Implementing Digital Trainings within Medical Rehabilitations: Improvement of Mental Health and Synergetic Outcomes with Healthcare Service
Abstract
:1. Introduction
1.1. Mental Health and the COVID-19 Pandemic
1.2. Therapy for Medical, Psychosomatic Rehabilitation Patients
1.3. Importance of Communication in Medical, Psychosomatic Rehabilitation Treatment Programs
1.4. Compensatory Carry-Over Action Model
1.5. Goal of the Study
2. Materials and Methods
2.1. Study Design
2.2. Recruitment and Data Collection
2.3. Participants
2.4. Interventions
2.5. Instruments
2.5.1. Depressive Symptoms and Symptoms of Anxiety
2.5.2. Perceived Stress
2.5.3. Loneliness
2.5.4. Rehabilitation Goals
2.5.5. Perceived Communication
2.5.6. Satisfaction with Rehabilitation
2.5.7. Statistical Analyses
3. Results
3.1. Randomization Check
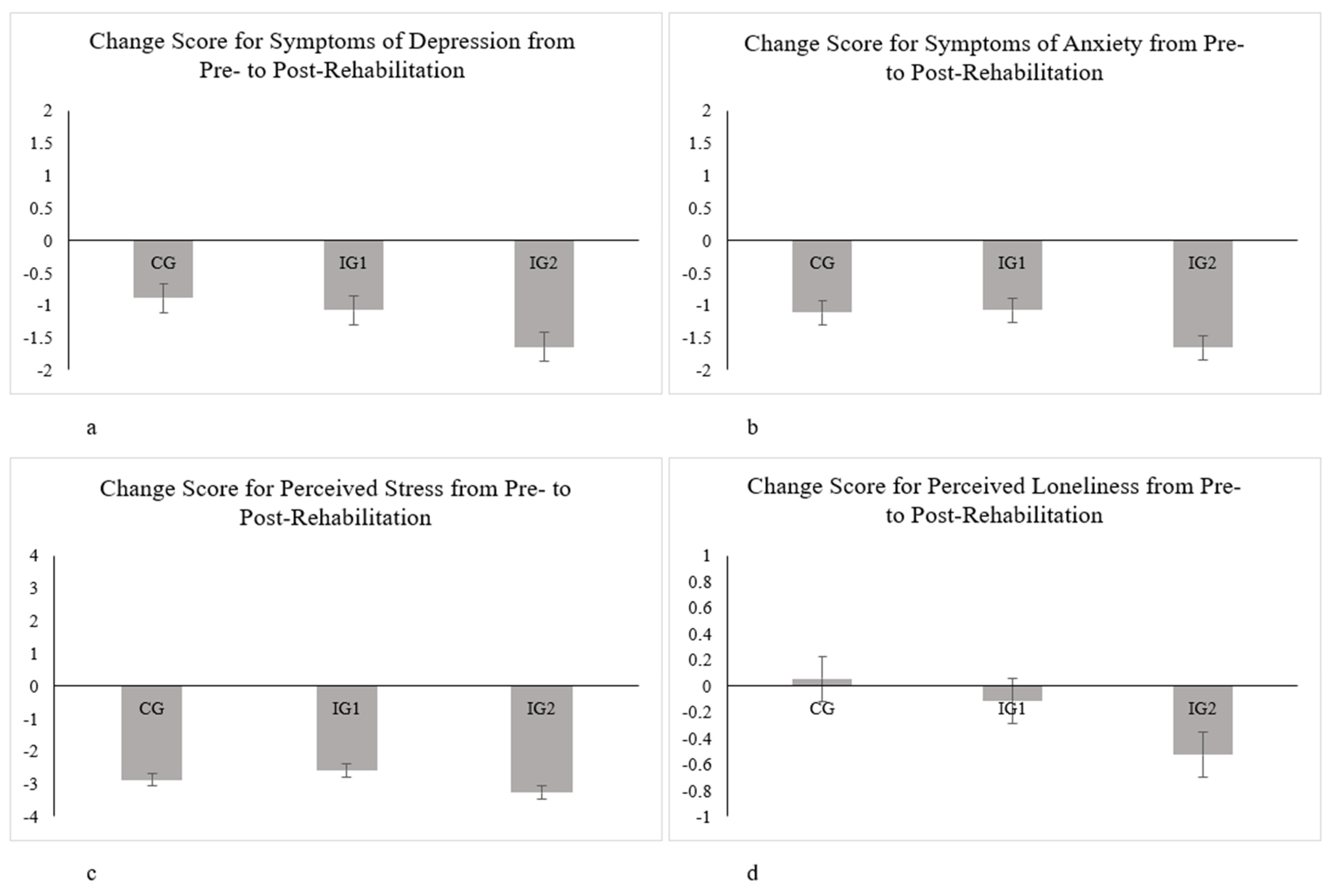
3.2. MMRM ANCOVA from before Rehabilitation Treatment to after Rehabilitation Treatment
3.3. Changes in Mental Health Symptoms with Regard to the Intervention Group from before Rehabilitation Treatment and after Rehabilitation Treatment
3.4. Effect Sizes
3.5. Association between Reaching Rehabilitation Goals Post-Rehabilitation and Satisfaction with Rehabilitation Post-Rehabilitation
3.6. Association between Perceived Communication and Satisfaction with Rehabilitation Post-Rehabilitation
4. Discussion
4.1. Reduction in Mental Health-Related Symptoms and the Effectiveness of Different Digital Trainings
4.2. Interpretation of Effect Sizes
4.3. Rehabilitation Goals
4.4. Limitations and Suggestions for Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Silver, R.C.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Balkhi, F.; Nasir, A.; Zehra, A.; Riaz, R. Psychological and behavioral response to the coronavirus (COVID-19) pandemic. Cureus 2020, 12, e7923. [Google Scholar] [CrossRef] [PubMed]
- Rogers, J.P.; Chesney, E.; Oliver, D.; Pollak, T.; McGuire, P.; Fusar-Poli, P.; Zandi, M.; Lewis, G.; David, A. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 611–627. [Google Scholar] [CrossRef]
- Fiorillo, A.; Gorwood, P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry 2020, 63, 1–4. [Google Scholar] [CrossRef] [Green Version]
- Van Rheenen, T.E.; Meyer, D.; Neill, E.; Phillipou, A.; Tan, E.J.; Toh, W.L.; Rossell, S.L. Mental health status of individuals with a mood-disorder during the COVID-19 pandemic in Australia: Initial results from the COLLATE project. J. Affect. Disord. 2020, 275, 69–77. [Google Scholar] [CrossRef]
- Chevance, A.; Gourion, D.; Hoertel, N.; Llorca, P.-M.; Thomas, P.; Bocher, R.; Moro, M.-R.; Laprévote, V.; Benyamina, A.; Fossati, P.; et al. Ensuring mental health care during the SARS-CoV-2 epidemic in France: A narrative review. L’encephale 2020, 46, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Hao, F.; Tan, W.; Jiang, L.; Zhang, L.; Zhao, X.; Zou, Y.; Hu, Y.; Luo, X.; Jiang, X.; McIntyre, R.S.; et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020, 87, 100–106. [Google Scholar] [CrossRef]
- Yao, H.; Chen, J.-H.; Xu, Y.-F. Rethinking online mental health services in China during the COVID-19 epidemic. Asian J. Psychiatry 2020, 50, 102015. [Google Scholar] [CrossRef]
- Baumeister, H.; Grässle, C.; Ebert, D.D.; Krämer, L.V. Blended psychotherapy—Verzahnte Psychotherapie: Das Beste aus zwei Welten? PiD Psychother. Dialog 2018, 19, 33–38. [Google Scholar] [CrossRef]
- Erbe, D.; Psych, D.; Eichert, H.C.; Riper, H.; Ebert, D.D. Blending face-to-face and internet-based interventions for the treatment of mental disorders in adults: Systematic review. J. Med. Internet Res. 2017, 19, e6588. [Google Scholar] [CrossRef] [Green Version]
- Kemmeren, L.L.; Van Schaik, A.; Smit, J.H.; Ruwaard, J.; Rocha, A.; Henriques, M.; Ebert, D.D.; Titzler, I.; Hazo, J.-B.; Dorsey, M.; et al. Unraveling the black box: Exploring usage patterns of a blended treatment for depression in a multicenter study. JMIR Ment. Health 2019, 6, e12707. [Google Scholar] [CrossRef] [PubMed]
- Kleiboer, A.; Smit, J.; Bosmans, J.; Ruwaard, J.; Andersson, G.; Topooco, N.; Berger, T.; Krieger, T.; Botella, C.; Baños, R.; et al. European comparative effectiveness research on blended depression treatment versus treatment-as-usual (E-COMPARED): Study protocol for a randomized controlled, non-inferiority trial in eight European countries. Trials 2016, 17, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schuster, R.; Pokorny, R.; Berger, T.; Topooco, N.; Laireiter, A.-R. The advantages and disadvantages of online and blended therapy: Survey study amongst licensed psychotherapists in Austria. J. Med. Internet Res. 2018, 20, e11007. [Google Scholar] [CrossRef] [PubMed]
- Titzler, I.; Saruhanjan, K.; Berking, M.; Riper, H.; Ebert, D.D. Barriers and facilitators for the implementation of blended psychotherapy for depression: A qualitative pilot study of therapists’ perspective. Internet Interv. 2018, 12, 150–164. [Google Scholar] [CrossRef] [PubMed]
- Friedl, N.; Krieger, T.; Chevreul, K.; Hazo, J.B.; Holtzmann, J.; Hoogendoorn, M.; Kleiboer, A.; Mathiasen, K.; Urech, A.; Riper, H.; et al. Using the personalized advantage index for individual treatment allocation to blended treatment or treatment as usual for depression in secondary care. J. Clin. Med. 2020, 9, 490. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. International Classification of Functioning, Disability and Health. 2001. Available online: http://apps.who.int/iris/bitstream/handle/10665/42407/9241545429.pdf?sequence=1 (accessed on 12 August 2021).
- Scheidt, C.E. Psychosomatic medicine in Germany. Int. J. Body Mind Cult. 2017, 4, 78–86. [Google Scholar]
- Becker, J.; Beutel, M.E.; Gerzymisch, K.; Schulz, D.; Siepmann, M.; Knickenberg, R.J.; Schmädeke, S.; Ferdinand, P.; Zwerenz, R. Evaluation of a video-based internet intervention as preparation for inpatient psychosomatic rehabilitation: Study protocol for a randomized controlled trial. Trials 2016, 17, 287. [Google Scholar] [CrossRef] [Green Version]
- Zwerenz, R.; Becker, J.; Knickenberg, R.J.; Hagen, K.; Dreier, M.; Wölfling, K.; Beutel, M. Enhancing inpatient psychotherapeutic treatment with online self-help: Study protocol for a randomized controlled trial. Trials 2015, 16, 98. [Google Scholar] [CrossRef] [Green Version]
- Zwerenz, R.; Gerzymisch, K.; Edinger, J.; Holme, M.; Knickenberg, R.J.; Spörl-Dönch, S.; Kiwus, U.; Beutel, M. Evaluation of an internet-based aftercare program to improve vocational reintegration after inpatient medical rehabilitation: Study protocol for a cluster-randomized controlled trial. Trials 2013, 14, 26. [Google Scholar] [CrossRef] [Green Version]
- Dahmen, A.; Gao, L.; Keller, F.M.; Lehr, D.; Becker, P.; Lippke, S. Psychosomatische Nachsorge: Curriculum Hannover online vs. Curriculum Hannover und vs. Care as Usual. 30th Rehabilitation Science Colloquium. German Congress for Rehabilitation Research. Participation and the world of work in special times. Online Congress, 22–25 March 2021. DRV Publications; pp. 195–197. Available online: https://www.deutsche-rentenversicherung.de/…/reha-kolloquium_node.html (accessed on 12 August 2021).
- Schmädeke, S.; Kockler, T.; Olbrich, D. DE-RENA—Rehabilitationsnachsorge mit einer Smartphone-App für depressive Patienten: Ergebnisse zur Akzeptanz und Wirksamkeit. Rehabil. Swissenschaftliches Kolloqu. 2019, 383–387. [Google Scholar]
- Yeomans, F.E.; Clarkin, J.F.; Kernberg, O.F. Transference-Focused Psyhotherapy for Borderline Personality Disorder: A Clinical Guide; American Psychiatric Publishing: Washington, DC, USA, 2015. [Google Scholar]
- Zerbo, E.; Cohen, S.; Bielska, W.; Caligor, E. Transference-focused psychotherapy in the general psychiatry residency: A useful and applicable model for residents in acute clinical settings. Psychodyn. Psychiatry 2013, 41, 163–181. [Google Scholar] [CrossRef]
- Moscara, M.; Bergonzini, E. Integrating the principles of transference-focused psychotherapy with psychiatric consultation for patients admitted to a general hospital: A clinical application of a psychotherapeutic tool. Int. J. Appl. Psychoanal. Stud. 2020, 18, 18–29. [Google Scholar] [CrossRef]
- Söllner, W.; Creed, F. European guidelines for training in consultation-liaison psychiatry and psychosomatics: Report of the EACLPP workgroup on training in consultation-liaison psychiatry and psychosomatics. J. Psychosom. Res. 2007, 62, 501–509. [Google Scholar] [CrossRef]
- Haverkampf, C.J. Communication-focused therapy for depression. J. Psychiatry Psychother. Commun. 2017, 6, 101–104. [Google Scholar]
- Haverkampf, C.J. Communication-focused therapy (CFT) for anxiety and panic attacks. J. Psychiatry Psychother. Commun. 2017, 6, 91–95. [Google Scholar]
- Rider, E.; Keefer, C.H. Communication skills competencies: Definitions and a teaching toolbox. Med. Educ. 2006, 40, 624–629. [Google Scholar] [CrossRef]
- Lippke, S.; Dahmen, A.; Gao, L.; Guza, E.; Nigg, C.R. To what extent is internet activity predictive of psychological well-being? Psychol. Res. Behav. Manag. 2021, 14, 207–219. [Google Scholar] [CrossRef]
- Luo, C.; Sanger, N.; Singhal, N.; Pattrick, K.; Shams, I.; Shahid, H.; Hoang, P.; Schmidt, J.; Lee, J.; Haber, S.; et al. A comparison of electronically-delivered and face to face cognitive behavioural therapies in depressive disorders: A systematic review and meta-analysis. EClinicalMedicine 2020, 24, 100442. [Google Scholar] [CrossRef]
- Karyotaki, E.; Kemmeren, L.; Riper, H.; Twisk, J.; Hoogendoorn, A.; Kleiboer, A.; Mira, A.; Mackinnon, A.; Meyer, B.; Botella, C.; et al. Is self-guided internet-based cognitive behavioural therapy (iCBT) harmful? An individual participant data meta-analysis. Psychol. Med. 2018, 48, 2456–2466. [Google Scholar] [CrossRef]
- Sasseville, M.; LeBlanc, A.; Boucher, M.; Dugas, M.; Mbemba, G.; Tchuente, J.; Chouinard, M.-C.; Beaulieu, M.; Beaudet, N.; Skidmore, B.; et al. Digital health interventions for the management of mental health in people with chronic diseases: A rapid review. BMJ Open 2021, 11, e044437. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The patient health questionnaire-2. Med. Care 2003, 41, 1284–1292. [Google Scholar] [CrossRef]
- Löwe, B.; Wahl, I.; Rose, M.; Spitzer, C.; Glaesmer, H.; Wingenfeld, K.; Schneider, A.; Brähler, E. A 4-item measure of depression and anxiety: Validation and standardization of the patient health questionnaire-4 (PHQ-4) in the general population. J. Affect. Disord. 2010, 122, 86–95. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Monahan, P.O.; Löwe, B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. 2007, 146, 317–325. [Google Scholar] [CrossRef]
- Löwe, B.; Kroenke, K.; Gräfe, K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J. Psychosom. Res. 2005, 58, 163–171. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385. [Google Scholar] [CrossRef]
- Cohen, S.; Williamson, G. Perceived stress in a probability sample of the United States. Soc. Psychol. Health 1988, 13, 31–67. [Google Scholar]
- Radloff, L.S. The CES-D scale. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Russell, D. UCLA loneliness scale (version 3): Reliability, validity, and factor structure. J. Pers. Assess. 1996, 66, 20–40. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics; Pearson: Boston, MA, USA, 2019. [Google Scholar]
- Field, A. Discovering Statistics Using SPSS; SAGE Publications: New York, NY, USA, 2009. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1988. [Google Scholar]
- Kirk, R.E. Practical significance: A concept whose time has come. Educ. Psychol. Meas. 1996, 56, 746–759. [Google Scholar] [CrossRef]
- Mittag, O.; Welti, F. Medizinische Rehabilitation im europäischen Vergleich und Auswirkungen des europäischen Rechts auf die deutsche Rehabilitation. Bundesgesundheitsblatt Gesundh. Gesundh. 2017, 60, 378–385. [Google Scholar] [CrossRef] [PubMed]
- Liebherz, S.; Rabung, S. Do patients’ symptoms and interpersonal problems improve in psychotherapeutic hospital treatment in Germany? A systematic review and meta-analysis. PLoS ONE 2014, 9, e105329. [Google Scholar] [CrossRef] [Green Version]
- Steffanowski, A.; Löschmann, C.; Schmidt, J.; Wittmann, W.W.; Nübling, R. Meta-Analyse der Effekte Stationärer Psychosomatischer Rehabilitation; Universität Mannheim: Mannheim, Germany, 2001. [Google Scholar]
- Keller, F.M.; Dahmen, A.; Derksen, C.; Kötting, L.; Lippke, S. Psychosomatic Rehabilitants and the general population during COVID-19: An online cross-sectional and longitudinal study of digital trainings. Internet Interv. Technol. Digit. Innov. Ment. Health Behav. Chang. 2021, in press. [Google Scholar]
- Stucki, G.; Ewert, T.; Cieza, A. Value and application of the ICF in rehabilitation medicine. Disabil. Rehabil. 2002, 24, 932–938. [Google Scholar] [CrossRef]
- Aboussouan, A.B.; Mandell, D.; Johnson, J.; Thompson, N.; Huffman, K.L. An interdisciplinary chronic pain rehabilitation program effectively treats impairment in sexual function, depression, alexithymia, and pain in women with chronic pelvic pain. J. Psychosom. Obstet. Gynecol. 2020, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Brakemeier, E.-L.; Radtke, M.; Engel, V.; Zimmermann, J.; Tuschen-Caffier, B.; Hautzinger, M.; Schramm, E.; Berger, M.; Normann, C. Overcoming treatment resistance in chronic depression: A pilot study on outcome and feasibility of the cognitive behavioral analysis system of psychotherapy as an inpatient treatment program. Psychother. Psychosom. 2014, 84, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Fenton, G.; Morley, S. A tale of two RCTs: Using randomized controlled trials to benchmark routine clinical (psychological) treatments for chronic pain. Pain 2013, 154, 2108–2119. [Google Scholar] [CrossRef] [PubMed]
- Nelson, B.W.; Pettitt, A.; Flannery, J.E.; Allen, N.B. Rapid assessment of psychological and epidemiological correlates of COVID-19 concern, financial strain, and health-related behavior change in a large online sample. PLoS ONE 2020, 15, e0241990. [Google Scholar] [CrossRef]
- Kobelt, A.; Grosch, E. Indikation zur ambulanten Nachsorge (curriculum Hannover) in der psychosomatischen Rehabilitation. Psychotherapeut 2005, 50, 340–346. [Google Scholar] [CrossRef]
- Streiner, D.L. Starting at the beginning: An introduction to coefficient alpha and internal consistency. J. Pers. Assess. 2003, 80, 99–103. [Google Scholar] [CrossRef]
| Measure | Group | Pre–Treatment | Post–Treatment |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Symptoms of Depression | |||
| CG | 3.48 (1.87) | 2.59 (1.70) | |
| IG1 | 3.43 (1.63) | 2.33 (1.68) | |
| IG2 | 3.67 (1.51) | 2.01 (1.08) | |
| Symptoms of Anxiety | |||
| CG | 3.73 (1.74) | 2.61 (1.69) | |
| IG1 | 3.56 (1.63) | 2.47 (1.66) | |
| IG2 | 3.83 (1.56) | 2.24 (1.36) | |
| Perceived Stress | |||
| CG | 9.84 (2.83) | 7.00 (3.35) | |
| IG1 | 9.35 (2.31) | 6.78 (3.27) | |
| IG2 | 9.68 (2.04) | 6.45 (2.96) | |
| Perceived Loneliness | |||
| CG | 4.51 (1.74) | 4.54 (1.66) | |
| IG1 | 4.29 (1.63) | 4.17 (1.66) | |
| IG2 | 4.56 (2.00) | 4.13 (1.64) | |
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ß | p | ß | p | ß | p | ß | p | ß | p | ß | p | |
| Age | 0.07 | 0.09 | 0.05 | 0.12 | 0.05 | 0.17 | 0.04 | 0.25 | 0.03 | 0.37 | 0.02 | 0.46 |
| Gender | 0.05 | 0.23 | 0.06 | 0.06 | 0.07 | 0.05 | 0.07 | 0.03 | 0.07 | 0.03 | 0.07 | 0.03 |
| Intervention Group | −0.01 | 0.84 | −0.03 | 0.32 | −0.02 | 0.55 | −0.02 | 0.51 | −0.02 | 0.61 | −0.03 | 0.45 |
| Reduction of psychological symptoms | – | – | 0.50 | <0.01 | 0.38 | <0.01 | 0.27 | <0.01 | 0.23 | <0.01 | 0.20 | <0.01 |
| Improvement of physiological status | – | – | – | – | 0.22 | <0.01 | 0.18 | <0.01 | 0.15 | <0.01 | 0.14 | <0.01 |
| Improvement of coping with stress and management of stress | – | – | – | – | – | – | 0.19 | <0.01 | 0.16 | <0.01 | 0.12 | 0.01 |
| Relaxation and resting | – | – | – | – | – | – | – | – | 0.15 | <0.01 | 0.14 | <0.01 |
| Improvement of one’s own confidence | – | – | – | – | – | – | – | – | – | – | 0.11 | 0.01 |
| R2 | 0.01 | 0.26 | 0.29 | 0.31 | 0.32 | 0.33 |
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| ß | p | ß | p | ß | p | ß | p | |
| Age | 0.05 | 0.24 | 0.02 | 0.50 | 0.01 | 0.78 | 0.01 | 0.98 |
| Gender | 0.04 | 0.29 | 0.01 | 0.76 | 0.02 | 0.55 | 0.02 | 0.47 |
| Intervention Group | −0.01 | 0.89 | 0.01 | 0.89 | 0.01 | 0.78 | 0.01 | 0.91 |
| Taking worries and fears seriously | – | – | 0.48 | <0.01 | 0.29 | <0.01 | 0.25 | <0.01 |
| Early enough discussion on treatment steps and plans | – | – | – | – | 0.28 | <0.01 | 0.22 | <0.01 |
| Sufficient provision of information | – | – | – | – | – | – | 0.12 | 0.03 |
| R2 | 0.01 | 0.24 | 0.28 | 0.29 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Keller, F.M.; Dahmen, A.; Derksen, C.; Kötting, L.; Lippke, S. Implementing Digital Trainings within Medical Rehabilitations: Improvement of Mental Health and Synergetic Outcomes with Healthcare Service. Int. J. Environ. Res. Public Health 2021, 18, 8936. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18178936
Keller FM, Dahmen A, Derksen C, Kötting L, Lippke S. Implementing Digital Trainings within Medical Rehabilitations: Improvement of Mental Health and Synergetic Outcomes with Healthcare Service. International Journal of Environmental Research and Public Health. 2021; 18(17):8936. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18178936
Chicago/Turabian StyleKeller, Franziska Maria, Alina Dahmen, Christina Derksen, Lukas Kötting, and Sonia Lippke. 2021. "Implementing Digital Trainings within Medical Rehabilitations: Improvement of Mental Health and Synergetic Outcomes with Healthcare Service" International Journal of Environmental Research and Public Health 18, no. 17: 8936. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18178936







