More Is Not Enough: A Deeper Understanding of the COVID-19 Impacts on Healthcare, Energy and Environment Is Crucial
Abstract
:1. Introduction
- The structural changes in healthcare, energy and environment, in particular the cross-sections of the three sectors, have been overviewed, which offers insights and perspectives for the in-depth understanding of the complicated COVID-19 impacts. Through the broad overview, several interesting and practical observations have been highlighted.
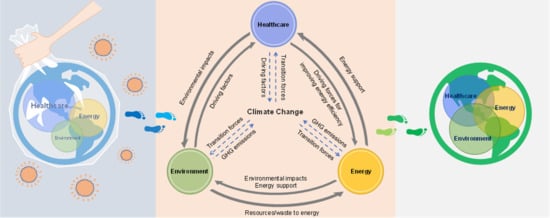
- A novel concept of the healthcare–energy–environment nexus under climate change constraints has been proposed and discussed to potentially guide more balance and innovation about the sustainable development of the healthcare–energy–environment coupling system.
- Based on the proposed nexus, the dynamics of the attention, being triggered by COVID-19, to healthcare, energy and environment in view of decision-makers have been illustrated, which is taken to analyse the on-going situation and look ahead future scenarios to sustainable development goals.
2. The Changes in Healthcare Systems—Energy and Environmental Perspectives
2.1. Impacts on Healthcare Resources
- The severe shortage of medical resources such as hospital beds, ventilators and intensive care unit (ICU) beds would destroy the crisis management unless the pandemic curve of COVID-19 cases could be flattened over a long time [32] by containment measures or vaccines support. However, several years are needed to produce a licensed vaccine, even at the pandemic speed [35]. To this end, the lockdowns were broadly implemented in worldwide countries [36]. Although the lockdown strategy would, in turn, put pressure on the healthcare resources and the sustainability of the energy sector, it is a compromise by considering both the healthcare resources and the flatness of the infection curve.
- The energy and environmental footprints have been increased by the global emergent production and logistics of healthcare resources due to the resource shortage and the regional heterogeneity in healthcare resource accessibility and availability. For example, the energy consumption by emergency logistics is about 17 times that by regular logistics [37]. Before the COVID-19 crisis, the healthcare sector has been one of the major contributors to climate emissions. Healthcare sector’s footprint is 4.4% of global net greenhouse gas (GHG) emissions [38]. Healthcare activities in the middle- and low- income countries counted for 3 to 5% of national total carbon emissions, and the proportion in some developed countries ranged from 5 to 15% [39]. For example, the GHG emissions related to healthcare activities contributed 8% of total emissions in the US in 2007 [40], and this proportion was enlarged to 9.8% in 2013 [41]. Such proportions in both developed and developing countries would be understandably increased under the COVID-19 circumstances.
2.2. Impacts on other Infectious Diseases
2.3. Impacts on Non-Communicable Diseases and e-Healthcare
3. The Changes in Energy Consumption—Healthcare and Environmental Relevance
- With sufficient collaboration between the healthcare and energy sectors, healthcare facilities and services rely on reliable electricity [28] and affordable energy, especially the clean and renewable power [98] to effectively treat patients. The reliable energy used for COVID-19 response was regarded as one of the main missing links in the healthcare systems of underdeveloped countries [7]. For connecting such a missing link, Rinkoo et al. [7] recommended a “green public-health infrastructure concept” for the COVID-19 response.
- The COVID-19 pandemic is not only a health and economic crisis but also a justice crisis [99]. Generally, as the rural areas lack access to electricity and 24/7 health services, distributed energy systems with local clean and renewable sources might be an appropriate solution for healthcare centres in such areas [98]. The development of both energy and healthcare technologies would contribute a breakthrough to the justice issue.
4. The Changes in the Environment—Air Pollution and Solid Waste
5. Nexus, Attention Dynamics and Future Outlook
5.1. Healthcare–Energy–Environment Nexus
5.2. Dynamics of the Attention to Healthcare, Energy and Environment
- (a)
- Before COVID-19, the promising development of healthcare, energy and environment (Figure 5a): The harmonious development has been receiving initial attention worldwide. The net zero-emissions healthcare by 2050 [38] is a good example to present the focus on healthcare’s climate footprint and its related factors. According to a survey with 3500 consumers [146], healthcare, energy and environment were thought to be the top three priorities for innovation and technology. Advanced technologies promoting the development of healthcare, energy and environment have been reviewed and commented by Lim et al. [147].
- (b)
- During the COVID-19 outbreak, the emergency development of healthcare (Figure 5b): The COVID-19 pandemic not only prioritises the healthcare sector but also reduces the attention to the cross-sections (i.e., healthcare and energy, healthcare and environment and even energy and environment). The rapid response of COVID-19 fighting was seriously treated during the outbreak time, even if at the expense of energy waste and environmental pollution [37].
- (c)
- During the mitigation time, healthcare still dominants energy and environment (Figure 5c): Compared to the outbreak time, the energy sector in the mitigation time has been paid more attention as it is directly related to the economic recovery. More environmental issues have been exposed in the mitigation time; the environment has been gradually back to managerial and public view. For example, both the energy and environment dimensions have been considered in the transition of sustainable supply and production during COVID-19 [148]. The ‘15-min city’ [149] has been appealed again to build a lifestyle with a safe and low-carbon environment, although the ‘15-min city’ is not a new concept.
- (d)
- After the pandemic (projected), the repercussion and sustainable development with more balance and cross-section attention (Figure 5d): For the situation after the pandemic, it is projected that more attention might be focused on the cross-sections of healthcare, energy and environment, as illustrated in Figure 5d, which is discussed in the future outlook part in Section 5.3.
5.3. Future Outlook and Suggestions
6. Conclusions
- During COVID-19, healthcare has been prioritised at the expense of energy and environmental costs. The extra energy consumption and extra environmental footprints, due to the blooms of e-healthcare and the regional heterogeneity in healthcare resource accessibility and availability, deserve more assessment.
- The lockdown measures due to COVID-19 do not necessarily benefit other infectious diseases, which may also cause extra energy and environmental footprints in the following years. The weight of priority for different infectious diseases should be adjusted dynamically, and smarter and more flexible lockdown strategies are worthy of more investigation.
- The energy sector plays a strong support role in effective healthcare and environmental management. COVID-19 has speeded up the energy transitions, for which more attention and personalised assessment with a consideration of the environmental footprint in different countries are needed to navigate the energy transitions under the COVID-19 pandemic.
- Although GHG emissions have been reduced temporarily by global lockdowns, spatial differences are significant in the reduction rate, varying from 3.7 to 18.8%. More particulate matter and O3 pollution have been observed in several regions. The long-run GHG emissions and air pollution are still hard to estimate accurately due to the recovery of economic activities and stimulus packages during and after the pandemic.
- After implementing containment measures, the change rate of solid waste generation presents spatial heterogeneity in worldwide cities with the change rate ranging from –30 to +40%. The sharply varied and uncertain fluctuations in the amount of municipal solid waste might severely threaten the sustainability of operations of the incineration facilities in the waste-to-energy systems.
- Although industrial plastic recycling has been hindered, household waste recycling programmes are not necessarily affected significantly by COVID-19. The recycling programmes with waste segregation at the source have a slight impact; whilst those with waste segregation at the end have been affected greatly. The phenomenon of illegal waste dumping was observed more frequently during COVID-19, which may accelerate the spread of the virus and threaten the healthcare system.
- In spite of in its early stages, digitalisation plays an important role during this pandemic, e.g., e-healthcare, energy digitalisation and digital waste management. A climate footprint-focused digitalisation development pathway under the incorporation of the Circular Economy and the transitions of clean and renewable energy has a great potential to take off.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Disclaimer
Conflicts of Interest
References
- WHO. WHO Coronavirus Disease (COVID-19) Dashboard. 2020. Available online: https://covid19.who.int/ (accessed on 26 December 2020).
- Naidoo, R.; Fisher, B. Reset sustainable development goals for a pandemic world. Nature 2020, 583, 198–201. [Google Scholar] [CrossRef] [PubMed]
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int. J. Surg. 2020, 78, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Saxe, J.G. The Blind Men and the Elephant; Enrich Spot Limited: Hong Kong, China, 2016. [Google Scholar]
- Hollander, J.E.; Carr, B.G. Virtually perfect? Telemedicine for COVID-19. N. Engl. J. Med. 2020, 382, 1679–1681. [Google Scholar] [CrossRef]
- Broto, V.C.; Kirshner, J. Energy access is needed to maintain health during pandemics. Nat. Energy 2020, 5, 419–421. [Google Scholar] [CrossRef]
- Rinkoo, A.V.; Songara, D.; Sharma, A.; Patnaik, B.R.; Singh, R.R.; Srivastava, R.K. Reliable energy and responsive built environment: The missing links in COVID-19 response in resource-limited settings. Trop. Med. Health 2020, 48, 67. [Google Scholar] [CrossRef]
- Semenza, J.C.; Sudre, B.; Oni, T.; Suk, J.E.; Giesecke, J. Linking environmental drivers to infectious diseases: The European environment and epidemiology network. PLoS Negl. Trop. Dis. 2013, 7, e2323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aalto, E.A.; Lafferty, K.D.; Sokolow, S.H.; Grewelle, R.E.; Ben-Horin, T.; Boch, C.A.; Raimondi, P.T.; Bograd, S.J.; Hazen, E.L.; Jacox, M.G.; et al. Models with environmental drivers offer a plausible mechanism for the rapid spread of infectious disease outbreaks in marine organisms. Sci. Rep. 2020, 10, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Li, M.; Yang, Y.; Lu, Y.; Zhang, D.; Liu, Y.; Cui, X.; Yang, L.; Liu, R.; Liu, J.; Li, G.; et al. Natural host–environmental media–human: A new potential pathway of COVID-19 outbreak. Engineering 2020, 6, 1085–1098. [Google Scholar] [CrossRef]
- Sarkar, P.; Debnath, N.; Reang, D. Coupled human-environment system amid COVID-19 crisis: A conceptual model to understand the nexus. Sci. Total Environ. 2021, 753, 141757. [Google Scholar] [CrossRef]
- Oni, T. COVID-19 is Showing Us the Link between Human and Planetary Health. 2020. Available online: https://www.weforum.org/agenda/2020/04/on-earth-day-heres-what-covid-19-can-teach-us-about-improving-our-planetary-health/ (accessed on 30 October 2020).
- Frontera, A.; Cianfanelli, L.; Vlachos, K.; Landoni, G.; Cremona, G. Severe air pollution links to higher mortality in COVID-19 patients: The “double-hit” hypothesis. J. Infect. 2020, 81, 255–259. [Google Scholar] [CrossRef]
- Domínguez-Amarillo, S.; Fernández-Agüera, J.; Cesteros-García, S.; González-Lezcano, R.A. Bad air can also kill: Residential indoor air quality and pollutant exposure risk during the COVID-19 crisis. Int. J. Environ. Res. Public Health 2020, 17, 7183. [Google Scholar] [CrossRef] [PubMed]
- Austin, K.F. Degradation and disease: Ecologically unequal exchanges cultivate emerging pandemics. World Dev. 2020, 137, 105163. [Google Scholar] [CrossRef] [PubMed]
- Cimerman, S.; Chebabo, A.; da Cunha, C.A.; Rodríguez-Morales, A.J. Deep impact of COVID-19 in the healthcare of Latin America: The case of Brazil. Braz. J. Infect. Dis. 2020, 24, 93–95. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, K.; Chatterjee, K.; Kumar, A.; Shankar, S. Healthcare impact of COVID-19 epidemic in India: A stochastic mathematical model. Med. J. Armed Forces India 2020, 76, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Ruan, G.; Wu, D.; Zheng, X.; Zhong, H.; Kang, C.; Dahleh, M.A.; Sivaranjani, S.; Xie, L. A cross-domain approach to analysing the short-run impact of COVID-19 on the US electricity sector. Joule 2020, 4, 2322–2337. [Google Scholar] [CrossRef]
- Werth, A.; Gravino, P.; Prevedello, G. Impact analysis of COVID-19 responses on energy grid dynamics in Europe. Appl. Energy 2021, 281, 116045. [Google Scholar] [CrossRef] [PubMed]
- Nakada, L.Y.K.; Urban, R.C. COVID-19 pandemic: Impacts on the air quality during the partial lockdown in São Paulo state, Brazil. Sci. Total Environ. 2020, 730, 139087. [Google Scholar] [CrossRef]
- Wang, Q.; Su, M. A preliminary assessment of the impact of COVID-19 on environment–A case study of China. Sci. Total Environ. 2020, 728, 138915. [Google Scholar] [CrossRef]
- Eroğlu, H. Effects of COVID-19 outbreak on environment and renewable energy sector. Environ. Dev. Sustain. 2020. [Google Scholar] [CrossRef]
- Chakraborty, I.; Maity, P. COVID-19 outbreak: Migration, effects on society, global environment and prevention. Sci. Total Environ. 2020, 728, 138882. [Google Scholar] [CrossRef]
- Gillingham, K.T.; Knittel, C.R.; Li, J.; Ovaere, M.; Reguant, M. The short-run and long-run effects of COVID-19 on energy and the environment. Joule 2020, 4, 1337–1341. [Google Scholar] [CrossRef]
- Mofijur, M.; Fattah, I.R.; Alam, M.A.; Islam, A.S.; Ong, H.C.; Rahman, S.A.; Najafi, G.; Ahmed, S.F.; Alhaz Uddin, M.; Mahlia, T.M.I. Impact of COVID-19 on the social, economic, environmental and energy domains: Lessons learnt from a global pandemic. Sustain. Prod. Consum. 2021, 26, 343–359. [Google Scholar] [CrossRef] [PubMed]
- Elavarasan, R.M.; Pugazhendhi, R. Restructured society and environment: A review on potential technological strategies to control the COVID-19 pandemic. Sci. Total Environ. 2020, 725, 138858. [Google Scholar] [CrossRef] [PubMed]
- Zeka, A.; Tobias, A.; Leonardi, G.; Bianchi, F.; Lauriola, P.; Crabbe, H.; Vardoulakis, S.; Guo, Y.; Honda, Y.; Gasparrini, A.; et al. Responding to COVID-19 requires strong epidemiological evidence of environmental and societal determining factors. Lancet Planet. Health 2020, 4, e375–e376. [Google Scholar] [CrossRef]
- SEforALL. COVID-19 Response: Powering Health Facilities. Sustainable Energy for All (SEforALL). 2020. Available online: https://www.seforall.org/energy-and-health/covid-19-response-powering-health-facilities (accessed on 30 October 2020).
- Chudasama, Y.V.; Gillies, C.L.; Zaccardi, F.; Coles, B.; Davies, M.J.; Seidu, S.; Khunti, K. Impact of COVID-19 on routine care for chronic diseases: A global survey of views from healthcare professionals. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 965–967. [Google Scholar] [CrossRef]
- Ji, Y.; Ma, Z.; Peppelenbosch, M.P.; Pan, Q. Potential association between COVID-19 mortality and healthcare resource availability. Lancet Glob. Health 2020, 8, e480. [Google Scholar] [CrossRef] [Green Version]
- Miller, I.F.; Becker, A.D.; Grenfell, B.T.; Metcalf, C.J.E. Disease and healthcare burden of COVID-19 in the United States. Nat. Med. 2020, 26, 1212–1217. [Google Scholar] [CrossRef]
- Emanuel, E.J.; Persad, G.; Upshur, R.; Thome, B.; Parker, M.; Glickman, A.; Zhang, C.; Boyle, C.; Smith, M.; Phillips, J.P. Fair allocation of scarce medical resources in the time of COVID-19. N. Engl. J. Med. 2020, 382, 2049–2055. [Google Scholar] [CrossRef]
- Kavanagh, M.M.; Erondu, N.A.; Tomori, O.; Dzau, V.J.; Okiro, E.A.; Maleche, A.; Aniebo, I.C.; Rugege, U.; Holmes, C.B.; Gostin, L.O. Access to lifesaving medical resources for African countries: COVID-19 testing and response, ethics, and politics. Lancet 2020, 395, 1735–1738. [Google Scholar] [CrossRef]
- Randolph, H.E.; Barreiro, L.B. Herd immunity: Understanding COVID-19. Immunity 2020, 52, 737–741. [Google Scholar] [CrossRef]
- Lurie, N.; Saville, M.; Hatchett, R.; Halton, J. Developing COVID-19 vaccines at pandemic speed. N. Engl. J. Med. 2020, 382, 1969–1973. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.M.; Heesterbeek, H.; Klinkenberg, D.; Hollingsworth, T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet 2020, 395, 931–934. [Google Scholar] [CrossRef]
- Klemeš, J.J.; Fan, Y.V.; Jiang, P. The energy and environmental footprints of COVID-19 fighting measures–PPE, disinfection, supply chains. Energy 2020, 211, 118701. [Google Scholar] [CrossRef] [PubMed]
- Arup. Health Care Climate Footprint Report. 2019. Available online: https://noharm-uscanada.org/content/global/health-care-climate-footprint-report (accessed on 29 October 2020).
- The World Bank. Climate-Smart Healthcare: Low-Carbon and Resilience Strategies for the Health Sector. 2017. Available online: http://documents1.worldbank.org/curated/en/322251495434571418/pdf/113572-WP-PUBLIC-FINAL-WBG-Climate-smart-Healthcare-002.pdf (accessed on 29 October 2020).
- Chung, J.W.; Meltzer, D.O. Estimate of the carbon footprint of the US health care sector. JAMA 2009, 302, 1970–1972. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eckelman, M.J.; Sherman, J. Environmental impacts of the US health care system and effects on public health. PLoS ONE 2016, 11, e0157014. [Google Scholar] [CrossRef] [Green Version]
- Blumenthal, D.; Fowler, E.J.; Abrams, M.; Collins, S.R. COVID-19—Implications for the health care system. N. Engl. J. Med. 2020, 383, 1483–1488. [Google Scholar] [CrossRef]
- Graff, M.; Carley, S. COVID-19 assistance needs to target energy insecurity. Nat. Energy 2020, 5, 352–354. [Google Scholar] [CrossRef]
- Phillips, C.A.; Caldas, A.; Cleetus, R.; Dahl, K.A.; Declet-Barreto, J.; Licker, R.; Merner, D.; Pablo Ortiz-Partida, J.; Phelan, A.L.; Spanger-Siegfried, E.; et al. Compound climate risks in the COVID-19 pandemic. Nat. Clim. Chang. 2020, 10, 586–588. [Google Scholar] [CrossRef]
- Ridwan, R. COVID-19 and dengue: A deadly duo. Trop. Dr. 2020, 50, 270–272. [Google Scholar] [CrossRef]
- Rubin, R. What happens when COVID-19 collides with flu season? JAMA 2020, 324, 923–925. [Google Scholar] [CrossRef]
- Bhatt, S.; Gething, P.W.; Brady, O.J.; Messina, J.P.; Farlow, A.W.; Moyes, C.L.; Drake, J.M.; Brownstein, J.S.; Hoen, A.G.; Sankoh, O.; et al. The global distribution and burden of dengue. Nature 2013, 496, 504–507. [Google Scholar] [CrossRef] [PubMed]
- Navarro, J.C.; Arrivillaga-Henríquez, J.; Salazar-Loor, J.; Rodriguez-Morales, A.J. COVID-19 and dengue, co-epidemics in Ecuador and other countries in Latin America: Pushing strained health care systems over the edge. Travel Med. Infect. Dis. 2020, 37, 101656. [Google Scholar] [CrossRef] [PubMed]
- Paraguay Press Release. Paraguay Reports Most Dengue Cases in It’s History, COVID-19 Pandemic Has Complicated the Situation. 2020. Available online: http://outbreaknewstoday.com/paraguay-reports-most-dengue-cases-in-its-history-covid-19-pandemic-has-complicated-the-situation-62620/ (accessed on 30 October 2020).
- Yong, C. NEA Starts Intensive Dengue Exercise; Cases at Record High. 2020. Available online: https://www.straitstimes.com/singapore/nea-starts-intensive-dengue-exercise-cases-at-record-high (accessed on 30 October 2020).
- National Environment Agency (NEA). 2020. Available online: https://www.nea.gov.sg/media/news/news/index/number-of-weekly-dengue-cases-expected-to-exceed-the-historical-high-of-891-unless-urgent-collective-community-action-is-taken (accessed on 30 October 2020).
- Lam, L.T.; Chua, Y.X.; Tan, D.H. Roles and challenges of primary care physicians facing a dual outbreak of COVID-19 and dengue in Singapore. Fam. Pract. 2020, 37, 578–579. [Google Scholar] [CrossRef] [PubMed]
- Yan, G.; Lee, C.K.; Lam, L.T.; Yan, B.; Chua, Y.X.; Lim, A.Y.; Phang, K.F.; Kew, G.S.; Teng, H.; Ngai, C.H.; et al. Covert COVID-19 and false-positive dengue serology in Singapore. Lancet Infect. Dis. 2020, 20, 536. [Google Scholar] [CrossRef] [Green Version]
- Biswas, S.; Sukla, S. COVID-19 virus infection and transmission are observably less in highly dengue-endemic countries: Is pre-exposure to dengue virus protective against COVID-19 severity and mortality? Will the reverse scenario be true? Clin. Exp. Investig. 2020, 1, 1–5. [Google Scholar] [CrossRef]
- Nicolelis, M.A.; Raimundo, R.L.; Peixoto, P.S.; de Andreazzi, C.S. How super-spreader cities, highways, hospital bed availability, and dengue fever influenced the COVID-19 epidemic in Brazil. medRxiv 2020. [Google Scholar] [CrossRef]
- Jones, N. How coronavirus lockdowns stopped flu in its tracks. Nature 2020. [Google Scholar] [CrossRef]
- Soo, R.J.J.; Chiew, C.J.; Ma, S.; Pung, R.; Lee, V. Decreased influenza incidence under COVID-19 control measures, Singapore. Emerg. Infect. Dis. 2020, 26, 1933. [Google Scholar] [CrossRef]
- Lwin, M.O.; Lu, J.; Sheldenkar, A.; Schulz, P.J.; Shin, W.; Gupta, R.; Yang, Y. Global sentiments surrounding the COVID-19 pandemic on Twitter: Analysis of Twitter trends. JMIR Public Health Surveill. 2020, 6, e19447. [Google Scholar] [CrossRef]
- Mandavilli, A. The New York Times. ‘The Biggest Monster’ is Spreading. And It’s Not the Coronavirus. 2020. Available online: https://www.nytimes.com/2020/08/03/health/coronavirus-tuberculosis-aids-malaria.html (accessed on 30 October 2020).
- Stop TB Partnership. The Potential Impact of the COVID-19 Response on Tuberculosis in High-Burden Countries: A Modelling Analysis. 2020. Available online: http://www.stoptb.org/assets/documents/news/Modeling%20Report_1%20May%202020_FINAL.pdf (accessed on 30 October 2020).
- Cavallo, J.J.; Donoho, D.A.; Forman, H.P. Hospital capacity and operations in the coronavirus disease 2019 (COVID-19) pandemic—planning for the nth patient. JAMA Health Forum 2020, 1, e200345. [Google Scholar] [CrossRef]
- Cohen, I.G.; Gostin, L.O.; Weitzner, D.J. Digital smartphone tracking for COVID-19: Public health and civil liberties in tension. JAMA 2020, 323, 2371–2372. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, M.; Dewatripont, M.; Muraille, E.; Platteau, J.P.; Goldman, M. Preparing for a responsible lockdown exit strategy. Nat. Med. 2020, 26, 643–644. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, P.; Fu, X.; Fan, Y.V.; Klemeš, J.J.; Chen, P.; Ma, S.; Zhang, W. Spatial-temporal potential exposure risk analytics and urban sustainability impacts related to COVID-19 mitigation: A perspective from car mobility behaviour. J. Clean. Prod. 2021, 279, 123673. [Google Scholar] [CrossRef] [PubMed]
- Apicella, M.; Campopiano, M.C.; Mantuano, M.; Mazoni, L.; Coppelli, A.; Del Prato, S. COVID-19 in people with diabetes: Understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol. 2020, 8, 782–792. [Google Scholar] [CrossRef]
- Charlton, E. 28 Million Elective Surgeries May Be Cancelled Worldwide: How Non-COVID-19 Medical Care Is Suffering. 2020. Available online: https://www.weforum.org/agenda/2020/05/covid-19-elective-surgery-cancellation-cancer-pandemic/ (accessed on 18 November 2020).
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Silver, R.C.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Doraiswamy, P.M. Digital Medicine Can Diagnose and Treat What Ails You. Scientific American. Available online: https://www.com/article/digital-medicine-can-diagnose-and-treat-what-ails-you/ (accessed on 15 November 2020).
- Loeb, A.E.; Rao, S.S.; Ficke, J.R.; Morris, C.D.; Riley, L.H., III; Levin, A.S. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J. Am. Acad. Orthop. Surg. 2020, 28, e469–e476. [Google Scholar] [CrossRef]
- Iyengar, K.; Jain, V.K.; Vaishya, R. Pitfalls in telemedicine consultations in the era of COVID 19 and how to avoid them. Diabetes Metab. Syndr. 2020, 14, 797–799. [Google Scholar]
- Ting, D.S.W.; Carin, L.; Dzau, V.; Wong, T.Y. Digital technology and COVID-19. Nat. Med. 2020, 26, 459–461. [Google Scholar] [CrossRef] [Green Version]
- Fusco, A.; Dicuonzo, G.; Dell’Atti, V.; Tatullo, M. Blockchain in Healthcare: Insights on COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 7167. [Google Scholar] [CrossRef]
- Khan, Z.H.; Siddique, A.; Lee, C.W. Robotics Utilization for Healthcare Digitization in Global COVID-19 Management. Int. J. Environ. Res. Public Health 2020, 17, 3819. [Google Scholar] [CrossRef]
- Research and Markets. Remote Healthcare (mHealth, Tele-ICUs, & Virtual Health) Market—Global Outlook and Forecast 2020–2025. 2020. Available online: https://www.researchandmarkets.com/reports/5125678/remote-healthcare-mhealth-tele-icus-and (accessed on 30 October 2020).
- Webster, P. Virtual health care in the era of COVID-19. Lancet 2020, 395, 1180–1181. [Google Scholar] [CrossRef]
- Dorsey, E.R.; Topol, E.J. Telemedicine 2020 and the next decade. Lancet 2020, 395, 859. [Google Scholar] [CrossRef]
- Bardhan, I.; Chen, H.; Karahanna, E. Connecting systems, data, and people: A multidisciplinary research roadmap for chronic disease management. Manag. Inf. Syst. Q. 2020, 44, 185–200. [Google Scholar]
- Anthes, E. Alexa, do I have COVID-19? Nature 2020, 586, 22–25. [Google Scholar] [CrossRef]
- Gravitz, L. Technology: Monitoring gets personal. Nature 2016, 538, S8–S10. [Google Scholar] [CrossRef] [Green Version]
- Strubell, E.; Ganesh, A.; McCallum, A. Energy and policy considerations for deep learning in NLP. arXiv 2019, arXiv:1906.02243. [Google Scholar]
- Bertoldi, P.; Avgerinou, M.; Castellazzi, L. Trends in Data Centre Energy Consumption under the European Code of Conduct for Data Centre Energy Efficiency, EUR 28874 EN; Publications Office of the European Union: Luxembourg, 2017; ISBN 978-92-79-76445-5. JRC108354. [Google Scholar] [CrossRef]
- Masanet, E.; Shehabi, A.; Lei, N.; Smith, S.; Koomey, J. Recalibrating global data center energy-use estimates. Science 2020, 367, 984–986. [Google Scholar] [CrossRef]
- Holmner, Å.; Ebi, K.L.; Lazuardi, L.; Nilsson, M. Carbon footprint of telemedicine solutions-unexplored opportunity for reducing carbon emissions in the health sector. PLoS ONE 2014, 9, e105040. [Google Scholar] [CrossRef] [Green Version]
- Wyatt, K.D.; Poole, L.R.; Mullan, A.F.; Kopecky, S.L.; Heaton, H.A. Clinical evaluation and diagnostic yield following evaluation of abnormal pulse detected using Apple Watch. J. Am. Med. Inform. Assoc. 2020, 27, 1359–1363. [Google Scholar] [CrossRef]
- Majumder, S.; Mondal, T.; Deen, M.J. Wearable sensors for remote health monitoring. Sensors 2017, 17, 130. [Google Scholar] [CrossRef]
- Ghosh, A.; Raha, A.; Mukherjee, A. Energy-efficient IoT-health monitoring system using approximate computing. Internet Things 2020, 9, 100166. [Google Scholar] [CrossRef]
- Saba, T.; Haseeb, K.; Ahmed, I.; Rehman, A. Secure and energy-efficient framework using Internet of Medical Things for e-healthcare. J. Infect. Public Health 2020, 13, 1567–1575. [Google Scholar] [CrossRef] [PubMed]
- Arora, N.; Robinson, K.; Charm, T.; Grimmelt, A.; Ortega, M.; Staack, Y.; Whitehead, S.; Yamakawa, N. Consumer Sentiment and Behavior Continue to Reflect the Uncertainty of the COVID-19 Crisis. 2020. Available online: https://www.mckinsey.com/business-functions/marketing-and-sales/our-insights/a-global-view-of-how-consumer-behavior-is-changing-amid-covid-19# (accessed on 28 October 2020).
- Klemeš, J.J.; Fan, Y.V.; Tan, R.R.; Jiang, P. Minimising the present and future plastic waste, energy and environmental footprints related to COVID-19. Renew. Sustain. Energy Rev. 2020, 127, 109883. [Google Scholar] [CrossRef]
- IEA. Global Energy Review 2020: The Impacts of the COVID-19 Crisis on Global Energy Demand and CO2 Emissions; International Energy Agency (IEA): Paris, France, 2020. Available online: https://www.iea.org/reports/global-energy-review-2020 (accessed on 30 October 2020).
- Senthilkumar, V.S.; Reddy, K.S.; Subramaniam, U. COVID-19: Impact analysis and recommendations for power and energy sector operation. Appl. Energy 2020, 279, 115739. [Google Scholar]
- IEA. Global Energy and CO2 Emissions in 2020; International Energy Agency (IEA): Paris, France, 2020. Available online: https://www.iea.org/reports/global-energy-review-2020/global-energy-and-co2-emissions-in-2020#abstract (accessed on 30 October 2020).
- Klemeš, J.J.; Fan, Y.V.; Jiang, P. COVID-19 pandemic facilitating energy transition opportunities. Int. J. Energy Res. 2020. [Google Scholar] [CrossRef]
- Anser, M.K.; Yousaf, Z.; Khan, M.A.; Voo, X.H.; Nassani, A.A.; Alotaibi, S.M.; Abro, M.M.Q.; Khalid Zaman, K. The impacts of COVID-19 measures on global environment and fertility rate: Double coincidence. Air Qual. Atmos. Health 2020, 13, 1083–1092. [Google Scholar] [CrossRef]
- Hosseini, S.E. An outlook on the global development of renewable and sustainable energy at the time of COVID-19. Energy Res. Soc. Sci. 2020, 68, 101633. [Google Scholar] [CrossRef]
- Walsh, D.; Nayler, S. Nuclear Power and the COVID-19 Crisis. Environ. J. 2020. Available online: https://environmentjournal.online/articles/nuclear-power-and-the-turbulent-times/ (accessed on 16 November 2020).
- Sovacool, B.K.; Schmid, P.; Stirling, A.; Walter, G.; MacKerron, G. Differences in carbon emissions reduction between countries pursuing renewable electricity versus nuclear power. Nat. Energy 2020, 5, 928–935. [Google Scholar] [CrossRef]
- Yoneoka, S.; Millison, D. COVID-19 is an Opportunity to Re-Tool the Health Sector’s Energy Supply. 2020. Available online: https://blogs.adb.org/COVID-19-opportunity-to-re-tool-healthsector-s-energy-supply (accessed on 30 October 2020).
- Brosemer, K.; Schelly, C.; Gagnon, V.; Arola, K.L.; Pearce, J.M.; Bessette, D.; Olabisi, L.S. The energy crises revealed by COVID: Intersections of indigeneity, inequity, and health. Energy Res. Soc. Sci. 2020, 68, 101661. [Google Scholar] [CrossRef]
- Wang, J.; Shen, J.; Ye, D.; Yan, X.; Zhang, Y.; Yang, W.; Li, X.; Wang, J.; Zhang, L.; Pan, L. Disinfection technology of hospital wastes and wastewater: Suggestions for disinfection strategy during coronavirus Disease 2019 (COVID-19) pandemic in China. Environ. Pollut. 2020, 262, 114665. [Google Scholar] [CrossRef]
- Mandal, I.; Pal, S. COVID-19 pandemic persuaded lockdown effects on environment over stone quarrying and crushing areas. Sci. Total Environ. 2020, 732, 139281. [Google Scholar] [CrossRef] [PubMed]
- Lecocq, T.; Hicks, S.P.; Van Noten, K.; Van Wijk, K.; Koelemeijer, P.; De Plaen, R.S.; Massin, F.; Hillers, G.; Anthony, R.E.; Apoloner, M.T.; et al. Global quieting of high-frequency seismic noise due to COVID-19 pandemic lockdown measures. Science 2020, 369, 1338–1343. [Google Scholar] [CrossRef]
- Shakil, M.H.; Munim, Z.H.; Tasnia, M.; Sarowar, S. COVID-19 and the environment: A critical review and research agenda. Sci. Total Environ. 2020, 745, 141022. [Google Scholar] [CrossRef] [PubMed]
- Cheval, S.; Mihai Adamescu, C.; Georgiadis, T.; Herrnegger, M.; Piticar, A.; Legates, D.R. Observed and potential impacts of the COVID-19 pandemic on the environment. Int. J. Environ. Res. Public Health 2020, 17, 4140. [Google Scholar] [CrossRef] [PubMed]
- Le Quéré, C.; Jackson, R.B.; Jones, M.W.; Smith, A.J.; Abernethy, S.; Andrew, R.M.; De-Gol, A.J.; Willis, D.R.; Shan, Y.; Canadell, J.G.; et al. Temporary reduction in daily global CO2 emissions during the COVID-19 forced confinement. Nat. Clim. Chang. 2020, 10, 647–653. [Google Scholar] [CrossRef]
- Liu, Z.; Ciais, P.; Deng, Z.; Lei, R.; Davis, S.J.; Feng, S.; Zheng, B.; Cui, D.; Dou, X.; Zhu, B.; et al. Near-real-time monitoring of global CO2 emissions reveals the effects of the COVID-19 pandemic. Nat. Commun. 2020, 11, 5172. [Google Scholar] [CrossRef]
- Chen, L.W.A.; Chien, L.C.; Li, Y.; Lin, G. Nonuniform impacts of COVID-19 lockdown on air quality over the United States. Sci. Total Environ. 2020, 745, 141105. [Google Scholar] [CrossRef]
- Zhang, Z.; Xue, T.; Jin, X. Effects of meteorological conditions and air pollution on COVID-19 transmission: Evidence from 219 Chinese cities. Sci. Total Environ. 2020, 741, 140244. [Google Scholar] [CrossRef]
- United in Science Report: Climate Change Has Not Stopped for COVID-19. Available online: https://www.unenvironment.org/news-and-stories/press-release/united-science-report-climate-change-has-not-stopped-covid19 (accessed on 29 October 2020).
- Wang, Q.; Lu, M.; Bai, Z.; Wang, K. Coronavirus pandemic reduced China’s CO2 emissions in short-term, while stimulus packages may lead to emissions growth in medium-and long-term. Appl. Energy 2020, 278, 115735. [Google Scholar] [CrossRef]
- Le, T.; Wang, Y.; Liu, L.; Yang, J.; Yung, Y.L.; Li, G.; Seinfeld, J.H. Unexpected air pollution with marked emission reductions during the COVID-19 outbreak in China. Science 2020, 369, 702–706. [Google Scholar] [CrossRef]
- Tobías, A.; Carnerero, C.; Reche, C.; Massagué, J.; Via, M.; Minguillón, M.C.; Alastuey, A.; Querol, X. Changes in air quality during the lockdown in Barcelona (Spain) one month into the SARS-CoV-2 epidemic. Sci. Total Environ. 2020, 726, 138540. [Google Scholar] [CrossRef] [PubMed]
- Adams, M.D. Air pollution in Ontario, Canada during the COVID-19 State of Emergency. Sci. Total Environ. 2020, 742, 140516. [Google Scholar] [CrossRef] [PubMed]
- Muhammad, S.; Long, X.; Salman, M. COVID-19 pandemic and environmental pollution: A blessing in disguise? Sci. Total Environ. 2020, 728, 138820. [Google Scholar] [CrossRef] [PubMed]
- Duer, J. The Plastic Pandemic Is only Getting Worse during COVID-19. 2020. Available online: https://www.weforum.org/agenda/2020/07/plastic-waste-management-covid19-ppe/ (accessed on 29 October 2020).
- Prata, J.C.; Silva, A.L.; Walker, T.R.; Duarte, A.C.; Rocha-Santos, T. COVID-19 pandemic repercussions on the use and management of plastics. Environ. Sci. Technol. 2020, 54, 7760–7765. [Google Scholar] [CrossRef] [PubMed]
- Adyel, T.M. Accumulation of plastic waste during COVID-19. Science 2020, 369, 1314–1315. [Google Scholar]
- Praphornkul, P. COVID-19 Has Positive Impact on Ecosystem. 2020. Available online: https://thainews.prd.go.th/en/news/detail/TCATG200418155259223 (accessed on 30 October 2020).
- Hicks, R. COVID-19 Has Hobbled Asia’s Recycling Trade as Demand for Recycled Plastic Dips and Recyclers Face Ruin. 2020. Available online: https://www.eco-business.com/zh-hans/news/covid-19-has-hobbled-asias-recycling-trade-as-demand-for-recycled-plastic-dips-and-recyclers-face-ruin/ (accessed on 30 October 2020).
- Sarkodie, S.A.; Owusu, P.A. Impact of COVID-19 pandemic on waste management. Environ. Dev. Sustain. 2020. [Google Scholar] [CrossRef]
- Urban, R.C.; Nakada, L.Y.K. COVID-19 pandemic: Solid waste and environmental impacts in Brazil. Sci. Total Environ. 2021, 755, 142471. [Google Scholar] [CrossRef]
- Fan, Y.V.; Jiang, P.; Hemzal, M.; Klemeš, J.J. An update of COVID-19 influence on waste management. Sci. Total Environ. 2021, 754, 142014. [Google Scholar] [CrossRef]
- Low, D.W.; Koh, A. Singapore’s Food Delivery Surge during Lockdown Highlights Waste Problems. 2020. Available online: www.bloomberg.com/news/articles/2020-06-24/singapore-binges-on-plastics-ordering-food-during-virus-lockdown (accessed on 30 October 2020).
- Staub, C. City Data Shows COVID-19 Impacts on Recycling Tonnages. Available online: https://resource-recycling.com/recycling/2020/04/28/city-data-shows-covid-19-impacts-on-recycling-tonnages (accessed on 30 October 2020).
- WRM. Ontario Residents Generate More Garbage during Pandemic. Waste & Recycling Magazine (WRM). Available online: https://www.wasterecyclingmag.ca/municpal-waste/ontario-residents-generate-more-garbage-during-pandemic/1003283746/ (accessed on 30 October 2020).
- Farrer, M. Australian Councils Struggle with Huge Rise in Household Rubbish during COVID-19 Lockdown. 2020. Available online: https://www.theguardian.com/australia-news/2020/jun/03/australian-councils-struggle-with-huge-rise-in-household-rubbish-during-covid-19-lockdown (accessed on 30 October 2020).
- Co, C. More Refuse Collected from HDB Estates during Circuit Breaker Period: Town Councils. 2020. Available online: https://www.channelnewsasia.com/news/singapore/covid19-circuit-breaker-household-waste-increase-12680454 (accessed on 30 October 2020).
- Dzhanova, Y. Sanitation Workers Battle Higher Waste Levels in Residential Areas as Coronavirus Outbreak Persists. 2020. Available online: https://www.cnbc.com/2020/05/16/coronavirus-sanitation-workers-battle-higher-waste-levels.html (accessed on 30 October 2020).
- Oyedotun, T.D.T.; Kasim, O.F.; Famewo, A.; Oyedotun, T.D.; Moonsammy, S.; Ally, N.; Renn-Moonsammy, D.M. Municipal waste Management in the era of COVID-19: Perceptions, Practices, and Potentials for Research in Developing Countries. Res. Glob. 2020, 2, 100033. [Google Scholar]
- Naughton, C.C. Will the COVID-19 pandemic change waste generation and composition? The need for more real-time waste management data and systems thinking. Resour. Conserv. Recycl. 2020, 162, 105050. [Google Scholar] [CrossRef]
- You, S.; Sonne, C.; Ok, Y.S. COVID-19’s unsustainable waste management. Science 2020, 368, 1438. [Google Scholar]
- Zambrano-Monserrate, M.A.; Ruano, M.A.; Sanchez-Alcalde, L. Indirect effects of COVID-19 on the environment. Sci. Total Environ. 2020, 728, 138813. [Google Scholar] [CrossRef] [PubMed]
- Shanghai observer. Has Shanghai’s Garbage Sorting Regressed during the Pandemic? The Latest “Monthly Report” Says. 2020. Available online: https://www.jfdaily.com/news/detail?id=237811 (accessed on 30 October 2020).
- Jiang, P.; Fan, Y.V.; Zhou, J.; Zheng, M.; Liu, X.; Klemeš, J.J. Data-driven analytical framework for waste-dumping behaviour analysis to facilitate policy regulations. Waste Manag. 2020, 103, 285–295. [Google Scholar] [CrossRef]
- Sarc, R.; Curtis, A.; Kandlbauer, L.; Khodier, K.; Lorber, K.E.; Pomberger, R. Digitalisation and intelligent robotics in value chain of circular economy oriented waste management–A review. Waste Manag. 2019, 95, 476–492. [Google Scholar] [CrossRef] [PubMed]
- Abdallah, M.; Talib, M.A.; Feroz, S.; Nasir, Q.; Abdalla, H.; Mahfood, B. Artificial intelligence applications in solid waste management: A systematic research review. Waste Manag. 2020, 109, 231–246. [Google Scholar] [CrossRef] [PubMed]
- Countryside Alliance. Coronavirus Lockdown Sees Huge Rise in Fly-Tipping across UK. 2020. Available online: https://www.itv.com/news/2020-04-14/coronavirus-lockdown-sees-huge-rise-in-fly-tipping-across-uk (accessed on 30 October 2020).
- Mihai, F.C. Assessment of COVID-19 waste flows during the emergency state in Romania and related public health and environmental concerns. Int. J. Environ. Res. Public Health 2020, 17, 5439. [Google Scholar] [CrossRef] [PubMed]
- Nzediegwu, C.; Chang, S.X. Improper solid waste management increases potential for COVID-19 spread in developing countries. Resour. Conserv. Recycl. 2020, 161, 104947. [Google Scholar] [CrossRef] [PubMed]
- Howard, D.B.; Soria, R.; Thé, J.; Schaeffer, R.; Saphores, J.D. The energy-climate-health nexus in energy planning: A case study in Brazil. Renew. Sustain. Energy Rev. 2020, 132, 110016. [Google Scholar] [CrossRef]
- Romero-Lankao, P.; McPhearson, T.; Davidson, D.J. The food-energy-water nexus and urban complexity. Nat. Clim. Chang. 2017, 7, 233–235. [Google Scholar] [CrossRef]
- Wang, X.C.; Klemeš, J.J.; Wang, Y.; Dong, X.; Wei, H.; Xu, Z.; Varbanov, P.S. Water-Energy-Carbon Emissions nexus analysis of China: An environmental input-output model-based approach. Appl. Energy 2020, 261, 114431. [Google Scholar] [CrossRef]
- Ching, J.; Kajino, M. Rethinking air quality and climate change after COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 5167. [Google Scholar] [CrossRef] [PubMed]
- Pires, A.; Martinho, G. Waste hierarchy index for circular economy in waste management. Waste Manag. 2019, 95, 298–305. [Google Scholar] [CrossRef]
- Steffen, B.; Egli, F.; Pahle, M.; Schmidt, T.S. Navigating the clean energy transition in the COVID-19 crisis. Joule 2020, 4, 1137–1141. [Google Scholar] [CrossRef] [PubMed]
- IoT Business News. Global Research Shows Healthcare, Energy and Environment as Top Consumer Priorities for Tech and Innovation. 2015. Available online: https://iotbusinessnews.com/2015/04/21/69441-global-research-shows-healthcare-energy-and-environment-as-top-consumer-priorities-for-tech-and-innovation/ (accessed on 30 October 2020).
- Lim, H.R.; Kim, H.S.; Qazi, R.; Kwon, Y.T.; Jeong, J.W.; Yeo, W.H. Advanced soft materials, sensor integrations, and applications of wearable flexible hybrid electronics in healthcare, energy, and environment. Adv. Mater. 2020, 32, 1901924. [Google Scholar] [CrossRef]
- Sarkis, J.; Cohen, M.J.; Dewick, P.; Schröder, P. A brave new world: Lessons from the COVID-19 pandemic for transitioning to sustainable supply and production. Resour. Conserv. Recycl. 2020, 159, 104894. [Google Scholar] [CrossRef] [PubMed]
- Sisson, P. How the ‘15-Minute City’ Could Help Post-Pandemic Recovery. 2020. Available online: https://www.bloomberg.com/news/articles/2020-07-15/mayors-tout-the-15-minute-city-as-covid-recovery (accessed on 30 October 2020).
- Horton, R. Offline: The second wave. Lancet 2020, 395, 1960. [Google Scholar] [CrossRef]
- Mathiesen, B.V.; Lund, H.; Karlsson, K. 100% Renewable energy systems, climate mitigation and economic growth. Appl. Energy 2011, 88, 488–501. [Google Scholar] [CrossRef]
- C40. Advancing towards Zero Waste Declaration. 2020. Available online: https://www.c40.org/other/zero-waste-declaration (accessed on 28 October 2020).
- European Commission. 2050 Long-Term Strategy. 2018. Available online: https://ec.europa.eu/clima/policies/strategies/2050_en (accessed on 28 October 2020).
- European Commission. A European Green Deal: Striving to Be the First Climate-Neutral Continent. 2019. Available online: https://ec.europa.eu/info/strategy/priorities-2019-2024/european-green-deal_en (accessed on 30 October 2020).
- Kissler, S.M.; Tedijanto, C.; Goldstein, E.; Grad, Y.H.; Lipsitch, M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science 2020, 368, 860–868. [Google Scholar] [CrossRef]
- Merchant, H. Coronavirus may stay with us forever! BMJ 2020, 369, m1790-rr. [Google Scholar]
- Murphy, N. Flu and Pneumonia Deaths Now Three Times Higher than Coronavirus after Steep Drop. 2020. Available online: https://www.mirror.co.uk/news/uk-news/flu-pneumonia-deaths-now-three-22400123#source=push (accessed on 30 October 2020).
- Faust, J.S.; Lin, Z.; Del Rio, C. Comparison of estimated excess deaths in New York city during the COVID-19 and 1918 influenza pandemics. JAMA Netw. Open 2020, 3, e2017527. [Google Scholar] [CrossRef]
- Favale, T.; Soro, F.; Trevisan, M.; Drago, I.; Mellia, M. Campus traffic and e-Learning during COVID-19 pandemic. Comput. Netw. 2020, 176, 107290. [Google Scholar] [CrossRef]
- Brynjolfsson, E.; Horton, J.J.; Ozimek, A.; Rock, D.; Sharma, G.; TuYe, H.Y. COVID-19 and remote work: An early look at US data. Natl. Bur. Econ. Res. 2020. [Google Scholar] [CrossRef]
- Kim, R.Y. The impact of COVID-19 on consumers: Preparing for digital sales. IEEE Eng. Manag. Rev. 2020, 48, 12–218. [Google Scholar] [CrossRef]
- Gensch, C.O.; Prakash, S.; Hilbert, I. Is digitalisation a driver for sustainability? In Sustainability in a Digital World; Springer: Cham, Switzerland, 2017; pp. 117–129. [Google Scholar]
- Bieser, J.C.; Hilty, L.M. Assessing indirect environmental effects of information and communication technology (ICT): A systematic literature review. Sustainability 2018, 10, 2662. [Google Scholar] [CrossRef] [Green Version]
- Royston, S. Digitalisation, Energy and Healthcare. 2019. Available online: http://www.demand.ac.uk/wp-content/uploads/2019/01/Digitalisation-energy-and-healthcare-working-paper.pdf (accessed on 28 October 2020).
- Itten, R.; Hischier, R.; Andrae, A.S.; Bieser, J.C.; Cabernard, L.; Falke, A.; Ferreboeuf, H.; Hilty, L.M.; Keller, R.L.; Lees-Perasso, E.; et al. Digital transformation—life cycle assessment of digital services, multifunctional devices and cloud computing. Int. J. Life Cycle Assess. 2020, 25, 2093–2098. [Google Scholar] [CrossRef]
- Čuček, L.; Klemeš, J.J.; Kravanja, Z. A review of footprint analysis tools for monitoring impacts on sustainability. J. Clean. Prod. 2012, 34, 9–20. [Google Scholar] [CrossRef]
- Manzanedo, R.D.; Manning, P. COVID-19: Lessons for the climate change emergency. Sci. Total Environ. 2020, 742, 140563. [Google Scholar] [CrossRef]
- Ibn-Mohammed, T.; Mustapha, K.B.; Godsell, J.M.; Adamu, Z.; Babatunde, K.A.; Akintade, D.D.; Acquaye, A.; Fujii, H.; Ndiaye, M.M.; Yamoah, F.A.; et al. A critical review of the impacts of COVID-19 on the global economy and ecosystems and opportunities for circular economy strategies. Resour. Conserv. Recycl. 2021, 164, 105169. [Google Scholar] [CrossRef]
- Emenike, S.N.; Falcone, G. A review on energy supply chain resilience through optimisation. Renew. Sustain. Energy Rev. 2020, 134, 110088. [Google Scholar] [CrossRef]
- Gates, B. Responding to COVID-19—A once-in-a-century pandemic? N. Engl. J. Med. 2020, 382, 1677–1679. [Google Scholar] [CrossRef]
- Simpson, S.; Kaufmann, M.C.; Glozman, V.; Chakrabarti, A. Disease X: Accelerating the development of medical countermeasures for the next pandemic. Lancet Infect. Dis. 2020, 20, e108–e115. [Google Scholar] [CrossRef] [Green Version]
- Botzen, W.; Duijndam, S.; van Beukering, P. Lessons for climate policy from behavioral biases towards COVID-19 and climate change risks. World Dev. 2020, 137, 105214. [Google Scholar] [CrossRef] [PubMed]
- Jiang, P.; Fan, Y.V.; Klemeš, J.J. Impacts of COVID-19 on energy demand and consumption: Challenges, lessons and emerging opportunities. Appl. Energy. 2021, 285, 116441. [Google Scholar] [CrossRef]





Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiang, P.; Klemeš, J.J.; Fan, Y.V.; Fu, X.; Bee, Y.M. More Is Not Enough: A Deeper Understanding of the COVID-19 Impacts on Healthcare, Energy and Environment Is Crucial. Int. J. Environ. Res. Public Health 2021, 18, 684. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18020684
Jiang P, Klemeš JJ, Fan YV, Fu X, Bee YM. More Is Not Enough: A Deeper Understanding of the COVID-19 Impacts on Healthcare, Energy and Environment Is Crucial. International Journal of Environmental Research and Public Health. 2021; 18(2):684. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18020684
Chicago/Turabian StyleJiang, Peng, Jiří Jaromír Klemeš, Yee Van Fan, Xiuju Fu, and Yong Mong Bee. 2021. "More Is Not Enough: A Deeper Understanding of the COVID-19 Impacts on Healthcare, Energy and Environment Is Crucial" International Journal of Environmental Research and Public Health 18, no. 2: 684. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18020684