Comorbidity of Geo-Helminthes among Malaria Outpatients of the Health Facilities in Ethiopia: Systematic Review and Meta-Analysis
Abstract
:1. Background
2. Methods
2.1. Search Strategy and Selection of Studies
2.2. Data Extraction and Management
2.3. Data Synthesis and Analysis
3. Results
3.1. Search
3.2. Included Study Characteristics
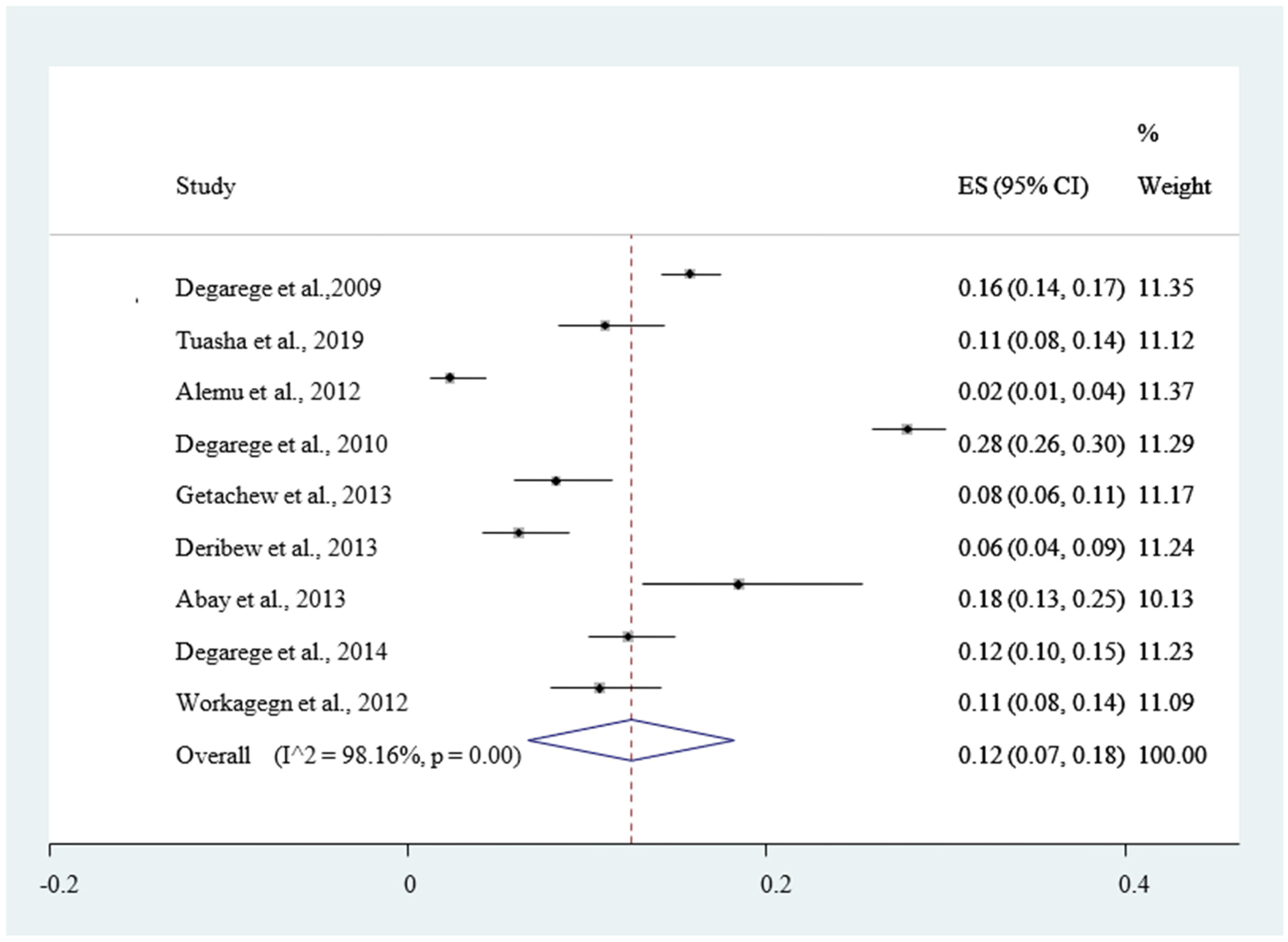
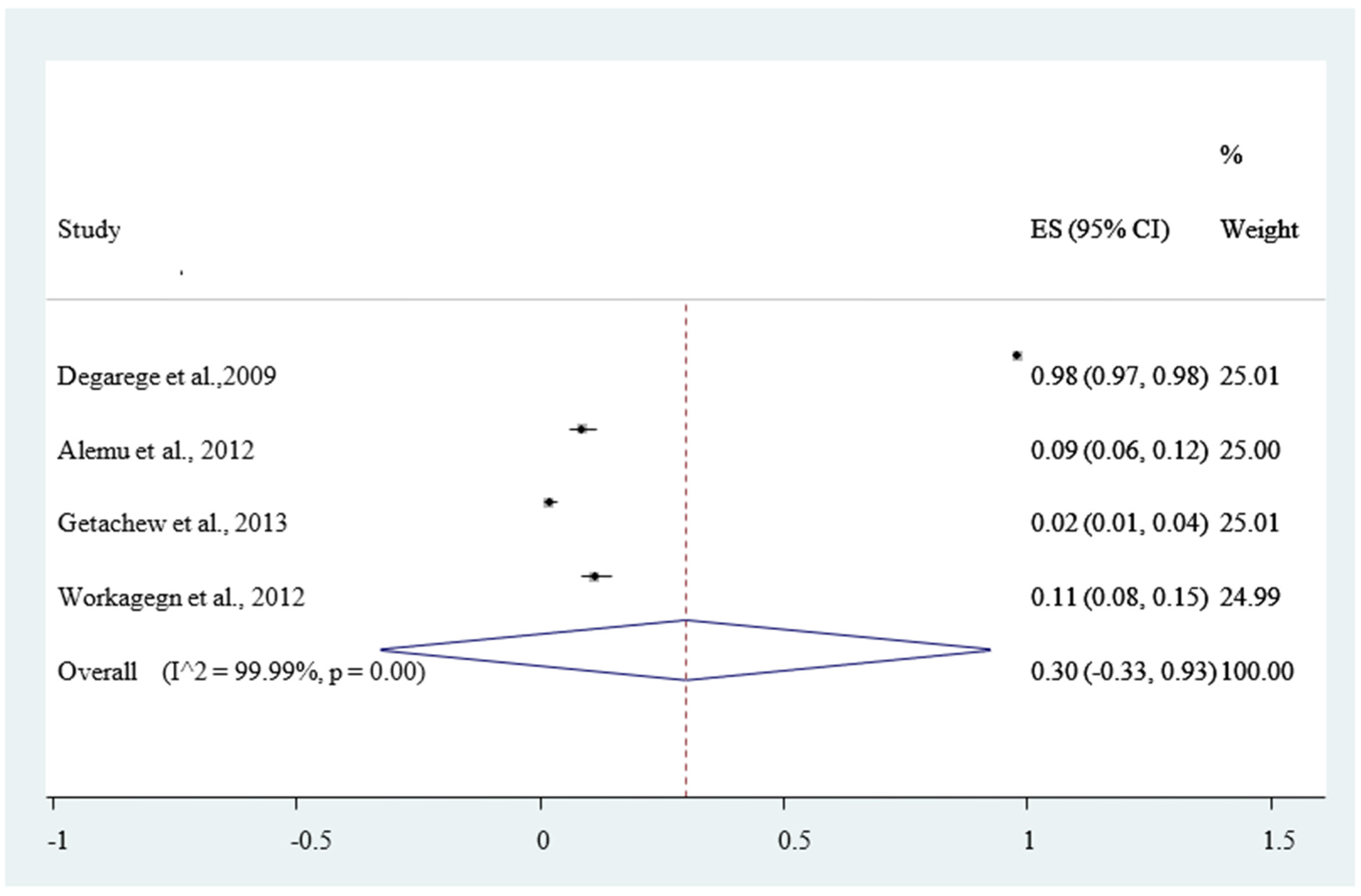
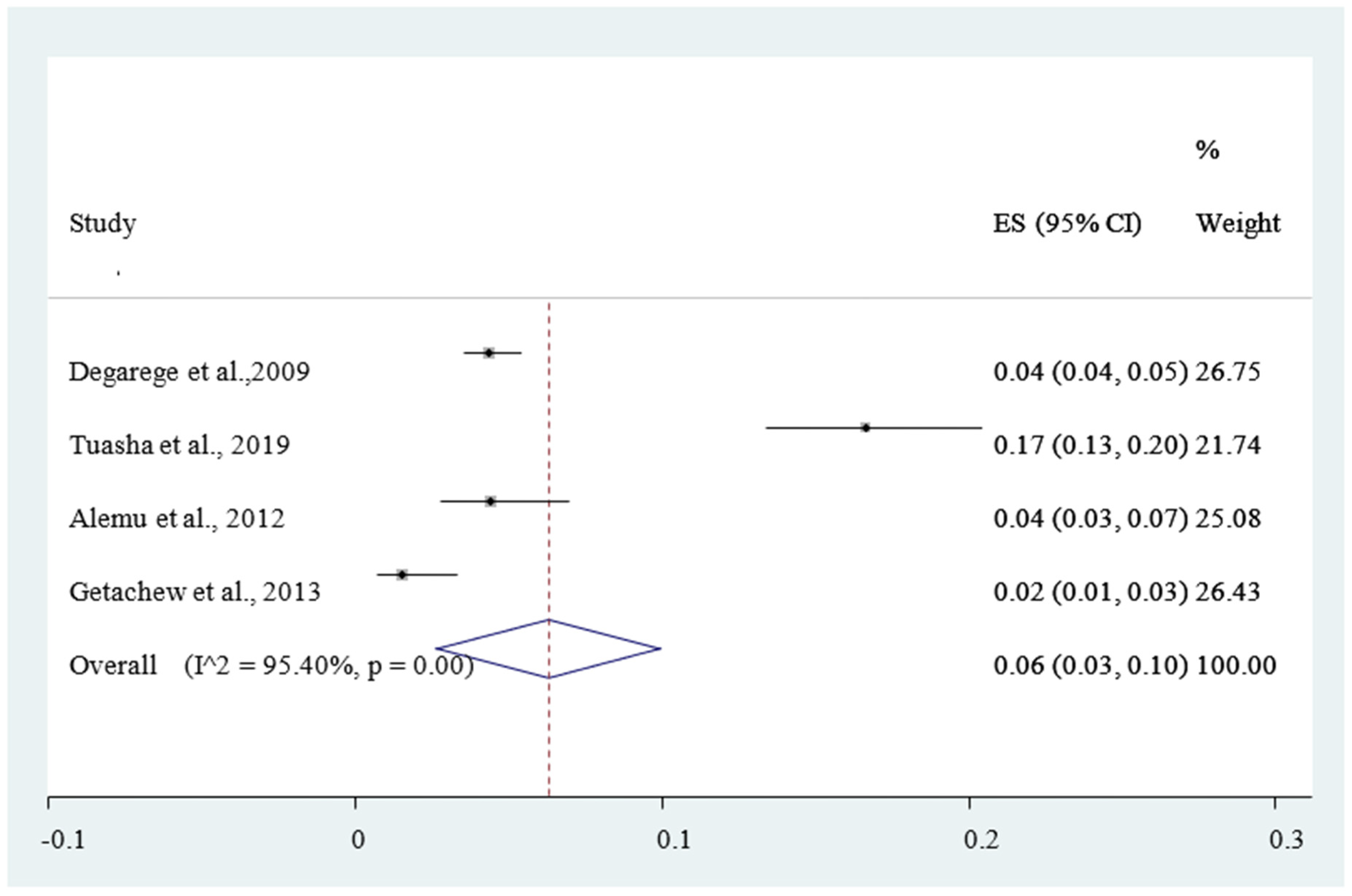
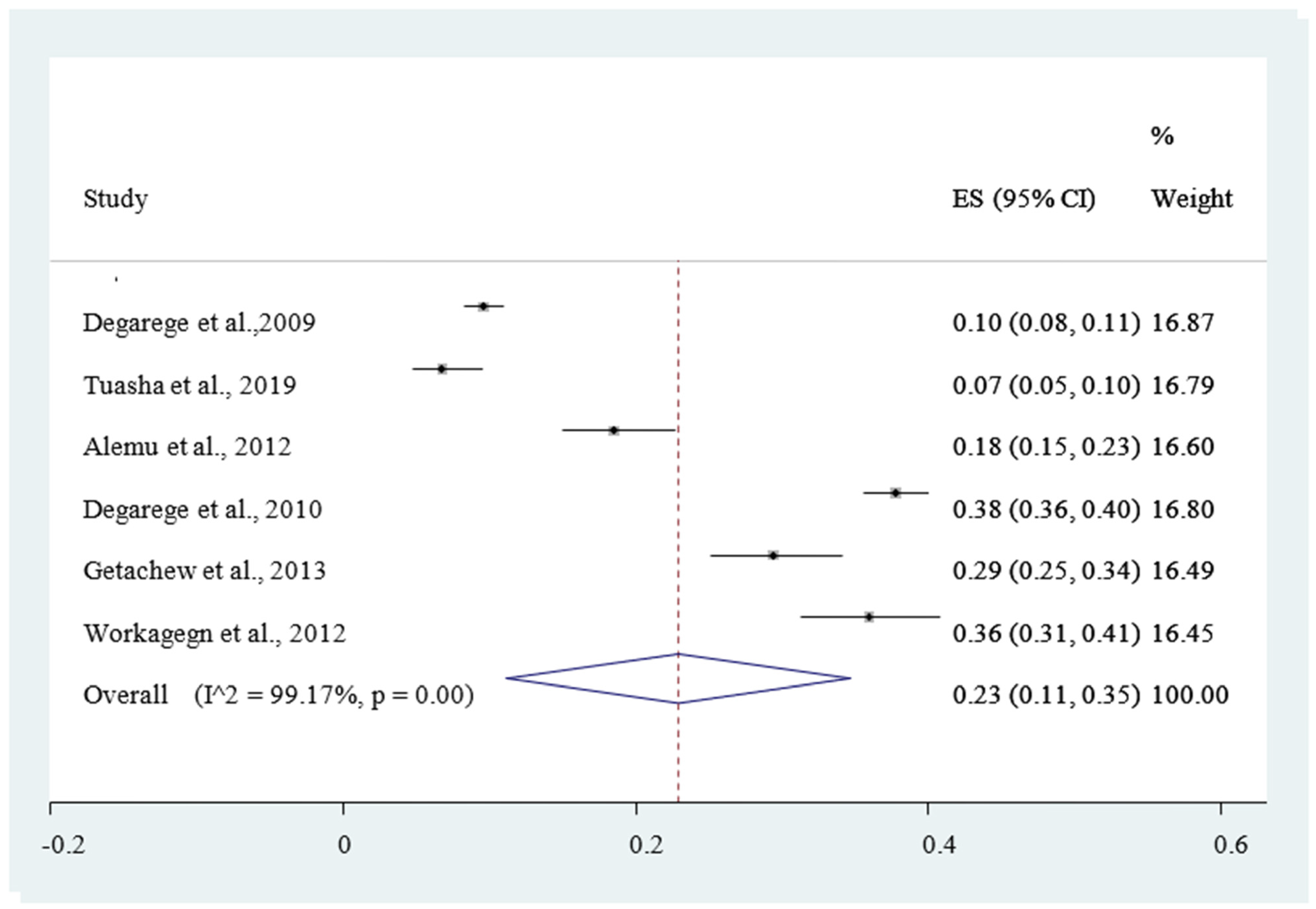
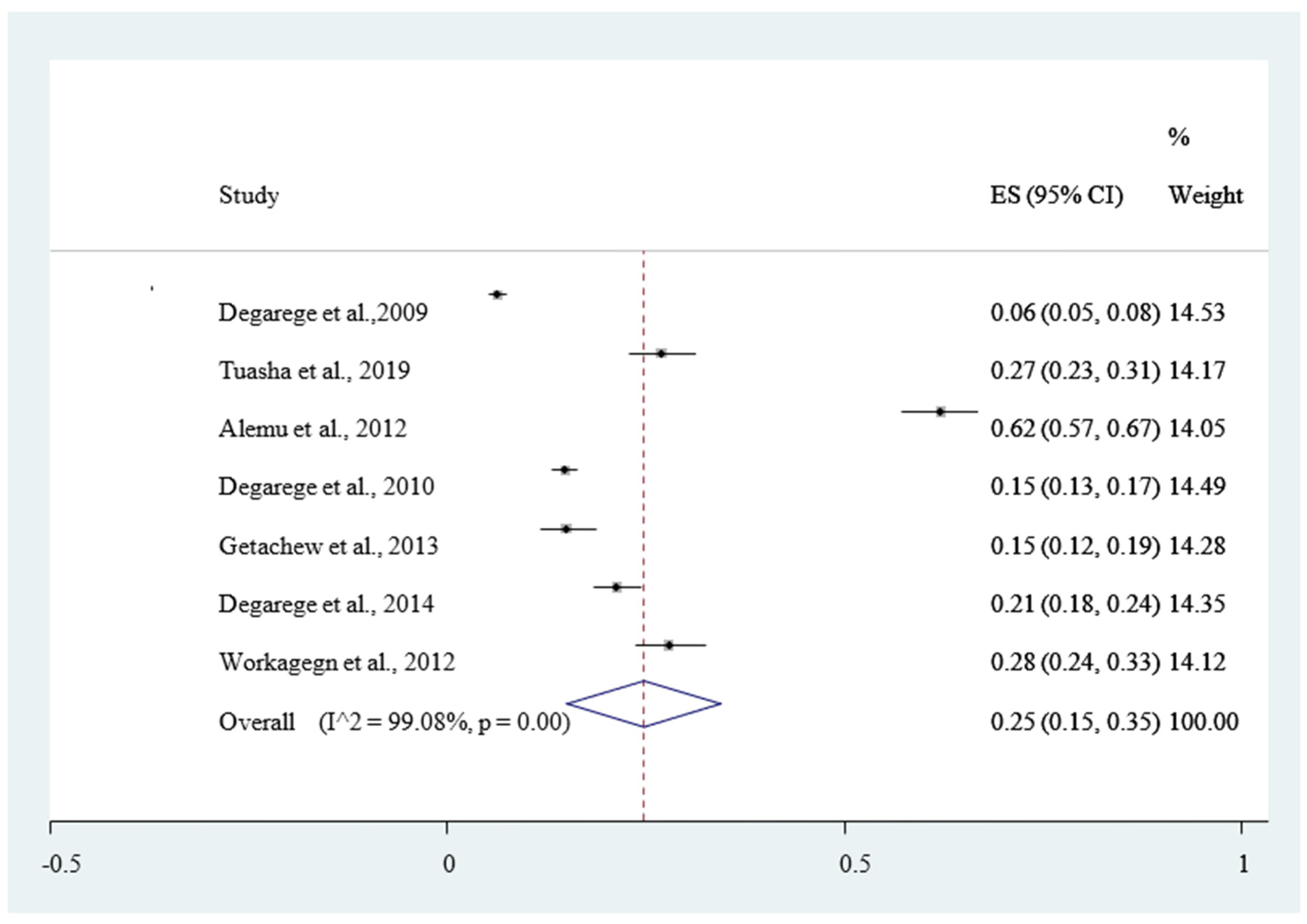
3.3. Pooled Prevalence of Malaria and Intestinal Helminthiases
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AHRI | Armauer Hansen Research Institute |
| EPHI | Ethiopian Public Health Institute |
| JBI | The Joanna Briggs Institute |
| JBI-MAStARI | The Joanna Briggs Institute Meta-Analysis of Statistical Assessment and Review Instrument |
| LMICs | Low- and Middle-Income Countries |
| MOH | Ministry of Health |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-analyses |
| PROSPERO | International Prospective Registry of Systematic Reviews |
| SDG | Sustainable Development Goal |
| SNNPR | Southern Nations Nationalities and Peoples Region |
| STH | Soil Transmitted Helminthiases |
| SSA | Sub-Saharan Africa |
| WHO | The World Health Organization |
References
- De Silva, N.R.; Brooker, S.; Hotez, P.J.; Montresor, A.; Engels, D.; Savioli, L. Soil-transmitted helminth infections: Updating the global picture. Trends Parasitol. 2003, 19, 547–551. [Google Scholar] [CrossRef] [PubMed]
- Njunda, A.L.; Fon, S.G.; Assob, J.C.; Nsagha, D.S.; Kwenti, T.D.; Kwenti, T.E. Coinfection with malaria and intestinal parasites, and its association with anaemia in children in Cameroon. Infect. Dis. Poverty 2015, 4, 43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kinung’hi, S.M.; Magnussen, P.; Kaatano, G.M.; Kishamawe, C.; Vennervald, B.J. Malaria and helminth co-infections in school and preschool children: A cross-sectional study in Magu district, north-western Tanzania. PLoS ONE 2014, 9, e86510. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The World Health Organization (WHO). The “World Malaria Report 2019”; World Health Organization: Geneva, Switzerland, 2020; Available online: https://apps.who.int/iris/bitstream/handle/10665/330011/9789241565721-eng.pdf (accessed on 4 August 2020).
- Makenga, G.; Menon, S.; Baraka, V.; Minja, D.T.; Nakato, S.; Delgado-Ratto, C.; Francis, F.; Lusingu, J.P.; Van Geertruyden, J.P. Prevalence of malaria parasite aemia in school-aged children and pregnant women in endemic settings of sub-Saharan Africa: A systematic review and meta-analysis. Parasite Epidemiol. Control 2020, 11, e00188. [Google Scholar] [CrossRef]
- The World Health Organization (WHO). Schistosomiasis. Available online: https://www.who.int/news-room/factsheets/detail/schistosomiasis (accessed on 26 July 2020).
- Efunshile, A.M.; Olawale, T.; Stensvold, C.R.; Kurtzhals, J.A.L.; König, B. Epidemiological study of the association between malaria and helminth infections in Nigeria. Am. J. Trop. Med. Hyg. 2015, 92, 578–582. [Google Scholar] [CrossRef] [Green Version]
- Simon, B.; Willis, A.; Rachel, P.; Benson, E.; Sian, E.C.; Robert, W.S.; Peter, J.H. Epidemiology of plasmodium-helminth co-infection in Africa: Population at risk, potential impact on anemia and prospects for combining control. Am. J. Trop. Med. Hyg. 2007, 77, 88–98. [Google Scholar]
- Luxemburger, C.; Kyaw, L.T.; White, N.J.; Webster, H.K.; Kyle, D.E.; Maclankirri, L.; Chongsuphajaisiddhi, T.; Nosten, F. The epidemiology of malaria in a Karen population on the western border of Thailand. Trans. R. Soc. Trop. Med. Hyg. 1996, 90, 105–111. [Google Scholar] [CrossRef] [Green Version]
- Degarege, A.; Legesse, M.; Medhin, G.; Animut, A.; Erko, B. Malaria and related outcomes in patients with intestinal helminths: A cross-sectional study. BMC Infect. Dis. 2012, 12, 291. [Google Scholar] [CrossRef] [Green Version]
- Mulu, A.; Legesse, M.; Erko, B.; Belyhun, Y.; Nugussie, D.; Shimelis, T.; Kassu, A.; Elias, D.; Moges, B. Epidemiological and clinical correlates of malaria-helminth co-infections in Southern Ethiopia. Malar. J. 2013, 12, 227. [Google Scholar] [CrossRef] [Green Version]
- Adedoje, A.; Tijani, B.D.; Akanbi, A.A., II; Ojurongbe, T.A.; Adeyeba, O.A.; Ojurongbe, O. Co-endemicity of Plasmodium falciparum and intestinal helminthes infection in school aged children in rural communities of Kwara state in Nigeria. PLoS Negl. Trop. Dis. 2015, 9, e0003940. [Google Scholar] [CrossRef]
- Spiegel, A.; Tall, A.; Raphenon, G.; Trape, J.-F.; Druilhe, P. Increased frequency of malaria attacks in subjects co-infected by intestinal worms and Plasmodium falciparum malaria. Trans. R. Soc. Trop. Med. Hyg. 2003, 97, 198–199. [Google Scholar] [CrossRef]
- Akinbo, F.O.; Okaka, C.E.; Omoregie, R. Prevalence of intestinal parasitic infections among HIV patients in Benin City, Nigeria. Libyan J. Med. 2010, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yatich, N.J.; Yi, J.; Agbenyega, T.; Turpin, A.; Rayner, J.C.; Stiles, J.K.; Ellis, W.O.; Funkhouser, E.; Ehiri, J.E.; Williams, J.H.; et al. Malaria and intestinal helminth co-infection among pregnant women in Ghana: Prevalence and risk factors. Am. J. Trop. Med. Hyg. 2009, 80, 896–901. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ndibazza, J.; Webb, E.L.; Lule, S.; Mpairwe, H.; Akello, M.; Oduru, G.; Kizza, M.; Akurut, H.; Muhangi, L.; Magnussen, P.; et al. Associations between maternal helminth and malaria infections in pregnancy and clinical malaria in the offspring: A birth cohort in entebbe, Uganda. J. Infect. Dis. 2013, 208, 2007–2016. [Google Scholar] [CrossRef]
- Wanyonyi, W.A.; Mulambalah, C.S.; Mulama, D.H.; Omukunda, E.; Siteti, D.I. Malaria and geohelminthiasis coinfections in expectant women: Effect on maternal health and birth outcomes in a malaria endemic region in Kenya. J. Parasitol. Res. 2018, 2018, 2613484. [Google Scholar] [CrossRef] [Green Version]
- Yatich, N.J.; Jolly, P.E.; Funkhouser, E.; Agbenyega, T.; Rayner, J.C.; Ehiri, J.E.; Turpin, A.; Stiles, J.K.; Ellis, W.O.; Jiang, Y.; et al. The effect of malaria and intestinal helminth coinfection on birth outcomes in Kumasi, Ghana. Am. J. Trop. Med. Hyg. 2010, 82, 28–34. [Google Scholar] [CrossRef] [Green Version]
- Ezeamama, A.E.; Friedman, J.F.; Acosta, L.P.; Bellinger, D.C.; Langdon, G.C.; Manalo, D.L.; Olveda, R.M.; Kurtis, J.D.; Mcgarvey, S.T. Helminth infection and cognitive impairment among Filipino children. Am. J. Trop. Med. Hyg. 2005, 72, 540–548. [Google Scholar] [CrossRef] [Green Version]
- Mireku, M.O.; Boivin, M.J.; Davidson, L.L.; Ouédraogo, S.; Koura, G.K.; Alao, M.J.; Massougbodji, A.; Cot, M.; Bodeau-Livinec, F. Impact of helminth infection during pregnancy on cognitive and motor functions of one-year-old children. PLoS Negl. Trop. Dis. 2015, 9, e0003463. [Google Scholar] [CrossRef] [Green Version]
- Yapi, R.B.; Hürlimann, E.; Houngbedji, C.A.; Ndri, P.B.; Silue, K.D.; Soro, G.; Kouame, F.N.; Vounatsou, P.; Fürst, T.; N’Goran, E.K.; et al. Infection and co-infection with helminths and Plasmodium among school children in Côte d’Ivoire: Results from a national cross-sectional survey. PLoS Negl. Trop. Dis. 2014, 8, e2913. [Google Scholar] [CrossRef]
- Tapajós, R.; Castro, D.; Melo, G.; Balogun, S.; James, M.; Pessoa, R.; Almeida, A.; Costa, M.; Pinto, R.; Albuquerque, B.; et al. Malaria impact on cognitive function of children in a peri-urban community in the Brazilian Amazon. Malar. J. 2019, 18, 173. [Google Scholar] [CrossRef]
- Sokhna, C.; Le Hesran, J.Y.; Mbaye, P.A.; Akiana, J.; Camara, P.; Diop, M.; Ly, A.; Druilhe, P. Increase of malaria attacks among children presenting concomitant infection by Schistosoma mansoni in Senegal. Malar. J. 2004, 3, 43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nacher, M.; Gay, F.; Singhasivanon, P.; Krudsood, S.; Treeprasertsuk, S.; Mazier, D.; Vouldoukis, I.; Looareesuwan, S. Ascaris lumbricoides infection is associated with protection from cerebral malaria. Parasite Immunol. 2000, 22, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, A.J.; Hansen, A.M.; Hee, L.; Ball, H.J.; Potter, S.M.; Walker, J.C.; Hunt, N.H. Earlycy tokine production is associated with protection from murine cerebral malaria. Infect. Immun. 2005, 73, 5645–5653. [Google Scholar] [CrossRef] [Green Version]
- Helmby, H.; Bickle, Q. Immune modulation by helminth infections. Parasite Immunol. 2006, 28, 479–481. [Google Scholar] [CrossRef] [PubMed]
- Turner, J.D.; Faulkner, H.; Kamgno, J.; Cormont, F.; Van Snick, J.; Else, K.J.; Grencis, R.K.; Behnke, J.M.; Boussinesq, M.; Bradley, J.E. Th2 cytokines are associated with reduced worm burdens in a human intestinal helminth infection. J. Infect. Dis. 2003, 188, 1768–1775. [Google Scholar] [CrossRef]
- Pierrot, C.; Adam, E.; Hot, D.; Lafitte, S.; Capron, M.; George, J.D.; Khalife, J. Contribution of T cells and neutrophils in protection of young susceptible rats from fatal experimental malaria. J. Immunol. 2007, 178, 1713–1722. [Google Scholar] [CrossRef]
- Nacher, M.; Singhasivanon, P.; Traoe, B.; Vannaphan, S.; Gay, F.; Chindanond, D.; Francois, J.; Mazier, D.; Looareesuwan, S. Helminths infection are associated with protection from cerebral malaria and increased nitrogen derivatives concentrations in Thailand. Am. J. Trop. Med. Hyg. 2002, 66, 304–309. [Google Scholar] [CrossRef]
- Yaman, F.M.; Mokela, D.; Genton, B.; Rockett, K.A.; Alpers, M.P.; Clark, I.A. Association between serum levels of reactive nitrogen intermediates and coma in children with cerebral malaria in Papua New Guinea. Trans. R. Soc. Trop. Med. Hyg. 1996, 90, 270–273. [Google Scholar] [CrossRef]
- Murray, M.J.; Murray, A.B.; Murray, M.B.; Murray, C.J. Parotid enlargement, forehead edema and suppression of malaria as nutritional consequences of ascariasis. Am. J. Clin. Nutr. 1977, 30, 2117–2121. [Google Scholar] [CrossRef] [Green Version]
- Murray, J.; Murray, A.; Murray, M.; Murray, C. The biological suppression of malaria: An ecological and nutritional interrelationship of a host and two parasites. Am. J. Clin. Nutr. 1978, 31, 1363–1366. [Google Scholar] [CrossRef] [Green Version]
- Nacher, M.; Singhasivanon, P.; Traore, B.; Dejvorakul, S.; Phumartanaprapin, W.; Looareesuwan, S.; Gay, F. Hookworm infection is associated with decreased body temperature during mild Plasmodium falciparum malaria. Am. J. Trop. Med. Hyg. 2001, 65, 131–137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hesran, J.; Akiana, J.; Ndiaye, E.I.; Dia, M.; Senghor, P.; Konate, L. Severe malarial attack is associated with high prevalence of Ascaris lumbricoides infection among children in rural Senegal. Trans. R. Soc. Trop. Med. Hyg. 2004, 98, 397–399. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, A.E.; Tukahebwa, E.M.; Kasten, J.; Clarke, S.E.; Magnussen, P.; Olsen, A.; Kabatereine, N.B.; Ndyomugyenyi, R.; Brooker, S. Epidemiology of helminths infections and their relationship to clinical malaria in southwest Uganda. Trans. R. Soc. Trop. Med. Hyg. 2005, 99, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Kelly-Hope, L.A.; Diggle, P.J.; Rowlingson, B.S.; Gyapong, J.O.; Kyelem, D.; Coleman, M.; Thomson, M.C.; Obsomer, V.; Lindsay, S.W.; Hemingway, J.; et al. Negative spatiala ssociation between lymphatic filariasis and malaria in West Africa. Trop. Med. Int. Health 2006, 11, 129–135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nacher, M.; Sighasivanon, P.; Yimsamran, S.; Manibunyong, W.; Thanyavanich, N.; Wuthisen, P.; Looareesuwan, S. Intestinal helminths infection are associated with increased incidence of Plasmodium falciparum malaria in Thailand. J. Parasitol. 2002, 88, 55–58. [Google Scholar] [CrossRef]
- Mutapi, F.; Ndhlovn, P.D.; Hagan, P.; Woolhouse, M.E. Anti Schistosome antibody responsesin children coinfected with malaria. Parasite Immunol. 2000, 22, 207–208. [Google Scholar] [CrossRef]
- Diallon, T.O.; Remoue, F.; Schacht, A.M.; Charrier, N.; Dompnier, J.P.; Pillet, S.; Garraud, O.; N’Diaye, A.A.; Capron, M.; Riveau, G. Schistosomiasis coinfection in humans influencesin flammatory markers in uncomplicated Plasmodium falciparum malaria. Parasite Immunol. 2004, 26, 365–369. [Google Scholar] [CrossRef]
- MOOSE (Meta-analyses Of Observational Studies in Epidemiology) Checklist. A Reporting Checklist for Authors, Editors, and Reviewers of Meta-analyses of ObservationalStudies. Available online: https://0-www-elsevier-com.brum.beds.ac.uk/data/promis_misc/ISSM_MOOSE_Checklist.pdf (accessed on 6 August 2020).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- The Joanna Briggs Institute Critical Appraisal Tools for Use in JBI Systematic Reviews Checklist for Prevalence Studies. Available online: http://joannabriggs.org/research/critical-appraisal-tools.html (accessed on 3 July 2020).
- Rendina-Gobioff, G. Detecting Publication Bias in Random Effects Meta-Analysis: An Empirical Comparison of Statistical Methods. Graduate Thesis, University of South Florida, Tampa, FL, USA, 2006. Available online: http://scholarcommons.usf.edu/etd/2671 (accessed on 12 October 2020).
- Abay, S.M.; Tilahun, M.; Fikrie, N.; Habtewold, A. Plasmodium falciparum and Schistosoma mansoni coinfection and the side benefit of artemether-lumefantrine in malaria patients. J. Infect. Dev. Ctries. 2013, 7, 468–474. [Google Scholar] [CrossRef] [Green Version]
- Degarege, A.; Animut, A.; Legesse, M.; Erko, B. Malaria severity status in patients with soil-transmitted helminth infections. Acta Trop. 2009, 112, 8–11. [Google Scholar] [CrossRef]
- Tuasha, N.; Hailemeskel, E.; Erko, B.; Petros, B. Comorbidity of intestinal helminthiases among malaria outpatients of Wondo Genet health centers, southern Ethiopia: Implications for integrated control. BMC Infect. Dis. 2019, 19, 659. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Degarege, A.; Animut, A.; Legesse, M.; Erko, B. Malaria and helminth co-infections in outpatients of Alaba Kulito Health Center, southern Ethiopia: A cross sectional study. BMC Res. Notes 2010, 3, 143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Getachew, M.; Tafess, K.; Zeynudin, A.; Yewhalaw, D. Prevalence Soil Transmitted Helminthiasis and malaria co-infection among pregnant women and risk factors in Gilgel Gibe dam Area, Southwest Ethiopia. BMC Res. Notes 2013, 6, 263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Degarege, A.; Animut, A.; Legesse, M.; Medhin, G.; Erko, B. Malaria and helminth co-infection and nutritional status of febrile patients in Southern Ethiopia. J. Infect. Public Health 2014, 7, 32–37. [Google Scholar] [CrossRef] [Green Version]
- Fanuael, W.; Asrat, H.; Nigus, F. Malaria and Intestinal Helminth Coinfections among Acute Febrile Outpatients in Arbaminch Health Center, Southern Ethiopia. Available online: https://www.escmid.org/escmid_publications/escmid_elibrary/material/?mid=10184 (accessed on 26 September 2020).
- Alemu, A.; Shiferaw, Y.; Ambachew, A.; Hamid, H. Malaria helminth co–infections and their contribution for aneamia in febrile patients attending Azzezo health center, Gondar, Northwest Ethiopia: A cross sectional study. Asian Pac. J. Trop. Med. 2012, 5, 803–809. [Google Scholar] [CrossRef]
- Getie, S.; Wondimeneh, Y.; Getnet, G.; Workineh, M.; Worku, L.; Kassu, A.; Moges, B. Prevalence and clinical correlates of Schistosoma mansoni co-infection among malaria infected patients, Northwest Ethiopia. BMC Res. Notes 2015, 8, 480. [Google Scholar] [CrossRef] [Green Version]
- Deribew, K.; Tekeste, Z.; Petros, B. Urinary schistosomiasis and malaria associated anemia in Ethiopia. Asian Pac. J. Trop. Biomed. 2013, 3, 307–310. [Google Scholar] [CrossRef] [Green Version]
- Masoud, N.S. Plasmodium and Soil-Transmitted Helminth Co-Infection: Epidemiological Interaction and Impact among Children Living in Endemic Areas of Bagamoya, Coastal Region of Tanzania. Doctoral Dissertation, University of Basel, Basel, Switzerland, 2018. Available online: http://edoc.unibas.ch/diss/DissB_11506 (accessed on 15 October 2020).
- Egwunyenga, A.O.; Ajayi, J.A.; Nmorsi, O.P.; Duhlinska-Popova, D.D. Plasmodium/intestinal helminth co-infections among pregnant Nigerian women. Memórias Inst. Oswaldo Cruz 2001, 96, 1055–1059. [Google Scholar] [CrossRef] [Green Version]
- Babamale, O.A.; Ugbomoiko, U.S.; Heukelbach, J. High prevalence of Plasmodium falciparum and soil-transmitted helminth co-infections in a periurban community in Kwara State, Nigeria. J. Infect. Public Health 2018, 11, 48–53. [Google Scholar] [CrossRef]
- Yatich, N.J.; Funkhouser, E.; Ehiri, J.E.; Agbenyega, T.; Stiles, J.K.; Rayner, J.C.; Turpin, A.; Ellis, W.O.; Jiang, Y.; Williams, J.H.; et al. Malaria, intestinal helminths and other risk factors for stillbirth in Ghana. Infect. Dis. Obstet. Gynecol. 2010, 2010, 350763. [Google Scholar] [CrossRef] [Green Version]
- Ezeamama, A.E.; Mc Garvey, S.T.; Acosta, L.P.; Zierler, S.; Manalo, D.L.; Wu, H.W.; Kurtis, J.D.; Mor, V.; Olveda, R.M.; Friedman, J.F. The synergistic effect of concomitant schistosomiasis, hookworm, and trichuris infections on children’s anemia burden. PLoS Negl. Trop. Dis. 2008, 2, e245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mireku, M.O. The Effects of Anemia during Pregnancy and Its Risk Factors on the Cognitive Development of One-Year-Old Children in Benin. Ph.D. Thesis, Université Pierre et Marie Curie—Paris 6, Paris, France, 2016. Available online: https://tel.archives-ouvertes.fr/tel-01401973 (accessed on 8 July 2020).
- Righetti, A.A.; Glinz, D.; Adiossan, L.G.; Koua, A.Y.; Niamké, S.; Hurrell, R.F.; Weg Müller, R.; N’Goran, E.K.; Utzinger, J. Interactions and potential implications of Plasmodium falciparum-hookworm coinfection in different age groups in south-central Côte d’Ivoire. PLoS Negl. Trop. Dis. 2012, 6, e1889. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malta, D.C.; Goulart, E.M.; Costa, M.F. Nutritional status and socioeconomic factors associated with failure in school: A prospective study of first grade students in Belo Horizonte, Brazil. Cad. Saúde Pública 1998, 14, 157–164. [Google Scholar] [CrossRef] [PubMed]
- dos Santos, L.M.; dos Santos, D.N.; Bastos, A.C.; Assis, A.M.; Prado, M.S.; Barreto, M.L. Determinants of early cognitive development: Hierarchical analysis of a longitudinal study. Cad. Saúde Pública 2008, 24, 427–437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benzecry, S.G.; Alexandre, M.A.; Vítor -Silva, S.; Salinas, J.L.; de Melo, G.C.; Marinho, H.A.; Paes, A.T.; de Siqueira, A.M.; Monteiro, W.M.; Lacerda, M.V.; et al. Micronutrient deficiencies and Plasmodium vivax malaria among children in the Brazilian Amazon. PLoS ONE 2016, 11, e0151019. [Google Scholar] [CrossRef] [Green Version]
- Kotepui, M.; Kotepui, K.U.; Milanez, G.D.; Masangkay, F.R. Global prevalence and mortality of severe Plasmodium malariae infection: A systematic review and meta-analysis. Malar. J. 2020, 19, 1–3. [Google Scholar] [CrossRef]
- Deress, T.; Girma, M. Plasmodium falciparum and Plasmodium vivax Prevalence in Ethiopia: A Systematic Review and Meta-Analysis. Malar. Res. Treat. 2019, 2019, 7065064. [Google Scholar] [CrossRef] [Green Version]
- Kotepui, M.; Kotepui, K.U.; Milanez, G.D.; Masangkay, F.R. Prevalence and risk factors related to poor outcome of patients with severe Plasmodium vi vax infection: A systematic review, meta-analysis, and analysis of case reports. BMC Infect. Dis. 2020, 20, 363. [Google Scholar] [CrossRef]
- Aron, J.L.; May, R.M. The population dynamics of malaria. In The Population Dynamics of Infectious Diseases: Theory and Applications; Springer: Boston, MA, USA, 1982; pp. 139–179. [Google Scholar]
- Kotepui, M.; Kotepui, K.U.; Milanez, G.D.; Masangkay, F.R. Plasmodium spp. mixed infection leading to severe malaria: A systematic review and meta-analysis. Sci. Rep. 2020, 10, 1–12. [Google Scholar] [CrossRef]
- Karshima, S.N. Prevalence and distribution of soil-transmitted helminth infections in Nigerian children: A systematic review and meta-analysis. Infect. Dis. Poverty 2018, 7, 69. [Google Scholar] [CrossRef] [Green Version]
- Zibaei, M.; Nosrati, M.R.; Shadnoosh, F.; Houshmand, E.; Karami, M.F.; Rafsanjani, M.K.; Majidiani, H.; Ghaffarifar, F.; Cortes, H.C.; Dalvand, S.; et al. Insights into hookworm prevalence in Asia: A systematic review and meta-analysis. Trans. R. Soc. Trop. Med. Hyg. 2020, 114, 141–154. [Google Scholar] [CrossRef]
- Hailegebriel, T.; Nibret, E.; Munshea, A. Prevalence of Soil-Transmitted Helminth Infection among School-Aged Children of Ethiopia: A Systematic Review and Meta- Analysis. Infect. Dis. Res. Treat. 2020, 13, 1178633720962812. [Google Scholar]
- Taghipour, A.; Ghodsian, S.; Jabbari, M.; Olfatifar, M.; Abdoli, A.; Ghaffarifar, F. Global prevalence ofintestinal parasitic infections and associated risk factors in pregnant women: A systematic review and meta-analysis. Trans. R. Soc. Trop. Med. Hyg. 2020, 1–14. [Google Scholar] [CrossRef]
- Afroz, S.; Debsarma, S.; Dutta, S.; Rhaman, M.M.; Mohsena, M. Prevalence of helminthic infestations among Bangladeshi rural children and its trend since mid-seventies. IMC J. Med. Sci. 2019, 13, 004. [Google Scholar] [CrossRef] [Green Version]
- Leta, G.T.; Mekete, K.; Wuletaw, Y. National mapping of soil-transmitted helminth and schistosome infections in Ethiopia. BMC Parasites Vectors 2020, 13, 437. [Google Scholar] [CrossRef]
- Silver, Z.A.; Kaliappan, S.P.; Samuel, P.; Venugopal, S.; Kang, G.; Sarkar, R.; Ajjampur, S.S. Geographical distribution of soil transmitted helminths and the effects of community type in South Asia and South East Asia–A systematic review. PLoS Negl. Trop. Dis. 2018, 12, e0006153. [Google Scholar] [CrossRef] [Green Version]




| Quality Assessment Criteria Probing Questions (Q) | Study Level Bias Score | Judgment | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Included Studies | Q-1 | Q-2 | Q-3 | Q-4 | Q-5 | Q-6 | Q-7 | Q-8 | Q-9 | Total No Yes (Y) | Percentage of Yes (Y) | |
| Degarege et al. 2009 | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 | 100.0% | Low |
| Tuasha et al. 2019 | Y | Y | Y | Y | U | Y | Y | Y | Y | 8 | 88.9% | Low |
| Getie et al. 2015 | Y | Y | Y | Y | Y | Y | U | Y | Y | 8 | 88.9% | Low |
| Alemu et al. 2012 | Y | Y | Y | Y | U | U | Y | Y | Y | 7 | 77.8% | Moderate |
| Degarege et al. 2010 | Y | Y | Y | U | Y | Y | Y | Y | Y | 9 | 100.0% | Low |
| Getachew et al. 2013 | Y | Y | Y | Y | Y | U | Y | Y | Y | 8 | 88.9% | Low |
| Deribew et al. 2013 | Y | Y | Y | Y | U | Y | U | Y | Y | 7 | 77.8% | Moderate |
| Abay et al. 2013 | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 | 100.0% | Low |
| Degarege et al. 2014 | Y | Y | Y | Y | Y | U | Y | Y | Y | 8 | 88.9% | Low |
| Workagegn et al. 2012 | Y | Y | Y | Y | Y | Y | U | Y | U | 7 | 77.8% | Moderate |
| Subtotal | ||||||||||||
| Y = Yes | 89% | |||||||||||
| U = Unclear | 11% | |||||||||||
| N = No | 0% | |||||||||||
| Overall risk of bias assessment score 89% | ||||||||||||
| S. No | Author, Year of Publication | Year Study Conducted | Region | Study Design | Sample Size | P.f | P.v | Mixed | Co-Inf Mal+ IH | Hw | Al | Tt |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Degarege et al., 2009 | November and December 2007 | SNNPR | Cross-sectional | 1802 | 283 | 1764 | 79 | 81 | 173 | 113.5 | 37.8 |
| 2 | Tuasha et al., 2019 | December 2009 to July 2010 | SNNPR | Cross-sectional | 427 | 47 | 71 | 145 | 29 | 115 | 92 | |
| 3 | Getie et al., 2015 | February to May 2013 | Amhara | Cross-sectional | 205 | 147 | 53 | 5 | 40 | |||
| 4 | Alemu et al., 2012 | February to March 2011 | Amhara | Cross-sectional | 384 | 9 | 33 | 17 | 19.6 | 71 | 238.5 | |
| 5 | Degarege et al., 2010 | November and December 2007 | SNNPR | Cross-sectional | 1802 | 502 | 255 | 681 | 267 | 149.6 | ||
| 6 | Getachew et al., 2013 | August to September, 2011 | SNNPR | Cross-sectional | 388 | 45 | 275.8 | 51.6 | 30 | 114 | 58 | 13 |
| 7 | Deribew et al., 2013 | November to December 2008 | Afar | Cross-sectional | 387 | 24 | 11 | |||||
| 8 | Abay et al., 2013 | November to December 2009 | Oromia | Cross-sectional | 152 | 28 | 149.5 | 162 | ||||
| 9 | Degarege et al., 2014 | December 2010 to February 2011 | SNNPR | Cross-sectional | 702 | 86 | 136 | 149.5 | 162 | |||
| 10 | Workagegn et al., 2012 | November 2010 to January 2011 | SNNPR | Cross-sectional | 384 | 187 | 197 | 30 | 138 | 107 | 63 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boltena, M.T.; El-Khatib, Z.; Sahlemichael Kebede, A.; Asamoah, B.O.; Tadesse Boltena, A.; Yeshambaw, M.; Biru, M. Comorbidity of Geo-Helminthes among Malaria Outpatients of the Health Facilities in Ethiopia: Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 862. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18030862
Boltena MT, El-Khatib Z, Sahlemichael Kebede A, Asamoah BO, Tadesse Boltena A, Yeshambaw M, Biru M. Comorbidity of Geo-Helminthes among Malaria Outpatients of the Health Facilities in Ethiopia: Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2021; 18(3):862. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18030862
Chicago/Turabian StyleBoltena, Minyahil Tadesse, Ziad El-Khatib, Abraham Sahlemichael Kebede, Benedict Oppong Asamoah, Andualem Tadesse Boltena, Melese Yeshambaw, and Mulatu Biru. 2021. "Comorbidity of Geo-Helminthes among Malaria Outpatients of the Health Facilities in Ethiopia: Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 18, no. 3: 862. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18030862






