Research Trends of Follow-Up Care after Neonatal Intensive Care Unit Graduation for Children Born Preterm: A Scoping Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Research Procedure
2.2.1. Identifying the Research Question
2.2.2. Identifying Relevant Studies
Searching Strategies
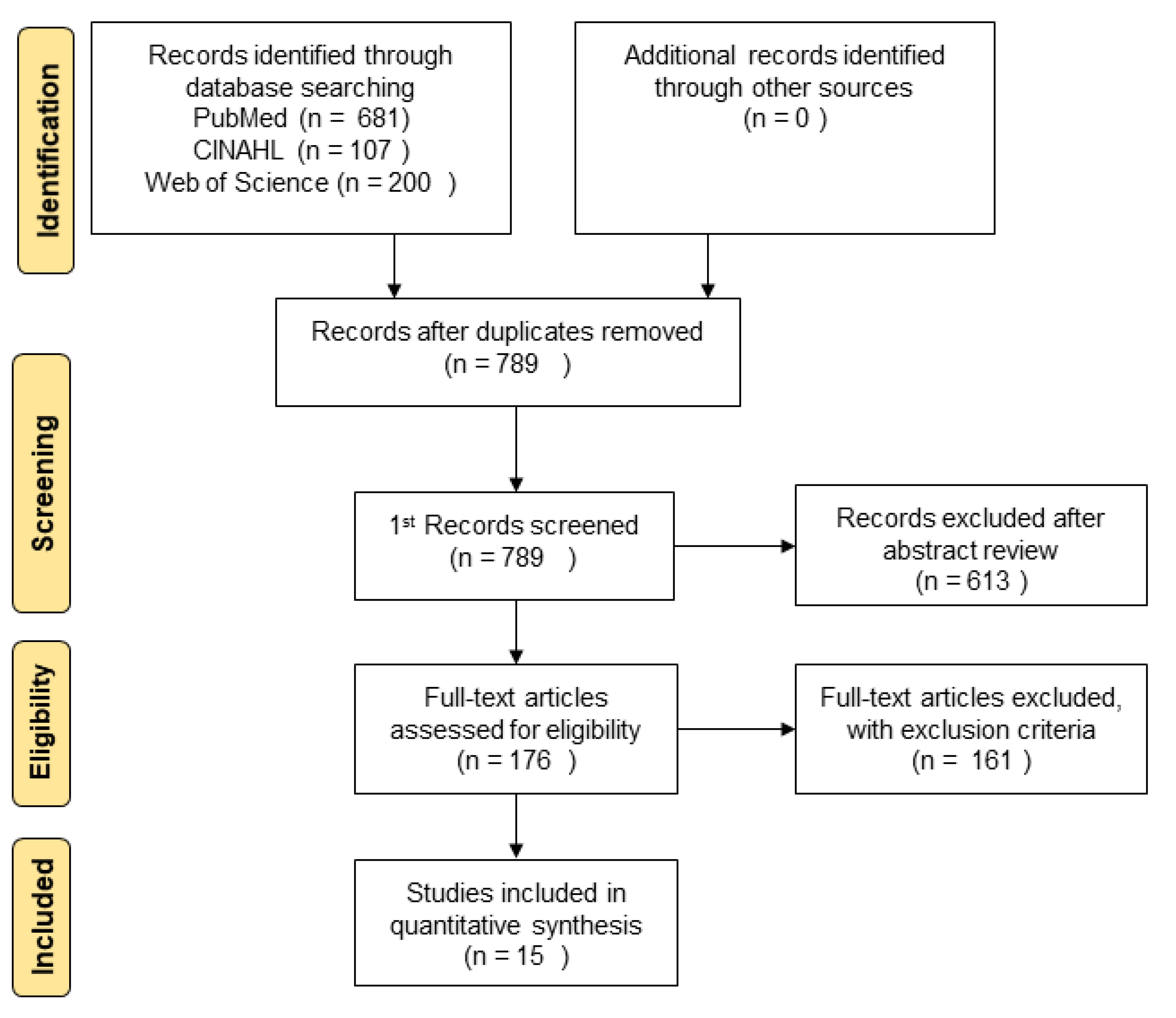
Searching Result
2.2.3. Study Selection
2.2.4. Charting the Data
2.2.5. Collating, Summarizing, and Reporting Results
2.2.6. Consultation Exercise
3. Results
3.1. General Characteristics of Reviewed Studies
3.2. Elements of Follow-Up Care after NICU Graduation
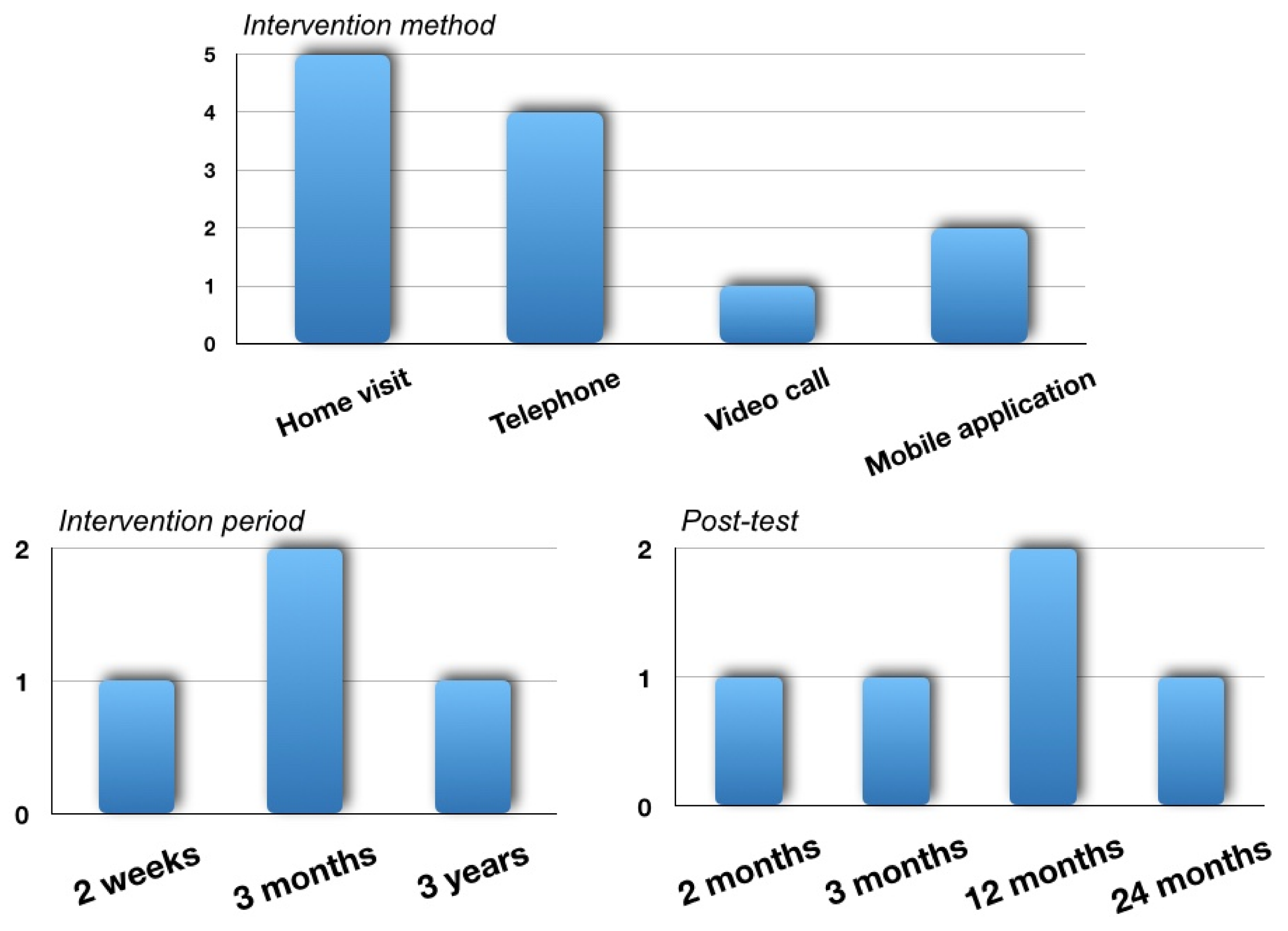
3.3. Characteristics of Follow-Up Care Intervention after NICU Graduation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Altimier, L.; Phillips, R. The neonatal integrative developmental care model: Advanced clinical application of the seven core measures for neuroprotective family-centered developmental care. Newborn Infant Nurs. Rev. 2016, 16, 230–244. [Google Scholar] [CrossRef]
- Chung, Y.S. Future of neonatology in Korea; the way forward. J. Korean Med. Assoc. 2016, 59, 506–513. [Google Scholar] [CrossRef] [Green Version]
- Mohammed, R.E.; Khamis, G.M.; Sabry, Y.Y. Effect of preterm neonates’ developmental supportive care program on nurses’ performance. Nurs. Health Sci. 2018, 7, 33–45. [Google Scholar]
- University of Utah Health. Health Outcomes for Preemies Salt Lake City: University of Utah Health. Available online: https://healthcare.utah.edu/womenshealth/pregnancy-birth/preterm-birth/when-is-it-safe-to-deliver.php (accessed on 1 February 2021).
- Synnes, A.; Hicks, M. Neurodevelopmental outcomes of preterm children at school age and beyond. Clin. Perinatol. 2018, 45, 393–408. [Google Scholar] [CrossRef] [PubMed]
- Amer, R.; Moddemann, D.; Seshia, M.; Alvaro, R.; Synnes, A.; Lee, K.S.; Shah, P.S. Neurodevelopmental outcomes of infants born at <29 weeks of gestation admitted to canadian neonatal intensive care units based on location of birth. J. Pediatr. 2018, 196, 31–37. [Google Scholar] [PubMed]
- Do, C.H.T.; Kruse, A.Y.; Wills, B.; Sabanathan, S.; Clapham, H.; Pedersen, F.K.; Pham, T.N.; Vu, P.M.; Børresen, M.L. Neurodevelopment at 2 years corrected age among Vietnamese preterm infants. Arch. Dis. Child. 2020, 105, 134–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holm, K.G.; Clemensen, J.; Brødsgaard, A.; Smith, A.C.; Maastrup, R.; Zachariassen, G. Growth and breastfeeding of preterm infants receiving neonatal tele-homecare compared to hospital-based care. J. Neonatal Perinat. Med. 2019, 12, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.; Evans, T.A.; Draper, E.S.; Field, D.J.; Manktelow, B.N.; Marlow, N.; Mattews, R.; Petrou, S.; Seaton, S.E.; Smith, L.K.; et al. Neurodevelopmental outcomes following late and moderate prematurity: A population-based cohort study. Arch. Dis. Child Fetal Neonatal Ed. 2015, 100, F301–F308. [Google Scholar] [CrossRef] [Green Version]
- Fumagalli, M.; Provenzi, L.; De Carli, P.; Dessimone, F.; Sirgiovanni, I.; Giorda, R.; Cinnante, C.; Squarcina, L.; Pozzoli, U.; Triulzi, F.; et al. From early stress to 12-month development in very preterm infants: Preliminary findings on epigenetic mechanisms and brain growth. PLoS ONE 2018, 13, e0190602. [Google Scholar] [CrossRef]
- Charkaluk, M.L.; Truffert, P.; Marchand-Martin, L.; Mur, S.; Kaminski, M.; Ancel, P.Y.; Pierrat, V.; Epipage Study Group. Very preterm children free of disability or delay at age 2: Predictors of schooling at age 8: A population-based longitudinal study. Early Hum. Dev. 2011, 87, 297–302. [Google Scholar] [CrossRef] [Green Version]
- Oh, J.A.; Kim, Y.Y.; Park, Y.K.; Yoo, S.Y.; Im, M.H.; Cho, H. Human Growth and Development; Soomoonsa: Seoul, Korea, 2020; p. 7. [Google Scholar]
- Treyvaud, K.; Doyle, L.W.; Lee, K.J.; Ure, A.; Inder, T.E.; Hunt, R.W.; Anderson, P.J. Parenting behavior at 2 years predicts school-age performance at 7 years in very preterm children. J. Child Psychol. Psychiatry 2016, 57, 814–821. [Google Scholar] [CrossRef]
- Granero-Molina, J.; Fernández Medina, I.M.; Fernández-Sola, C.; Hernández-Padilla, J.M.; Jiménez Lasserrotte, M.D.M.; López Rodríguez, M.D.M. Experiences of mothers of extremely preterm infants after hospital discharge. J. Pediatr. Nurs. 2019, 45, e2–e8. [Google Scholar] [CrossRef]
- Park, J.H.; Lee, H.; Cho, H. Analysis of the supportive care needs of the parents of preterm children in South Korea using big data text-mining: Topic modeling. Child Health Nurs. Res. 2021, 27, 34–42. [Google Scholar] [CrossRef]
- Leahy-Warren, P.; Coleman, C.; Bradley, R.; Mulcahy, H. The experiences of mothers with preterm infants within the first-year post discharge from NICU: Social support, attachment and level of depressive symptoms. BMC Pregnancy Childbirth 2020, 20, 1–10. [Google Scholar] [CrossRef]
- Berry, M.J.; Saito-Benz, M.; Gray, C.; Dyson, R.M.; Dellabarca, P.; Ebmeier, S.; Foley, D.; Elder, D.E.; Richardson, V.F. Outcomes of 23- and 24-weeks gestation infants in Wellington, New Zealand: A single centre experience. Sci. Rep. 2017, 7, 12769. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koc, E.; Demirel, N.; Bas, A.Y.; Isik, D.W.; Hirfanoglu, I.M.; Tunc, T.; Sari, F.N.; Karastekin, G.; Ozdemir, R.; Altunhan, H.; et al. Early neonatal outcomes of very-low-birth-weight infants in Turkey: A prospective multicenter study of the Turkish Neonatal Society. PLoS ONE 2019, 14, e0226679. [Google Scholar] [CrossRef] [Green Version]
- Stroustrup, A.; Bragg, J.B.; Spear, E.A.; Aguiar, A.; Zimmerman, E.; Isler, J.R.; Busgang, S.A.; Curtin, P.C.; Gennings, C.; Andra, S.S.; et al. Cohort profile: The neonatal intensive care unit hospital exposures and long-term health (NICU-HEALTH) cohort, a prospective preterm birth cohort in New York City. BMJ Open 2019, 9, e032758. [Google Scholar] [PubMed]
- Ericson, J.; Flacking, R.; Hellström-Westas, L.; Eriksson, M. Changes in the prevalence of breast feeding in preterm infants discharged from neonatal units: A register study over 10 years. BMJ Open 2016, 6, e012900. [Google Scholar] [CrossRef] [Green Version]
- Dusing, S.C.; Tripathi, T.; Marcinowski, E.C.; Thacker, L.R.; Brown, L.F.; Hendricks-Muñoz, K.D. Supporting play exploration and early developmental intervention versus usual care to enhance development outcomes during the transition from the neonatal intensive care unit to home: A pilot randomized controlled trial. BMC Pediatr. 2018, 18, 46. [Google Scholar] [CrossRef]
- Pineda, R.; Heiny, E.; Nellis, P.; Dunsirn-Baillie, S.; Wallendorf, M.; Smith, J. The baby bridge program: A sustainable program that can improve therapy service delivery for preterm infants following NICU discharge. PLoS ONE 2020, 15, e0233411. [Google Scholar] [CrossRef]
- Lee, S.Y.; Chau, J.P.C.; Choi, K.C.; Lo, S.H.S. Feasibility of a guided participation discharge program for very preterm infants in a neonatal intensive care unit: A randomized controlled trial. BMC Pediatr. 2019, 19, 402. [Google Scholar] [CrossRef]
- Yi-Ling, C.; Tzu-Ying, L.; Meei-Ling, G.; Kuan-Chia, L. The effectiveness of an intervention program for fathers of hospitalized preterm infants on paternal support and attachment 1 month after discharge. J. Perinat. Neonatal Nurs. 2019, 33, 160–169. [Google Scholar]
- Kim, N.H.; Youn, Y.A.; Cho, S.J.; Hwang, J.H.; Kim, E.K.; Kim, E.A.; Lee, S.M. The predictors for the non-compliance to follow-up among very low birth weight infants in the Korean neonatal network. PLoS ONE 2018, 13, e0204421. [Google Scholar] [CrossRef]
- Ravarian, A.; Vameghi, R.; Heidarzadeh, M.; Nariman, S.; Sagheb, S.; Nori, F.; Saeedershadi, F.; Norozi, M.; Vameghi, R. Factors influencing the attendance of preterm infants to neonatal follow up and early intervention services following discharge from neonatal intensive care unit during first year of life in Iran. Iran J. Child Neurol. 2018, 12, 67–76. [Google Scholar]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef] [Green Version]
- Seo, H.J.; Kim, S.Y. What is scoping review? Health Technol. Assess. 2018, 6, 16–21. [Google Scholar]
- Peters, M.D.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Cassia, B. Guidance for conducting systematic scoping reviews. JBI Evid. Implement. 2015, 13, 141–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seo, H.J. The scoping review approach to synthesize nursing research evidence. Korean J. Adult Nurs. 2020, 32, 433–439. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar]
- Kim, J.S.; Shin, H.S. Development of the developmental support competency scale for nurses caring for preterm infants. J. Korean Acad. Nurs. 2016, 46, 793–803. [Google Scholar] [CrossRef] [PubMed]
- Kaye, S. Historical trends in neonatal nursing. J. Pedrinat. Neonat. Nurs. 2016, 30, 273–276. [Google Scholar] [CrossRef]
- Hintz, S.R.; Gould, J.B.; Bennett, M.V.; Lu, T.; Gray, E.E.; Jocson, M.A.L.; Fuller, M.G.; Lee, H.C. Factors associated with successful first high-risk infant clinic visit for very low birth weight infants in California. J. Pediatr. 2019, 210, 91–98. [Google Scholar] [CrossRef]
- Swearingen, C.; Simpson, P.; Cabacungan, E.; Cohen, S. Social disparities negatively impact neonatal follow-up clinic attendance of premature infants discharged from the neonatal intensive care unit. J. Perinatol. 2020, 40, 790–797. [Google Scholar] [CrossRef]
- Feehan, K.; Kehinde, F.; Sachs, K.; Mossabeb, R.; Berhane, Z.; Pachter, L.M.; Broady, S.; Turchi, R.M. Development of a multidisciplinary medical home program for NICU graduates. Matern. Child Health J. 2020, 24, 11–21. [Google Scholar] [CrossRef]
- Liu, Y.; McGowan, E.; Tucker, R.; Glasgow, L.; Kluckman, M.; Vohr, B. Transition home plus program reduces medicaid spending and health care use for high-risk infants admitted to the neonatal intensive care unit for 5 or more days. J. Pediatr. 2018, 200, 91–97. [Google Scholar] [CrossRef]
- Whittingham, K.; Boyd, R.N.; Sanders, M.R.; Colditz, P. Parenting and prematurity: Understanding parent experience and preferences for support. J. Child Fam. Stud. 2014, 23, 1050–1061. [Google Scholar] [CrossRef]
- Brummelte, S.; Grunau, R.E.; Synnes, A.R.; Whitfield, M.F.; Thomas, J.P. Declining cognitive development from 8 to 18 months in preterm children predicts persisting higher parenting stress. Early Hum. Dev. 2011, 87, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Suttora, C.; Spinelli, M.; Monzani, D. From prematurity to parenting stress: The mediating role of perinatal post-traumatic stress disorder. Eur. J. Dev. Psychol. 2014, 11, 478–493. [Google Scholar] [CrossRef]
- Jung, S.Y.; Tak, Y.R. Family-centered care for hospitalized children: Concept analysis. Child Health Nur. Res. 2017, 23, 28–36. [Google Scholar] [CrossRef] [Green Version]
- Yoo, S.Y.; Cho, H. Exploring the influences of nurses’ partnership with parents, attitude to families’ importance in nursing care, and professional self-efficacy on quality of pediatric nursing care: A path model. Int. J. Environ. Res. Public Health 2020, 17, 5452. [Google Scholar] [CrossRef]
- Castel, S.; Creveuil, C.; Beunard, A.; Blaizot, X.; Proia, N.; Guillois, B. Effects of an intervention program on maternal and paternal parenting stress after preterm birth: A randomized trial. Early Hum. Dev. 2016, 103, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Koreska, M.; Petersen, M.; Andersen, B.L.; Brødsgaard, A. Supporting families on their journey towards a normal everyday life facilitating partnership in an early discharge program for families with premature infants. J. Spec. Pediatr. Nurs. 2020, 25, e12274. [Google Scholar] [CrossRef] [PubMed]
- Hendricks-Munoz, K.D.; Prendergast, C.C. Barriers to provision of developmental care in the neonatal intensive care unit: Neonatal nursing perceptions. Am. J. Perinatol. 2007, 24, 71–77. [Google Scholar] [CrossRef]
- Luu, T.M.; Xie, L.F.; Peckre, P.; Cote, S.; Karsenti, T.; Walker, C.D.; Gosselin, J. Web-based intervention to teach developmentally supportive care to parents of preterm infants: Feasibility and acceptability study. JMIR Res. Protoc. 2017, 6, e8289. [Google Scholar] [CrossRef] [Green Version]
- Majewska, J.; Zajkiewicz, K.; Wacław-Abdul, K.; Baran, J.; Szymczyk, D. Neuromotor development of children aged 6 and 7 years born before the 30th week gestation. BioMed Res. Int. 2018, 2018, 2820932. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Category | Characteristics | Total |
|---|---|---|
| n (%) | ||
| Publish year | 2016 | 2 (13.3) |
| 2017 | 2 (13.3) | |
| 2018 | 6 (40.0) | |
| 2019 | 3 (20.0) | |
| 2020 | 2 (13.3) | |
| Academic field | Medicine | 9 (60.0) |
| Nursing | 3 (20.0) | |
| Others | 2 (13.3) | |
| Unknown | 1 (6.7) | |
| Research nation | USA | 11 (73.3) |
| Sweden | 2 (13.3) | |
| Spain | 1 (6.7) | |
| India | 1 (6.7) | |
| Study design | Review | 4 (26.7) |
| Experimental study | 6 (40.0) | |
| Descriptive study | 5 (33.3) | |
| Subject | Infant born preterm | 6 (40.0) |
| Family | 2 (13.3) | |
| Parents | 2 (13.3) | |
| Toddler born preterm | 1 (6.7) | |
| Paper | 1 (6.7) | |
| Not applicable | 3 (20.0) |
| Element | Contents (Number of Reviewed Paper) |
|---|---|
| Developmental monitoring |
|
| Growth and developmental support |
|
| Feeding & nutrition |
|
| Parenting support |
|
| Parent care |
|
| Attachment |
|
| Family centered care |
|
| Continuity of care from the NICU |
|
| Multidisciplinary team |
|
| Home nursing |
|
| Support for various needs |
|
| No. | Intervention Name | Intervention Goal | Intervention Method | Experimental Period | Intervention Contents (Provider) | Post Test | Outcome (Scale) |
|---|---|---|---|---|---|---|---|
| R2 | Supporting play exploration and early development intervention (SPEEDIE) |
|
|
| (Phase 1)
|
|
|
| R3 | Proactive telephone support | Not reported |
|
|
|
|
|
| R10 | Transition Home Plus program | To provide a continuum of individualized family-centered, culturally sensitive support, provide education, and link the family to appropriate community resources |
| 90 days |
| Eight 3-month quarters after infant’s birth |
|
| R11 | mHealthPHCP | Empowering mothers of preterms and the community health workers in the care of preterms at home after discharge from the NICU | Mobile application | Not report |
| 3, 6, 9, and 12 months of CA |
|
| R12 | Baby Bridge program | To minimize the gaps in therapy services that high risk premature infants often experience after discharge from the NICU | Home visit | Not report | Not report | Not report |
|
| R13 | Telemedicine | Not report |
| Not report |
| Not applicable |
|
| R14 | Early Discharge Programme | To advance discharge and prevent the newborn from suffering from the complications of a prolonged hospitalization |
| Not report | Not report | Not applicable |
|
| R15 | Transition home program | Not report |
| 3 years |
|
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, S.R.; Cho, H. Research Trends of Follow-Up Care after Neonatal Intensive Care Unit Graduation for Children Born Preterm: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 3268. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18063268
Kang SR, Cho H. Research Trends of Follow-Up Care after Neonatal Intensive Care Unit Graduation for Children Born Preterm: A Scoping Review. International Journal of Environmental Research and Public Health. 2021; 18(6):3268. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18063268
Chicago/Turabian StyleKang, So Ra, and Haeryun Cho. 2021. "Research Trends of Follow-Up Care after Neonatal Intensive Care Unit Graduation for Children Born Preterm: A Scoping Review" International Journal of Environmental Research and Public Health 18, no. 6: 3268. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18063268






