The Association between Quitline Characteristics and Smoking Cessation by Educational Attainment, Income, Race/Ethnicity, and Sex
Abstract
:1. Introduction
2. Materials and Methods
Study Population
3. Measures
3.1. Outcome Variable
3.2. Exposure Variables
Quitline Budget per Smoker
3.3. Quitline Services Data
3.4. Counseling Sessions Offered per Quit Attempt
3.5. Hours per Week Counseling Is Available
3.6. Quitline Reach
3.7. Tobacco Control Policy Covariates
3.8. Demographic Characteristics
4. Statistical Analysis
4.1. Weights
4.2. Regression Models
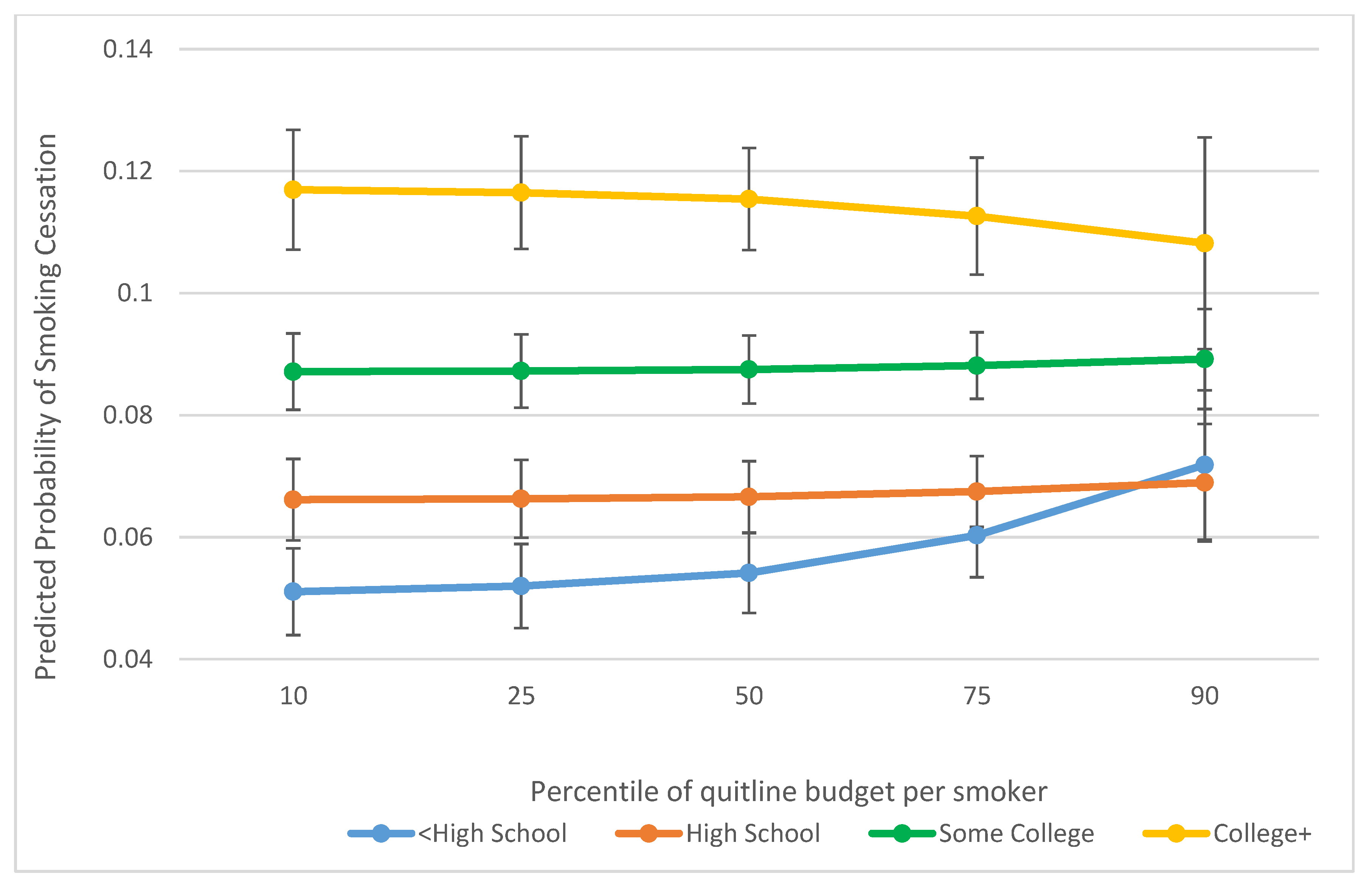
5. Results
6. Discussion
6.1. Main Effects
6.2. Effect Modification
6.3. Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Bivariate Model a | Adjusted Model b | |
|---|---|---|
| OR (95% CI) | OR (95% CI) | |
| Budget per smoker | 1.001 (0.994, 1.009) | 1.002 (0.994, 1.009) |
| Reach | 0.998 (0.912, 1.091) | 0.983 (0.897, 1.076) |
| ≥Median reach vs. <median | ||
| Counseling sessions | 0.997 (0.914, 1.087) | 0.987 (0.906, 1.075) |
| ≥5 sessions offered vs. <5 | ||
| Hours Available for Counseling 7 a.m.–7 p.m. vs. not 7 a.m.–7 p.m. | 1.000 (0.885, 1.129) | 0.999 (0.878, 1.136) |
| Budget per Smoker | Reach | Counseling Sessions | Hours of Counseling | |
|---|---|---|---|---|
| Sex | 0.029 * | 0.629 | 0.634 | 0.587 |
| Race/ethnicity | 0.595 | 0.285 | 0.079 | 0.506 |
| Education | 0.247 | 0.213 | 0.053 | 0.010 |
| Family income | 0.974 | 0.381 | 0.644 | 0.065 |
| Bivariate Model a | Adjusted Model b | |
|---|---|---|
| OR (95% CI) | OR (95% CI) | |
| Budget per smoker | 1.003 (0.998, 1.009) | 1.002 (0.996, 1.008) |
| Reach | 1.002 (0.937, 1.071) | 0.973 (0.923, 1.026) |
| ≥Median reach vs. <median | ||
| Counseling sessions | 1.008 (0.925, 1.098) | 0.992 (0.924, 1.064) |
| ≥5 sessions offered vs. <5 | ||
| Hours Available for counseling 7 a.m.–7 p.m. vs. not 7 a.m.–7 p.m. | 1.015 (0.916, 1.124) | 1.019 (0.920, 1.130) |
| Budget per Smoker | Reach | Counseling Sessions | Hours of Counseling | |
|---|---|---|---|---|
| Sex | 0.039 * | 0.537 | 0.830 | 0.307 |
| Race/ethnicity | 0.982 | 0.451 | 0.088 | 0.828 |
| Education | 0.072 | 0.072 | 0.060 | 0.081 |
| Family income | 0.914 | 0.508 | 0.424 | 0.138 |

References
- U. S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Ofice on Smoking and Health: Atlanta, GA, USA, 2014.
- Jamal, A.; Phillips, E.; Gentzke, A.S.; Homa, D.M.; Babb, S.D.; King, B.A.; Neff, L.J. Current Cigarette Smoking Among Adults—United States, 2016; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2018; pp. 53–59.
- Babb, S.; Malarcher, A.; Schauer, G.; Asman, K.; Jamal, A. Quitting Smoking Among Adults—United States, 2000–2015. Morbidity Mortal. Weekly Rep. 2017, 65, 1457–1464. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trinidad, D.R.; Pérez-Stable, E.J.; White, M.M.; Emery, S.L.; Messer, K. A Nationwide Analysis of US Racial/Ethnic Disparities in Smoking Behaviors, Smoking Cessation, and Cessation-Related Factors. Am. J. Public Health 2011, 101, 699–706. [Google Scholar] [CrossRef] [PubMed]
- North American Quitline Consortium What is a Quitline. Available online: https://www.naquitline.org/page/whatisquitline (accessed on 5 December 2020).
- North American Quitline Consortium History. Available online: http://www.naquitline.org/?page=History (accessed on 24 March 2018).
- Varghese, M.; Sheffer, C.; Stitzer, M.; Landes, R.; Brackman, S.L.; Munn, T. Socioeconomic disparities in telephone-based treatment of tobacco dependence. Am. J. Public Health 2014, 104, e76–e84. [Google Scholar] [CrossRef] [PubMed]
- Stead, L.F.; Hartmann-Boyce, J.; Perera, R.; Lancaster, T. Telephone counselling for smoking cessation. Cochrane Database Syst. Rev. 2013, 8, CD002850. [Google Scholar] [CrossRef] [PubMed]
- Matkin, W.; Ordóñez-Mena, J.M.; Hartmann-Boyce, J. Telephone counselling for smoking cessation. Cochrane Database Syst. Rev. 2019, 5, Cd002850. [Google Scholar] [CrossRef]
- Stein, C.C.; Bailey, L. NAQC FY2019 Annual Survey: Progress Update on State Quitlines; North American Quitline Consortium: Pheonix, AZ, USA, 2020. [Google Scholar]
- Fildes, E.E.; Wilson, M.A.; Crawford, B.J.; Kapella-Mshigeni, S.; Wilson, L.A.; Henkelman, W. Tobacco quitlines in the United States. Nurs. Clin. North Am. 2012, 47, 97–107. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Best Practices for Comprehensive Tobacco Control Programs—2014; U.S Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health: Atlanta, GA, USA, 2014.
- Lichtenstein, E.; Zhu, S.H.; Tedeschi, G.J. Smoking cessation quitlines: An underrecognized intervention success story. Am. Psychol. 2010, 65, 252–261. [Google Scholar] [CrossRef] [Green Version]
- Kaufman, A.; Augustson, E.; Davis, K.; Finney Rutten, L.J. Awareness and use of tobacco quitlines: Evidence from the Health Information National Trends Survey. J. Health Commun. 2010, 15 (Suppl. 3), 264–278. [Google Scholar] [CrossRef] [PubMed]
- Schauer, G.L.; Malarcher, A.M.; Zhang, L.; Engstrom, M.C.; Zhu, S.H. Prevalence and correlates of quitline awareness and utilization in the United States: An update from the 2009-2010 National Adult Tobacco Survey. Nicotine Tob. Res. 2014, 16, 544–553. [Google Scholar] [CrossRef]
- Maher, J.E.; Rohde, K.; Dent, C.W.; Stark, M.J.; Pizacani, B.; Boysun, M.J.; Dilley, J.A.; Yepassis-Zembrou, P.L. Is a statewide tobacco quitline an appropriate service for specific populations? Tob. Control 2007, 16 (Suppl. 1), i65–i70. [Google Scholar] [CrossRef]
- Kerkvliet, J.L.; Fahrenwald, N.L. Tobacco quitline outcomes for priority populations. South Dak. Med. J. South Dak. State Med. Assoc. 2015, Special Issue 2015, 63–68. [Google Scholar]
- Boles, M.; Rohde, K.; He, H.; Maher, J.E.; Stark, M.J.; Fenaughty, A.; O’Connor, T. Effectiveness of a tobacco quitline in an indigenous population: A comparison between Alaska Native people and other first-time quitline callers who set a quit date. Int. J. Circumpolar Health 2009, 68, 170–181. [Google Scholar] [CrossRef] [PubMed]
- Ruggles, S.; Genadek, K.; Goeken, R.; Grover, J.; Sobek, M. Integrated Public Use Microdata Series: Version 7.0 Tobacco USE Supplement to the Current Population Survey 2010–2011; University of Minnesota: Minneapolis, MN, USA, 2017. [Google Scholar]
- Ruggles, S.; Genadek, K.; Goeken, R.; Grover, J.; Sobek, M. Integrated Public Use Microdata Series: Version 7.0 Tobacco Use Supplement to the Current Population Survey 2014–2015; University of Minnesota: Minneapolis, MN, USA, 2017. [Google Scholar]
- Ruggles, S.; Genadek, K.; Goeken, R.; Grover, J.; Sobek, M. Integrated Public Use Microdata Series: Version 7.0 Tobacco Use Supplement to the Current Population Survey 2018; University of Minnesota: Minneapolis, MN, USA, 2017. [Google Scholar]
- National Cancer Institute, Division of Cancer Control & Population Sciences. Tobacco Use Supplement to the Current Population Survey; National Institutes of Health, National Cancer Institute, Division of Cancer Control & Population Sciences: Bethesda, MD, USA, 2018.
- US Census Bureau, A.C.S. Annual Estimates of the Resident Population for Selected Age Groups by Sex: April 1, 2010 to July 1, 2019; US Census Bureau: Washington, DC, USA, 2020.
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System (BRFSS) Prevalence Data (2011 to Present); Centers for Disease Control and Prevention: Atlanta, GA, USA, 2020.
- Centers for Disease Control and Prevention. National Quitline Data Warehouse; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2020.
- North American Quitline Consortium. Measuring Reach of Quitline Programs; North American Quitline Consortium: Phoenix, AZ, USA, 2009. [Google Scholar]
- Mann, N.; Nonnemaker, J.; Chapman, L.; Shaikh, A.; Thompson, J.; Juster, H. Comparing the New York State Smokers’ Quitline Reach, Services Offered, and Quit Outcomes to 44 Other State Quitlines, 2010 to 2015. Am. J. Health Promot. 2018, 32, 1264–1272. [Google Scholar] [CrossRef] [PubMed]
- Orzechowski, W.; Walker, R. The Tax Burden on Tobacco Volume 51, 1970–2016, 2018 ed.; Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health: Atlanta, GA, USA, 2018.
- American Nonsmokers’ Rights Foundation. Tobacco Control Laws Database: A Tool for Researchers; American Nonsmokers’ Rights Foundation: Berkeley, CA, USA, 2018. [Google Scholar]
- Current Population Survey. Design and Methodology; U.S. Department of Labor, Bureau of Labor Statistics: Washington, DC, USA, 2006.
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate—A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. B 1995, 57, 289–300. [Google Scholar] [CrossRef]
- North American Quitline Consortium. Quitline Service Offering Models: A Review of the Evidence and Recommendations for Practice in Times of Limited Resources; North American Quitline Consortium: Phoenix, AZ, USA, 2012. [Google Scholar]
- Centers for Disease Control and Prevention, Increases in quitline calls and smoking cessation website visitors during a national tobacco education campaign—March 19–June 10, 2012. MMWR Morb. Mortal. Wkly Rep. 2012, 61, 667–670.
- Farrelly, M.C.; Davis, K.C.; Nonnemaker, J.M.; Kamyab, K.; Jackson, C. Promoting calls to a quitline: Quantifying the influence of message theme, strong negative emotions and graphic images in television advertisements. Tobacco Control 2011, 20, 279. [Google Scholar] [CrossRef]
- Saul, J.E.; Bonito, J.A.; Provan, K.; Ruppel, E.; Leischow, S.J. Implementation of tobacco cessation quitline practices in the United States and Canada. Am. J. Public Health 2014, 104, e98–e105. [Google Scholar] [CrossRef] [PubMed]
- Mann, N.; Nonnemaker, J.; Davis, K.; Chapman, L.; Thompson, J.; Juster, H.R. The Potential Impact of the New York State Smokers’ Quitline on Population-Level Smoking Rates in New York. Int. J. Environ. Res. Public Health 2019, 16, 4477. [Google Scholar] [CrossRef] [Green Version]
- Lien, R.K.; Schillo, B.A.; Mast, J.L.; Lukowski, A.V.; Greenseid, L.O.; Keith, J.D.; Keller, P.A. Tobacco User Characteristics and Outcomes Related to Intensity of Quitline Program Use: Results From Minnesota and Pennsylvania. J. Public Health Manag. Pract. 2016, 22, E36–E46. [Google Scholar] [CrossRef]
- Carlin-Menter, S.; Michael, C.; Celestino, P.; Hyland, A.; Mahoney, M.; Willett, J.; Juster, H. Does Offering More Support Calls to Smokers Influence Quit Success? J. Public Health Manag. Pract. JPHMP 2011, 17, E9–E15. [Google Scholar] [CrossRef] [PubMed]
- Allen, A.M.; Yuan, N.P.; Wertheim, B.C.; Krupski, L.; Bell, M.L.; Nair, U. Gender differences in utilization of services and tobacco cessation outcomes at a state quitline. Transl. Behav. Med. 2019, 9, 663–668. [Google Scholar] [CrossRef] [PubMed]
- Martinez, S.A.; Beebe, L.A.; Campbell, J.E. Oklahoma Tobacco Helpline utilization and cessation among American Indians. Am. J. Prev. Med. 2015, 48 (Suppl. 1), S47–S53. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.H.; Gardiner, P.; Cummins, S.; Anderson, C.; Wong, S.; Cowling, D.; Gamst, A. Quitline utilization rates of African-American and white smokers: The California experience. Am. J. Health Promot. 2011, 25 (Suppl. 5), S51–S58. [Google Scholar] [CrossRef] [PubMed]
- LaVeist, T.A.; Nickerson, K.J.; Bowie, J.V. Attitudes about Racism, Medical Mistrust, and Satisfaction with Care among African American and White Cardiac Patients. Med. Care Res. Rev. 2000, 57 (Suppl. 1), 146–161. [Google Scholar] [CrossRef]
- Drwecki, B.B.; Moore, C.F.; Ward, S.E.; Prkachin, K.M. Reducing racial disparities in pain treatment: The role of empathy and perspective-taking. PAIN 2011, 152, 1001–1006. [Google Scholar] [CrossRef]
- Grady, M.; Edgar, T. Appendix D Racial disparities in health care: Highlights from focus group findings. In Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care; National Academies Press: Washington, DC, USA, 2003. [Google Scholar]
- Sheffer, C.E.; Brackman, S.L.; Cottoms, N.; Olsen, M. Understanding the barriers to use of free, proactive telephone counseling for tobacco dependence. Qual. Health Res. 2011, 21, 1075–1085. [Google Scholar] [CrossRef]
- Vickerman, K.A.; Schauer, G.L.; Malarcher, A.M.; Zhang, L.; Mowery, P.; Nash, C.M. Quitline Use and Outcomes among Callers with and without Mental Health Conditions: A 7-Month Follow-Up Evaluation in Three States. BioMed Res. Int. 2015, 2015, 817298. [Google Scholar] [CrossRef] [Green Version]
- Lukowski, A.V.; Morris, C.D.; Young, S.E.; Tinkelman, D. Quitline Outcomes for Smokers in 6 States: Rates of Successful Quitting Vary by Mental Health Status. Nicotine Tob. Res. 2015, 17, 924–930. [Google Scholar] [CrossRef]
- Syed, I.U. Clearing the Smoke Screen: Smoking, Alcohol Consumption, and Stress Management Techniques among Canadian Long-Term Care Workers. Int. J. Environ. Res. Public Health 2020, 17, 6027. [Google Scholar] [CrossRef]
- Pampel, F.; Khlat, M.; Bricard, D.; Legleye, S. Smoking Among Immigrant Groups in the United States: Prevalence, Education Gradients, and Male-to-Female Ratios. Nicotine Tob. Res. 2019, 22, 532–538. [Google Scholar] [CrossRef]

| Variables | Quitline Budget Analytic Sample | Quitline Reach Analytic Sample | Counseling Sessions Analytic Sample | Counseling Hours Analytic Sample |
|---|---|---|---|---|
| Age, mean (SD) | 46.5 (0.2) | 46.7 (0.2) | 46.7 (0.2) | 46.7 (0.2) |
| Sex, % | ||||
| Male | 53.9% | 53.8% | 53.8% | 53.8% |
| Female | 46.1% | 46.2% | 46.2% | 46.2% |
| Race/Ethnicity, % | ||||
| Non-Hispanic White | 72.2% | 72.4% | 72.4% | 72.5% |
| Non-Hispanic Black | 12.2% | 11.9% | 11.9% | 11.9% |
| Hispanic | 10.0% | 10.1% | 10.0% | 10.0% |
| Other Non-Hispanic | 5.5% | 5.6% | 5.6% | 5.6% |
| Income, % | ||||
| $0–14,999 | 20.7% | 20.2% | 20.1% | 20.1% |
| $15,000–29,999 | 21.3% | 20.9% | 20.8% | 20.8% |
| $30,000–$49,999 | 22.8% | 22.8% | 22.8% | 22.8% |
| $50,000–74,999 | 17.0% | 17.3% | 17.4% | 17.4% |
| $75,000 and over | 18.2% | 18.8% | 18.9% | 18.8% |
| Education, % | ||||
| Less than High School | 16.2% | 16.0% | 15.9% | 16.0% |
| HS Graduate | 37.9% | 37.8% | 37.9% | 37.9% |
| Some College | 31.6% | 31.9% | 31.9% | 31.9% |
| College | 14.3% | 14.3% | 14.3% | 14.3% |
| 90-day Cessation, % | 7.975% | 7.985% | 7.980% | 7.971% |
| 30-day Cessation, % | 9.523% | 9.544% | 9.547% | 9.541% |
| State-level Smoke-free laws, % | 66.9% | 68.5% | 68.9% | 68.8% |
| State-level Cigarette Price, mean (SD) | 6.5 (0.3) | 6.6 (0.3) | 6.6 (0.3) | 6.6 (0.3) |
| N | 46,962 | 56,936 | 57,940 | 57,618 |
| Budget per smoker in USD, mean (SD) | 3.5 (0.5) | -- | -- | -- |
| Reaching ≥ 0.7% of smokers, % | -- | 35.9% | ||
| Counseling sessions ≥ 5, % | -- | -- | 58.3% | -- |
| Counseling available at least from 7 a.m. to 7 p.m. (7 days/week), % | -- | -- | -- | 53.7% |
| Bivariate Model a | Adjusted Model b | |
|---|---|---|
| OR (95% CI) | OR (95% CI) | |
| Budget per smoker | 1.005 (0.998, 1.011) | 1.004 (0.998, 1.010) |
| Reach | 1.005 (0.932, 1.082) | 0.975 (0.911, 1.043) |
| ≥Median reach vs. <median | ||
| Counseling sessions | 0.988 (0.909, 1.075) | 0.971 (0.901, 1.045) |
| ≥5 sessions offered vs. <5 | ||
| Hours Available for Counseling 7 a.m–7 p.m. vs. not 7 a.m.–7 p.m. | 1.017 (0.915, 1.130) | 1.019 (0.915, 1.135) |
| Budget per Smoker | Reach | Counseling Sessions | Hours of Counseling | |
|---|---|---|---|---|
| Sex | 0.008 | 0.429 | 0.585 | 0.452 |
| Race/ethnicity | 0.949 | 0.568 | 0.095 | 0.565 |
| Education | 0.023 | 0.055 | 0.022 * | 0.022 * |
| Family income | 0.897 | 0.321 | 0.770 | 0.054 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Colston, D.C.; Simard, B.J.; Xie, Y.; McLeod, M.C.; Elliott, M.R.; Thrasher, J.F.; Fleischer, N.L. The Association between Quitline Characteristics and Smoking Cessation by Educational Attainment, Income, Race/Ethnicity, and Sex. Int. J. Environ. Res. Public Health 2021, 18, 3297. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18063297
Colston DC, Simard BJ, Xie Y, McLeod MC, Elliott MR, Thrasher JF, Fleischer NL. The Association between Quitline Characteristics and Smoking Cessation by Educational Attainment, Income, Race/Ethnicity, and Sex. International Journal of Environmental Research and Public Health. 2021; 18(6):3297. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18063297
Chicago/Turabian StyleColston, David C., Bethany J. Simard, Yanmei Xie, Marshall Chandler McLeod, Michael R. Elliott, James F. Thrasher, and Nancy L. Fleischer. 2021. "The Association between Quitline Characteristics and Smoking Cessation by Educational Attainment, Income, Race/Ethnicity, and Sex" International Journal of Environmental Research and Public Health 18, no. 6: 3297. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18063297






