Understanding the Variation within a Dietary Guideline Index Score to Identify the Priority Food Group Targets for Improving Diet Quality across Population Subgroups
Abstract
:1. Introduction
2. Materials and Methods
Identifying the Diet Guideline Index Components Most in Need of Intervention
3. Results
3.1. Sample Characteristics
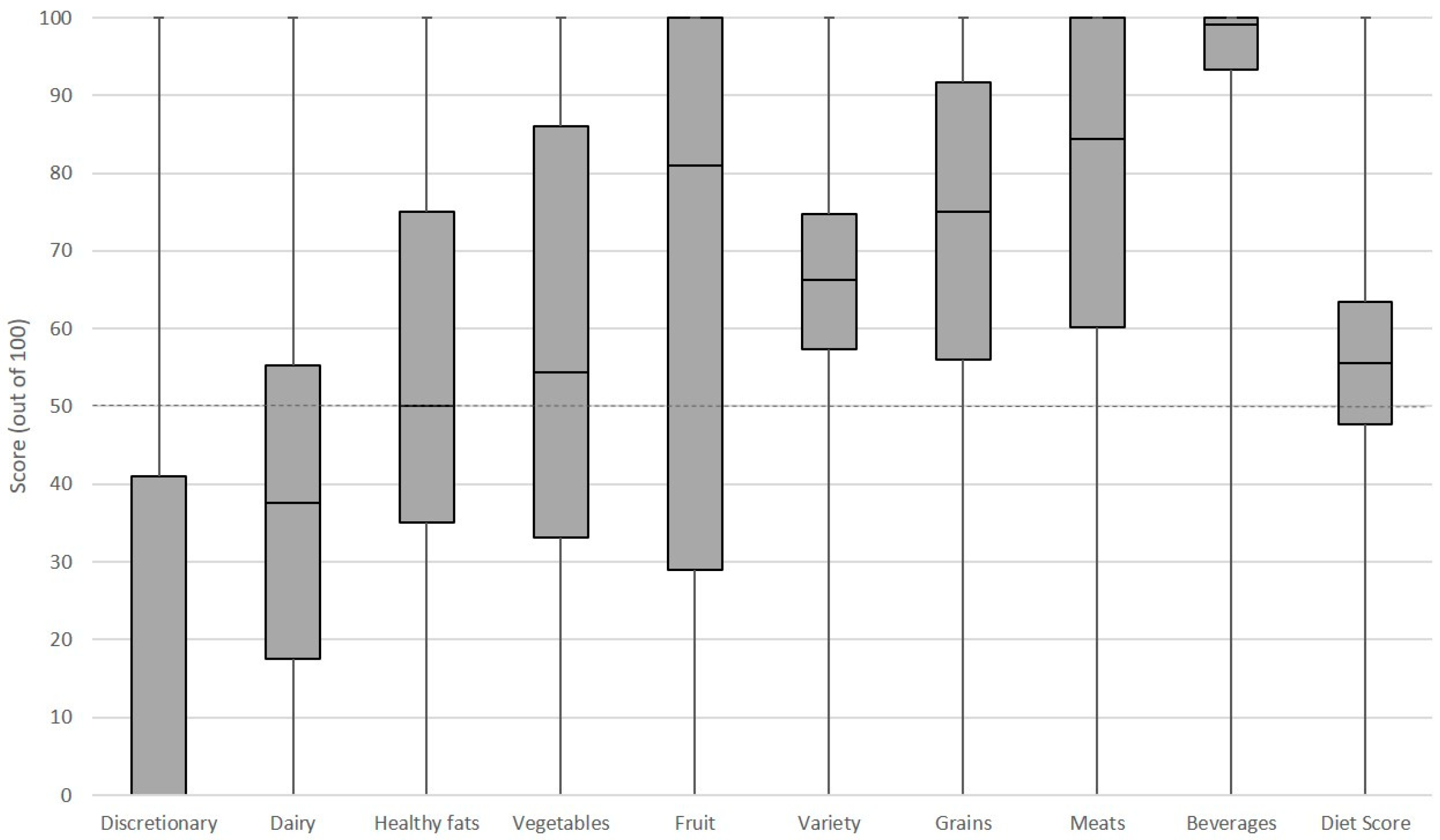
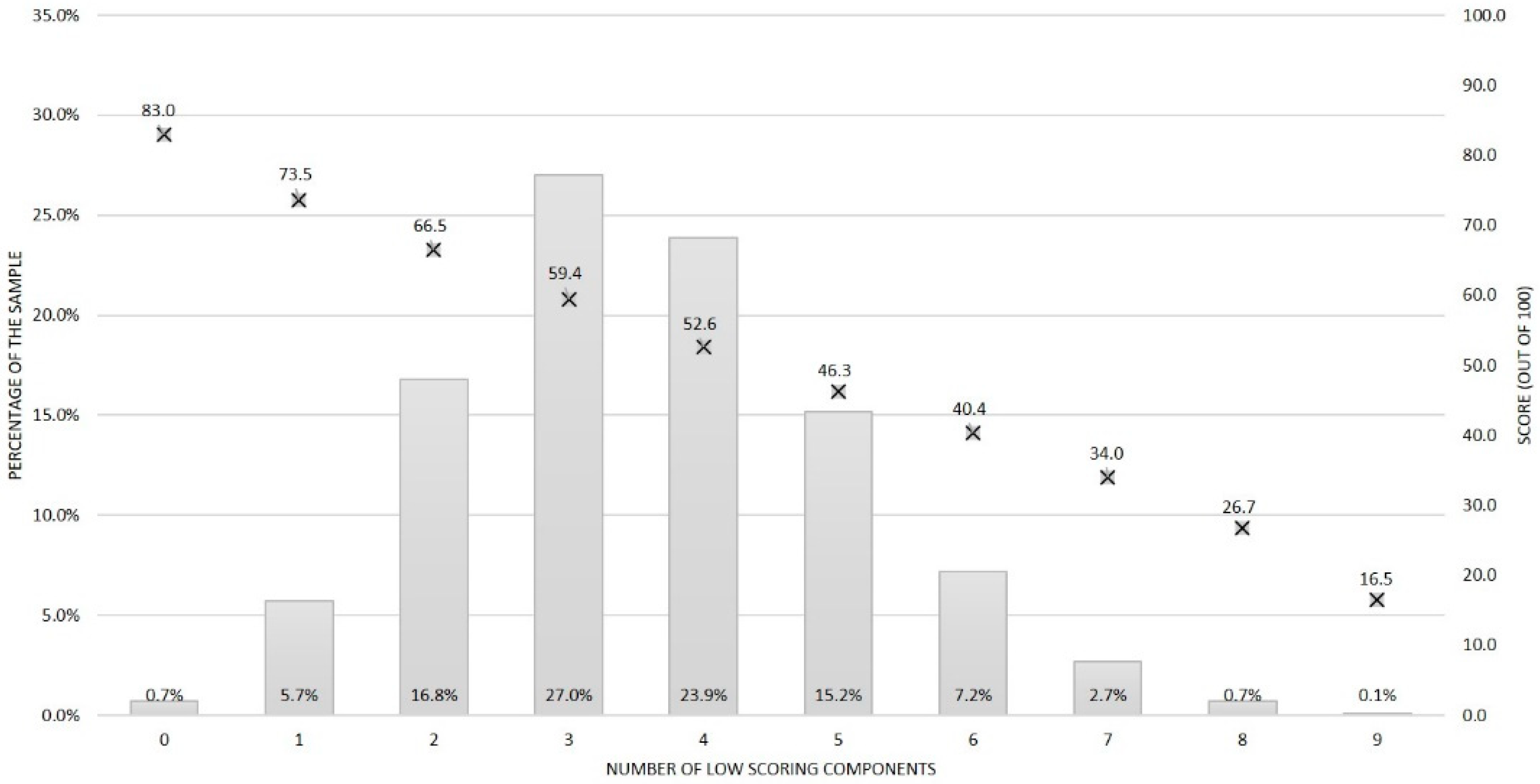
3.2. Overall Distribution of the Low Scoring Components
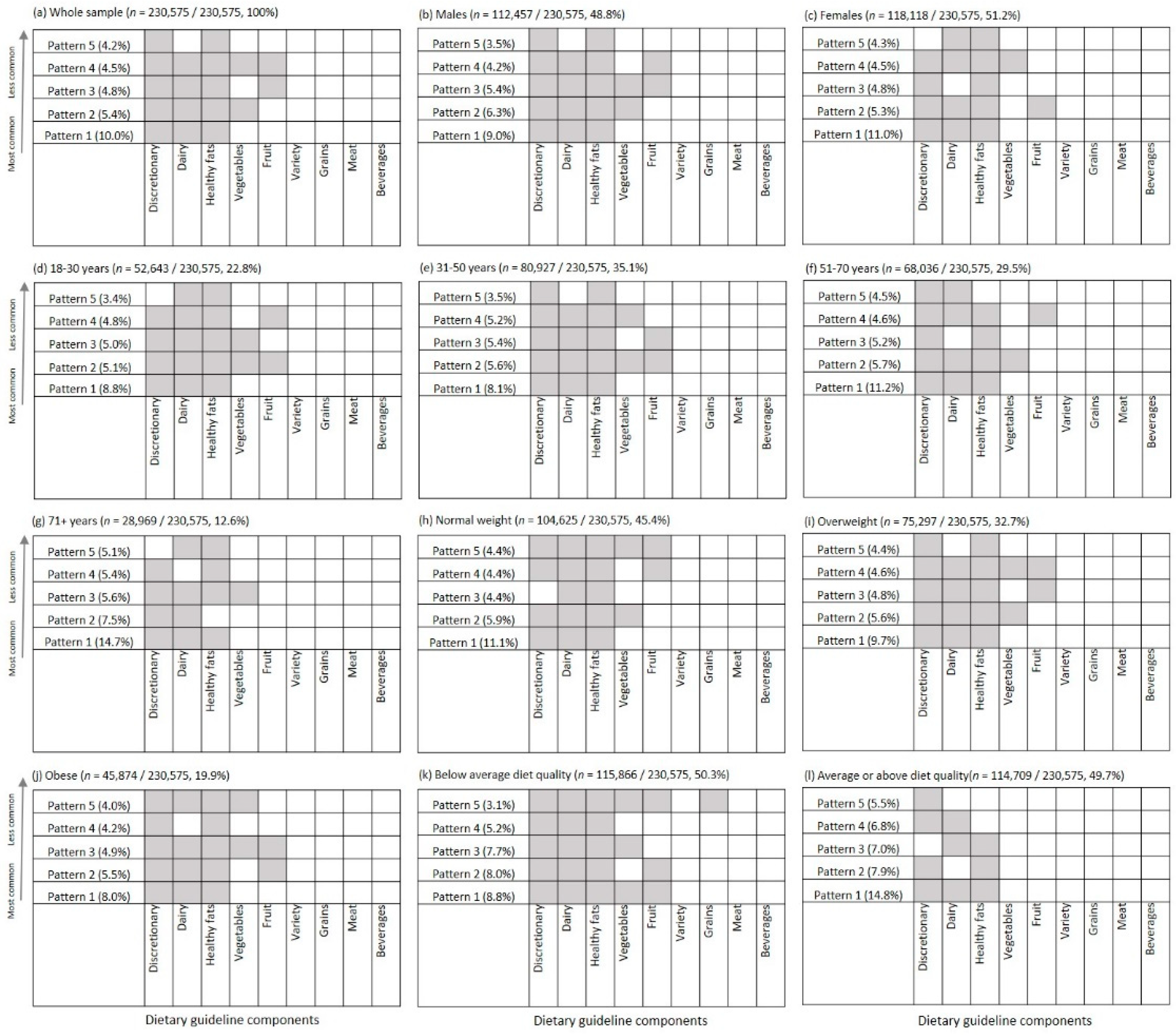
3.3. Combinations of Low Scoring Components
4. Discussion
4.1. Strengths and Limitations
4.2. Implications and Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Australian Institute of Health and Welfare. Nutrition Across the Life Stages; Australian Government: Canberra, Australia, 2018.
- Public Health England. National Diet and Nutrition Survey, Results from Years 7 and 8 (combined) of the Rolling Programme (2014/2015 to 2015/2016); Public Health England: London, UK, 2019.
- Rekhy, R.; McConchie, R. Promoting consumption of fruit and vegetables for better health. Have campaigns delivered on the goals? Appetite 2014, 79, 113–123. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Noncommunicable Diseases Country Profiles 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- National Health & Medical Research Council. Australian Dietary Guidelines-Educator Guide; Australian Government: Canberra, Australia, 2013.
- US Department of Agriculture. ChooseMyPlate. 2020. Available online: https://www.choosemyplate.gov/ (accessed on 31 May 2020).
- Government of Canada. Canada’a Food Guide. 2017. Available online: https://food-guide.canada.ca/en/ (accessed on 16 October 2020).
- Public Health England. The Eatwell Guide. 2018. Available online: https://www.gov.uk/government/publications/the-eatwell-guide (accessed on 16 October 2020).
- Australian Bureau of Statistics, 4364.0.55.007-Australian Health Survey: Nutrition First Results-Foods and Nutrients, 2011–2012; Australian Government: Canberra, Australia, 2014.
- Australian Bureau of Statistics, 4364.0.55.001-National Health Survey: First Results, 2014–2015; Australian Government: Canberra, Australia, 2014.
- Krebs-Smith, S.M.; Guenther, P.M.; Subar, A.F.; Kirkpatrick, S.I.; Dodd, K.W. Americans do not meet federal dietary recommendations. J. Nutr. 2010, 140, 1832–1838. [Google Scholar] [CrossRef]
- Hack, S.; Jessri, M.; L’Abbe, M.R. Evaluating Diet Quality of Canadian Adults Using Health Canada’s Surveillance Tool Tier System: Findings from the 2015 Canadian Community Health Survey-Nutrition. Nutrients 2020, 12, 1113. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Afshin, A.; Benowitz, N.L.; Bittner, V.; Daniels, S.R.; Franch, H.A.; Jacoba, D.R., Jr.; Kraus, W.E.; Kris-Etherton, P.M.; Krummel, D.A.; et al. Population approaches to improve diet, physical activity, and smoking habits: A scientific statement from the American Heart Association. Circulation 2012, 126, 1514–1563. [Google Scholar] [CrossRef] [PubMed]
- Grunseit, A.C.; O’Hara, B.J.; Chau, J.Y.; Briggs, M.; Bauman, A.E. Getting the message across: Outcomes and risk profiles by awareness levels of the “measure-up” obesity prevention campaign in Australia. PLoS ONE 2015, 10, e0121387. [Google Scholar] [CrossRef] [PubMed]
- O’Hara, B.J.; Grunseit, A.; Phongsavan, P.; Bellew, W.; Briggs, M.; Bauman, A.E. Impact of the Swap It, Don’t Stop It Australian National Mass Media Campaign on Promoting Small Changes to Lifestyle Behaviors. J. Health Commun. 2016, 21, 1276–1285. [Google Scholar] [CrossRef] [PubMed]
- Pollard, C.M.; Miller, M.R.; Daly, A.M.; Crouchley, K.E.; O’Donoghue, K.J.; Lang, A.J.; Binns, C.W. Increasing fruit and vegetable consumption: Success of the Western Australian Go for 2&5 campaign. Public Health Nutr. 2008, 11, 314–320. [Google Scholar] [PubMed] [Green Version]
- Castiglione, C.; Mazzocchi, M. Ten years of five-a-day policy in the UK: Nutritional outcomes and environmental effects. Ecol. Econ. 2019, 157, 185–194. [Google Scholar] [CrossRef]
- Ashfield-Watt, P.A. Fruits and vegetables, 5+ a day: Are we getting the message across? Asia Pac. J. Clin. Nutr. 2006, 15, 245. [Google Scholar]
- Halicka, E.; Rejman, K. Fruit and vegetable promotion programs in the European Union. Probl. World Agric. 2007, 1, 38–45. [Google Scholar]
- Harris, J.; Felix, L.; Miners, A.; Murray, E.; Michie, S.; Ferguson, E.; Free, C.; Lock, K.; Landon, J.; Edwards, P. Adaptive e-learning to improve dietary behaviour: A systematic review and cost-effectiveness analysis. Health Technol. Assess. 2011, 15, 1–160. [Google Scholar] [CrossRef] [PubMed]
- Villinger, K.; Wahl, D.R.; Boeing, H.; Schupp, H.T.; Renner, B. The effectiveness of app-based mobile interventions on nutrition behaviours and nutrition-related health outcomes: A systematic review and meta-analysis. Obes. Rev. 2019, 20, 1465–1484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hendrie, G.A.; Hussain, M.S.; Brindal, E.; James-Martin, G.; Williams, G.; Crook, A. Impact of a Mobile Phone App to Increase Vegetable Consumption and Variety in Adults: Large-Scale Community Cohort Study. JMIR Mhealth Uhealth 2020, 8, e14726. [Google Scholar] [CrossRef] [PubMed]
- Wallace, T.C.; Bailey, R.L.; Blumberg, J.B.; Burton-Freeman, B.; Chen, C.O.; Crowe-White, K.M.; Drewnowski, A.; Hooshmand, S.; Johnson, E.; Lewis, R.; et al. Fruits, vegetables, and health: A comprehensive narrative, umbrella review of the science and recommendations for enhanced public policy to improve intake. Crit. Rev. Food Sci. Nutr. 2020, 60, 2174–2211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, R.L.; Rollo, M.E.; Schumacher, T.; Collins, C.E. Diet Quality Scores of Australian Adults Who Have Completed the Healthy Eating Quiz. Nutrients 2017, 9, 880. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hendrie, G.A.; Baird, D.; Golley, R.K.; Noakes, M. The CSIRO Healthy Diet Score: An Online Survey to Estimate Compliance with the Australian Dietary Guidelines. Nutrients 2017, 9, 47. [Google Scholar] [CrossRef] [Green Version]
- Kirkpatrick, S.I.; Reedy, J.; Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Wilson, M.M.; Lerman, J.L.; Tooze, J.A. Applications of the Healthy Eating Index for Surveillance, Epidemiology, and Intervention Research: Considerations and Caveats. J. Acad. Nutr. Diet 2018, 118, 1603–1621. [Google Scholar] [CrossRef]
- Hendrie, G.A.; Golley, R.K.; Noakes, M. Compliance with Dietary Guidelines Varies by Weight Status: A Cross-Sectional Study of Australian Adults. Nutrients 2018, 10, 197. [Google Scholar] [CrossRef] [Green Version]
- Hendrie, G.A.; Rebuli, M.A.; Golley, R.K. Reliability and relative validity of a diet index score for adults derived from a self-reported short food survey. Nutr. Diet 2017, 74, 291–297. [Google Scholar] [CrossRef]
- World Health Organization. Body Mass Index-BMI. 2020. Available online: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (accessed on 24 December 2020).
- National Health and Medical Research Council; Australian Government Department of Health and Ageing; New Zealand Ministry of Health. Nutrient Reference Values for Australia and New Zealand; National Health & Medical Research Council: Canberra, Australia, 2006.
- Hendrie, G.A.; Rebuli, M.A.; Golley, R.K.; Noakes, M. Adjustment Factors Can Improve Estimates of Food Group Intake Assessed Using a Short Dietary Assessment Instrument. J. Acad. Nutr. Diet 2018, 118, 1864–1873. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. 2016 Census QuickStats. 2017. Available online: https://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2016/quickstat/036 (accessed on 17 November 2020).
- Fayet-Moore, F.; McConnell, A.; Cassettari, T.; Tuck, K.; Petocz, P.; Kim, J. Discretionary intake among Australian adults: Prevalence of intake, top food groups, time of consumption and its association with sociodemographic, lifestyle and adiposity measures. Public Health Nutr. 2019, 22, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Ashton, L.M.; Sharkey, T.; Whatnall, M.C.; Williams, R.L.; Bezzina, A.; Aguiar, E.J.; Collins, C.E.; Hutchesson, M.J. Effectiveness of Interventions and Behaviour Change Techniques for Improving Dietary Intake in Young Adults: A Systematic Review and Meta-Analysis of RCTs. Nutrients 2019, 11, 825. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhattarai, N.; Prevost, A.T.; Wright, A.J.; Charlton, J.; Rudisill, C.; Gulliford, M.C. Effectiveness of interventions to promote healthy diet in primary care: Systematic review and meta-analysis of randomised controlled trials. BMC Public Health 2013, 13, 1203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Browne, S.; Minozzi, S.; Bellisario, C.; Sweeney, M.R.; Susta, D. Effectiveness of interventions aimed at improving dietary behaviours among people at higher risk of or with chronic non-communicable diseases: An overview of systematic reviews. Eur. J. Clin. Nutr. 2019, 73, 9–23. [Google Scholar] [CrossRef] [PubMed]
- Garriguet, D. Diet Quality in Canada; Statistics Canada: Ottowa, ON, Canada, 2009; p. 41. [Google Scholar]
- Hiza, H.A.; Casavale, K.O.; Guenther, P.M.; Davis, C.A. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. J. Acad. Nutr. Diet 2013, 113, 297–306. [Google Scholar] [CrossRef]
- Michie, S.; Atkins, L.; West, R. The Behaviour Change Wheel: A Guide to Designing Interventions; Silverback Publishing: Sutton, UK, 2014. [Google Scholar]
- Freeland-Graves, J.H.; Nitzke, S. Position of the Academy of Nutrition and Dietetics: Total Diet Approach to Healthy Eating. J. Acad. Nutr. Diet. 2013, 113, 307–317. [Google Scholar] [CrossRef]
- Sacks, F.M.; Svetkey, L.P.; Vollmer, W.M.; Appel, L.J.; Bray, G.A.; Harsha, D.; Obarzanek, E.; Conlin, P.R.; Miller, E.R.; Simons-Morton, D.G.; et al. Effects on Blood Pressure of Reduced Dietary Sodium and the Dietary Approaches to Stop Hypertension (DASH) Diet. N. Engl. J. Med. 2001, 344, 3–10. [Google Scholar] [CrossRef]
- Sofi, F.; Abbate, R.; Gensini, G.F.; Casini, A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: An updated systematic review and meta-analysis. Am. J. Clin. Nutr. 2010, 92, 1189–1196. [Google Scholar] [CrossRef] [Green Version]
- Desroches, S.; Lapointe, A.; Ratté, S.; Gravel, K.; Légaré, F.; Turcotte, S. Interventions to enhance adherence to dietary advice for preventing and managing chronic diseases in adults. Cochrane Database Syst. Rev. 2013, 2, CD008722. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Adherence to Long-Term Therapies: Evidence for Action. 2003. Available online: https://www.who.int/chp/knowledge/publications/adherence_report/en/ (accessed on 3 November 2020).
- Celis-Morales, C.; Lara, J.; Mathers, J.C. Personalising nutritional guidance for more effective behaviour change. Proc. Nutr. Soc. 2015, 74, 130–138. [Google Scholar] [CrossRef] [Green Version]
- Australian Bureau of Statistics. 4364.0.55.001-National Health Survey: First Results, 2017–2018; Australian Government: Canberra, Australia, 2018.
- Lean, M.; Lara, J.; Hill, J.O. Strategies for preventing obesity. BMJ Br. Med. J. 2006, 333, 959. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hill, J.O. Can a small-changes approach help address the obesity epidemic? A report of the Joint Task Force of the American Society for Nutrition, Institute of Food Technologists, and International Food Information Council. Am. J. Clin. Nutr. 2009, 89, 477–484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grieger, J.A.; Johnson, B.J.; Wycherley, T.P.; Golley, R.K. Comparing the Nutritional Impact of Dietary Strategies to Reduce Discretionary Choice Intake in the Australian Adult Population: A Simulation Modelling Study. Nutrients 2017, 9, 442. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Position in Sequence | Diet Quality Component | Assigned Value |
|---|---|---|
| 1 | Discretionary choices | 1 |
| 2 | Dairy | 0 |
| 3 | Healthy fats | 0 |
| 4 | Vegetables | 1 |
| 5 | Fruit | 1 |
| 6 | Variety | 0 |
| 7 | Grains | 0 |
| 8 | Meat | 0 |
| 9 | Beverages | 0 |
| Dietary pattern sequence | 10,011,000 | |
| Characteristic | Categories | n | % |
|---|---|---|---|
| Total sample | 230,575 | 100.0 | |
| Gender | Male | 112,457 | 48.8 |
| Female | 118,118 | 51.2 | |
| Age group | 18–30 years | 52,643 | 22.8 |
| 31–50 years | 80,927 | 35.1 | |
| 51–70 years | 68,036 | 29.5 | |
| 71+ years | 28,969 | 12.6 | |
| Weight status | Underweight | 4779 | 2.1 |
| Healthy weight | 104625 | 45.4 | |
| Overweight | 75,297 | 32.7 | |
| Obesity | 45,874 | 19.9 | |
| Diet quality score | Below average b | 115,866 | 50.3 |
| Average or above average | 114,709 | 49.7 | |
| Low scoring components | Discretionary choices | 183,220 | 79.5 |
| Healthy fats | 166,364 | 72.2 | |
| Dairy | 163,171 | 70.8 | |
| Vegetables | 103,638 | 44.9 | |
| Fruit | 95,409 | 41.4 | |
| Grains | 46,244 | 20.1 | |
| Meat | 36,070 | 15.6 | |
| Variety | 29,514 | 12.8 | |
| Beverages | 7118 | 3.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hendrie, G.A.; Lyle, G.; Mauch, C.E.; Haddad, J.; Golley, R.K. Understanding the Variation within a Dietary Guideline Index Score to Identify the Priority Food Group Targets for Improving Diet Quality across Population Subgroups. Int. J. Environ. Res. Public Health 2021, 18, 378. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18020378
Hendrie GA, Lyle G, Mauch CE, Haddad J, Golley RK. Understanding the Variation within a Dietary Guideline Index Score to Identify the Priority Food Group Targets for Improving Diet Quality across Population Subgroups. International Journal of Environmental Research and Public Health. 2021; 18(2):378. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18020378
Chicago/Turabian StyleHendrie, Gilly A., Greg Lyle, Chelsea E. Mauch, Joyce Haddad, and Rebecca K. Golley. 2021. "Understanding the Variation within a Dietary Guideline Index Score to Identify the Priority Food Group Targets for Improving Diet Quality across Population Subgroups" International Journal of Environmental Research and Public Health 18, no. 2: 378. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18020378







