The Psychosocial and Somatic Effects of Relocation from Remote Canadian First Nation Communities to Urban Centres on Indigenous Peoples with Chronic Kidney Disease (CKD)
Abstract
:1. Introduction
2. Chronic Kidney Disease (CKD)
2.1. Stages of Chronic Kidney Disease (CKD)
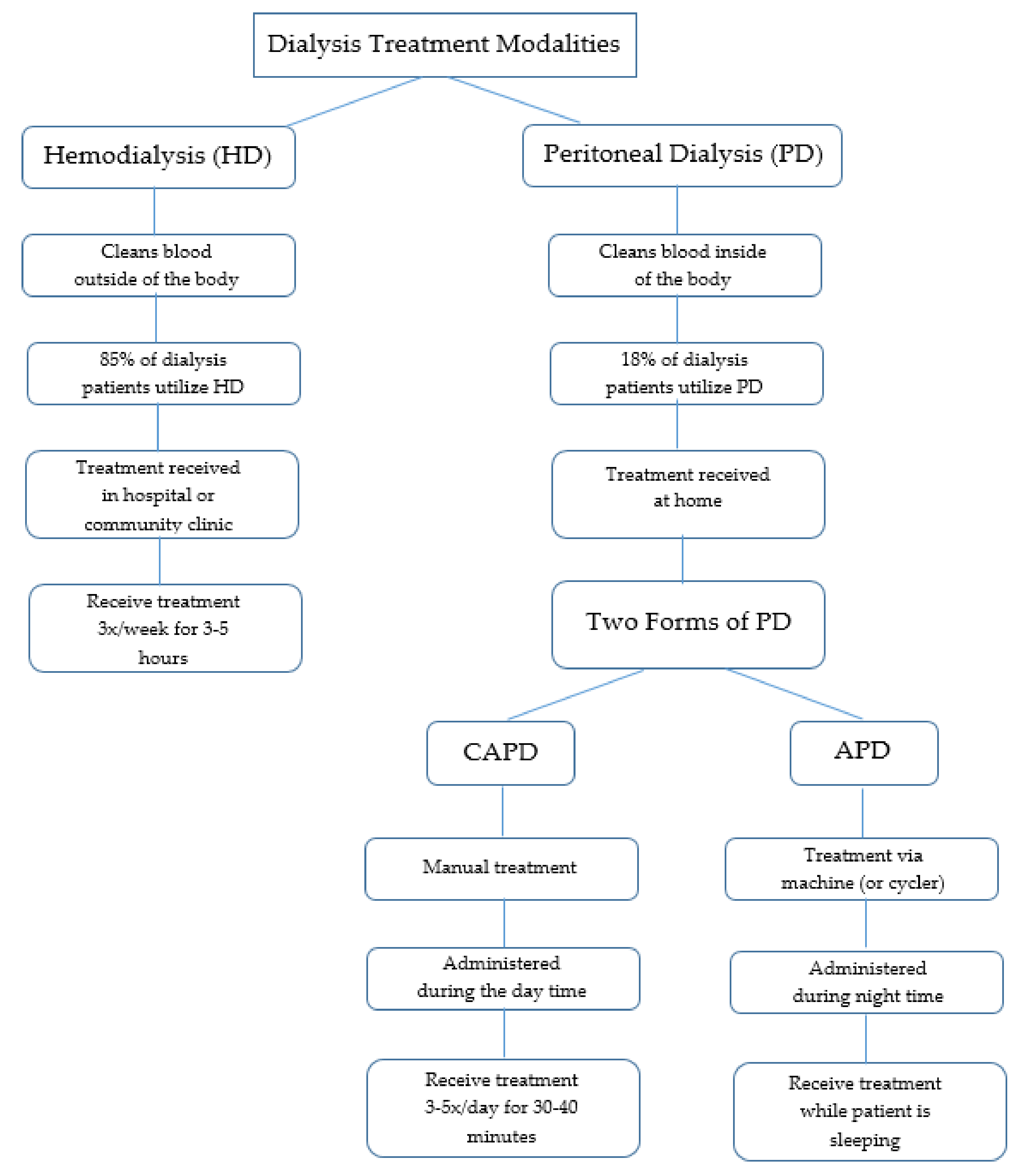
2.2. Forms of Treatment
2.2.1. Hemodialysis (HD)
2.2.2. Peritoneal Dialysis (PD)
3. Dialysis and Northern First Nation Communities
3.1. Quality of Living
3.2. Geographical Location
3.3. Medical Relocation
3.4. Selection of Dialysis Treatment
4. Methods
5. Literature Review
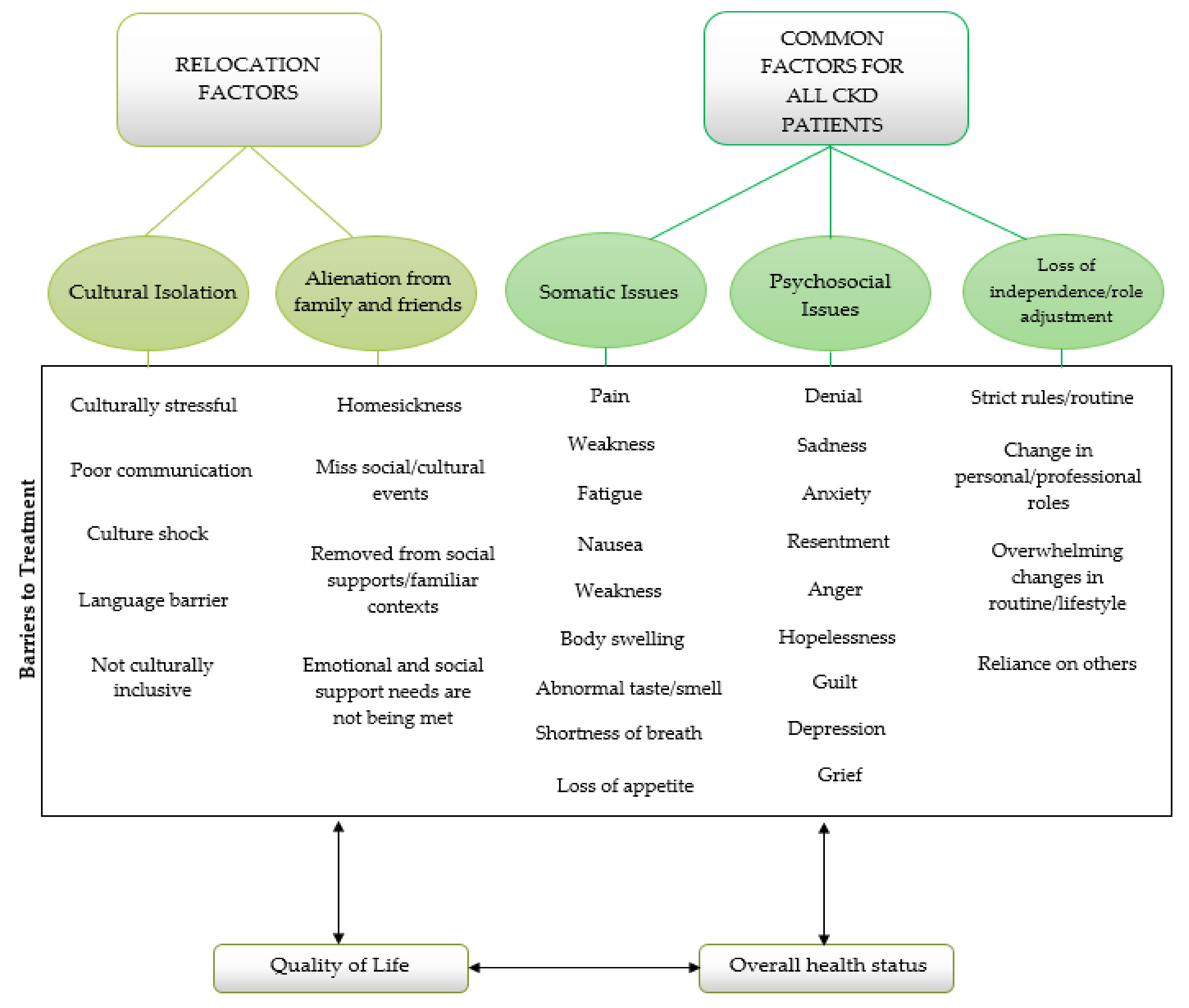
5.1. Cultural Isolation
5.2. Alienation from Family and Friends
5.3. Somatic Issues
5.4. Psychosocial Issues
5.5. Loss of Independence and Role Adjustment
6. Discussion
7. Future Implications
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- The Kidney Foundation of Canada. Facing the Facts. 2018. Available online: https://www.kidney.ca/facing-the-facts (accessed on 15 June 2018).
- Gao, S.; Manns, B.J.; Culleton, B.F.; Tonelli, M.; Quan, H.; Crowshoe, L.; Hemmelgarn, B.R. Prevalence of chronic kidney disease and survival among Aboriginal people. J. Am. Soc. Nephrol. 2007, 18, 2953–2959. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harasemiw, O.; Milks, S.; Oakley, L.; Lavallee, B.; Chartrand, C.; McLeod, L.; Di Nella, M.; Komenda, P. Remote dwelling location is a risk factor for CKD among indigenous Canadian. Kidney Int. Rep. 2018, 3, 825–832. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kolewaski, C.D.; Paterson, M.L.; Yeates, K.E.; Vlack, K.V.; Cheryl, E. Relocating from the mushkegowuk territory for hemodialysis: The cree illness experience and perceived quality of life. Pimatisiwin J. Aborig. Indig. Community Health 2010, 8, 103–150. [Google Scholar]
- Mathew, A.T.; Park, J.; Sachdeva, M.; Sood, M.M.; Yeates, K. Barriers to peritoneal dialysis in aboriginal patients. Can. J. Kidney Health Dis. 2018, 5, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Wilson, R.; Krefting, L.; Sutcliffe, P.; Van Busel, L. Native Canadians relocating for renal dialysis: Psychosocial and cultural issues. Can. Fam. Physician 1994, 40, 1934–1941. [Google Scholar] [PubMed]
- Young, T.K.; Kaufert, J.M.; McKenzie, J.K.; Hawkins, A.; O’neil, J. Excessive burden of end-stage renal disease among Canadian Indians: A national survey. Am. J. Public Health 1989, 20, 756–758. [Google Scholar] [CrossRef] [Green Version]
- Tonelli, M.; Hemmelgarn, B.; Manns, B.; Davison, S.; Bohm, C.; Gourishankar, S.; Gill, J.S. Use and outcomes of peritoneal dialysis among Aboriginal people in canada. J. Am. Soc. Nephrol. 2005, 16, 482–488. [Google Scholar] [CrossRef] [Green Version]
- Salvalaggio, G.; Kelly, L.; Minore, B. Perspectives on health: Experiences of first nations dialysis patients relocated from remote communities for treatment. Can. J. Rural Med. 2003, 8, 19–24. [Google Scholar]
- Sood, M.M.; Komenda, P.; Sood, A.R.; Reslerova, M.; Verrelli, M.; Sathianathan, C.; Rigatto, C. Adverse outcomes among Aboriginal patients receiving peritoneal dialysis. Can. Med. Assoc. J. 2010, 182, 1433–1439. [Google Scholar] [CrossRef] [Green Version]
- Mayo Clinic. Chronic Kidney Disease. 2018. Available online: https://www.mayoclinic.org/diseases-condition/chronic-kidney-disease/symptoms-causes/sync-20354521 (accessed on 17 June 2018).
- The National Institute of Diabetes and Digestive and Kidney Diseases. Kidney Disease Statistics for the United States. 2016. Available online: https://www.niddk.nih.gov/health-information/health-statistics/kidney-disease (accessed on 17 June 2018).
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 2013, 3, 1–150. [Google Scholar]
- Frank, A.; Auslander, G.K.; Weissgarten, J. Quality of life of patients with end-stage renal disease at various stages of the illness. Soc. Work Health Care 2003, 38, 1–27. [Google Scholar] [CrossRef]
- White, Y.; Grenyer, B.F. The biopsychosocial impact of end-stage renal disease: The experience of dialysis patients and their partners. J. Adv. Nurs. 1999, 30, 1312–1320. [Google Scholar] [CrossRef]
- Cunha, J.P. What is Dialysis? Peritoneal, Hemodialysis, Fistula, Diet & Life Expectancy. MedicineNet. 2017. Available online: www.medicinenet.com/dialysis/article.htm (accessed on 18 June 2018).
- National Kidney Foundation. Dialysis. 2017. Available online: https://www.kidney.org/atoz/content/dialysisinfo (accessed on 18 June 2018).
- Courts, N.F.; Boyette, B.G. Psychosocial adjustment of males on three types of dialysis. Clin. Nurs. Res. 1988, 7, 47–63. [Google Scholar] [CrossRef]
- Curtin, R.B.; Mapes, D.; Petillo, M.; Oberley, E. Long-term dialysis survivors: A transformational experience. Qual. Health Res. 2002, 12, 609–624. [Google Scholar] [CrossRef]
- Canadian Institute for Health Information. End-Stage Renal Disease among Aboriginal Peoples in Canada: Treatment and Outcomes; Canadian Institute for Health Information: Ottawa, ON, Canada, 2013. [Google Scholar]
- Murphy, S.W.; Foley, R.N.; Barrett, B.J.; Kent, G.M.; Morgan, J.; Barré, P.; Jindal, K.K. Comparative hospitalization of hemodialysis and peritoneal dialysis patients in Canada. Kidney Int. 2000, 57, 2557–2563. [Google Scholar] [CrossRef] [Green Version]
- Tonelli, M.; Manns, B.; Culleton, B.; Klarenbach, S.; Hemmelgarn, B.; Wiebe, N.; Gill, J.S. Association between proximity to the attending nephrologist and mortality among patients receiving hemodialysis. Can. Med. Assoc. J. 2007, 177, 1039–1044. [Google Scholar] [CrossRef] [Green Version]
- Tonelli, M.; Hemmelgarn, B.; Culleton, B.; Klarenbach, S.; Gill, J.S.; Wiebe, N.; Mann, B. Mortality of Canadians treated by peritoneal dialysis in remote locations. Kidney Int. 2007, 72, 1023–1028. [Google Scholar] [CrossRef] [Green Version]
- Zacharias, J.; Komenda, P.; Olson, J.; Bourne, A.; Franklin, D.; Bernstein, K. Home hemodialysis in the remote Canadian north: Treatment in manitoba fly-in communities. Semin. Dial. 2011, 24, 653–657. [Google Scholar] [CrossRef]
- Gionet, L. First Nations People: Selected Findings of the 2006 Census. 2009. Available online: https://www150.statcan.gc.ca/n1/pub/11-008-x/2009001/article/10864-eng.htm (accessed on 18 June 2018).
- Pauls, K. Water Access ‘a Disaster’ on Northern Man. Reserves. 2011. Available online: http://www.cbc.ca/news/canada/manitoba/water-access-a-disaster-on-northen-man-reserves-1/1012697 (accessed on 18 June 2018).
- Marrone, S. Understanding barriers to health care: A review of disparities in health care services among indigenous populations. Int. J. Circumpolar Health 2007, 66, 188–198. [Google Scholar] [CrossRef]
- Lavoie, J.G.; Kaufert, J.; Browne, A.J.; Mah O’Neil, J.S.; Sinclair, S.; BlueSky, K. Negotiating barriers, navigating the maze: First nation peoples’ experience of medical relocation. Can. Public Adm. 2015, 58, 295–314. [Google Scholar] [CrossRef]
- Shah, B.R.; Gunraj, N.; Hux, J.E. Markers of access to and quality of primary care for Aboriginal people in ontario, Canada. Am. J. Public Health 2003, 93, 798–802. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shah, C.P.; Farkas, C.S. The health of Indians in canadian cities: A challenge to the health care system. Can. Med. Assoc. J. 1985, 133, 859–863. [Google Scholar]
- Haverkamp, G.L.; Loosman, W.L.; van den Beukel, T.O.; Hoekstra, T.; Dekker, F.W.; Shaw, P.K.C.; Siegert, C.E. The association of acculturation and depressive and anxiety symptoms in immigrant chronic dialysis patients. Gen. Hosp. Psychiatry 2016, 28, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Peiris, D.; Brown, A.; Cass, A. Addressing inequities in access to quality health care for indigenous people. Can. Med. Assoc. J. 2008, 179, 985–986. [Google Scholar] [CrossRef] [Green Version]
- Gregory, D.; Whalley, W.; Olson, J.; Bain, M.; Harper, G.G.; Roberts, L.; Russell, C. Exploring the experience of type 2 diabetes in urban Aboriginal people. Can. J. Nurs. Res. Arch. 1999, 31, 101–115. [Google Scholar]
- Bello, A.K.; Hemmelgarn, B.; Lin, M.; Manns, B.; Klarenbach, S.; Thompson, S.; Tonelli, M. Impact of remote location on quality care delivery and relationships to adverse health outcomes in patients with diabetes and chronic kidney disease. Nephrol. Dial. Transplant. 2012, 27, 3849–3855. [Google Scholar] [CrossRef] [Green Version]
- Gregory, D.M.; Way, C.Y.; Hutchinson, T.A.; Barrett, B.J.; Parfrey, P.S. Patients’ perceptions of their experiences with ESRD and hemodialysis treatment. Qual. Health Res. 1998, 8, 764–783. [Google Scholar] [CrossRef]
- White, C.; McDonnell, H. Psychosocial distress in patients with end-stage kidney disease. J. Ren. Care 2014, 20, 74–81. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Genereux, D.; Fan, L.; Brownlee, K. The Psychosocial and Somatic Effects of Relocation from Remote Canadian First Nation Communities to Urban Centres on Indigenous Peoples with Chronic Kidney Disease (CKD). Int. J. Environ. Res. Public Health 2021, 18, 3838. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18073838
Genereux D, Fan L, Brownlee K. The Psychosocial and Somatic Effects of Relocation from Remote Canadian First Nation Communities to Urban Centres on Indigenous Peoples with Chronic Kidney Disease (CKD). International Journal of Environmental Research and Public Health. 2021; 18(7):3838. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18073838
Chicago/Turabian StyleGenereux, Denise, Lida Fan, and Keith Brownlee. 2021. "The Psychosocial and Somatic Effects of Relocation from Remote Canadian First Nation Communities to Urban Centres on Indigenous Peoples with Chronic Kidney Disease (CKD)" International Journal of Environmental Research and Public Health 18, no. 7: 3838. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph18073838




