Lessons from an International Initiative to Set and Share Good Practice on Human Health in Environmental Impact Assessment
Abstract
:1. Introduction
1.1. Background
1.2. Environmental Impact Assessment
- (g)
- ‘environmental impact assessment’ means a process consisting of:
- (i)
- the preparation of an environmental impact assessment report by the developer, as referred to in Article 5(1) and (2);
- (ii)
- the carrying out of consultations as referred to in Article 6 and, where relevant, Article 7;
- (iii)
- the examination by the competent authority of the information presented in the environmental impact assessment report and any supplementary information provided, where necessary, by the developer in accordance with Article 5(3), and any relevant information received through the consultations under Articles 6 and 7;
- (iv)
- the reasoned conclusion by the competent authority on the significant effects of the project on the environment, taking into account the results of the examination referred to in point (iii) and, where appropriate, its own supplementary examination; and
- (v)
- the integration of the competent authority’s reasoned conclusion into any of the decisions referred to in Article 8a.
1.3. Why Is the Amended EIA Directive Relevant to Human Health and to the Health Sector?
- 1.
- The environmental impact assessment shall identify, describe and assess in an appropriate manner, in the light of each individual case, the direct and indirect significant effects of a project on the following factors:
- (a)
- population and human health;
- (b)
- biodiversity, with particular attention to species and habitats protected under Directive 92/43/EEC and Directive 2009/147/EC;
- (c)
- land, soil, water, air and climate;
- (d)
- material assets, cultural heritage and the landscape;
- (e)
- the interaction between the factors referred to in points (a) to (d).
- 2.
- The effects referred to in paragraph 1 on the factors set out therein shall include the expected effects deriving from the vulnerability of the project to risks of major accidents and/or disasters that are relevant to the project concerned.
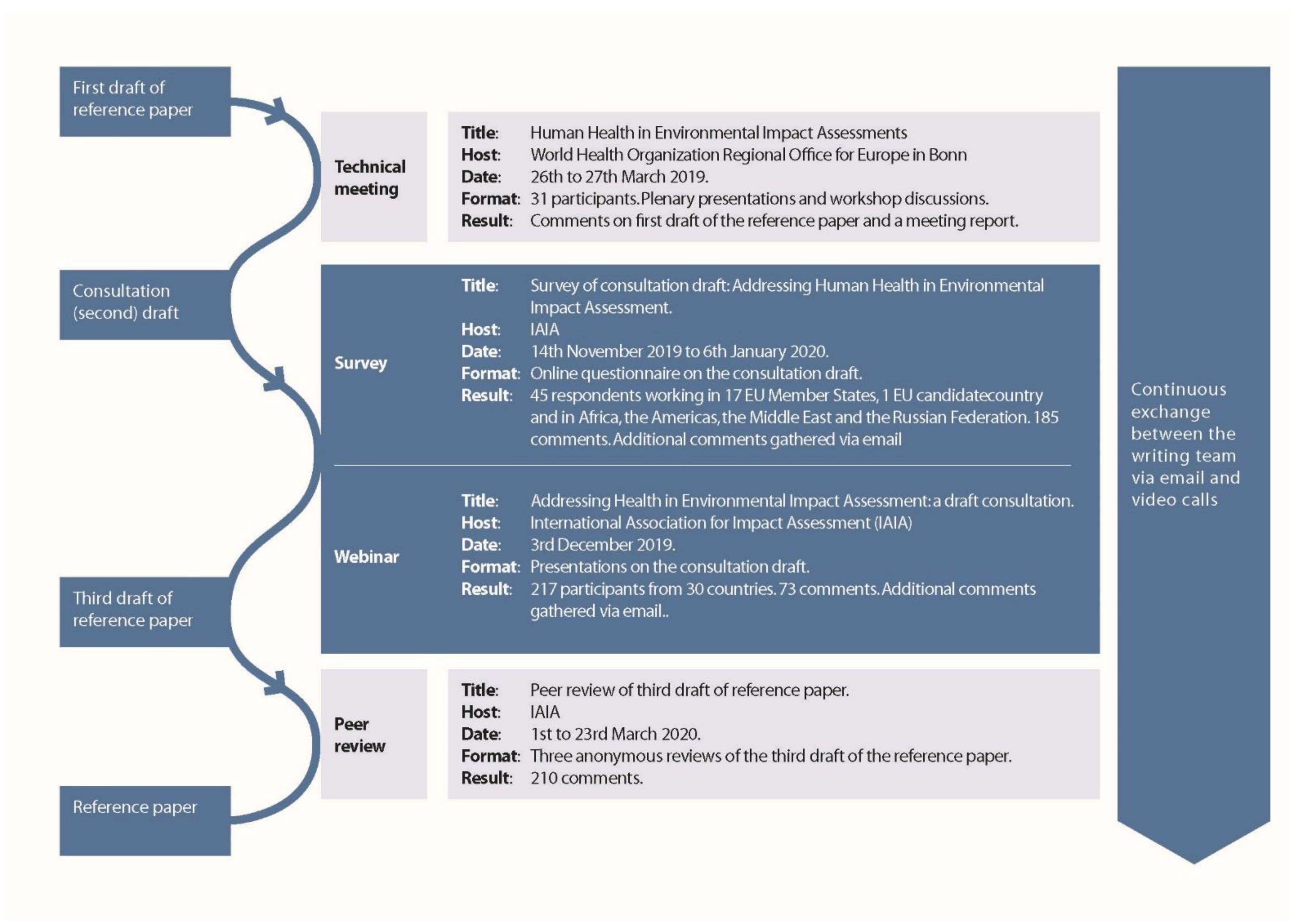
2. Materials and Methods
- How should population and human health be defined in EIA?
- How should the health sector participate in the EIA process?
- What is the relationship between EIA and HIA?
- What counts as evidence for changes in health?
- When is an effect ‘likely’ and ‘significant’?
- How should potential changes in health be reported?
- What are the risks from a business-as-usual coverage of population and human health in EIA?
- Who can conduct an assessment?
3. Results
4. Discussion
4.1. How Should Population and Human Health Be Defined in EIA?
4.2. How Should the Health Sector Participate in the EIA Process?
4.3. What Is the Relationship between EIA and HIA?
4.4. What Counts as Evidence for Changes in Health?
4.5. When Is an Effect ‘Likely’ and ‘Significant’?
4.6. How Should Potential Changes in Health Be Reported?
4.7. What Are the Risks from a Business-As-Usual Coverage of Population and Human Health in EIA?
4.8. Who Can Conduct an Assessment?
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cave, B.; Claßen, T.; Fischer-Bonde, B.; Humboldt-Dachroeden, S.; Martín-Olmedo, P.; Mekel, O.; Pyper, R.; Silva, F.; Viliani, F.; Xiao, Y. Human Health: Ensuring a High Level of Protection. A Reference Paper on Addressing Human Health in Environmental Impact Assessment as Per EU Directive 2011/92/EU Amended by 2014/52/EU; International Association for Impact Assessment and European Public Health Association: Utrecht, The Netherlands; Fargo, ND, USA, 2020; Available online: www.iaia.org/reference-and-guidance-documents.php (accessed on 13 January 2021).
- UN Environment. Assessing Environmental Impacts—A Global Review of Legislation; United Nations Environment Programme: Nairobi, Kenya; Available online: http://hdl.handle.net/20.500.11822/22691 (accessed on 8 November 2020).
- Morgan, R.K. Health and impact assessment: Are we seeing closer integration? Environ. Impact Assess. Rev. 2011, 31, 404–411. [Google Scholar] [CrossRef]
- European Parliament; Council of the European Union. Directive 2011/92/EU of the European Parliament and of the Council on the assessment of the effects of certain public and private projects on the environment. Off. J. Eur. Union 2011, L26, 1–21. [Google Scholar]
- European Parliament; Council of the European Union. Directive 2014/52/EU of the European Parliament and of the Council of 16 April 2014 Amending Directive 2011/92/EU on the Assessment of the Effects of Certain Public and Private Projects on the Environment Text with EEA Relevance. 2014. Available online: http://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32014L0052&from=EN (accessed on 12 November 2020).
- Working Party on the Accession of Montenegro. Accession of Montenegro. Offer on Specific Commitments in Services. Revision. WT/ACC/SPEC/CGR/2/Rev.3. World Trade Organization, 2008. Available online: https://docs.wto.org/dol2fe/Pages/SS/directdoc.aspx?filename=Q:/WT/ACCSPEC/CGR2R3.pdf (accessed on 20 January 2021).
- Inter-Agency Standing Committee Working Group (IASC-WG). Civil-Military Relationship in Complex Emergencies—An IASC Reference Paper. Inter-Agency Standing Committee. 2004. Available online: www.refworld.org/docid/4289ea8c4.html (accessed on 20 January 2021).
- Sustainable Ocean Business Action Platform. Blue Bonds: Reference Paper for Investments Accelerating Sustainable Ocean Business; United Nations Global Compact: New York, NY, USA, 2020; Available online: https://unglobalcompact.org/library/5741 (accessed on 20 January 2021).
- The National Environmental Policy Act of 1969, as Amended. Public Law 91-190, 42 U.S.C. 1969; pp. 4321–4347. Available online: www.energy.gov/nepa/downloads/national-environmental-policy-act-1969 (accessed on 8 November 2020).
- European Commission. Environmental Assessment. 2020. Available online: https://ec.europa.eu/environment/eia/index_en.htm (accessed on 10 November 2020).
- European Investment Bank. Environmental and Social Standards. 2018. Available online: www.eib.org/en/infocentre/publications/all/environmental-and-social-standards.htm (accessed on 4 November 2020).
- European Bank for Reconstruction and Development. Environmental and Social Policy. 2014. Available online: www.ebrd.com/cs/Satellite?c=Content&cid=1395238867768&pagename=EBRD%2FContent%2FDownloadDocument (accessed on 5 November 2020).
- Duinker, P.; Greig, L. The Impotence of Cumulative Effects Assessment in Canada: Ailments and Ideas for Redeployment. Environ. Manag. 2006, 37, 153–161. [Google Scholar] [CrossRef] [PubMed]
- EUR-Lex. National Transposition Measures Communicated by the Member States Concerning: Directive 2014/52/EU of the European Parliament and of the Council of 16 April 2014 amending Directive 2011/92/EU on the Assessment of the Effects of Certain Public and Private Projects on the Environment Text with EEA Relevance. Available online: https://eur-lex.europa.eu/legal-content/EN/NIM/?uri=celex:32014L0052 (accessed on 10 November 2020).
- Arabadjieva, K. ‘Better Regulation’ in Environmental Impact Assessment: The Amended EIA Directive. J. Environ. Law 2016, 28, 159–168. [Google Scholar] [CrossRef]
- Mayer, C. Directive 2014/52/eu: Big step forward or merely minimum consensus?—An attempt to evaluate the new eu-regulations on the assessment of the effects of certain public and private projects on the environment. Law Rev. 2016, 1, 97–108. [Google Scholar]
- Mercier, J.-R.; Mercier, C.-E.; Boutot, L.; Flament, T.; Baule, A. Transposing the revised EIA Directive in France: An opportunity for a genuine systemic approach or just more formalities? UVP 2016, 30, 133–142. [Google Scholar] [CrossRef]
- Fischer, T.; Therivel, R.; Bond, A.; Fothergill, J.; Marshall, R. The revised EIA Directive—Possible Implications for Practice in England. UVP 2016, 30, 133–142. [Google Scholar] [CrossRef]
- Hough, A. Coming down the tracks: Anticipated changes to the environmental impact assessment regime as a result of the Directive 2014/52/EU and the Aarhus Convention. Environ. Law Manag. 2016, 28. Available online: www.lawtext.com/publication/environmental-law-and-management/contents/volume-28/issue-2 (accessed on 12 November 2020).
- Mustow, S.E. The new EIA Directive (2014/52/EU) and UK water impact assessment practice. Impact Assess. Proj. Apprais. 2017, 35, 240–247. [Google Scholar] [CrossRef]
- Council of the European Communities. Council Directive 85/337/EEC on the assessment of the effects of certain public and private projects on the environment. Off. J. Eur. Union 1985, L175, 40–48. [Google Scholar]
- European Commission. Environmental Impact Assessment of Projects: Guidance on Scoping (Directive 2011/92/EU as Amended by 2014/52/EU); European Union: Luxembourg, 2017; Available online: http://ec.europa.eu/environment/eia/pdf/EIA_guidance_Scoping_final.pdf (accessed on 11 November 2020).
- European Commission. Environmental Impact Assessment of Projects: Guidance on Screening (Directive 2011/92/EU as Amended by 2014/52/EU); European Union: Luxembourg, 2017; Available online: http://ec.europa.eu/environment/eia/pdf/EIA_guidance_Screening_final.pdf (accessed on 10 November 2020).
- European Commission. Environmental Impact Assessment of Projects: Guidance on the Preparation of the Environmental Impact Assessment Report (Directive 2011/92/EU as Amended by 2014/52/EU); European Union: Luxembourg, 2017; Available online: http://ec.europa.eu/environment/eia/pdf/EIA_guidance_EIA_report_final.pdf (accessed on 12 November 2020).
- Rodríguez Rasero, F.J.; Moya Ruano, L.Á.; Vela Ríos, J.; Candau Bejarano, A. Manual Para la Evaluación de Impacto en Salud de Proyectos Sometidos a Instrumentos de Prevención y Control Ambiental en Andalucía [Guideline for HIA of Projects Subject to EIA Regulation]; Andalusian Regional Ministry of Health: Andalusia, Spain, 2015; Available online: www.juntadeandalucia.es/export/drupaljda/manual_prevencion_control_ambiental02.pdf (accessed on 10 October 2020).
- Dogliotti, E.; Achene, L.; Beccaloni, E.; Carere, M.; Comba, P.; Crebelli, R.; Lacchetti, I.; Pasetto, R.; Soggiu, M.; Testai, E. Linee Guida Per la Valutazione di Impatto Sanitario (DL.vo 104/2017); Istituto Superiore di Sanità: Roma, Italy, 2019. Available online: www.salute.gov.it/portale/documentazione/p6_2_2_1.jsp?lingua=italiano&id=2850 (accessed on 18 November 2020).
- Cave, B.; Fothergill, J.; Pyper, R.; Gibson, G.; Saunders, P. Health in Environmental Impact Assessment: A Primer for a Proportionate Approach; Ben Cave Associates Ltd., IEMA and The Faculty of Public Health: Lincoln, UK, 2017; Available online: www.iema.net/assets/newbuild/documents/IEMA%20Primer%20on%20Health%20in%20UK%20EIA%20Doc%20V11.pdf (accessed on 9 October 2020).
- Cave, B.; Fothergill, J.; Pyper, R.; Gibson, G. Health and Environmental Impact Assessment: A Briefing for Public Health Teams in England; Public Health England: London, UK, 2017. Available online: www.gov.uk/government/publications/health-and-environmental-impact-assessment-guide-for-local-teams (accessed on 10 November 2020).
- Metcalfe, O.; Higgins, C.; Lavin, T. Health Impact Assessment Guidance; Institute of Public Health in Ireland: Dublin, Ireland, 2009; Available online: www.publichealth.ie/sites/default/files/documents/files/IPH%20HIA_0.pdf (accessed on 6 November 2020).
- WHIASU. Health Impact Assessment: A Practical Guide; Wales Health Impact Assessment Support Unit: Wales, UK, 2012; Available online: www.wales.nhs.uk/sites3/Documents/522/Whiasu%20Guidance%20Report%20%28Welsh%29%20WEB.pdf; www.wales.nhs.uk/sites3/page.cfm?orgid=522&pid=63782; (accessed on 18 November 2020). [Google Scholar]
- World Health Organization Regional Office for Europe; European Centre for Health Policy. Health Impact Assessment: Main concepts and Suggested Approach. Gothenburg Consensus Paper; WHO Regional Office for Europe, ECHP: Brussels, Belgium, 1999; Available online: www.impactsante.ch/pdf/HIA_Gothenburg_consensus_paper_1999 (accessed on 17 November 2020).
- Quigley, R.; den Broeder, L.; Furu, P.; Bond, A.; Cave, B.; Bos, R. Health Impact Assessment: International Best Practice Principles. International Association for Impact Assessment. 2006. Available online: www.iaia.org/best-practice.php (accessed on 26 November 2020).
- Winkler, M.S.; Villiani, F.; Knoblauch, A.M.; Cave, B.; Divall, M.; Ramesh, G.; Harris-Roxas, B.; Furu, P. Health Impact Assessment International Best Practice Principles; International Association for Impact Assessment: Fargo, ND, USA, 2021. (in press) [Google Scholar]
- Harris-Roxas, B.; Viliani, F.; Bond, A.; Cave, B.; Divall, M.; Furu, P.; Harris, P.; Soeberg, M.; Wernham, A.; Winkler, M. Health impact assessment: The state of the art. Impact Assess. Proj. Apprais. 2012, 30, 43–52. [Google Scholar] [CrossRef]
- Jackson, R.J.; Bear, D.; Bhatia, R.; Cantor, S.B.; Cave, B.; Diez Roux, A.V.; Dora, C.; Fielding, J.E.; Zivin, J.S.G.; Levy, J.I.; et al. Improving Health in the United States: The role of Health Impact Assessment; Committee on Health Impact Assessment, Board on Environmental Studies and Toxicology, Division on Earth and Life Studies, National Research Council of the National Academies: Washington, DC, USA, 2011; Available online: www.nap.edu/catalog.php?record_id=13229 (accessed on 13 December 2020).
- World Health Organization Regional Office for Europe. Health in Impact Assessments: Opportunities Not to Be Missed. 2014. Available online: www.euro.who.int/en/health-topics/environment-and-health/health-impact-assessment/publications/2014/health-in-impact-assessments-opportunities-not-to-be-missed (accessed on 20 December 2020).
- Vohra, S.; Nowacki, J.; Martuzzi, M. Health Impact Assessments and Health in Environmental Assessments—Developing Further Implementation Strategies; Report of the Expert Meeting: Bonn, Germany, 24–25 September 2015; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2016; Available online: www.euro.who.int/en/health-topics/environment-and-health/health-impact-assessment/publications/2017/health-impact-assessments-and-health-in-environmental-assessments-developing-further-implementation-strategies-2016 (accessed on 18 December 2020).
- Nowacki, J. The Integration of Health into Environmental Assessments—With a Special Focus on Strategic Environmental Assessment; Dissertation for the degree of Doctor of Public Health, University Bielefeld: Bielefeld, Germany, 2018; Available online: www.euro.who.int/en/health-topics/environment-and-health/health-impact-assessment/publications/2018/the-integration-of-health-into-environmental-assessments-with-a-special-focus-on-strategic-environmental-assessment-2018 (accessed on 9 December 2020).
- Herber, O.R.; Bradbury-Jones, C.; Böling, S.; Combes, S.; Hirt, J.; Koop, Y.; Nyhagen, R.; Veldhuizen, J.D.; Taylor, J. What feedback do reviewers give when reviewing qualitative manuscripts? A focused mapping review and synthesis. BMC Med. Res. Methodol. 2020, 20, 122. [Google Scholar] [CrossRef] [PubMed]
- Glasson, J.; Therivel, R. Introduction to Environmental Impact Assessment, 4th ed.; Routledge: New York, NY, USA, 2014. [Google Scholar]
- Davies, K.; Sadler, B. Environmental Assessment and Human Health: Perspectives, Approaches, and Future Directions; Health Canada: Ottawa, ON, Canada, 1997; Available online: https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.513.5655&rep=rep1&type=pdf (accessed on 25 November 2020).
- Kindig, D.; Stoddart, G. What Is Population Health? Am. J. Public Health 2003, 93, 380–383. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Constitution; World Health Organization: Geneva, Switzerland, 1946; Available online: www.who.int/governance/eb/who_constitution_en.pdf (accessed on 15 October 2020).
- Milio, N. Promoting Health through Public Policy; F.A. Davis Company: Philadelphia, PA, USA, 1981. [Google Scholar]
- Mahoney, M.; Morgan, R.K. Health impact assessment in Australia and New Zealand: An exploration of methodological concerns. Promot. Educ. 2001, 8, 8–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harris, P.; McManus, P.; Sainsbury, P.; Viliani, F.; Riley, E. The institutional dynamics behind limited human health considerations in environmental assessments of coal mining projects in New South Wales, Australia. Environ. Impact Assess. Rev. 2021, 86, 106473. [Google Scholar] [CrossRef]
- Harris, P.J.; Harris, E.; Thompson, S.; Harris-Roxas, B.; Kemp, L. Human health and wellbeing in environmental impact assessment in New South Wales, Australia: Auditing health impacts within environmental assessments of major projects. Environ. Impact Assess. Rev. 2009, 29, 310–318. [Google Scholar] [CrossRef]
- Humboldt-Dachroeden, S.; Fischer-Bonde, B.; Gulis, G. Analysis of Health in Environmental Assessments—A Literature Review and Survey with a Focus on Denmark. Int. J. Environ. Res. Public Health 2019, 16, 4570. [Google Scholar] [CrossRef] [Green Version]
- Roué Le Gall, A.; Lemaire, N.; Jabot, F. Lessons learned from co-constructing a guide on healthy urban planning and on integrating health issues into environmental impact assessments conducted on French urban development projects. Impact Assess. Proj. Apprais. 2018, 36, 68–80. [Google Scholar] [CrossRef]
- Hilding-Rydevik, T.; Vohra, S.; Ruotsalainen, A.; Pettersson, A.; Pearce, N.; Breeze, C.; Hrncarova, M.; Lieskovska, Z.; Paluchova, K.; Thomas, L.; et al. Health Aspects in EIA. Österreichisches Institut für Raumplanung for the European Union. 2005. Available online: https://ec.europa.eu/environment/archives/eia/eia-studies-and-reports/pdf/D5_2-IMP3-FinalReport.pdf (accessed on 5 December 2020).
- Linzalone, N.; Assennato, G.; Ballarini, A.; Cadum, E.; Cirillo, M.; Cori, L.; De, M.F.; Musmeci, L.; Natali, M.; Rieti, S.; et al. Health Impact Assessment practice and potential for integration within Environmental Impact and Strategic Environmental Assessments in Italy. Int. J. Environ. Res. Public Health 2014, 11, 12683–12699. [Google Scholar] [CrossRef] [Green Version]
- Linzalone, N.; Ballarini, A.; Piccinelli, C.; Viliani, F.; Bianchi, F. Institutionalizing Health Impact Assessment: A consultation with experts on the barriers and facilitators to implementing HIA in Italy. J. Environ. Manag. 2018, 218, 95–102. [Google Scholar] [CrossRef]
- Iglesias-Merchan, C.; Domínguez-Ares, E. Challenges to integrate health impact assessment into environmental assessment procedures: The pending debate. Impact Assess. Proj. Apprais. 2020, 38, 299–307. [Google Scholar] [CrossRef]
- Walpita, Y.N.; Green, L. Health Impact Assessment (HIA): A Comparative Case Study of Sri Lanka and Wales: What Can a Developing Country Learn From the Welsh HIA System? Int. J. Health Serv. 2020. [Google Scholar] [CrossRef] [PubMed]
- Chanchitpricha, C.; Bond, A. Investigating the effectiveness of mandatory integration of health impact assessment within environmental impact assessment (EIA): A case study of Thailand. Impact Assess. Proj. Apprais. 2018, 36, 16–31. [Google Scholar] [CrossRef] [Green Version]
- Bhatia, R.; Wernham, A. Integrating human health into environmental impact assessment: An unrealized opportunity for environmental health and justice. Environ. Health Perspect. 2008, 116, 991–1000. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steinemann, A. Rethinking human health impact assessment. Environ. Impact Assess. Rev. 2000, 20, 627–645. [Google Scholar] [CrossRef]
- Harris-Roxas, B.; Harris, E. Differing forms, differing purposes: A typology of health impact assessment. Environ. Impact Assess. Rev. 2011, 31, 396–403. [Google Scholar] [CrossRef]
- Lindström, B.; Eriksson, M. Salutogenesis. J. Epidemiol. Community Health 2005, 59, 440. [Google Scholar] [CrossRef]
- Frohlich, K.L.; Potvin, L. Transcending the known in public health practice: The inequality paradox: The population approach and vulnerable populations. Am. J. Public Health 2008, 98, 216–221. [Google Scholar] [CrossRef]
- World Health Organization Regional Office for Europe. Environmental Health Equity Resource Package; WHO Regional Office for Europe: Copenhagen, Denmark, 2019; Available online: www.euro.who.int/en/EHinequalities2019resourcepack (accessed on 10 December 2020).
- Knight, E.K. Shifting public health practice to advance health equity: Recommendations from experts and community leaders. J. Public Health Manag. Pract. 2014, 20, 188–196. [Google Scholar] [CrossRef]
- Boyce, T.; Brown, C. Engagement and Participation for Health Equity; WHO Regional Office for Europe: Copenhagen, Denmark, 2017; Available online: www.euro.who.int/en/health-topics/health-determinants/social-determinants/publications/2017/engagement-andparticipation-for-health-equity-2017 (accessed on 12 December 2020).
- Braveman, P. What Are Health Disparities and Health Equity? We Need to Be Clear. Public Health Reports 2014, 129, 5–8. [Google Scholar] [CrossRef] [Green Version]
- Buse, C.G.; Lai, V.; Cornish, K.; Parkes, M.W. Towards environmental health equity in health impact assessment: Innovations and opportunities. Int. J. Public Health 2019, 64, 15–26. [Google Scholar] [CrossRef] [PubMed]
- European Commission. Ensuring a High Level of Health Protection, A Practical Guide; Health & Consumer Protection Directorate-General: Luxembourg, 2001; Available online: https://ec.europa.eu/health/ph_overview/Documents/key07_en.pdf (accessed on 5 October 2020).
- Consolidated version of the Treaty on the Functioning of the European Union—Part Three: Union Policies and Internal Actions—Title XIV: Public Health—Article 168 (ex Article 152 TEC). Off. J. 2008, 115, 122–124.
- World Health Organization. Health Promotion Glossary; WHO: Geneva, Switzerland, 1998; Available online: www.who.int/healthpromotion/about/HPG/en/ (accessed on 25 October 2020).
- Banken, R. Strategies for Institutionalising HIA. World Health Organization Regional Office for Europe. 2001. Available online: www.euro.who.int/data/assets/pdf_file/0010/101620/E75552.pdf (accessed on 19 November 2020).
- Simos, J.; Spanswick, L.; Palmer, N.; Christie, D. The role of health impact assessment in Phase V of the Healthy Cities European Network. Health Promot. Int. 2015, 30 (Suppl. 1), i71–i85. [Google Scholar] [CrossRef] [Green Version]
- Winkler, M.S.; Krieger, G.R.; Divall, M.J.; Cissé, G.; Wielga, M.; Singer, B.H.; Tanner, M.; Utzinger, J. Untapped potential of health impact assessment. Bull. World Health Organ. 2013, 91, 237–312. [Google Scholar] [CrossRef] [PubMed]
- Chilaka, M.A.; Ndioho, I. Health impact assessment in Nigeria: An initiative whose time has come. J. Public Health Afr. 2019, 10, 1014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bert, F.; Lo Moro, G.; Gualano, M.R.; Siliquini, R. Health impact assessment in Italy: It is time to act. Public Health 2020, 185, 223. [Google Scholar] [CrossRef]
- Jabot, F.; Tremblay, E.; Rivadeneyra, A.; Diallo, T.A.; Lapointe, G. A Comparative Analysis of Health Impact Assessment Implementation Models in the Regions of Montérégie (Québec, Canada) and Nouvelle-Aquitaine (France). Int. J. Environ. Res. Public Health 2020, 17, 6558. [Google Scholar] [CrossRef]
- Winkler, S.M.; Furu, P.; Viliani, F.; Cave, B.; Divall, M.; Ramesh, G.; Harris-Roxas, B.; Knoblauch, M.A. Current Global Health Impact Assessment Practice. Int. J. Environ. Res. Public Health 2020, 17, 2988. [Google Scholar] [CrossRef]
- Bond, A.; Retief, F.; Cave, B.; Fundingsland, M.; Duinker, P.N.; Verheem, R.; Brown, A.L. A contribution to the conceptualisation of quality in impact assessment. Environ. Impact Assess. Rev. 2018, 68, 49–58. [Google Scholar] [CrossRef] [Green Version]
- Linzalone, N.; Coi, A.; Lauriola, P.; Luise, D.; Pedone, A.; Romizi, R.; Sallese, D.; Bianchi, F.; Group, H.I.A.P.W. Participatory health impact assessment used to support decision-making in waste management planning: A replicable experience from Italy. Waste Manag. 2017, 59, 557–566. [Google Scholar] [CrossRef]
- Gamache, S.; Diallo, T.A.; Shankardass, K.; Lebel, A. The Elaboration of an Intersectoral Partnership to Perform Health Impact Assessment in Urban Planning: The Experience of Quebec City (Canada). Int. J. Environ. Res. Public Health 2020, 17, 7556. [Google Scholar] [CrossRef] [PubMed]
- Naik, Y.; Jones, S.; Christmas, H.; Roderick, P.; Cooper, D.; McGready, K.; Gent, M. Collaborative Health Impact Assessment and Policy Development to Improve Air Quality in West Yorkshire—A Case Study and Critical Reflection. Climate 2017, 5, 62. [Google Scholar] [CrossRef] [Green Version]
- Green, L.; Gray, B.J.; Ashton, K. Using health impact assessments to implement the sustainable development goals in practice: A case study in Wales. Impact Assess. Proj. Apprais. 2019, 1–11. [Google Scholar] [CrossRef]
- Viliani, F.; Edelstein, M.; Buckley, E.; Llamas, A.; Dar, O. Mining and emerging infectious diseases: Results of the Infectious Disease Risk Assessment and Management (IDRAM) initiative pilot. Extr. Ind. Soc. 2017, 4, 251–259. [Google Scholar] [CrossRef]
- Dannenberg, A.L.; Bhatia, R.; Cole, B.L.; Heaton, S.K.; Feldman, J.D.; Rutt, C.D. Use of health impact assessment in the U.S.: 27 case studies, 1999–2007. Am. J. Prev. Med. 2008, 34, 241–256. [Google Scholar] [CrossRef]
- de Leeuw, E. Engagement of Sectors Other than Health in Integrated Health Governance, Policy, and Action. Annu. Rev. Public Health 2017, 38, 329–349. [Google Scholar] [CrossRef] [Green Version]
- Cave, B. Health impact assessment: Principles and practice (book review: Birley, 2011). Impact Assess. Proj. Apprais. 2012, 30, 302–303. [Google Scholar] [CrossRef]
- Capolongo, S.; Lemaire, N.; Oppio, A.; Buffoli, M.; Roue Le Gall, A. Action planning for healthy cities: The role of multi-criteria analysis, developed in Italy and France, for assessing health performances in land-use plans and urban development projects. Epidemiol. Prev. 2016, 40, 257–264. [Google Scholar] [CrossRef]
- Kogel, C.C.; Rodriguez Pena, T.; Sanchez, I.; Tobella, M.; Lopez, J.A.; Espot, F.G.; Claramunt, F.P.; Rabal, G.; Gonzalez Viana, A. Health Impact Assessment (HIA) of a fluvial environment recovery project in a medium-sized Spanish town. Int. J. Environ. Res. Public Health 2020, 17, 1484. [Google Scholar] [CrossRef] [Green Version]
- UN Habitat; World Health Organization. Integrating Health in Urban and Territorial Planning: A Sourcebook. 2020. Available online: https://unhabitat.org/sites/default/files/2020/05/1-final_highres_20002_integrating_health_in_urban_and_territorial_planning_a_sourcebook.pdf (accessed on 15 November 2020).
- World Health Organization Regional Office for Europe. Environmental Health Inequalities in Europe. Available online: www.euro.who.int/en/EHinequalities2019 (accessed on 10 November 2020).
- Sharville, P.; Cave, B.; Jones, R.; Currie, E.; McNeice, V. Beef Health Girl and Friends: From Here to Equality; Ben Cave Associates Ltd.: Leeds, UK, 2010; Available online: www.gcph.co.uk/publications/202_health_girl_and_friends_from_here_to_equality (accessed on 12 November 2020).
- Greer, S.L.; Bekker, M.; de Leeuw, E.; Wismar, M.; Helderman, J.-K.; Ribeiro, S.; Stuckler, D. Policy, Politics and Public Health. Eur. J. Public Health 2017, 27, 40–43. [Google Scholar] [CrossRef]
- Bond, A.; Pope, J.; Fundingsland, M.; Morrison-Saunders, A.; Retief, F.; Hauptfleisch, M. Explaining the political nature of environmental impact assessment (EIA): A neo-Gramscian perspective. J. Clean. Prod. 2020, 244, 118694. [Google Scholar] [CrossRef]
- Cashmore, M.; Bond, A.; Cobb, D. The contribution of environmental assessment to sustainable development: Toward a richer empirical understanding. Environ. Manag. 2007, 40, 516–530. [Google Scholar] [CrossRef] [PubMed]
- Cashmore, M.; Bond, A.; Cobb, D. The role and functioning of environmental assessment: Theoretical reflections upon an empirical investigation of causation. J. Environ. Manag. 2008, 88, 1233–1248. [Google Scholar] [CrossRef] [PubMed]
- Morris, G.P.; Beck, S.A.; Hanlon, P.; Robertson, R. Getting strategic about the environment and health. Public Health 2006, 120, 889–903. [Google Scholar] [CrossRef] [PubMed]
- Polsky, C.; Stagg, K.; Gakh, M.; Bozlak, C.T. The Health in All Policies (HiAP) approach and the law: Preliminary lessons from California and Chicago. J. Law Med. Ethics 2015, 43 (Suppl. 1), 52–55. [Google Scholar] [CrossRef]
- Cole, B.L. Building Health Impact Assessment (HIA) Capacity: A Strategy for Congress and Government Agencies. Partnership for Prevention. 2008. Available online: www.healthedpartners.org/ceu/hia/hia02/02_04_partnerships4prevention_strategy_for_congress_hia_2008.pdf (accessed on 12 December 2020).
- McCallum, L.C.; Ollson, C.A.; Stefanovic, I.L. An adaptable Health Impact Assessment (HIA) framework for assessing health within Environmental Assessment (EA): Canadian context, international application. Impact Assess. Proj. Apprais. 2018, 36, 5–15. [Google Scholar] [CrossRef]
- Petticrew, M.; Roberts, H. Evidence, hierarchies, and typologies: Horses for courses. J. Epidemiol. Community Health 2003, 57, 527–529. [Google Scholar] [CrossRef] [Green Version]
- Brismar, A. Attention to impact pathways in EISs of large dam projects. Environ. Impact Assess. Rev. 2004, 24, 59–87. [Google Scholar] [CrossRef]
- Lees, J.; Jaeger, J.A.G.; Gunn, J.A.E.; Noble, B.F. Analysis of uncertainty consideration in environmental assessment: An empirical study of Canadian EA practice. J. Environ. Plann. Manag. 2016, 59, 2024–2044. [Google Scholar] [CrossRef]
- Jalava, K.; Pölönen, I.; Hokkanen, P.; Kuitunen, M. The precautionary principle and management of uncertainties in EIAs—Analysis of waste incineration cases in Finland. Impact Assess. Proj. Apprais. 2013, 31, 280–290. [Google Scholar] [CrossRef] [Green Version]
- Reis, S.; Morris, G.; Fleming, L.E.; Beck, S.; Taylor, T.; White, M.; Depledge, M.H.; Steinle, S.; Sabel, C.E.; Cowie, H.; et al. Integrating health and environmental impact analysis. Public Health 2015, 129, 1383–1389. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holdgate, M.W. A Perspective of Environmental Pollution; Cambridge University Press: Cambridge, UK, 1980. [Google Scholar]
- Smeets, E.; Weterings, R. Environmental Indicators: Typology and Overview; Technical Report No 25; TNO Centre for Strategy, Technology and Policy for the European Environment Agency: Copenhagen, Denmark, 1999; Available online: www.eea.europa.eu/publications/TEC25 (accessed on 10 December 2020).
- World Health Organization Regional Office for Europe. Development of Environment and Health Indicators for European Union Countries: Report on a WHO Working Group, Berlin Germany 14–16 May 2003; WHO Regional Office for Europe: Copenhagen, Denmark, 2003; Available online: https://apps.who.int/iris/handle/10665/107509 (accessed on 15 November 2020).
- World Health Organization Regional Office for Europe. Environmental Health Indicators for Europe: A Pilot Indicator-Based Report; WHO Regional Office for Europe: Copenhagen, Denmark, 2004. [Google Scholar]
- Wild, C.P. Complementing the Genome with an “Exposome”: The Outstanding Challenge of Environmental Exposure Measurement in Molecular Epidemiology. Cancer Epidemiol. Biomark. Prev. 2005, 14, 1847–1850. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siroux, V.; Agier, L.; Slama, R. The exposome concept: A challenge and a potential driver for environmental health research. Eur. Respir. Rev. 2016, 25, 124–129. [Google Scholar] [CrossRef] [Green Version]
- Vineis, P.; Robinson, O.; Chadeau-Hyam, M.; Dehghan, A.; Mudway, I.; Dagnino, S. What is new in the exposome? Environ. Int. 2020, 143, 105887. [Google Scholar] [CrossRef] [PubMed]
- Sarigiannis, D.A.; Karakitsios, S.P. Addressing complexity of health impact assessment in industrially contaminated sites via the exposome paradigm. Epidemiol. Prev. 2018, 42, 37–48. [Google Scholar] [CrossRef]
- Solomon, G.M.; Morello-Frosch, R.; Zeise, L.; Faust, J.B. Cumulative Environmental Impacts: Science and Policy to Protect Communities. Annu. Rev. Public Health 2016, 37, 83–96. [Google Scholar] [CrossRef] [Green Version]
- Baldwin, C.; Cave, B.; Rawstorne, P. Measuring the Impact of Public Understandings of Risk from Urban and Industrial Development on Community Psychosocial Well-Being: A Mixed Methods Strategy. Int. J. Community Well-Being 2019. [Google Scholar] [CrossRef] [Green Version]
- Ehrlich, A.; Ross, W. The significance spectrum and EIA significance determinations. Impact Assess. Proj. Apprais. 2015, 33, 87–97. [Google Scholar] [CrossRef]
- Winkler, M.S.; (Swiss Tropical and Public Health Institute, P.O. Box, CH-4002 Basel, Switzerland); Knoblauch, A.M.; (Swiss Tropical and Public Health Institute, P.O. Box, CH-4002 Basel, Switzerland); Viliani, F.; (International SOS, Vesterbrogade 149, 1620 København V Copenhagen, Denmark). Personal communication: HIA Guidance Documents and Risk from Zoonoses and Emerging Infectious Diseases. 2021. [Google Scholar]
- Lawrence, D.P. Impact significance determination—Back to basics. Environ. Impact Assess. Rev. 2007, 27, 755–769. [Google Scholar] [CrossRef]
- Jones, M.; Morrison-Saunders, A. Making sense of significance in environmental impact assessment. Impact Assess. Proj. Apprais. 2016, 34, 87–93. [Google Scholar] [CrossRef]
- Marusich, L.J.; Wilkinson, P.F. The Application of Fuzzy Logic Analysis to Assessing the Significance of Environmental Impacts: Case Studies from Mexico and Canada; Canadian Environmental Assessment Agency: Ottawa, ON, Canada, 2001. [Google Scholar]
- Wood, G.; Becker, J. Evaluating and Communicating Impact Significance in EIA: A Fuzzy Set Approach to Articulating Stakeholder Perspectives; Presentation to the International Association for Impact Assessment Conference: Vancouver, BC, Canada, 2004. [Google Scholar]
- Gullett, W. Environmental Impact Assessment and the Precautionary Principle: Legislating Caution in Environmental Protection. Aust. J. Environ. Manag. 1998, 5, 146–158. [Google Scholar] [CrossRef] [Green Version]
- Boothroyd, P. Social Policy Assessment Research: The Establishment, the Underground; A State of the Art Report; International Development Research Centre: Ottawa, ON, Canada, 1998; Available online: https://idl-bnc-idrc.dspacedirect.org/bitstream/handle/10625/22101/113279.pdf?isAllowed=y&sequence=1 (accessed on 9 December 2020).
- Burdge, R.J. Why is social impact assessment the orphan of the assessment process? Impact Assess. Proj. Apprais. 2002, 20, 3–9. [Google Scholar] [CrossRef] [Green Version]
- Singh, G.G.; Lerner, J.; Mach, M.; Murray, C.C.; Ranieri, B.; St-Laurent, G.P.; Wong, J.; Guimaraes, A.; Yunda-Guarin, G.; Satterfield, T.; et al. Scientific shortcomings in environmental impact statements internationally. People Nat. 2020, 2, 369–379. [Google Scholar] [CrossRef] [Green Version]
- Sadler, B. Environmental Assessment in a Changing World: Evaluating Practice to Improve Performance: Canadian Environmental Assessment Agency; International Association for Impact Assessment: Fargo, ND, USA, 1996. [Google Scholar]
- ICMM. Good Practice Guidance on Health Impact Assessment; International Council on Mining & Metals: London, UK, 2010; Available online: www.icmm.com/en-gb/publications/health-and-safety/good-practice-guidance-on-health-impact-assessment (accessed on 9 November 2020).
- McCallum, L.C.; Ollson, C.A.; Stefanovic, I.L. Prioritizing Health: A Systematic Approach to Scoping Determinants in Health Impact Assessment. Front. Public Health 2016, 4, 170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heller, J.; Givens, M.L.; Yuen, T.K.; Gould, S.; Jandu, M.B.; Bourcier, E.; Choi, T. Advancing efforts to achieve health equity: Equity metrics for health impact assessment practice. Int. J. Environ. Res. Public Health 2014, 11, 11054–11064. [Google Scholar] [CrossRef] [PubMed]
- Pyper, R.; Cave, B. Environmental topics: ‘Human health’ (7.2). In Environmental Impact Assessment Handbook; Carroll, B., Fothergill, J., Murphy, J., Turpin, T., Eds.; ICE Bookshop: London, UK, 2019; pp. 107–162. Available online: www.icevirtuallibrary.com/doi/abs/10.1680/eiah3e.61415.107 (accessed on 4 December 2020).
- Lee, N.; Colley, R.; Bonde, J.; Simpson, J. Reviewing the Quality of Environmental Statements and Environmental Appraisals; EIA Centre, Department of Planning and Landscape, University of Manchester: Manchester, UK, 1999. [Google Scholar]
- Fredsgaard, M.W.; Cave, B.; Bond, A. A Review Package for Health Impact Assessment Reports of Development Projects; Ben Cave Associates Ltd.: Leeds, UK, 2009. Available online: http://webarchive.nationalarchives.gov.uk/20170106084526/http://www.apho.org.uk/resource/item.aspx?RID=72419 (accessed on 5 December 2020).
- WHIASU. Quality Assurance Review Framework for Health Impact Assessment (HIA); Wales Health Impact Assessment Support Unit, Public Health Wales: Wales, UK, 2017; Available online: https://whiasu.publichealthnetwork.cymru/files/8815/3545/2412/Complete_QA_Framework.pdf (accessed on 10 November 2020).
- Wilkins, H. The need for subjectivity in EIA: Discourse as a tool for sustainable development. Environ. Impact Assess. Rev. 2003, 23, 401–414. [Google Scholar] [CrossRef]
- Nieuwenhuijsen, M.J.; Khreis, H.; Verlinghieri, E.; Mueller, N.; Rojas-Rueda, D. Participatory quantitative health impact assessment of urban and transport planning in cities: A review and research needs. Environ. Int. 2017, 103, 61–72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ádám, B.; Molnár, Á.; Ádány, R.; Bianchi, F.; Bitenc, K.; Chereches, R.; Cori, L.; Fehr, R.; Kobza, J.; Kollarova, J.; et al. Assessment of health risks of policies. Environ. Impact Assess. Rev. 2014, 48, 47–52. [Google Scholar] [CrossRef] [Green Version]
- Wood, C.; Lee, N.; Jones, C.E. Environmental statements in the UK: The initial experience. Proj. Apprais. 1991, 6, 187–194. [Google Scholar] [CrossRef] [Green Version]
- European Parliament; Council of the European Union. Directive 2001/42/EC of the European Parliament and of the Council on the Assessment of the Effects of Certain Plans and Programmes on the Environment. Off. J. Eur. Commun. 2001. Available online: http://data.europa.eu/eli/dir/2001/42/oj (accessed on 2 December 2020).
- Fischer, T.B. Reviewing the quality of strategic environmental assessment reports for English spatial plan core strategies. Environ. Impact Assess. Rev. 2010, 30, 62–69. [Google Scholar] [CrossRef]
- Bond, A.; Cave, B.; Ballantyne, R. Who plans for health improvement? SEA, HIA and the separation of spatial planning and health planning. Environ. Impact Assess. Rev. 2013, 42, 67–73. [Google Scholar] [CrossRef]
- Birley, M.; Peralta, G. Health Impact Assessment: A Good Practice Sourcebook; Asian Development Bank: Manila, Philippines, 2018. [Google Scholar] [CrossRef]
- Birley, M. Health Impact Assessment: Principles and Practice; Earthscan: London, UK, 2011. [Google Scholar]
- Fothergill, J.; Marshall, R. Compendium of National IA Professional Recognition Schemes: Individual Environmental Impact Assessment (EIA) Practitioners; International Association for Impact Assessment, Fothergill Training & Consulting: Fargo, ND, USA, 2019; Available online: www.iaia.org/pdf/innovationgrant_compendium_fothergill.pdf (accessed on 12 November 2020).
- Foldspang, A.; Birt, C.A.; Otok, R. ASPHER’s European List of Core Competences for the Public Health Professional, 5th ed.; Association of Schools of Public Health in the European Region (ASPHER): Brussels, Belgium, 2018; Available online: www.aspher.org/download/199/04-06-2018_aspher_s_european_list_of_core_competences_for_the_public_health_professional.pdf (accessed on 14 November 2020).
- World Health Organization Regional Office for Europe. The 10 Essential Public Health Operations. Available online: www.euro.who.int/en/health-topics/Health-systems/public-health-services/policy/the-10-essential-public-health-operations (accessed on 8 November 2020).
- Dempsey, C.; Battel-Kirk, B.; Barry, M. The CompHP Core Competencies Framework for Health Promotion Handbook; International Union of Health Promotion and Education (IUHPE): Paris, France, 2011; Available online: www.researchgate.net/publication/236150975_The_CompHP_core_competencies_framework_for_health_promotion_handbook (accessed on 10 November 2020).
- Public Health Agency of Canada. Core Competencies for Public Health in Canada: Release 1.0; Public Health Agency of Canada: Ottawa, ON, Canada, 2007; Available online: www.canada.ca/content/dam/phac-aspc/documents/services/public-health-practice/skills-online/core-competencies-public-health-canada/cc-manual-eng090407.pdf (accessed on 6 November 2020).
- Coggon, J.; Syrett, K.; Viens, A.M. Public Health Law: Ethics, Governance, and Regulation; Routledge: Abingdon, UK; New York, NY, USA, 2017; 196p. [Google Scholar]
- Commission on the Social Determinants of Health. Closing the Gap in a Generation. Health Equity through Action on the Social Determinants of Health; World Health Organization: Geneva, Switzerland, 2008; Available online: www.who.int/publications/i/item/WHO-IER-CSDH-08.1 (accessed on 5 November 2020).
- Humboldt-Dachroeden, S.; Rubin, O.; Sylvester Frid-Nielsen, S. The state of One Health research across disciplines and sectors—A bibliometric analysis. One Health 2020, 10, 100146. [Google Scholar] [CrossRef] [PubMed]
- Whitmee, S.; Haines, A.; Beyrer, C.; Boltz, F.; Capon, A.G.; de Souza Dias, B.F.; Ezeh, A.; Frumkin, H.; Gong, P.; Head, P.; et al. Safeguarding human health in the Anthropocene epoch: Report of The Rockefeller Foundation-Lancet Commission on planetary health. Lancet 2015, 386, 1973–2028. [Google Scholar] [CrossRef]
- Ottersen, O.P.; Dasgupta, J.; Blouin, C.; Buss, P.; Chongsuvivatwong, V.; Frenk, J.; Fukuda-Parr, S.; Gawanas, B.P.; Giacaman, R.; Gyapong, J.; et al. The political origins of health inequity: Prospects for change. Lancet 2014, 383, 630–667. [Google Scholar] [CrossRef]
- Mialon, M. An overview of the commercial determinants of health. Glob. Health 2020, 16, 74. [Google Scholar] [CrossRef] [PubMed]
| Dimensions | Themes |
|---|---|
| How should population and human health be defined in EIA? | The EIA definition of environment includes human health. Use the WHO definition of health, i.e., ‘physical, social, mental health and wellbeing’ and ‘absence of disease and infirmity’. Use the wider determinants of health, i.e., environmental, social and economic. Discuss risk factors and public understanding of risk. Take a public health approach. Consider inequalities in health and equity for vulnerable groups. Be consistent in the approach to health in EIA. |
| How should the health sector participate in the EIA process? | Public health should be engaged throughout EIA. Health experts should be particularly involved at the EIA scoping stage. Be proportionate in scoping health determinants. The health authority can provide advice and identify data sources. Health authorities should review EIA Report health chapters. Resources are needed for health input to EIA. |
| What is the relationship between EIA and HIA? | EIA is governed by EU legislation whereas standalone HIA is not. Methods and skills for HIA are a resource, and can support capacity building, for health in EIA. Both HIA and EIA rely on intersectoral working and cooperation. There is potential for duplication if an HIA is conducted at the same time as an assessment of health within an EIA. |
| What counts as evidence for changes in health? | Use best available evidence and peer-reviewed scientific literature. Qualitative and quantitative approaches are both valid. Evidence informing significance includes scientific literature, health priorities, baseline health data, policy review, consultation results and regulatory standards. |
| When is an effect ‘likely’ and ‘significant’? | ‘Likelihood’ is separate from ‘significance’. Health pathway models can be used to establish likelihood. ‘Significance’ in EIA is distinct from ‘statistical significance’. Significance for health in EIA …
|
| How should potential changes in health be reported in EIA? | Presenting the assessment of human health in the EIA Report is clearer if there is a dedicated chapter for human health. Focus on the ‘likely’ and ‘significant’ health effects of a project. Examine the effects on inequalities in health. Differentiate between ‘risk factors’ and ‘determinants of health’. The process of assessment should be transparent. Consider opportunities for promoting/improving population health as well as protection. Consider cumulative effects to population health from multiple stressors. Reporting should be evidenced based and it should enable reasoned conclusions to be made. Report health ‘effects’ in terms of ‘health outcomes’. Present the analysis of multiple criteria as a narrative. Communicate the health effects to stakeholders, decision makers and the public. Promote shared understanding between developers and health authorities. Use monitoring proportionately to track significant adverse health effects. Provide clarity on how to monitor, including governance for managing effects. Acknowledge that some settings have limited resources and poor data quality. |
| What are the risks from a business-as-usual coverage of population and human health in EIA? | A body of practice may emerge where the health sector is not engaged in EIA. There may be a failure to identify the health implications of a project. Opportunities to protect and improve population health may be missed. EIA compliance issues may be raised if not all the likely significant health effects of a project are reported within the EIA Report. |
| Who can conduct an assessment? | Health in EIA requires expertise in public health and impact assessment. Make use of the, currently separate, competence frameworks for public health and for impact assessment. Technical skills include assessment of specific determinants as well as knowledge of the EIA process, legal and ethical dimensions. Soft skills include health advocacy and intersectoral consensus building. Multi-disciplinary teams provide a breadth of skills for EIAs across different sectors. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cave, B.; Pyper, R.; Fischer-Bonde, B.; Humboldt-Dachroeden, S.; Martin-Olmedo, P. Lessons from an International Initiative to Set and Share Good Practice on Human Health in Environmental Impact Assessment. Int. J. Environ. Res. Public Health 2021, 18, 1392. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18041392
Cave B, Pyper R, Fischer-Bonde B, Humboldt-Dachroeden S, Martin-Olmedo P. Lessons from an International Initiative to Set and Share Good Practice on Human Health in Environmental Impact Assessment. International Journal of Environmental Research and Public Health. 2021; 18(4):1392. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18041392
Chicago/Turabian StyleCave, Ben, Ryngan Pyper, Birgitte Fischer-Bonde, Sarah Humboldt-Dachroeden, and Piedad Martin-Olmedo. 2021. "Lessons from an International Initiative to Set and Share Good Practice on Human Health in Environmental Impact Assessment" International Journal of Environmental Research and Public Health 18, no. 4: 1392. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18041392






