Effects of the Health-Awareness-Strengthening Lifestyle Program in a Randomized Trial of Young Adults with an At-Risk Mental State
Abstract
:1. Introduction
2. Methods
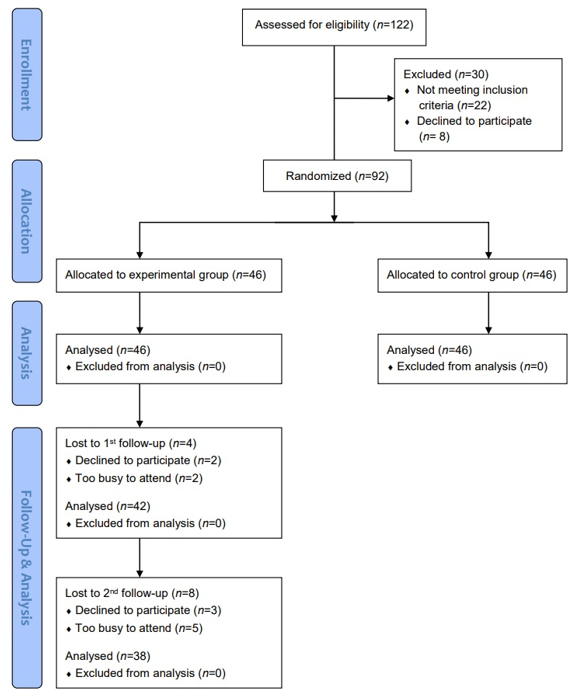
2.1. Research Design
2.2. Study Participants
2.3. Sample Characteristics
2.4. Data Collection
2.5. Health-Awareness-Strengthening Lifestyle Program
2.6. Instruments and Measurements
2.6.1. Demographic Inventory
2.6.2. Chinese Version of the Schizotypal Personality Questionnaire-Brief
2.6.3. Chinese Mandarin State and Trait Anxiety Inventory Form Y
2.6.4. Health-Promoting Lifestyle Profile–Short Form
2.6.5. World Health Organization Quality of Life-Brief Taiwan Version
2.6.6. 3-Month Physical Activity Checklist
2.6.7. Physical Assessments
2.7. Data Analysis
2.8. Identifying Information and Ethical Considerations
3. Results
3.1. Study Variables
3.2. Effects of the HASL Program in Post-test
3.3. Effects of the HASL Program in Differences between Pre- and Post-Test Analysis (T1–T0)
3.4. Prolonged Effects of the HASL Program
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Comprehensive Mental Health Action Plan 2013–2020–2030. 2019. Available online: https://www.who.int/mental_health/action_plan_2013/en/ (accessed on 8 December 2020).
- World Health Organization (WHO). ‘Zero Draft’ Global Mental Health Action Plan 2013 to 2020. 2013. Available online: http://www.who.int/mental_health/mhgap/consultation_global_mh_action_plan_2013_2020/en/ (accessed on 8 December 2020).
- Bonnett, L.J.; Varese, F.; Smith, C.T.; Flores, A.; Yung, A.R. Individualised prediction of psychosis in individuals meeting at-risk mental state (ARMS) criteria: Protocol for a systematic review of clinical prediction models. Diagn. Progn. Res. 2019, 3, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Fusar-Poli, P.; Bonoldi, I.; Yung, A.R.; Borgwardt, S.; Kempton, M.J.; Valmaggia, L.; Barale, F.; Caverzasi, E.; McGuire, P. Predicting psychosis: Meta-analysis of transition outcomes in individuals at high clinical risk. Arch. Gen. Psychiatr. 2012, 69, 220–229. [Google Scholar] [CrossRef] [Green Version]
- Yung, A.R.; Nelson, B. The ultra-high risk concept—A review. Can. J. Psychiatr. 2013, 58, 5–12. [Google Scholar] [CrossRef] [Green Version]
- Brummitt, K.; Addington, J. Treatment possibilities for individuals at clinical high risk of psychosis. Early Interv. Psychiatr. 2012, 7, 155–161. [Google Scholar] [CrossRef] [Green Version]
- Piskulic, D.; Addington, J.; Cadenhead, K.S.; Cannon, T.D.; Cornblatt, B.A.; Heinssen, R.; Perkins, D.O.; Seidman, L.J.; Tsuang, M.T.; Walker, E.F.; et al. Negative symptoms in individuals at clinical high risk of psychosis. Psychiatr. Res. 2012, 196, 220–224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, F.; Lou, M.; Lu, S.; Yen, W.; Tsai, C.; Ma, W. A preliminary study on the effectiveness of a stress management program for healthcare-related undergraduates with at-risk mental state. Perspect. Psychiatr. Care 2021, 57, 88–97. [Google Scholar] [CrossRef] [PubMed]
- McAusland, L.; Buchy, L.; Cadenhead, K.S.; Cannon, T.D.; Cornblatt, B.A.; Heinssen, R.; McGlashan, T.H.; Perkins, D.O.; Seidman, L.J.; Tsuang, M.T.; et al. Anxiety in youth at clinical high risk for psychosis. Early Interv. Psychiatr. 2017, 11, 480–487. [Google Scholar] [CrossRef] [PubMed]
- Amminger, G.P.; Nelson, B.; Markulev, C.; Yuen, H.P.; Schäfer, M.R.; Berger, M.; Mossaheb, N.; Schlögelhofer, M.; Smesny, S.; Hickie, I.B.; et al. The NEURAPRO Biomarker Analysis: Long-Chain Omega-3 Fatty Acids Improve 6-Month and 12-Month Outcomes in Youths at Ultra-High Risk for Psychosis. Biol. Psychiatr. 2019, 87, 243. [Google Scholar] [CrossRef] [PubMed]
- Carney, R.; Bradshaw, T.; Yung, A.R. Physical health promotion for young people at ultra-high risk for psychosis: An application of the COM-B model and behaviour-change wheel. Int. J. Ment. Health Nurs. 2016, 25, 536–545. [Google Scholar] [CrossRef] [Green Version]
- Carney, R.; Cotter, J.; Bradshaw, T.; Yung, A.R. Examining the physical health and lifestyle of young people at ultra-high risk for psychosis: A qualitative study involving service users, parents and clinicians. Psychiatr. Res. 2017, 255, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, S.; Schultze-Lutter, F.; Schimmelmann, B.; Maric, N.; Salokangas, R.; Riecher-Rössler, A.; Van Der Gaag, M.; Meneghelli, A.; Nordentoft, M.; Marshall, M.; et al. EPA guidance on the early intervention in clinical high risk states of psychoses. Eur. Psychiatr. 2015, 30, 388–404. [Google Scholar] [CrossRef]
- Corcoran, C.; Malaspina, D.; Hercher, L. Prodromal interventions for schizophrenia vulnerability: The risks of being “at risk”. Schizophr. Res. 2005, 73, 173–184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barr, V.J.; Robinson, S.; Marin-Link, B.; Underhill, L.; Dotts, A.; Ravensdale, D.; Salivaras, S. The expanded Chronic Care Model: An integration of concepts and strategies from population health promotion and the Chronic Care Model. Hosp. Q. 2003, 7, 73–82. [Google Scholar] [CrossRef] [Green Version]
- Huang, H.-C.; Lin, K.-C.; Wu, C.-S.; Miao, N.-F.; Chen, M.-Y. Health-promoting behaviors benefit the mental health of cirrhotic outpatients. Qual. Life Res. 2018, 27, 1521–1532. [Google Scholar] [CrossRef]
- Min, J.A.; Lee, C.U.; Lee, C. Mental health promotion and illness prevention: A challenge for psychiatrists. Psychiatr. Investig. 2013, 10, 307–316. [Google Scholar] [CrossRef] [Green Version]
- Parker, A.G.; Hetrick, S.E.; Jorm, A.F.; MacKinnon, A.J.; McGorry, P.D.; Yung, A.R.; Scanlan, F.; Stephens, J.; Baird, S.; Moller, B.; et al. The effectiveness of simple psychological and physical activity interventions for high prevalence mental health problems in young people: A factorial randomised controlled trial. J. Affect. Disord. 2016, 196, 200–209. [Google Scholar] [CrossRef] [PubMed]
- Breslin, G.; Shannon, S.; Haughey, T.; Donnelly, P.; Leavey, G. A systematic review of interventions to increase awareness of mental health and well-being in athletes, coaches and officials. Syst. Rev. 2017, 6, 1–15. [Google Scholar] [CrossRef]
- Ma, W.-F.; Wu, P.-L.; Yang, S.-J.; Cheng, K.-F.; Chiu, H.-T.; Lane, H.-Y. Sensitivity and specificity of the Chinese version of the Schizotypal Personality Questionnaire-Brief for identifying undergraduate students susceptible to psychosis. Int. J. Nurs. Stud. 2010, 47, 1535–1544. [Google Scholar] [CrossRef] [PubMed]
- Ma, W.-F.; Liu, Y.-C.; Chen, Y.-F.; Lane, H.-Y.; Lai, T.-J.; Huang, L.-C. Evaluation of psychometric properties of the Chinese Mandarin version State-Trait Anxiety Inventory Y form in Taiwanese outpatients with anxiety disorders. J. Psychiatr. Ment. Health Nurs. 2013, 20, 499–507. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Walker, S.N.; Sechrist, K.R.; Pender, N.J. The Health-Promoting Lifestyle Profile: Development and psychometric characteristics. Nurs. Res. 1987, 36, 76–81. [Google Scholar] [CrossRef]
- Raine, A.; Benishay, D. The SPQ-B: A Brief Screening Instrument for Schizotypal Personality Disorder. J. Pers. Disord. 1995, 9, 346–355. [Google Scholar] [CrossRef]
- Spielberger, C.D. Manual for the State-Trait Inventory STAI (Form Y); Mind Garden: Menlo Park, CA, USA, 1983. [Google Scholar]
- Wei, M.H.; Lu, C.M. Development of the Short-Form Chinese Health Promoting Lifestyle Profile. J. Health Educ. 2005, 24, 25–46. [Google Scholar]
- The Whoqol Group. The World Health Organization quality of life assessment (WHOQOL): Development and general psychometric properties. Soc. Sci. Med. 1998, 46, 1569–1585. [Google Scholar] [CrossRef]
- Yao, G.; Chung, C.-W.; Yu, C.-F.; Wang, J.-D. Development and verification of validity and reliability of the WHOQOL-BREF Taiwan version. J. Formos. Med. Assoc. 2002, 101, 342–351. [Google Scholar] [PubMed]
- Ma, W.-F.; Chiang, L.-C.; Yen, W.-J.; Huang, L.-C.; Tsai, T.-W. 3-Month Physical Activity Checklist: Development and validation with Taiwanese adults with mental illness. Int. J. Nurs. Stud. 2011, 48, 1517–1521. [Google Scholar] [CrossRef]
- Preti, A.; Cella, M. Randomized-controlled trials in people at ultra high risk of psychosis: A review of treatment effectiveness. Schizophr. Res. 2010, 123, 30–36. [Google Scholar] [CrossRef]
- Correll, C.U.; Hauser, M.; Auther, A.M.; Cornblatt, B.A. Research in people with psychosis risk syndrome: A review of the current evidence and future directions. J. Child Psychol. Psychiatr. 2010, 51, 390–431. [Google Scholar] [CrossRef] [PubMed]
- Wood, L.; Byrne, R.; Varese, F.; Morrison, A.P. Psychosocial interventions for internalised stigma in people with a schizophrenia-spectrum diagnosis: A systematic narrative synthesis and meta-analysis. Schizophr. Res. 2016, 176, 291–303. [Google Scholar] [CrossRef] [Green Version]
- Schwingel, A.; Gálvez, P. Divine Interventions: Faith-Based Approaches to Health Promotion Programs for Latinos. J. Relig. Health 2015, 55, 1891–1906. [Google Scholar] [CrossRef]
- Olvet, D.M.; Carrión, R.E.; Auther, A.M.; Cornblatt, B.A. Self-awareness of functional impairment in individuals at clinical high-risk for psychosis. Early Interv. Psychiatr. 2013, 9, 100–107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ma, W.-F.; Wu, P.-L.; Su, C.-H.; Yang, T.-C. The Effects of an Exercise Program on Anxiety Levels and Metabolic Functions in Patients with Anxiety Disorders. Biol. Res. Nurs. 2016, 19, 258–268. [Google Scholar] [CrossRef] [PubMed]
- Toral, M.V.; Godoy-Izquierdo, D.; De Guevara, N.M.L.; Galván, C.D.T.; Ballesteros, A.S.; García, J.F.G. Improvements in Health-Related Quality of Life, Cardio-Metabolic Health, and Fitness in Postmenopausal Women After an Exercise Plus Health Promotion Intervention: A Randomized Controlled Trial. J. Phys. Act. Health 2017, 14, 336–343. [Google Scholar] [CrossRef] [PubMed]
- Girdler, S.J.; Confino, J.E.; Woesner, M.E. Exercise as a Treatment for Schizophrenia: A Review. Psychopharmacol. Bull. 2019, 49, 56–69. [Google Scholar] [PubMed]
- Karlsson, V.; Danielsson, L. Motivators for patients with schizophrenia spectrum disorders to start and maintain exercising: A qualitative interview study. Eur. J. Physiother. 2020, 1–9. [Google Scholar] [CrossRef]
- Kohl, H.W., III; Craig, C.L.; Lambert, E.V.; Inoue, S.; Alkandari, J.R.; Leetongin, G.; Kahlmeier, S.; Lancet Physical Activity Series Working Group. The pandemic of physical inactivity: Global action for public health. Lancet 2012, 380, 294–305. [Google Scholar] [CrossRef] [Green Version]
- Popkin, B.M.; Hawkes, C. Sweetening of the global diet, particularly beverages: Patterns, trends, and policy responses. Lancet Diabetes Endocrinol. 2016, 4, 174–186. [Google Scholar] [CrossRef] [Green Version]
| Session | Dimensions | Definitions * | Prevention Strategies |
|---|---|---|---|
| 1 | Exercise | Engaging in sports and leisure activities | Counseling: Establishing role model Encouraging sharing of previous sports experience Providing mechanisms linking exercise and stress management Tools: Health education manual on benefits of sports and the obstacles to overcome, as well as exercise journal |
| Stress Management | Using relaxation techniques for stress management | Counseling: Advising time management and planning Encouraging the use of regular moderate aerobic exercise as the stress management ability Training of crisis management and response capabilities Tools: Stress management manuals | |
| Interpersonal Support | Developing social support systems and intimate relationships, encouraging sharing of ideas and spending time with friends and family, etc. | Counseling: Discussing the establishment of social network Training communication skills Strengthening mutual communication Encouraging the sharing of interpersonal difficulties and solution strategies | |
| 2 | Nutrition | Balancing daily diet and food choice | Counseling: Encouraging sharing of balanced nutritional intake Tools: Nutrition manuals, nutrition knowledge triangle, and nutrition journal |
| 3 | Self-Actualization | Maximizing individual abilities and potentials, including purpose in life, self-appreciation, positive thinking, etc. | Counseling: Encouraging sharing of personal vision, planning, and performance in academic and living, etc. Tools: Journal |
| Health Responsibility | Paying attention to health condition, seeking professional assistance if needed, and attending health lesson | Counseling: Encouraging sharing of health responsibility issues Establishing a health responsibility role model Tools: Mental health related manuals, emotional self-assessment booklet, and journal |
| Pre-Test | Post-Test | |||||||
|---|---|---|---|---|---|---|---|---|
| Control (n = 46) | Experimental (n = 46) | t | p | Control (n = 46) | Experimental (n = 46) | t | p | |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||||
| Health Promotion Lifestyles | 52.9 (9.4) | 54.9 (7.8) | −1.1 | 0.2586 | 53.8 (8.4) | 58.5 (7.8) | −2.7 | 0.0075 |
| Self-Actualization | 9.7 (2.5) | 9.6 (2.1) | 0.0 | 0.9638 | 9.6 (2.6) | 10.5 (2.1) | −1.7 | 0.0897 |
| Health Responsibility | 7.0 (2.7) | 7.1 (1.9) | −0.3 | 0.7538 | 7.3 (2.3) | 7.9 (2.1) | −1.3 | 0.2010 |
| Exercise | 7.9 (2.0) | 7.8 (2.1) | 0.3 | 0.7996 | 7.7 (2.2) | 8.4 (2.1) | −1.5 | 0.1397 |
| Nutrition | 9.0 (2.4) | 10.4 (1.9) | −3.1 | 0.0028 | 9.4 (2.3) | 10.9 (2.0) | −3.2 | 0.0017 |
| Interpersonal Support | 10.2 (2.8) | 10.2 (2.5) | 0.0 | 1.0000 | 10.3 (2.5) | 10.6 (2.1) | −0.7 | 0.5134 |
| Stress Management | 9.1 (2.0) | 9.7 (2.1) | −1.5 | 0.1347 | 9.5 (1.9) | 10.3 (2.1) | −1.8 | 0.0694 |
| State Anxiety | 47.9 (6.7) | 47.7 (8.8) | 0.1 | 0.8834 | 47.7 (9.5) | 42.5 (7.7) | 2.8 | 0.0060 |
| Trait Anxiety | 56.6 (5.6) | 55.7 (7.4) | 0.7 | 0.5079 | 56.0 (7.0) | 52.0 (7.0) | 2.7 | 0.0093 |
| Schizotypal Personality | 11.0 (4.5) | 11.4 (3.8) | −0.5 | 0.6158 | 10.3 (4.6) | 9.9 (4.0) | 0.4 | 0.6686 |
| Cognitive−Perceptual Deficits | 3.7 (1.9) | 3.5 (1.4) | 0.4 | 0.6612 | 3.5 (1.6) | 3.0 (1.6) | 1.3 | 0.1821 |
| Interpersonal Deficits | 5.0 (2.3) | 5.5 (2.1) | −1.0 | 0.3440 | 4.6 (2.4) | 4.8 (2.2) | −0.4 | 0.6795 |
| Disorganization | 2.3 (1.8) | 2.4 (1.7) | −0.4 | 0.6782 | 2.1 (1.8) | 2.0 (1.8) | 0.4 | 0.7081 |
| Quality of Life | 53.9 (7.5) | 56.0 (7.1) | −1.2 | 0.2165 | 55.0 (8.8) | 59.3 (7.3) | −2.3 | 0.0230 |
| Physical | 12.6 (2.2) | 12.8 (2.0) | −0.3 | 0.7582 | 13.2 (2.4) | 13.4 (2.3) | −0.5 | 0.6067 |
| Psychological | 10.7 (2.4) | 11.3 (2.0) | −1.3 | 0.2045 | 10.9 (2.5) | 12.1 (2.3) | −2.3 | 0.0237 |
| Social | 11.7 (2.3) | 12.4 (1.9) | −1.3 | 0.2019 | 12.3 (2.7) | 12.9 (1.8) | −1.3 | 0.2060 |
| Environmental | 13.4 (1.9) | 13.4 (1.9) | 0.0 | 1.0000 | 13.6 (2.1) | 14.2 (1.9) | −1.4 | 0.1726 |
| Physical Assessments | ||||||||
| Systolic Blood Pressure | 115.7 (15.7) | 111.7 (16.1) | 1.2 | 0.2383 | 118.6 (19.6) | 111.8 (15.9) | 1.8 | 0.0805 |
| Diastolic Blood Pressure | 74.0 (10.6) | 70.2 (9.8) | 1.8 | 0.0765 | 75.3 (10.8) | 72.9 (10.9) | 1.0 | 0.3145 |
| Body Mass Index | 22.5 (4.7) | 22.5 (4.0) | 0.0 | 0.9658 | 22.5 (4.8) | 22.6 (4.0) | −0.1 | 0.9419 |
| Waist/Hip Ratio | 0.79 (0.06) | 0.77 (0.08) | 1.0 | 0.5384 | 0.80 (0.09) | 0.78 (0.07) | 1.3 | 0.2293 |
| Physical Exercises | 68.4 (94.9) | 50.5 (95.6) | 0.9 | 0.3695 | 105.1 (121.1) | 94.0 (119.8) | 0.4 | 0.6682 |
| Control (n = 46) | Experimental (n = 46) | t | p | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||
| Health Promotion Lifestyles | 0.83 (6.82) | 3.61 (7.32) | −1.8 | 0.0699 |
| Self-Actualization | −0.02 (1.44) | 0.83 (2.11) | −2.2 | 0.0291 |
| Health Responsibility | 0.26 (1.52) | 0.76 (1.78) | −1.4 | 0.1622 |
| Exercise | −0.17 (1.92) | 0.57 (2.00) | −1.7 | 0.0841 |
| Nutrition | 0.21 (1.88) | 0.48 (1.72) | −0.7 | 0.4938 |
| Interpersonal Support | 0.17 (1.82) | 0.39 (1.77) | −0.6 | 0.5589 |
| Stress Management | 0.38 (1.86) | 0.59 (1.97) | −0.5 | 0.6165 |
| State Anxiety | −0.38 (8.70) | −5.13 (6.30) | 2.9 | 0.0048 |
| Trait Anxiety | −0.40 (4.28) | −3.72 (5.39) | 3.2 | 0.0021 |
| Schizotypal Personality | −0.69 (3.13) | −1.52 (2.87) | 1.3 | 0.1966 |
| Cognitive–Perceptual Deficits | −0.24 (1.65) | −0.48 (1.38) | 0.7 | 0.4593 |
| Interpersonal Deficits | −0.38 (1.50) | −0.61 (1.69) | 0.7 | 0.5073 |
| Disorganization | −0.07 (1.11) | −0.43 (1.56) | 1.3 | 0.2089 |
| Quality of Life | 0.56 (4.69) | 2.98 (6.06) | −1.9 | 0.0616 |
| Physical | 0.52 (1.36) | 0.65 (2.03) | −0.4 | 0.7253 |
| Psychological | 0.14 (1.49) | 0.77 (1.92) | −1.7 | 0.0934 |
| Social | 0.35 (2.32) | 0.44 (1.52) | −0.2 | 0.8397 |
| Environmental | 0.19 (1.58) | 0.82 (2.06) | −1.6 | 0.1153 |
| Physical Assessments | ||||
| Systolic Blood Pressure | 3.31 (12.52) | 0.22 (9.67) | 1.3 | 0.1997 |
| Diastolic Blood Pressure | 1.38 (8.81) | 3.02 (8.33) | −0.9 | 0.3742 |
| Body Mass Index | 0.10 (0.71) | −0.01 (1.15) | 0.5 | 0.6034 |
| Waist/Hip Ratio | 0.01 (0.06) | 0.01 (0.05) | 0.5 | 0.5968 |
| Physical Exercises | 46.03 (92.26) | 43.52 (124.11) | 0.1 | 0.9152 |
| T0 (n = 46) | T1 (n = 46) | T2 (n = 42) | T3 (n = 38) | p | |||
|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | T1 vs. T0 | T2 vs. T0 | T3 vs. T0 | |
| Health Promotion Lifestyles | 54.9 (7.8) | 58.5 (7.8) | 57.3 (8.1) | 56.6 (9.8) | 0.0007 | 0.0584 | 0.1610 |
| Self-Actualization | 9.6 (2.1) | 10.5 (2.1) | 10.1 (2.1) | 9.8 (2.2) | 0.0073 | 0.0491 | 0.4144 |
| Health Responsibility | 7.1 (1.9) | 7.9 (2.1) | 7.5 (1.8) | 7.4 (2.0) | 0.0034 | 0.2591 | 0.4290 |
| Exercise | 7.8 (2.1) | 8.4 (2.1) | 8.0 (2.2) | 8.2 (2.1) | 0.0522 | 0.6554 | 0.4158 |
| Nutrition | 10.4 (1.9) | 10.9 (2.0) | 11.0 (2.2) | 10.9 (2.1) | 0.0569 | 0.1148 | 0.2357 |
| Interpersonal Support | 10.2 (2.5) | 10.6 (2.1) | 10.5 (2.5) | 10.3 (2.3) | 0.1295 | 0.3160 | 0.6366 |
| Stress Management | 9.7 (2.1) | 10.3 (2.1) | 10.2 (1.8) | 10.1 (2.3) | 0.0413 | 0.0782 | 0.1006 |
| State Anxiety | 47.7 (8.8) | 42.5 (7.7) | 46.0 (8.4) | 45.6 (9.2) | <0.0001 | 0.2657 | 0.2201 |
| Trait Anxiety | 55.7 (7.4) | 52.0 (7.0) | 51.8 (7.6) | 52.2 (8.3) | <0.0001 | <0.0001 | <0.0001 |
| Schizotypal Personality | 11.4 (3.8) | 9.9 (4.0) | 10.1 (4.3) | 10.2 (4.5) | 0.0003 | 0.0092 | 0.0030 |
| Cognitive–Perceptual Deficits | 3.5 (1.4) | 3.0 (1.6) | 3.1 (1.9) | 3.2 (1.8) | 0.0173 | 0.1374 | 0.2905 |
| Interpersonal Deficits | 5.5 (2.1) | 4.8 (2.2) | 4.8 (2.1) | 5.1 (2.4) | 0.0137 | 0.0151 | 0.0050 |
| Disorganization | 2.4 (1.7) | 2.0 (1.8) | 2.2 (1.7) | 1.9 (1.5) | 0.0558 | 0.0870 | 0.0023 |
| Quality of Life | 56.0 (7.1) | 59.3 (7.3) | 58.2 (7.4) | 58.4 (9.1) | 0.0019 | 0.0308 | 0.0115 |
| Physical | 12.8 (2.0) | 13.4 (2.3) | 13.5 (2.6) | 13.7 (2.3) | 0.0293 | 0.0258 | 0.0032 |
| Psychological | 11.3 (2.0) | 12.1 (2.3) | 11.7 (2.4) | 11.8 (2.7) | 0.0060 | 0.3133 | 0.1493 |
| Social | 12.4 (1.9) | 12.9 (1.8) | 12.9 (1.8) | 12.7 (2.5) | 0.0471 | 0.0489 | 0.2025 |
| Environmental | 13.4 (1.9) | 14.2 (1.9) | 13.8 (2.1) | 14.1 (1.7) | 0.0083 | 0.1534 | 0.0131 |
| Physical Assessments | |||||||
| Systolic BP | 111.7 (16.1) | 111.8 (15.9) | 114.1 (16.5) | 113.5 (17.7) | 0.8858 | 0.4731 | 0.2516 |
| Diastolic BP | 70.2 (9.8) | 72.9 (10.9) | 72.7 (11.2) | 73.2 (11.5) | 0.0176 | 0.1590 | 0.0536 |
| Body Mass Index | 22.5 (4.0) | 22.6 (4.0) | 22.5 (4.1) | 22.8 (4.8) | 0.9655 | 0.6323 | 0.0844 |
| Waist/Hip Ratio | 0.77 (0.08) | 0.78 (0.07) | 0.80 (0.07) | 0.78 (0.08) | 0.4068 | 0.0190 | 0.0784 |
| Physical Exercises | 50.5 (95.6) | 94.0 (119.8) | 115.3 (191.7) | 113.8 (181.1) | 0.0162 | 0.0173 | 0.0209 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsai, C.-L.; Lin, Y.-W.; Hsu, H.-C.; Lou, M.-L.; Lane, H.-Y.; Tu, C.-H.; Ma, W.-F. Effects of the Health-Awareness-Strengthening Lifestyle Program in a Randomized Trial of Young Adults with an At-Risk Mental State. Int. J. Environ. Res. Public Health 2021, 18, 1959. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18041959
Tsai C-L, Lin Y-W, Hsu H-C, Lou M-L, Lane H-Y, Tu C-H, Ma W-F. Effects of the Health-Awareness-Strengthening Lifestyle Program in a Randomized Trial of Young Adults with an At-Risk Mental State. International Journal of Environmental Research and Public Health. 2021; 18(4):1959. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18041959
Chicago/Turabian StyleTsai, Ching-Lun, Ya-Wen Lin, Hsing-Chi Hsu, Mei-Ling Lou, Hsien-Yuan Lane, Cheng-Hao Tu, and Wei-Fen Ma. 2021. "Effects of the Health-Awareness-Strengthening Lifestyle Program in a Randomized Trial of Young Adults with an At-Risk Mental State" International Journal of Environmental Research and Public Health 18, no. 4: 1959. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18041959






