Recommendations for Safe Dental Care: A Systematic Review of Clinical Practice Guidelines in the First Year of the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Sources of Information
2.4. Selection of Guidelines
2.5. Data Charting Process
2.6. Synthesis of the Results
3. Results
3.1. Literature Search
3.2. Features of the Guidelines Included
3.3. Summary of Recommendations
3.3.1. Recommendations Regarding Triage and General Recommendations for Patients
3.3.2. Recommendations for the Waiting Room Area
3.3.3. Recommendations Regarding Personal Protective Equipment (PPE)
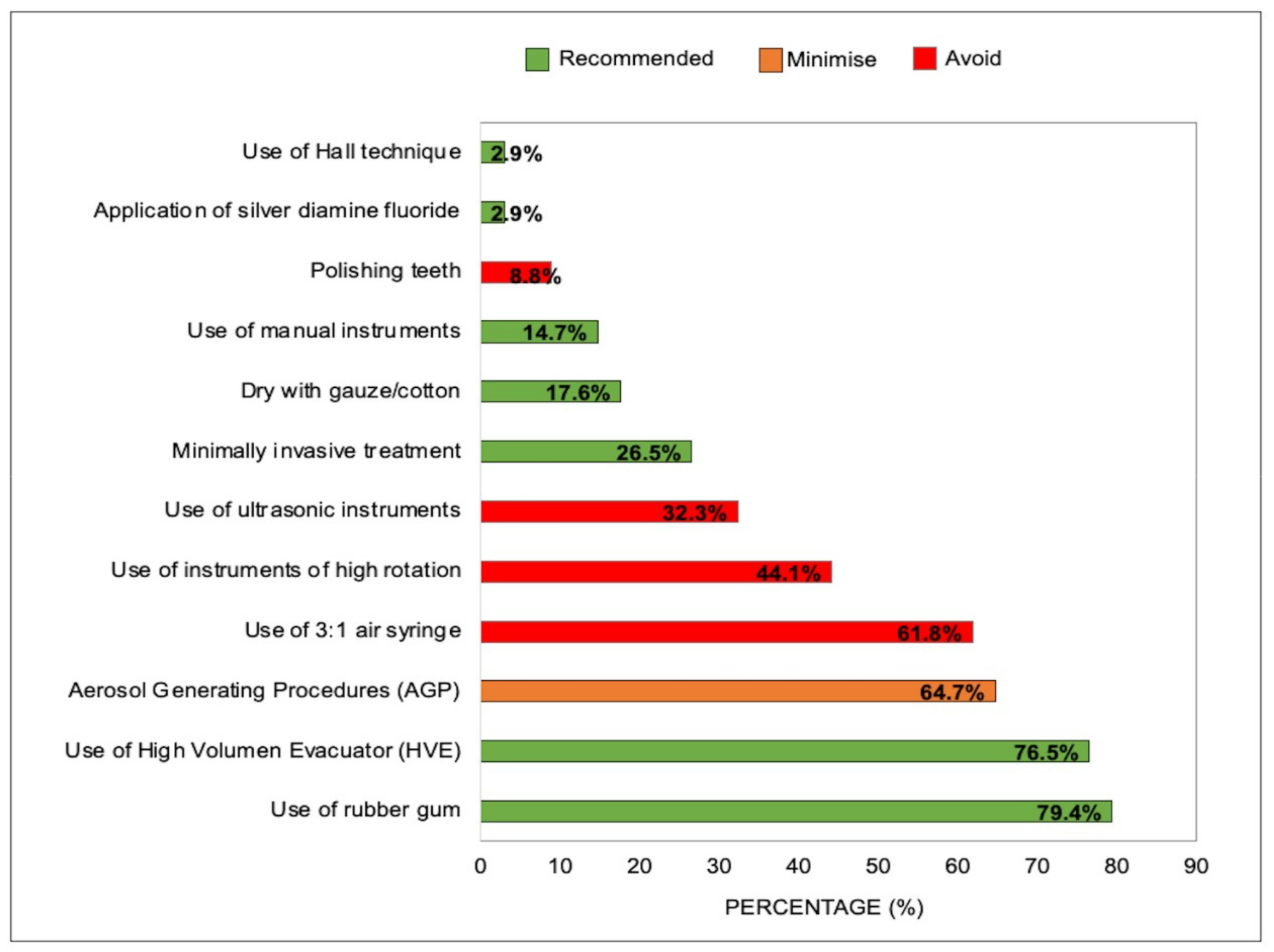
3.3.4. Recommendations for the Reduction in Aerosols during Dental Procedures
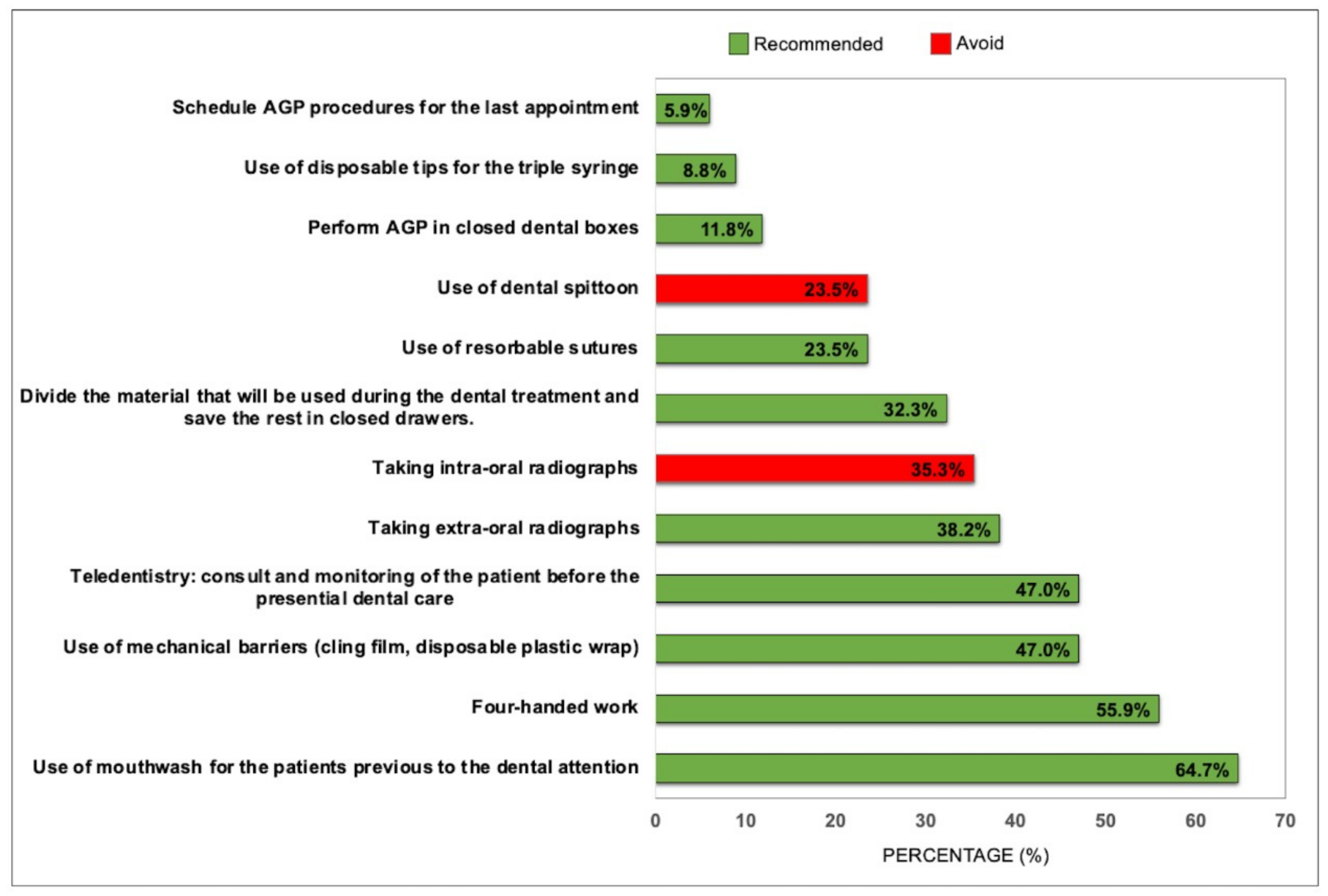
3.3.5. Recommendations to Minimize the Risk of Contamination
3.3.6. Recommendations after Dental Care
3.3.7. Recommendations on Dental Treatment Room Ventilation
3.3.8. Recommendations for Bathrooms in Dental Clinics
3.3.9. Recommendations for Treatment Rooms with More Than One Dental Chair
4. Discussion
4.1. Study Limitations
4.2. Clinical Implications and Future Prospects
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vokó, Z.; Pitter, J.G. The effect of social distance measures on COVID-19 epidemics in Europe: An interrupted time series analysis. GeroScience 2020, 42, 1075–1082. [Google Scholar] [CrossRef] [PubMed]
- Sharma, O.; Sultan, A.A.; Ding, H.; Triggle, C.R. A Review of the Progress and Challenges of Developing a Vaccine for COVID-19. Front. Immunol. 2020, 11, 2413. [Google Scholar] [CrossRef] [PubMed]
- Coulthard, P.; Thomson, P.; Dave, M.; Coulthard, F.P.; Seoudi, N.; Hill, M. The COVID-19 pandemic and dentistry: The clinical, legal and economic consequences-part 2: Consequences of withholding dental care. Br. Dent. J. 2020, 229, 801–805. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.; Zhu, J.; Liu, J.; Zhang, X.; Liu, Y.; Yang, Q. Hospital biosecurity capacitation: Analysis and recommendations for the prevention and control of COVID-19. J. Biosaf. Biosec. 2020, 2, 5–9. [Google Scholar] [CrossRef]
- Rossato, M.D.S.; Gregorio, D.; de Almeida-Pedrin, R.R.; Maia, L.P.; Poli, R.C.; Berger, S.B.; Fernandes, T.M.F. Evaluation of Dental Practices Changes During the COVID-19 Pandemic in Brazil. Eval. Health Prof. 2021, 44, 192–197. [Google Scholar] [CrossRef]
- Tarighi, P.; Eftekhari, S.; Chizari, M.; Sabernavaei, M.; Jafari, D.; Mirzabeigi, P. A review of potential suggested drugs for coronavirus disease (COVID-19) treatment. Eur. J. Pharmacol. 2021, 895, 173890. [Google Scholar] [CrossRef]
- Wise, J. Covid-19: The E484K mutation and the risks it poses. BMJ 2021, 372, n359. [Google Scholar] [CrossRef]
- Banakar, M.; Lankarani, K.B.; Jafarpour, D.; Moayedi, S.; Banakar, M.H.; MohammadSadeghi, A. COVID-19 transmission risk and protective protocols in dentistry: A systematic review. BMC Oral Health 2020, 20, 275. [Google Scholar] [CrossRef]
- Jiang, C.; Duangthip, D.; Auychai, P.; Chiba, M.; Folayan, M.; Hamama, H.; Kamnoedboon, P.; Lyons, K.; Matangkasombut, O.; Mathu-Muju, K. Changes in Oral Health Policies and Guidelines During the COVID-19 Pandemic. Front. Oral Health 2021, 2, 668444. [Google Scholar] [CrossRef]
- Schlenz, M.A.; Schmidt, A.; Wöstmann, B.; May, A.; Howaldt, H.-P.; Albert, D.; Ziedorn, D.; Krämer, N.; Schulz-Weidner, N. Perspectives from Dentists, Dental Assistants, Students, and Patients on Dental Care Adapted to the COVID-19 Pandemic: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 3940. [Google Scholar] [CrossRef]
- Estrich, C.G.; Gurenlian, J.R.; Battrell, A.; Bessner, S.K.; Lynch, A.; Mikkelsen, M.; Morrissey, R.; Araujo, M.W.; Vujicic, M. COVID-19 prevalence and related practices among dental hygienists in the United States. J. Dent. Hyg. Assoc. 2021, 95, 6–16. [Google Scholar]
- Clarkson, J.; Ramsay, C.; Richards, D.; Robertson, C.; Aceves-Martins, M.; Group, C.W. Aerosol generating procedures and their mitigation in international dental guidance documents-a rapid review. Cochrane Oral Health 2020. Available online: https://oralhealth.cochrane.org/news/aerosol-generating-procedures-and-their-mitigation-international-guidance-documents (accessed on 15 January 2021).
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alonso-Coello, P.; Aravena-Rivas, Y.; Deana, N.; Espinoza-Espinoza, G.; Muñoz-Milán, P.; Seiffert, A.; Zaror, C. Systematic Quality Assessment of Clinical Practice Guidelines to Minimize the Risk of Covid-19 Transmission during Dental Care. Heliyon 2021. [Google Scholar] [CrossRef]
- Office of Chief Dental Officer England (OCDO); National Health Services (NHS). Standard Operating Procedure. Transition to Recovery. A Phased Transition for Dental Practices towards the Resumption of the Full Range of Dental Provision. Available online: https://www.england.nhs.uk/coronavirus/publication/dental-standard-operating-procedure-transition-to-recovery/ (accessed on 15 January 2021).
- National Health Services (NHS). COVID-19 Guidance and Standard Operating Procedure: For the Provision of Urgent Dental Care in Primary Care Dental Settings. 2020. Available online: https://www.england.nhs.uk/coronavirus/primary-care/dental-practice/ (accessed on 15 January 2021).
- College of General Dentistry Practice Faculty of General Dental. Implications of COVID-19 for the Safe Management of General Dental Practice A Practical Guide. Available online: https://www.fgdp.org.uk/implications-covid-19-safe-management-general-dental-practice-practical-guide (accessed on 10 January 2021).
- The College of Dental Surgeons of Saskatchewan. CDSS Alert—COVID-19 Pandemic: IPC Interim Protocol Update. Available online: http://www.sdta.ca/mrws/filedriver/20201207_CDSS_Alert_Phase_5_IPC_Interim_Protocol_Update.pdf (accessed on 20 January 2021).
- Dental Association of Prince Edward Island. Member of the Canadian Dental Association (CDA). Return-to-Practice Office Manual. Adapting the Dental Office to the COVID-19 Pandemic. Available online: http://www.cda-adc.ca/_files/about/covid-19/PEI_Return%20to%20Practice%20Office%20Manual%20(PEI)%20-%202020-05-10.pdf (accessed on 1 March 2021).
- Public Health Scotland National Services Scotland (NHS). Novel Coronavirus (COVID-19) Guidance for Primary Care. Management of Patients in Primary Care. Including General Medical Practice, General Dental Practice, Optometry and Pharmacy; NHS: Edinburgh, UK, 2020.
- Scottish Dental Clinical Effectiveness Programme (SDCEP). Resuming General Dental Services Following COVID-19 Shutdown a Guide and Implementation Tools for General Dental Practice for Phase 2 of Dental Services Remobilisation. Available online: https://www.sdcep.org.uk/wp-content/uploads/2020/06/SDCEP-Resuming-General-Dental-Services-Following-COVID-19-Shutdown-Update-120620.pdf (accessed on 18 January 2021).
- Center for Disease Control Prevention. Guidance for Dental Settings. Interim Infection Prevention and Control Guidance for Dental Settings during the Coronavirus Disease 2019 (COVID-19) Pandemic. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html (accessed on 25 March 2021).
- American Dental Association (ADA). Return to Work Interim Guidance Toolkit. Available online: https://pages.ada.org/return-to-work-toolkit-american-dental-association (accessed on 12 April 2021).
- European Centre for Disease Prevention and Control (ECDC). COVID-19 Infection Prevention and Control Measures For Primary Care, Including General Practitioner Practices, Dental Clinics and Pharmacy Settings—First Update; ECDC: Solna, Sweden, 2020. [Google Scholar]
- Dental Council of India. Advisory: Dental Clinics Protocols. Available online: http://dciindia.gov.in/Admin/NewsArchives/Dental Clinics Protocols Final.pdf (accessed on 9 March 2021).
- Ministry of Health Dental Council. Guidelines for Oral Health Services at COVID-19 Alert Level 1. Available online: https://www.dcnz.org.nz/covid-19/guidelines-for-oral-health-services-at-covid-19-alert-levels/ (accessed on 16 March 2021).
- Alharbi, A.; Alharbi, S.; Alqaidi, S. Guidelines for Dental Care Provision during the COVID-19 Pandemic. Saudi Dent. J. 2020, 32, 181–186. [Google Scholar] [CrossRef]
- Ministerio de Salud de Argentina. COVID-19. Recomendaciones en Odontología. Available online: http://iah.salud.gob.ar/doc/449.pdf (accessed on 16 March 2021).
- Asociación Chilena de Enseñanza de la Odontología (ACHEO). Normativa de Contigencia COVID-19.
- Subsecretaría de Salud Pública División de Prevención y Control de Enfermedades Departamento de Salud Bucal Ministerio de Salud Gobierno de Chile. Orientaciones Para Atención Odontológica en Fase IV COVID-19. Available online: http://bibliodigital.saludpublica.uchile.cl:8080/dspace/bitstream/handle/123456789/631/17_ORIENTACIONES-ATENCION-ODONTOLOGICAS-COVID-19-.pdf?sequence=1&isAllowed=y (accessed on 25 January 2021).
- Ministerio de Salud Publica de Costa Rica Caja Costarricense de Seguro Social Colegio de Cirujanos Dentistas Ministerio de Justicia y Paz. LS-SS-008. Lineamiento Técnico Para la Prevención y Contención de COVID-19 Para Odontólogos y Personal Auxiliar de Costa Rica. Available online: https://www.ministeriodesalud.go.cr/sobre_ministerio/prensa/docs/ls_ss_008_lineamiento_tecnico_prevencion_contencion_odontologos_personal_auxiliar_12082020.pdf (accessed on 5 January 2021).
- Ministerio de Salud Instituto Ecuatoriano de Seguridad Social Fuerzas Armadas Sociedad Ecuatoriana de Salud Pública Federación Odontológica Ecuatoriana. Protocolo Para Atención Odontológica en Emergencias y Urgencias Odontológicas Durante la Emergencia Sanitaria por COVID-19. Available online: https://www.salud.gob.ec/wp-content/uploads/2020/06/PROTOCOLO-PARA-ATENCION-ODONTOLOGICA-DURANTE-LA-EMERGENCIA-SANITARIA-POR-COVID.pdf (accessed on 12 March 2021).
- Ministerio de Salud Gobierno de El Salvador. Lineamientos Técnicos Para la Atención Odontológica Posterior a la Emergencia por COVID-19. Available online: http://asp.salud.gob.sv/regulacion/pdf/derogados/lineamientostecnicosparalaatencionodontologicaposterioralaemergenciaporCOVID19-Acuerdo1408.pdf (accessed on 23 January 2021).
- Ministerio de Salud República de Panamá. Guía Para el Manejo Odontológico de Pacientes Sospechosos o Confirmados por COVID-19 en las Instalaciones de Salud. Available online: https://panama.campusvirtualsp.org/covid-19/respuesta-de-los-servicios-de-salud (accessed on 25 April 2021).
- Ministerio de Salud Pública y Bienestar Social Gobierno Nacional. Protocolo Para Atención Odontológica de Retorno Gradual. Available online: https://www.mspbs.gov.py/dependencias/portal/adjunto/76dd5d-Protocolodeatencinodontolgicaderetornogradual07.05.20.pdf (accessed on 18 April 2021).
- Colegio Odontológico del Perú Consejo Administrativo Nacional. Protocolo de Bioseguridad Para el Cirujano Dentista Durante y Post Pandemia COVID-19. Available online: http://www.cop.org.pe/wp-content/uploads/2020/04/PROTOCOLO-DE-BIOSEGURIDAD-PARA-EL-CIRUJANO-DENTISTA.pdf (accessed on 6 April 2021).
- Instituto de Evaluación de Tecnologías en Salud e Investigación (IETSI). Recomendaciones Clínicas Para Realizar Procedimientos en Odontoestomatología en el Contexto de Pandemia por COVID-19. Available online: http://www.essalud.gob.pe/ietsi/pdfs/guias/Recomendaciones_OdontoestomatologIa_COVID.pdf (accessed on 2 April 2021).
- del Carmen Trullols-Casas, M.; Ausina-Márquez, V.; Martínez-Beneyto, Y.; Martínez-Sanz, E.; Llamas-Ortuño, E.; Expósito-Delgado, A.; Almerich-Torres, T.; Mateos-Moreno, V.; Blanco-González, J.-M. Recommendations by the Spanish Society of Epidemiology and Oral Public Health (SESPO) for the Healthcare Adaptation of Public Health Dental Clinics in Spain during the COVID-19 Pandemic. J. Clin. Exp. Dent. 2020, 12, e1183. [Google Scholar] [CrossRef]
- Consejo de Dentistas de España. Plan Estratégico de Acción Para el Periodo de Desescalada COVID-19. Available online: https://www.consejodentistas.es/comunicacion/actualidad-consejo/notas-de-prensa-consejo/item/1783-plan-estrategico-de-accion-para-clinicas-dentales-durante-el-periodo-de-desescalada.html (accessed on 13 April 2021).
- Ministerio de Salud Pública de Uruguay. Recomendaciones del Ministerio de Salud Pública Para Profesionales Odontólogos e Higienistas Dentales. Prevención y Control de Coronavirus COVID-19. Available online: https://www.gub.uy/ministerio-salud-publica/sites/ministerio-salud-publica/files/documentos/noticias/MSP_RECOMENDACIONES_ODONTOLOGOS_HIGIENISTAS_DENTALES.pdf (accessed on 28 January 2021).
- Colegio Estomatológico de Guatemala. Protocolo de Bioseguridad Odontológica con Énfasis en COVID-19. Available online: https://colegioestomatologico.gt/wp-content/uploads/2020/08/Protocolo-de-Bioseguridad-Odontologica-con-enfasis-en-COVID-19-1.pdf (accessed on 20 March 2021).
- Conselho Regional de Odontologia de São Paulo. Orientação de Biossegurança. Adequações Técnicas em Tempos de COVID-19. Available online: http://www.crosp.org.br/uploads/paginas/38f65fd62bd4e5e56b16e859ada6c751.pdf (accessed on 12 April 2021).
- Agência Nacional de Vigilância Sanitária. ANVISA. Nota técnica GVIMS/GGTES/ANVISA No 04/2020. Orientações Para Serviços de Saúde: Medidas de Prevenção e Controle que Devem ser Adotadas Durante a Asistencia aos Casos Suspeitos ou Confirmados de Infeccção pelo Novo Coronavírus (SARS- CoV-2). Available online: http://renastonline.ensp.fiocruz.br/sites/default/files/arquivos/recursos/nota_tecnica_n_04-2020_gvims-ggtes-anvisa-atualizada-27-10-2020.pdf (accessed on 16 April 2021).
- Secretaria de Estado da Saúde Superintendência de Planeamento em Saúde Diretoria de Atenção Primária à Saúde Núcleo Estadual de Saúde Bucal Estado de Santa Catarina. Nota Técnica Conjunta nº014/2020-DAPS/DIVS/DIVE/SES/COMSES/SC. Recomendações ao atendimento odontológico no SUS em Santa Catarina. Available online: https://www.saude.sc.gov.br/coronavirus/arquivos/NotaTecnicaConjunta014-2020-daps-divs-dive-ses-cosems.pdf (accessed on 8 March 2021).
- Ordem dos Médicos Dentistas de Portugal, Nacional de Promoção da Saude Oral, Programa Nacional de Prevenção e Controlo de Infecções e das Resistências aos Antimicrobianos. COVID-19: Procedimentos em Clínicas, Consultórios ou Serviços de Saúde Oral dos Cuidados de Saúde Primários, Setor Social e Privado. Available online: https://www.dgs.pt/directrizes-da-dgs/orientacoes-e-circulares-informativas/orientacao-n-0222020-de-01052020-pdf.aspx (accessed on 12 March 2021).
- Conselho Federal de Odontologia ITI Brasil, ITI México Faculdade ILAPEO, Consejo Mexicano de Rehabilitación Oral y Maxilofacial a.c. AMP, APP, Universidad de Concepción Centro de Rehabilitación Oral Avanzada e Implantología-Facultad de Odontología. Manual de Buenas Prácticas en Bioseguridad para Ambientes Odontológicos. Available online: http://webdental.cl/descargas/manual-covid/Manual-de-Buenas-Practicas-en-Bioseguridad-para-Ambientes-Odontologicos.pdf (accessed on 23 March 2021).
- Asociación Latinoamericana de Odontopediatria. Ruta de Atención Para Procedimientos de Odontología Pediátrica Durante la Etapa de Confinamiento o Cuarentena de la Pandemia COVID-19. Rev. Odontoped. Latinoam. 2020, 10, 1–13. [Google Scholar]
- World Health Organization (WHO). Considerations for the Provision of Essential Oral Health Services in the Context of COVID-19: Interim Guidance; World Health Organization (WHO): Geneva, Switzerland, 2020. [Google Scholar]
- Kowalski, S.C.; Morgan, R.L.; Falavigna, M.; Florez, I.D.; Etxeandia-Ikobaltzeta, I.; Wiercioch, W.; Zhang, Y.; Sakhia, F.; Ivanova, L.; Santesso, N. Development of rapid guidelines: 1. Systematic survey of current practices and methods. Health Res. Policy Syst. 2018, 16, 61. [Google Scholar] [CrossRef]
- World Health Organization. WHO Handbook for Guideline Development; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Alene, M.; Yismaw, L.; Assemie, M.A.; Ketema, D.B.; Mengist, B.; Kassie, B.; Birhan, T.Y. Magnitude of asymptomatic COVID-19 cases throughout the course of infection: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0249090. [Google Scholar] [CrossRef]
- Chu, D.K.; Akl, E.A.; Duda, S.; Solo, K.; Yaacoub, S.; Schünemann, H.J.; Chu, D.K.; Akl, E.A.; El-harakeh, A.; Bognanni, A.; et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet 2020, 395, 1973–1987. [Google Scholar] [CrossRef]
- Araujo, M.W.; Estrich, C.G.; Mikkelsen, M.; Morrissey, R.; Harrison, B.; Geisinger, M.L.; Ioannidou, E.; Vujicic, M. COVID-2019 among dentists in the United States: A 6-month longitudinal report of accumulative prevalence and incidence. J. Am. Dent. Assoc. 2021, 152, 425–433. [Google Scholar] [CrossRef]
- Polednik, B. Exposure of staff to aerosols and bioaerosols in a dental office. Build. Environ. 2021, 187, 107388. [Google Scholar] [CrossRef]
- Chatoutsidou, S.E.; Saridaki, A.; Raisi, L.; Katsivela, E.; Tsiamis, G.; Zografakis, M.; Lazaridis, M. Airborne particles and microorganisms in a dental clinic: Variability of indoor concentrations, impact of dental procedures, and personal exposure during everyday practice. Indoor Air. 2021, 3, 1164–1177. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.A.; Jouhar, R. Dissemination of Aerosol and Splatter in Clinical Environment during Cavity Preparation: An In Vitro Study. Int. J. Environ. Res. Public Health 2021, 18, 3773. [Google Scholar] [CrossRef]
- Samaranayake, L.P.; Fakhruddin, K.S.; Buranawat, B.; Panduwawala, C. The efficacy of bio-aerosol reducing procedures used in dentistry: A systematic review. Acta Odontol. Scand. 2021, 79, 69–80. [Google Scholar] [CrossRef]
- Elmahgoub, F.; Coll, Y. Could certain mouthwashes reduce transmissibility of COVID-19? Evid. Based Dent. 2021, 22, 82–83. [Google Scholar] [CrossRef] [PubMed]
- Cavalcante-Leão, B.L.; de Araujo, C.-M.; Basso, I.-B.; Schroder, A.-G.-D.; Guariza-Filho, O.; Ravazzi, G.-C.; Gonçalves, F.-M.; Zeigelboim, B.-S.; Santos, R.-S.; Stechman-Neto, J. Is there scientific evidence of the mouthwashes effectiveness in reducing viral load in Covid-19? A systematic review. J. Clin. Exp. Dent. 2021, 13, e179. [Google Scholar] [CrossRef] [PubMed]
- Nazarenko, Y. Air filtration and SARS-CoV-2. Epidemiol. Health 2020, 42, e2020049. [Google Scholar] [CrossRef]
- Tang, J.W.; Bahnfleth, W.P.; Bluyssen, P.M.; Buonanno, G.; Jimenez, J.L.; Kurnitski, J.; Li, Y.; Miller, S.; Sekhar, C.; Morawska, L. Dismantling myths on the airborne transmission of severe acute respiratory syndrome coronavirus (SARS-CoV-2). J. Hosp. Infect. 2021, 110, 89–96. [Google Scholar] [CrossRef]
- Mackenzie, D. Ultraviolet light fights new virus. Engineering 2020, 6, 851–853. [Google Scholar] [CrossRef]
- Temkin, E.; Schwaber, M.J.; Solter, E.; Vaturi, A.; Hen, D.; Lugassy, C.G.; Teitler, N.; Nutman, A.; Rubinovitch, B.; Ben-Zvi, H. Extremely low prevalence of asymptomatic COVID-19 among healthcare workers caring for COVID-19 patients in Israeli hospitals: A cross-sectional study. Clin. Microbiol. Infect. 2021, 27, e130.e1–e130.e4. [Google Scholar] [CrossRef] [PubMed]
- Johnson, I.; Gallagher, J.E.; Verbeek, J.H.; Innes, N. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Oral Health 2020, 4, CD011621. [Google Scholar] [CrossRef]
- Gallagher, J.E.; Johnson, I.; Verbeek, J.H.; Clarkson, J.E.; Innes, N. Relevance and paucity of evidence: A dental perspective on personal protective equipment during the COVID-19 pandemic. Br. Dent. J. 2020, 229, 121–124. [Google Scholar] [CrossRef] [PubMed]
- Barycka, K.; Szarpak, L.; Filipiak, K.J.; Jaguszewski, M.; Smereka, J.; Ladny, J.R.; Turan, O. Comparative effectiveness of N95 respirators and surgical/face masks in preventing airborne infections in the era of SARS-CoV2 pandemic: A meta-analysis of randomized trials. PLoS ONE 2020, 15, e0242901. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Olonisakin, T.F.; Pribis, J.P.; Zupetic, J.; Yoon, J.H.; Holleran, K.M.; Jeong, K.; Shaikh, N.; Rubio, D.M.; Lee, J.S. A checklist is associated with increased quality of reporting preclinical biomedical research: A systematic review. PLoS ONE 2017, 12, e0183591. [Google Scholar] [CrossRef] [Green Version]
- Singh, P.; Pal, K.; Chakravraty, A.; Ikram, S. Execution and viable applications of Face shield “a safeguard” against viral infections of cross-protection studies: A comprehensive review. J. Mol. Struct. 2021, 1238, 130443. [Google Scholar] [CrossRef]
- Mustafa, R.A.; Garcia, C.A.C.; Bhatt, M.; Riva, J.J.; Vesely, S.; Wiercioch, W.; Nieuwlaat, R.; Patel, P.; Hanson, S.; Newall, F.; et al. How to use GRADE when there is "no" evidence? A case study of the expert evidence approach. J. Clin. Epidemiol. 2021, 137, 231–235. [Google Scholar] [CrossRef]
- Norris, S.L.; Sawin, V.I.; Ferri, M.; Raques Sastre, L.; Porgo, T.V. An evaluation of emergency guidelines issued by the World Health Organization in response to four infectious disease outbreaks. PLoS ONE 2018, 13, e0198125. [Google Scholar]
- Akl, E.A.; Morgan, R.L.; Rooney, A.A.; Beverly, B.; Katikireddi, S.V.; Agarwal, A.; Alper, B.S.; Alva-Diaz, C.; Amato, L.; Ansari, M.T. Developing trustworthy recommendations as part of an urgent response (1–2 weeks): A GRADE concept paper. J. Clin. Epidemiol. 2021, 129, 1–11. [Google Scholar] [CrossRef]
- Deana, N.F.; Zaror, C.; Seiffert, A.; Aravena-Rivas, Y.; Muñoz-Millán, P.; Espinoza-Espinoza, G.; Pineda, P.; Alonso-Coello, P. Quality appraisal of clinical practice guidelines on dental services provision during the first months ot the Covid-19 pandemic. J. Evid. Based Dent. Pract. 2021, 101633. [Google Scholar] [CrossRef]
- Limeres Posse, J.; van Harten, M.T.; Mac Giolla Phadraig, C.; Diniz Freitas, M.; Faulks, D.; Dougall, A.; Daly, B.; Diz Dios, P. The Impact of the First Wave of the COVID-19 Pandemic on Providing Special Care Dentistry: A Survey for Dentists. Int. J. Environ. Res. Public Health 2021, 18, 2970. [Google Scholar] [CrossRef] [PubMed]
- Estrich, C.G.; Mikkelsen, M.; Morrissey, R.; Geisinger, M.L.; Ioannidou, E.; Vujicic, M.; Araujo, M.W. Estimating COVID-19 prevalence and infection control practices among US dentists. J. Am. Dent. Assoc. 2020, 151, 815–824. [Google Scholar] [CrossRef] [PubMed]
- Martinho, F.C.; Griffin, I.L. A cross-sectional survey on the impact of Coronavirus disease 2019 on the clinical practice of endodontists across the United States. J. Endod. 2021, 47, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Kamerow, D. Covid-19: The crisis of personal protective equipment in the US. BMJ 2020, 369, m1367. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Guide Title | Country | Organization | Language | Publication Date/Update | Reference |
|---|---|---|---|---|---|
| COVID-19. Recommendations for dental care. (COVID-19. Recomendaciones en Odontología) | Argentina | Health Ministry of Argentina | Spanish | 10 June 2020 (1st Edition) | [28] |
| Manual of Good Practices in Biosecurity for dental environments. (Manual de buenas prácticas en bioseguridad para ambientes odontológicos) | Brazil | Federal Dental Council, ITI Brazil, ITI Mexico ILAPEO Faculty, Mexican Council of Oral and Maxillofacial Rehabilitation, AMP, APP, University of Concepción, Centre for Advanced Oral Rehabilitation and Implantology–Dental Faculty | Spanish, Portuguese | 26 May 2020 (2nd Edition) | [46] |
| Biosecurity Guidelines. Technical adaptations in times of COVID-19. (Orientação de biossegurança. Adequações técnicas em tempos de COVID-19) | Brazil | São Paulo Regional Dental Council | Portuguese | July 2020 (2nd Edition) | [42] |
| Technical note GVIMS/GGTES/ANVISA n. 04/2020 Guidelines for health services: prevention and control measures that should be adopted during attention to suspected or confirmed cases of infection by the new coronavírus (SARS-CoV-2). (Nota técnica GVIMS/GGTES/ANVISA n. 04/2020 Orientações para serviços de saúde: medidas de prevenção e controle que devem ser adotadas durante a assistência aos casos suspeitos ou confirmados de infeccção pelo novo coronavírus (SARS-CoV-2)). | Brazil | National Health Vigilance Agency-ANVISA | Portuguese | 27 December 2020 (5th Edition) | [43] |
| Joint technical note nº014/2020-DAPS/DIVS/DIVE/SES/COMSES/SC. Recommendations for dental attention to SUS in Santa Catarina (Nota técnica conjunta nº014/2020-DAPS/DIVS/DIVE/SES/COMSES/SC. Recomendações ao atendimento odontológico do SUS em Santa Catarina) | Brazil | Health Secretary of Santa Catarina | Portuguese | 15 October 2020 (2st Edition) | [44] |
| CDSS Alert–COVID-19 Pandemic: IPC Interim Protocol Update. | Canada | The College of Dental Surgeons of Saskatchewan | English | 7 December 2020 (2nd Edition) | [18] |
| Return-to-practice office manual. Adapting the dental office to the COVID-19 Pandemic | Canada | Dental Association of Prince Edward Island. Member of the Canadian Dental Association [19] | English | 10 May 2020 (1st Edition) | [19] |
| Rules for attention during the COVID-19 epidemic. (Normativa de atención contingencia COVID-19) | Chile | Chilean Dentistry Teaching Association [29] | Spanish | 1 June 2020 (1st Edition) | [29] |
| Guidelines for dental attention in COVID-19 Phase IV. (Orientaciones para atención odontológica en fase IV COVID-19) | Chile | Public Health Undersecretary, Disease Prevention and Control Division, Oral Health Department, Health Ministry, Government of Chile | Spanish | 17 May 2020 | [30] |
| LS-SS-008. Technical Guidelines for the prevention and containment of COVID-19 for dentists and auxiliary staff in Costa Rica. (LS-SS-008. Lineamiento técnico para la prevención y contención de COVID-19 para odontólogos y personal auxiliar de Costa Rica) | Costa Rica | Health Ministry, Costa Rican Social Security Fund, College of Dental surgeons, Justice and Peace Ministry | Spanish | 12 August 2020 (2nd Edition) | [31] |
| Protocol for dental attention in urgent and emergency cases during the COVID–19 health emergency.(Protocolo para atención odontológica en emergencias y urgencias odontológicas durante la emergencia sanitaria por COVID–19) | Ecuador | Health Ministry, Ecuadorian Institute of Social Security, Armed Forces, Ecuadorian Society of Public Health, Ecuadorian Dental Federation | Spanish | May 2020 (3rd Edition) | [32] |
| Technical guidelines for dental attention after the COVID-19 emergency. (Lineamientos técnicos para la atención odontológica posterior a la emergencia por COVID-19) | El Salvador | Health Ministry, Government of El Salvador | Spanish | 14 June 2020 (1st Edition) | [33] |
| Standard operating procedure. Transition to recovery. A phased transition for dental practices towards the resumption of the full range of dental provision | England | Office of Chief Dental Officer England (OCDO), National Health Services (NHS) | English | 28 August 2020 (3rd Edition) | [15] |
| COVID-19 guidance and standard operating procedure. For the provision of urgent dental care in primary care dental settings and designated urgent dental care provider sites | England | National Health Services (NHS) | English | 28 August 2020 (3rd Edition) | [16] |
| Dental Biosecurity Protocol with emphasis on COVID-19. (Protocolo de Bioseguridad Odontológica con énfasis en COVID-19) | Guatemala | College of Stomatology of Guatemala | Spanish | May 2020 (1st Edition) | [41] |
| Advisory: Dental Clinics Protocols | India | Dental Council of India | English | 7 May 2020 (1st Edition) | [25] |
| Guidelines for oral health services at COVID-19 Alert Level 1 | New Zealand | Ministry of Health, Dental Council | English | December 2020 (6th Edition) | [26] |
| Guidelines for dental attention to patients with suspected or confirmed COVID-19 in health facilities. (Guía para el manejo odontológico de pacientes sospechosos o confirmados por COVID-19 en las instalaciones de salud) | Panama | Health Ministry of Panama | Spanish | March 2020 (1st Edition) | [34] |
| Protocol for dental attention during gradual return. (Protocolo para atención Odontológica de retorno gradual) | Paraguay | Ministry of Public Health and Social Welfare, National Government | Spanish | 7 May 2020 (1st Edition) | [35] |
| Biosecurity protocol for dental surgeons during and after the COVID-19 pandemic. (Protocolo de bioseguridad para el cirujano dentista durante y post pandemia COVID-19) | Peru | Dental College of Peru, National Administrative Council | Spanish | 26 April 2020 (1st Edition) | [36] |
| Clinical recommendations for the execution of dental-stomatological procedures in the context of the COVID-19 pandemic. (Recomendaciones clínicas para realizar procedimientos en odontoestomatología en el contexto de pandemia por COVID-19) | Peru | Institute for Technology Evaluation in Health and Research (IETSI) | Spanish | 13 April 2020 (1st Edition) | [37] |
| COVID-19: Procedures in primary oral health care services, clinics or consultancies, public and private sectors. (COVID-19: Procedimentos em clínicas, consultórios ou serviços de saúde oral dos cuidados de saúde primários, setor social e privado) | Portugal | Order of Dental Surgeons, National Oral Health Promotion Programme, National Programme for the Prevention and Control of Infections and Microbial Resistance | Portuguese | 27 July 2020 (2nd Edition) | [45] |
| Guidelines for dental care provision during the COVID-19 pandemic | Saudi Arabia | University | English | 7 April 2020 (1st Edition) | [27] |
| Novel coronavirus (COVID-19) Guidance for primary care | Scotland | Public Health Scotland, National Health Services Scotland (NHS) | English | 17 September 2020 (12th Edition) | [20] |
| Resuming General Dental Services Following COVID-19 Shutdown.A guide and implementation tools for general dental practice. For Phases 2 and 3 of dental services remobilisation | Scotland | Scottish Dental Clinical Effectiveness Programme (SDCEP) | English | 12 June 2020 (1st Edition) | [21] |
| Strategic Action Plan for the COVID-19 scale-back period. (Plan Estratégico de acción para el periodo de desescalada COVID-19) | Spain | Dental Council of Spain | Spanish | 2 May 2020 (2nd Edition) | [39] |
| Recommendations by the Spanish Society of Epidemiology and Oral Public Health (SESPO) for the healthcare adaptation of public health dental clinics in Spain during the COVID-19 pandemic | Spain | Spanish Society of Epidemiology and Oral Public Health (SESPO) | Spanish | December 2020 (1st Edition) | [38] |
| COVID-19 infection prevention and control measures for primary care, including general practitioner practices, dental clinics and pharmacy settings: first update | Europe | European Centre for Disease Prevention and Control (ECDC) | English | 19 October 2020 (2nd Edition) | [24] |
| Implications of COVID-19 for the safe management of general dental practice. A practical guide | UK | College of General Dentistry, Faculty of General Dental Practice | English | 2 October 2020 (2nd Edition) | [17] |
| Health Ministry recommendations for dental professionals and dental hygienists. (Recomendaciones del ministerio de salud pública para profesionales odontólogos e higienistas dentales) | Uruguay | Public Health Ministry of Uruguay | Spanish | 27 March 2020 (1st Edition) | [40] |
| Guidance for Dental Settings. Interim Infection Prevention and Control Guidance for Dental Settings During the coronavirus disease 2019 (COVID-19) Pandemic | USA | Center for Disease Control and Prevention | English | 4 December 2020 (2nd Edition) | [22] |
| Return to Work Interim Guidance Toolkit | USA | American Dental Association (ADA) | English | 23 July 2020 (2nd Edition) | [23] |
| Attention path for Odontopediatric procedures during shutdown or quarantine stages of the COVID-19 pandemic. (Ruta de atención para procedimientos de Odontología Pediátrica durante la etapa de confinamiento o cuarentena de la pandemia COVID-19) | - | Latin American Association of Odontopediatrics (ALOP) | English, Spanish, Portuguese | 11 April 2020 (1st Edition) | [47] |
| Considerations for the provision of essential oral health services in the context of COVID-19: interim guidance, 3 August 2020 | - | World Health Organization (WHO) | Arabic, Chinese, English, French, Portuguese, Russian, Spanish | 3 August 2020 (1st Edition) | [48] |
| Topic | Recommendation | N (%) |
|---|---|---|
| 1. Telephone triage: before dental care | Assess and record with a survey the symptoms of suspected and confirmed cases of COVID-19, before they attend for dental care. | 27 (79.4%) |
| 2. In-person triage: once the patient arrives at the clinic, before dental care | Assess and record with a survey the symptoms of suspected and confirmed cases of COVID-19. | 26 (76.5%) |
| once the patient arrives for dental care. Assess and record with a survey the symptoms of suspected and confirmed cases of COVID-19, associated with taking the patient’s temperature. | 13 (38.2%) | |
| 3. Patients with confirmed or suspected COVID-19 | Only urgent or emergency treatment | 16 (47.0%) |
| Delay the dental treatment | 13 (38.2%) | |
| Refer the patient to a health centre that receives and treats patients with confirmed or suspected COVID-19. | 9 (26.5%) | |
| Treat the patient in an isolated room. | 8 (23.5%) | |
| Treat the patient at the end of the day. | 4 (11.8%) | |
| Treat these patients on a different day | 4 (11.8%) | |
| Do not provide clinical services | 2 (5.9%) | |
| 4. Presence of accompanying persons | Patients not requiring assistance should attend the clinic alone. Only patients who require assistance, such as minors, patients with special needs and elderly patients, should be accompanied. | 24 (70.6%) |
| 5. General guidelines for patients | Wash hands or use alcohol-based disinfectant. | 28 (82.3%) |
| Physical distancing (between patients) | 19 (55.9%) | |
| Remove personal ornaments | 11 (32.3%) | |
| Avoid bringing personal objects and avoid the use of cellphones | 7 (20.6%) | |
| Hair should be tied back | 4 (11.8%) | |
| Do not brush teeth in the dental clinic | 4 (11.8%) | |
| Brush teeth in the dental clinic before dental care | 4 (11.8%) | |
| 6. Returning home | Give guidance for safe return home | 1 (2.9%) |
| Recommendation | N (%) |
|---|---|
| Physical separation measures to maintain social distancing: separate chairs (1 to 2 m between chairs), remove unnecessary chairs to encourage social distancing between patients, decrease the maximum capacity of the waiting room, delineate physical spaces with tables and chairs to define the flow zones. | 29 (85.3%) |
| Take away all shared objects from the waiting room: magazines, books, informative booklets, table games or toys. | 26 (76.5%) |
| Provide alcohol-based hand disinfectant at the entrance to the waiting room. | 23 (67.6%) |
| Install visual alerts in waiting room areas making recommendations about hand-washing protocols, social distancing and coughing. | 17 (50.0%) |
| Install a transparent panel in the reception area to separate staff from patients. | 17 (50.0%) |
| Install signs indicating the safe social distance in the reception area. | 12 (35.3%) |
| Install a disinfectant doormat at the entrance to the clinic. | 7 (20.6%) |
| Population | Respirator N95 or Similar | Surgical Mask | Gloves | Disposable Cap | Shoe Covers | External Protective Clothing (Disposable Apron/Gown) | Face Protection (Goggles/Face Shield) | CPGs without Report |
|---|---|---|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |
| Dentist | 32 (94.1%) | 24 (70.6%) | 31 (91.2%) | 23 (67.6%) | 11 (32.3%) | 32 (94.1%) | 32 (94.1%) | 2 (5.9%) |
| Dental assistant | 13 (38.2%) | 10 (29.4%) | 12 (35.3%) | 13 (38.2%) | 3 (8.8%) | 16 (47.0%) | 16 (47.0%) | 15 (44.1%) |
| Patients | - | 24 (70.6%) | - | 7 (20.6%) | 6 (17.6%) | 11 (32.3%) | 11 (32.3%) | 8 (23.5%) |
| Reception staff | - | 14 (41.2%) | - | 7 (20.6%) | 1 (2.9%) | 4 (11.8%) | 9 (26.5%) | 18 (52.9%) |
| Cleaning staff | - | 8 (23.5%) | 6 (17.6%) | 3 (8.8%) | 2 (5.9%) | 5 (14.7%) | 7 (20.6%) | 27 (79.4%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deana, N.F.; Seiffert, A.; Aravena-Rivas, Y.; Alonso-Coello, P.; Muñoz-Millán, P.; Espinoza-Espinoza, G.; Pineda, P.; Zaror, C. Recommendations for Safe Dental Care: A Systematic Review of Clinical Practice Guidelines in the First Year of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 10059. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph181910059
Deana NF, Seiffert A, Aravena-Rivas Y, Alonso-Coello P, Muñoz-Millán P, Espinoza-Espinoza G, Pineda P, Zaror C. Recommendations for Safe Dental Care: A Systematic Review of Clinical Practice Guidelines in the First Year of the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(19):10059. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph181910059
Chicago/Turabian StyleDeana, Naira Figueiredo, Andrea Seiffert, Yanela Aravena-Rivas, Pablo Alonso-Coello, Patricia Muñoz-Millán, Gerardo Espinoza-Espinoza, Patricia Pineda, and Carlos Zaror. 2021. "Recommendations for Safe Dental Care: A Systematic Review of Clinical Practice Guidelines in the First Year of the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 18, no. 19: 10059. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph181910059






