;3) | 0 (0;1) | 13.2 ± 3.6 | 16.1 ± 5.3 |
| 2016 | 104 | 48 (46) | 56 (54) | 70.9 ± 9.3 | CVS (47%) | 2 (1;3) | 0 (0;1) | 12.7 ± 1.6 | 15.3 ± 1.9 |
| 2017 | 197 | 65 (33) | 132 (67) | 71.4 ± 8.4 | CABG (44%) | 3 (2;4) | 0 (0;1) | 12.9 ± 1.6 | 15.5 ± 2.0 |
| 2018 | 148 | 44 (30) | 104 (70) | 71.1 ± 9.6 | CABG (43%) | 3 (2;4) | 1 (0;1) | 12.8 ± 1.8 | 15.4 ± 2.7 |
| Total | 1551 | 533 (34) | 1018 (66) | 70.2 ± 9.7 | CABG (41%) | 2 (1;4) | 0 (0;1) | 13.2 ± 2.7 | 16.0 ± 3.6 |
| Year | ULW | 30STS | 6MWD | Borg D | Borg F | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T0 | T1 | Δ | T0 | T1 | Δ | T0 | T1 | Δ | T0 | T1 | Δ | T0 | T1 | Δ | |
| Mean ± SD | Mean ± SD | Mean ± SD | Median IQR (25;75) | Median IQR (25;75) | |||||||||||
| 2006 | 11.9 ± 6.9 | 18.5 ± 6.7 | 6.5 ± 4.7 | 6.8 ± 5.9 | 10.3 ± 7.0 | 3.5 ± 3.9 | 239 ± 161 | 354 ± 142 | 115 ± 93 | 6 (5;7) | 2 (2;4) | −3 (−4;−2) | 6 (5;7) | 3 (2;4) | −3 (−4;−2) |
| 2007 | 13.4 ± 6.2 | 19.9 ± 6.5 | 6.4 ± 5.1 | 7.5 ± 5.2 | 10.9 ± 6.2 | 3.2 ± 3.0 | 242 ± 132 | 336 ± 131 | 94 ± 74 | 5 (4;7) | 2 (1;4) | −3 (−4;−2) | 5 (4;7) | 2 (1;4) | −3 (−4;−2) |
| 2008 | 14.3 ± 7.0 | 19.8 ± 6.9 | 5.0 ± 4.9 | 7.1 ± 6.1 | 10.8 ± 7.0 | 3.5 ± 3.0 | 235 ± 139 | 342 ± 131 | 107 ± 71 | 6 (5;7) | 2 (1;4) | −3 (−4;−2) | 6 (5;7) | 2 (1;3) | −3 (−5;−2) |
| 2009 | 14.4 ± 6.7 | 20.5 ± 6.4 | 5.7 ± 5.1 | 8.0 ± 5.4 | 12.2 ± 6.2 | 3.4 ± 3.4 | 231 ± 131 | 342 ± 127 | 110 ± 72 | 6 (4;7) | 2 (2;3) | −3 (−4;−2) | 6 (4;8) | 3 (2;4) | −3 (−4;−2) |
| 2010 | 19.4 ± 6.6 | 25.2 ± 8.0 | 4.7 ± 6.9 | 9.5 ± 4.6 | 13.9 ± 5.8 | 3.2 ± 3.3 | 243 ± 131 | 356 ± 118 | 114 ± 63 | 5 (3;6) | 2 (1;3) | −2 (−4;−1) | 5 (3;6) | 2 (1;3) | −3 (−4;−2) |
| 2011 | 19.7 ± 8.2 | 25.3 ± 8.1 | 4.8 ± 6.2 | 9.4 ± 6.1 | 13.3 ± 5.8 | 2.9 ± 3.3 | 263 ± 137 | 359 ± 133 | 96 ± 62 | 4 (3;6) | 2 (2;3) | −2 (−3;−1) | 4 (3;6) | 2 (1;3) | −2 (−3;−1) |
| 2012 | 18.7 ± 6.4 | 25.0 ± 6.6 | 5.4 ± 5.0 | 8.7 ± 4.5 | 13.1 ± 5.2 | 3.3 ± 3.1 | 237 ± 120 | 346 ± 119 | 109 ± 67 | 5 (3;7) | 2 (1;3) | −2 (−4;−1) | 4 (3;6) | 2 (1;3) | −2 (−4;−1) |
| 2013 | 19.6 ± 6.1 | 25.2 ± 5.7 | 4.9 ± 4.3 | 9.6 ± 4.5 | 13.4 ± 5.1 | 3.1 ± 2.9 | 259 ± 118 | 357 ± 126 | 99 ± 63 | 4 (3;5) | 2 (1;2) | −2 (−3;−1) | 4 (2;6) | 2 (1;3) | −2 (−3;−1) |
| 2014 | 20.1 ± 7.7 | 26.9 ± 10.8 | 6.2 ± 8.5 | 8.8 ± 4.9 | 13.4 ± 5.0 | 3.5 ± 3.5 | 241 ± 122 | 356 ± 117 | 115 ± 64 | 5 (3;8) | 2 (1;3) | −3 (−4;−2) | 4 (3;7) | 2 (1;4) | −2 (−4;−1) |
| 2015 | 17.7 ± 6.4 | 24.9 ± 7.6 | 6.7 ± 5.7 | 9.5 ± 4.8 | 13.6 ± 5.2 | 3.4 ± 3.2 | 271 ± 118 | 389 ± 124 | 118 ± 77 | 4 (3;7) | 2 (1;3) | −2 (−4;−1) | 4 (2;7) | 2 (0;3) | −2 (−4;−1) |
| 2016 | 18.3 ± 6.8 | 24.9 ± 7.2 | 6.0 ± 6.2 | 8.6 ± 5.3 | 12.9 ± 6.2 | 3.6 ± 4.3 | 270 ± 119 | 379 ± 122 | 110 ± 70 | 4 (3;5) | 2 (1;3) | −2 (−3;−1) | 4 (3;5) | 2 (1;2) | −2 (−3;−1) |
| 2017 | 19.3 ± 6.7 | 25.4 ± 7.1 | 5.6 ± 5.2 | 8.3 ± 5.2 | 12.5 ± 5.0 | 3.6 ± 3.1 | 271 ± 108 | 378 ± 110 | 107 ± 61 | 5 (3;6) | 2 (1;3) | −3 (−4;−1) | 4 (2;6) | 2 (1;3) | −2 (−4; 0) |
| 2018 | 17.9 ± 6.2 | 23.4 ± 6.2 | 5.5 ± 5.0 | 8.4 ± 4.5 | 12.0 ± 4.2 | 3.5 ± 2.4 | 267 ± 105 | 376 ± 122 | 109 ± 61 | 4 (3;6) | 2 (1;3) | −3 (−4;−1) | 4 (2;6) | 2 (1;3) | −2 (−4;−1) |
| Total | 17.7 ± 7.1 | 23.8 ± 7.5 | 5.6 ± 4.9 | 8.6 ± 5.2 | 12.6 ± 5.6 | 3.4 ± 4.2 | 254 ± 124 | 361 ± 124 | 107 ± 68 | 5 (3;7) | 2 (1;3) | −3 (−4;−1) | 5 (3;7) | 2 (1;3) | −2 (−4;−1) |
| Year | ΔULW | Δ30STS | Δ6MWD | ΔBorg D | ΔBorg F | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | |
| 2006 | 42 | 64.6 | 37 | 56.9 | 58 | 89.2 | 58 | 89.2 | 56 | 86.2 |
| 2007 | 54 | 57.4 | 47 | 50.0 | 80 | 85.1 | 85 | 90.4 | 85 | 90.4 |
| 2008 | 42 | 53.2 | 45 | 57.0 | 68 | 86.1 | 70 | 88.6 | 74 | 93.7 |
| 2009 | 60 | 53.6 | 65 | 58.0 | 103 | 92.0 | 100 | 89.3 | 101 | 90.2 |
| 2010 | 36 | 43.4 | 42 | 50.6 | 80 | 96.4 | 72 | 86.7 | 75 | 90.4 |
| 2011 | 52 | 43.0 | 55 | 45.5 | 106 | 87.6 | 94 | 77.7 | 101 | 83.5 |
| 2012 | 88 | 52.4 | 92 | 54.8 | 152 | 90.5 | 145 | 86.3 | 143 | 85.1 |
| 2013 | 90 | 46.6 | 112 | 58.0 | 171 | 88.6 | 159 | 82.4 | 160 | 82.9 |
| 2014 | 45 | 51.7 | 48 | 55.2 | 80 | 92.0 | 75 | 86.2 | 65 | 74.7 |
| 2015 | 58 | 58.0 | 56 | 56.0 | 94 | 94.0 | 87 | 87.0 | 77 | 77.0 |
| 2016 | 55 | 52.9 | 62 | 59.6 | 95 | 91.3 | 83 | 79.8 | 81 | 77.9 |
| 2017 | 104 | 52.8 | 121 | 61.4 | 186 | 94.4 | 162 | 82.2 | 135 | 68.5 |
| 2018 | 73 | 49.3 | 84 | 56.8 | 140 | 94.6 | 123 | 83.1 | 115 | 77.7 |
| Total | 799 | 51.5 | 866 | 55.8 | 1413 | 91.1 | 1313 | 84.7 | 1268 | 81.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Costi, S.; Tonelli, R.; Brogneri, A.; Florini, F.; Tilocca, N.; Vicentini, M.; Baroncini, S.; Cerulli, M.; Clini, E. Changes in Clinical Characteristics and Outcomes of Patients Admitted to Inpatient Cardiac Rehabilitation. Int. J. Environ. Res. Public Health 2021, 18, 8871. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18168871
Costi S, Tonelli R, Brogneri A, Florini F, Tilocca N, Vicentini M, Baroncini S, Cerulli M, Clini E. Changes in Clinical Characteristics and Outcomes of Patients Admitted to Inpatient Cardiac Rehabilitation. International Journal of Environmental Research and Public Health. 2021; 18(16):8871. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18168871
Chicago/Turabian StyleCosti, Stefania, Roberto Tonelli, Antonio Brogneri, Fabio Florini, Nicolò Tilocca, Massimo Vicentini, Serena Baroncini, Massimo Cerulli, and Enrico Clini. 2021. "Changes in Clinical Characteristics and Outcomes of Patients Admitted to Inpatient Cardiac Rehabilitation" International Journal of Environmental Research and Public Health 18, no. 16: 8871. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18168871








