Dental Workload Reduction during First SARS-CoV-2/COVID-19 Lockdown in Germany: A Cross-Sectional Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Development and Calibration of the Questionnaire
2.2. Online Survey
2.3. Data Analysis
3. Results
4. Discussion
4.1. Burdening Effects
4.2. Economic Impact
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- RKI Robert Koch Institut. COVID-19 in Germany. Available online: https://www.rki.de/EN/Home/homepage_node.html (accessed on 8 February 2021).
- Bundesgesetzblatt. Law to Protect the Population in an Epidemic Situation of National Importance. [Article in German]. Available online: https://www.bgbl.de/xaver/bgbl/start.xav#__bgbl__%2F%2F*%5B%40attr_id%3D%27bgbl120s0587.pdf%27%5D__1598610149389 (accessed on 8 February 2021).
- RKI Robert Koch Institut. COVID-19 in Germany. Available online: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/2020-06-17-en.pdf?__blob=publicationFile (accessed on 8 February 2021).
- Sinjari, B.; Rexhepi, I.; Santilli, M.D.; Addazio, G.; Chiacchiaretta, P.; Di Carlo, P.; Caputi, S. The Impact of COVID-19 Related Lockdown on Dental Practice in Central Italy-Outcomes of a Survey. Int. J. Environ. Res. Public Health 2020, 17, 5780. [Google Scholar] [CrossRef] [PubMed]
- Papi, P.; Di Murro, B.; Penna, D.; Pompa, G. Digital prosthetic workflow during COVID-19 pandemic to limit infection risk in dental practice. Oral Dis. 2020, 10, 1111. [Google Scholar]
- Cagetti, M.G.; Balian, A.; Camoni, N.; Campus, G. Influence of the COVID-19 Pandemic on Dental Emergency Admissions in an Urgent Dental Care Service in North Italy. Int. J. Environ. Res. Public Health 2021, 18, 1812. [Google Scholar] [CrossRef] [PubMed]
- American Dental Association. ADA Develops Guidance on Dental Emergency, Nonemergency Care. 2020. Available online: https://www.ada.org/en/publications/ada-news/2020-archive/march/ada-develops-guidance-on-dental-emergency-nonemergency-care (accessed on 28 February 2021).
- German Federal States’ Dental Chamber (Bundeszahnärztekammer, BZÄK). Sars-CoV-2/COVID 19. [Article in German]. Available online: https://www.bzaek.de/berufsausuebung/sars-cov-2covid-19.html (accessed on 11 January 2021).
- National Association of Statutory Health Insurance Dentists (Kassenzahnärztliche Bundesvereinigung, KZBV). SARS-CoV-2/COVID-19: Measures of the Dental Profession for the Maintenance of Care [Article in German]. Available online: https://www.kzbv.de/coronavirus-massnahmenpaket-der-zahnaerzteschaft.1379.de.html (accessed on 10 March 2021).
- Campus, G.; Diaz-Betancourt, M.; Cagetti, M.G.; Carvalho, J.C.; Carvalho, T.S.; Cortés-Martinicorena, J.F.; Deschner, J.; Douglas, G.V.A.; Giacaman, R.A.; Machiulskiene, V.; et al. Study Protocol for an Online Questionnaire Survey on Symptoms/Signs, Protective Measures, Level of Awareness and Perception Regarding COVID-19 Outbreak among Dentists. A Global Survey. Int. J. Environ. Res. Public. Health 2020, 17, 5598. [Google Scholar] [CrossRef] [PubMed]
- Cagetti, M.G.; Cairoli, J.L.; Senna, A.; Campus, G. COVID-19 Outbreak in North Italy: An Overview on Dentistry. A Questionnaire Survey. Int. J. Environ. Res. Public Health 2020, 17, 3835. [Google Scholar] [CrossRef] [PubMed]
- Wolf, T.G.; Zeyer, O.; Campus, G. COVID-19 in Switzerland and Liechtenstein: A Cross-Sectional Survey among Dentists’ Awareness, Protective Measures and Economic Effects. Int. J. Environ. Res. Public Health 2020, 17, 9051. [Google Scholar] [CrossRef] [PubMed]
- Eurostat. First Population Estimates—EU Population in 2020 at almost 448 Million—More Deaths than Births. Available online: https://ec.europa.eu/eurostat/documents/2995521/11081097/3-10072020-AP-DE.pdf/7f863daa-c1ac-758f-e82b-954726c4621f (accessed on 8 February 2021).
- Ottnad, A.; Linnartz, E. Federal Competition Instead of Distribution Disputes. Proposals for the Restructuring of the Federal States and the Reform of Fiscal Equalization. (Föderaler Wettbewerb Statt Verteilungsstreit. Vorschläge zur Neugliederung der Bundesländer und zur Reform des Finanzausgleichs; Eine Studie des IWG Bonn [Article in German]); Campus Verlag: New York, NY, USA; Frankfurt am Main, Germany, 1997. [Google Scholar]
- Federal and State Statistical Offices. Gross Domestic Product, Gross Value Added. Bruttoinlandsprodukt, Bruttowertschöpfung. (Statistische Ämter des Bundes und der Länder. [Article in German]). Available online: https://www.statistikportal.de/de/vgrdl/ergebnisse-laenderebene/bruttoinlandsprodukt-bruttowertschoepfung/bip (accessed on 8 February 2021).
- The Federal Government of Germany (Deutsche Bundesregierung). Meeting of the Federal Chancellor with the Heads of Government of the Federal States on 22.03.2020. Available online: https://www.bundesregierung.de/breg-de/themen/coronavirus/besprechung-der-bundeskanzlerin-mit-den-regierungschefinnen-und-regierungschefs-der-laender-vom-22-03-2020-1733248 (accessed on 8 February 2021).
- Cotrin, P.; Moura, W.; Gambardela-Tkacz, C.M.; Castilho Pelloso, F.; dos Santos, L.; de Barros Carvalho, M.D.; Pelloso, S.M.; Freitas, K.M.S. Healthcare Workers in Brazil during the COVID-19 Pandemic: A Cross-Sectional Online Survey. Inquiry 2020, 57, 46958020963711. [Google Scholar] [PubMed]
- Liu, Q.; Luo, D.; Haase, J.E.; Yiaohong, G.; Wang, X.Q.; Liu, S.; Xia, L.; Zhongchun, L.; Yang, J.; Yang, B.X. The experiences of health-care providers during the COVID-19 crisis in China: A qualitative study. Lancet Glob. Health 2020, 8, e790–e798. [Google Scholar] [CrossRef]
- Xiao, H.; Zhang, Y.; Kong, D.; Li, S.; Yang, N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 2020, 26, e923541–e923549. [Google Scholar]
- Shoja, E.; Aghamohammadi, V.; Bazyar, H.; Moghaddam, H.R.; Nasiri, K.; Dashti, M.; Choupani, A.; Garaee, M.; Aliasgharzadeh, S.; Asgari, A. Covid-19 effects on the workload of Iranian healthcare workers. BMC Public Health 2020, 20, 1636. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Wang, W.; Sun, Y.; Yian, W.; Liu, Z.; Wang, R.; Yi, L.; Yang, J.; Song, X.; Zhou, X.; et al. The prevalence and risk factors of psychological disturbances of frontline medical staff in china under the COVID-19 epidemic: Workload should be concerned. J. Affect. Disord. 2020, 277, 510–514. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Cao, J.; Sun, R.; Zhang, L.; Liu, B. Analysis of anxiety-related factors amongst frontline dental staff during the COVID-19 pandemic in Yichang, China. BMC Oral Health 2020, 20, 342. [Google Scholar] [CrossRef] [PubMed]
- Long, H.; Zhao, H.; Chen, A.; Yao, Z.; Cheng, B.; Lu, Q. Protecting medical staff from skin injury/disease caused by personal protective equipment during epidemic period of COVID-19: Experience from China. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 919–921. [Google Scholar] [CrossRef] [PubMed]
- Nasseh, K.; Vujicic, M. Modeling the impact of COVID-19 on U.S. Dental Spending—June 2020 Update. Health Policy Institute Research Brief. American Dental Association. June 2020. Available online: https://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIBrief_0620_1.pdf?la=en (accessed on 8 February 2021).
- Choi, S.E.; Simon, L.; Riedy, C.A.; Barrow, J.R. Modeling the Impact of COVID-19 on Dental Insurance Coverage and Utilization. J. Dent. Res. 2021, 100, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Moraes, R.R.; Correa, M.B.; Queiroz, A.B.; Daneris, A.; Lopes, J.P.; Pereira-Conci, T.; D’Avila, O.P.; Cenci, M.S.; Lima, G.S.; Demarco, F.F. COVID-19 challenges to dentistry in the new pandemic epicenter: Brazil. PLoS ONE 2020, 15, e0242251. [Google Scholar] [CrossRef] [PubMed]
- Chamorro-Petronacci, C.; Martin Carreras-Presas, C.; Sanz-Marchena, A.; Rodríguez-Fernández, A.M.; María Suárez-Quintanilla, J.; Rivas-Mundiña, B.; Suárez-Quintanilla, J.; Pérez-Sayáns, M. Assessment of the Economic and Health-Care Impact of COVID-19 (SARS-CoV-2) on Public and Private Dental Surgeries in Spain: A Pilot Study. Int. J. Environ. Res. Public Health 2020, 17, 5139. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Krois, J.; Gomez, J. Impact of SARS-CoV2 (Covid-19) on dental practices: Economic analysis. J. Dent. 2020, 99, 103387. [Google Scholar] [CrossRef] [PubMed]
- Jevon, P.; Shamsi, S. COVID-19 and medical emergencies in the dental practice. Br. Dent. J. 2020, 229, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Wolf, T.G.; Seeberger, G.K.; Callaway, A.; Briseño-Marroquín, B.; Rusca, P.; Frank, M.; Otterbach, E.J. Is liberal independent dental practice in danger? Assessing forms of dental practice in the European Regional Organization (ERO) zone of the FDI World Dental Federation. Quintessence Int. 2018, 26, 313–324. [Google Scholar]
- Banerjee, A.; Chaudhury, S. Statistics without tears: Populations and samples. Industrial. Psyc. J. 2010, 19, 60–65. [Google Scholar] [CrossRef] [PubMed]
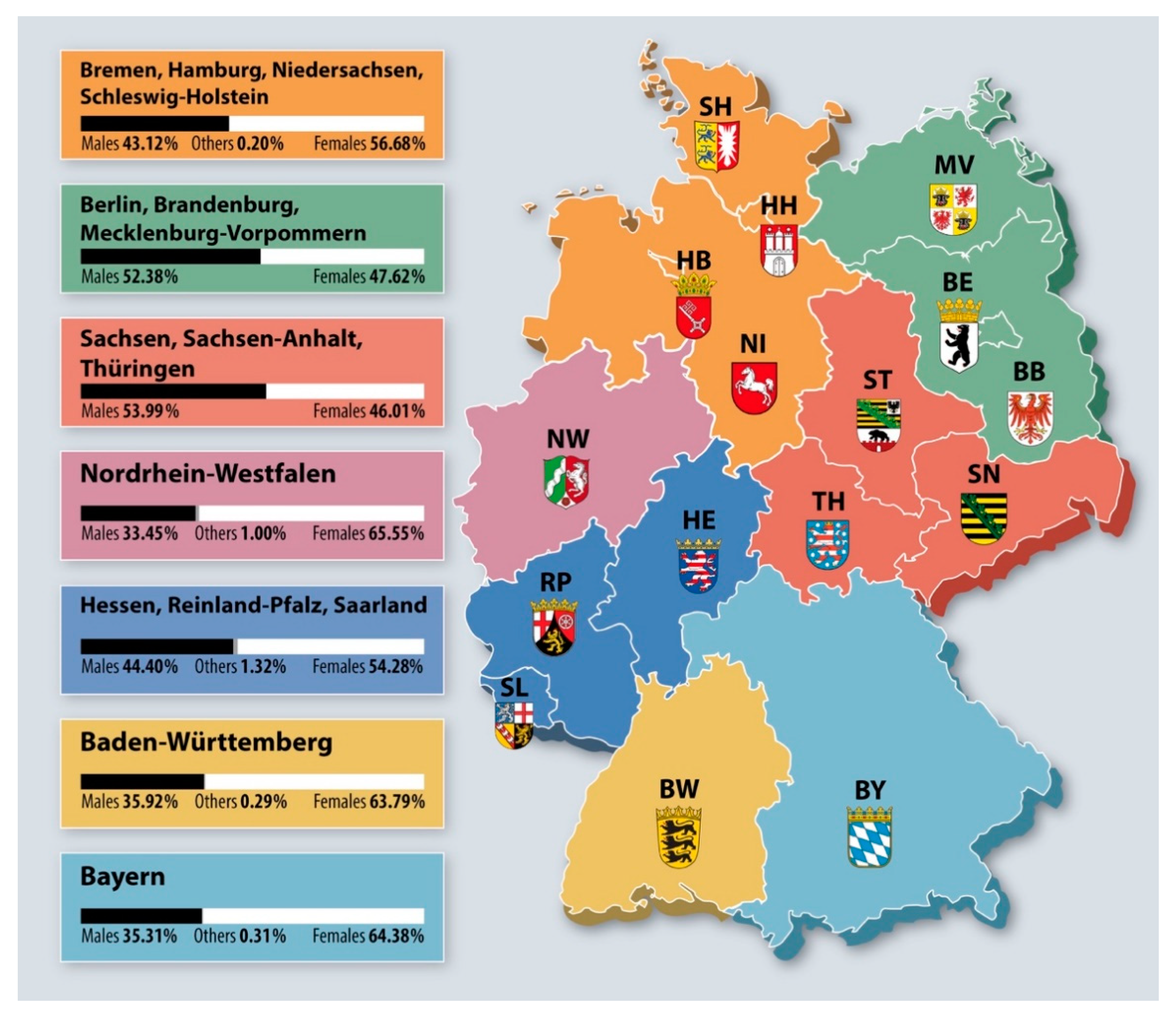

| GNP Ranking of German Macro Areas | ||||||||
| Gender | BY n (%) | BW n (%) | HB-HH-NI-SH n (%) | HE-RP-SL n (%) | NW n (%) | BE-BB-MV n (%) | SN-ST-TH n (%) | Total n (%) |
| Males | 113 (35.31) | 125 (35.92) | 213 (43.12) | 202 (44.40) | 199 (33.45) | 77 (52.38) | 149 (53.99) | 1078 (40.91) |
| Females | 206 (64.38) | 222 (63.79) | 280 (56.68) | 247 (54.29) | 390 (65.55) | 70 (47.62) | 127 (46.01) | 1542 (58.52) |
| Other | 1 (0.31) | 1 (0.29) | 1 (0.20) | 6 (1.32) | 6 (1.01) | -- | -- | 15 (0.57) |
| Total | 320 (12.14) | 348 (13.21) | 494 (20.89) | 455 (17.27) | 595 (22.58) | 147 (5.79) | 276 (10.47) | 2635 |
| Workload | GNP Ranking of German Macro Areas | |||||||
|---|---|---|---|---|---|---|---|---|
| % Reduction | BY n (%) | BW n (%) | HB-HH-NI-SH n (%) | HE-RP-SL n (%) | NW n (%) | BE-BB-MV n (%) | SN-ST-TH n (%) | Total n (%) |
| <20% | 70 (14.74) | 25 (18.12) | 33 (12.84) | 55 (12.67) | 62 (11.29) | 36 (10.98) | 30 (10.24) | 311 (12.57) |
| 21–40% | 110 (23.16) | 24 (17.39) | 48 (16.68) | 81 (18.66) | 101 (18.40) | 59 (17.99) | 52 (17.75) | 475 (19.20) |
| 41–50% | 128 (26.95) | 37 (26.81) | 62 (24.12) | 120 (27.65) | 164 (29.87) | 113 (34.45) | 95 (32.42) | 719 (29.06) |
| 61–80% | 100 (21.05) | 33 (23.91) | 70 (27.24) | 121 (27.88) | 142 (25.87) | 83 (25.30) | 73 (24.91) | 622 (25.14) |
| 81–100% | 67 (14.11) | 19 (13.77) | 44 (17.12) | 57 (13.13) | 80 (14.57) | 37 (11.28) | 43 (14.68) | 347 (14.03) |
| Total | 475 (20.00) | 138 (5.58) | 257 (10.38) | 434 (17.54) | 549 (22.20) | 328 (13.26) | 293 (11.84) | 2474 |
| Workload | Area of Practice | ||||
|---|---|---|---|---|---|
| % Reduction | Rural Town n (%) | Small Town n (%) | Medium Town n (%) | Large Town n (%) | Total n (%) |
| <20% | 101 (12.55) | 88 (13.92) | 71 (11.02) | 51 (13.04) | 311 (12.58) |
| 21–40% | 141 (17.52) | 24 (18.83) | 142 (22.05) | 72 (18.41) | 474 (19.17) |
| 41–50% | 249 (30.93) | 174 (27.53) | 180 (27.95) | 113 (28.90) | 716 (28.96) |
| 61–80% | 199 (24.72) | 164 (25.95) | 161 (25.00) | 102 (26.09) | 626 (25.33) |
| 81–100% | 115 (14.29) | 87 (13.77) | 90 (13.98) | 53 (13.55) | 345 (13.96) |
| Total | 805 (37.56) | 632 (25.57) | 644 (26.05) | 391 (15.82) | 2472 |
| Workload | Type of Practice | ||||
|---|---|---|---|---|---|
| % Reduction | Single Practice n (%) | Practice with Employed Dentist n (%) | Medical/Dental Care Centers n (%) | University/Public Health n (%) | Total n (%) |
| <20% | 190 (11.61) | 46 (8.11) | 81 (33.06) | 13 (19.12) | 330 (13.14) |
| 21–40% | 305 (18.63) | 115 (20.28) | 57 (23.27) | 14 (20.59) | 491 (19.55) |
| 41–50% | 507 (30.97) | 168 (29.63) | 28 (11.43) | 12 (19.12) | 716 (28.50) |
| 61–80% | 418 (25.53) | 157 (27.69) | 44 (17.96) | 16 (23.53) | 635 (25.28) |
| 81–100% | 217 (12.52) | 81 (14.29) | 30 (12.24) | 12 (17.65) | 345 (13.53) |
| Total | 1637 (65.17) | 567 (22.57) | 240 (9.55) | 68 (2.71) | 2517 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wolf, T.G.; Deschner, J.; Schrader, H.; Bührens, P.; Kaps-Richter, G.; Cagetti, M.G.; Campus, G. Dental Workload Reduction during First SARS-CoV-2/COVID-19 Lockdown in Germany: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 3164. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18063164
Wolf TG, Deschner J, Schrader H, Bührens P, Kaps-Richter G, Cagetti MG, Campus G. Dental Workload Reduction during First SARS-CoV-2/COVID-19 Lockdown in Germany: A Cross-Sectional Survey. International Journal of Environmental Research and Public Health. 2021; 18(6):3164. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18063164
Chicago/Turabian StyleWolf, Thomas Gerhard, James Deschner, Harald Schrader, Peter Bührens, Gudrun Kaps-Richter, Maria Grazia Cagetti, and Guglielmo Campus. 2021. "Dental Workload Reduction during First SARS-CoV-2/COVID-19 Lockdown in Germany: A Cross-Sectional Survey" International Journal of Environmental Research and Public Health 18, no. 6: 3164. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18063164






