Trends in Percutaneous Coronary Interventions in New South Wales, Australia
Abstract
:1. Introduction
2. Methods
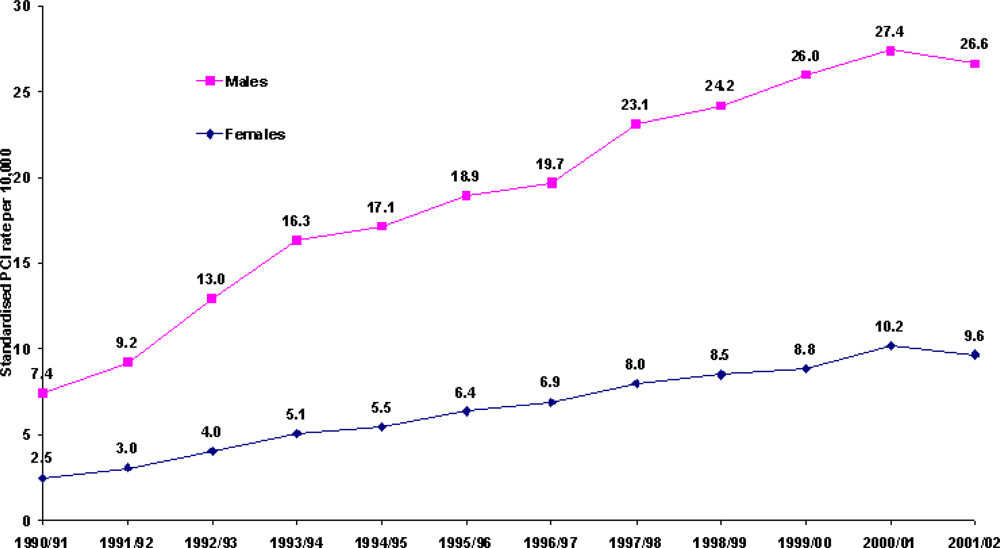
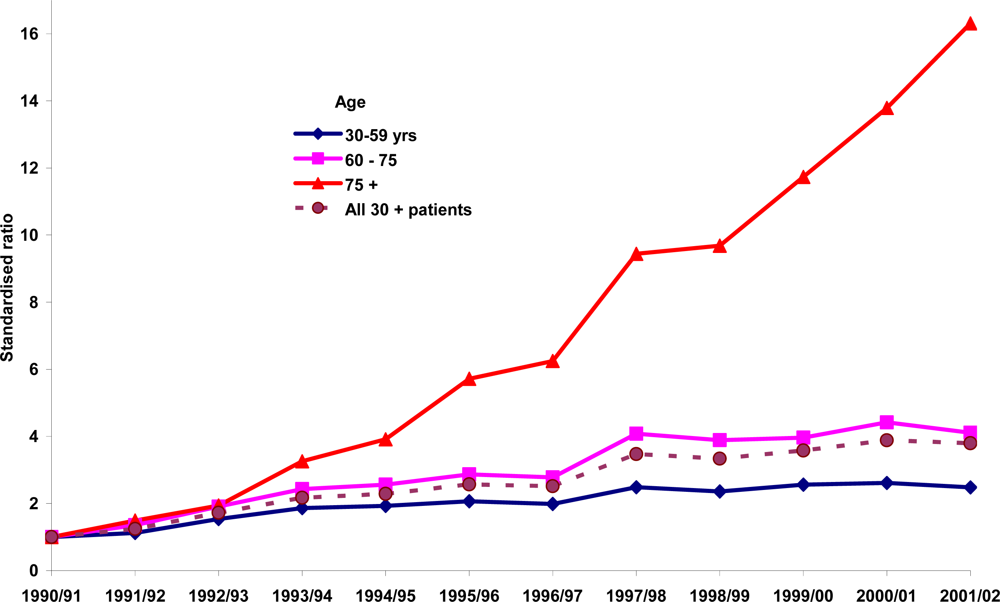
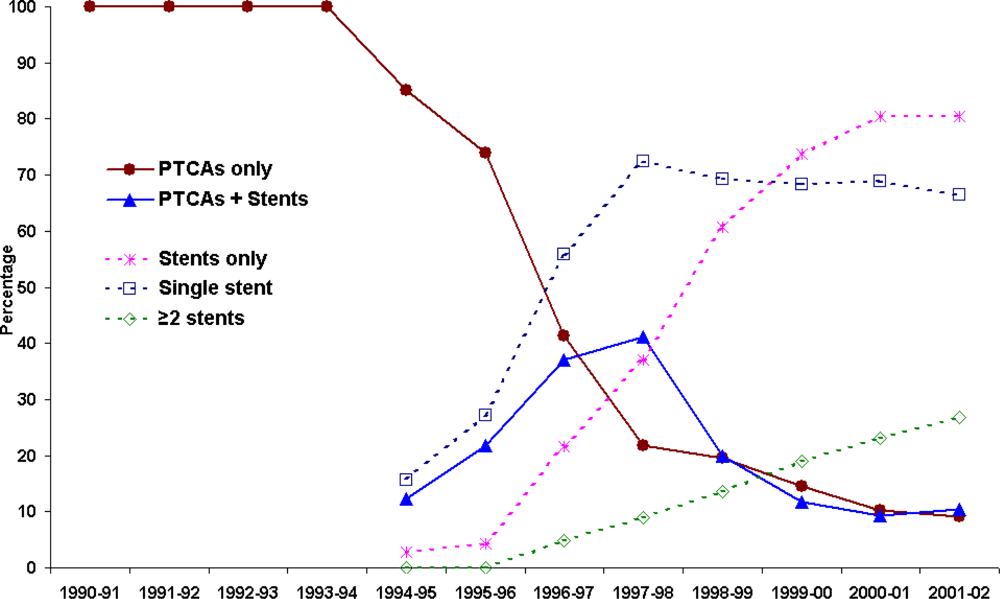
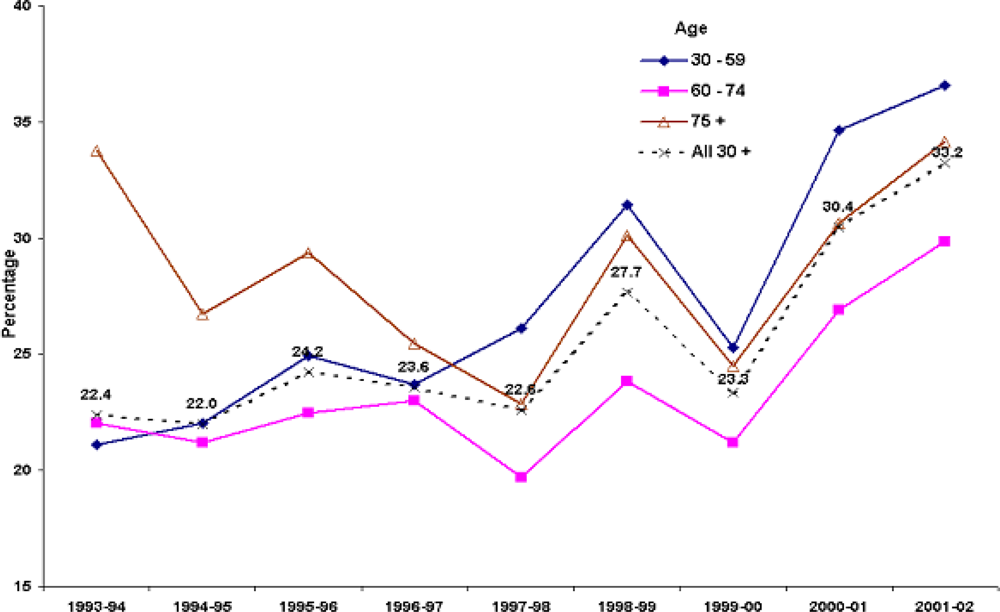
3. Results
5. Discussion
Competing interests
Authors’ contributions
Acknowledgments
References
- Mueller, RL; Sanborn, TA. The history of interventional cardiology: Cardiac catheterization, angioplasty, and related interventions. Am. Heart J 1995, 129, 146–172. [Google Scholar]
- Wilms, G; Baert, AL. The history of angiography. J. Belge. Radiol 1995, 78, 299–302. [Google Scholar]
- Gruntzig, AR; Senning, A; Siegenthaler, WE. Nonoperative dilatation of coronary-artery stenosis: percutaneous transluminal coronary angioplasty. N. Engl. J. Med 1979, 301, 61–68. [Google Scholar]
- Payne, MM. Charles Theodore Dotter: The father of intervention. Tex. Heart Inst. J 2001, 28, 28–38. [Google Scholar]
- Regulation (EC) No 139/2004 Merger Procedure. Available at http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2004:024:0001:0022:EN:PDF (accessed on 25 August 2005).
- National Heart Foundation of Australia Coronary Angioplasty, Report No. 10; National Heart Foundation of Australia: Canberra, Australia, 1996.
- OECD: Moise, P.; Jacobzone, S.; the ARD-IHD Experts Group OECD Study of Cross-national Differences in the Treatment, Costs and Outcomes of Ischaemic Heart Disease, OECD Health Working Papers No. 3 (DELSA/ELSA/WD/HEA(2003)3); Organisation for Economic Cooperation and Development: Paris, France, 2003.
- AIHW: Davies, J. Coronary Revascularisation in Australia, 2000, AIHW Cat. No. AUS 35, Bulletin No. 7; Australian Institute of Health and Welfare: Canberra, Australia, 2003.
- AIHW: Davies, J.; Senes, S. Coronary Angioplasty in Australia 1999, AIHW Cat. No. CVD 19, Cardiovascular Disease Series No. 19; Australian Institute of Health and Welfare and National Heart Foundation of Australia: Canberra, Australia, 2002.
- AIHW Health in Rural and Remote Australia: The First Report of The Australian Institute of Health and Welfare on Rural Health, AIHW Cat. No. PHE 6, ABS Cat. No. 8919.0; Australian Institute of Health and Welfare: Canberra, Australia, 1998.
- AIHW: Moon, L.; Waters, A.M. Socioeconomic Inequalities in Cardiovascular Disease in Australia: Current Picture and Trends Since The 1990s, Bulletin No. 37. AIHW Cat. No. AUS 74; Australian Institute of Health and Welfare: Canberra, Australia, 2006.
- Yu, XQ; Robertson, C; Brett, I. Socioeconomic correlates of mortality differentials by local government area in rural northern New South Wales, 1981–1995. Aust. N Z. J. Public Health 2000, 24, 365–369. [Google Scholar]
- Carlisle, DM; Valdez, RB; Shapiro, MF; Brook, RH. Geographic variation in rates of selected surgical procedures within Los Angeles County. Health Serv. Res 1995, 30, 27–42. [Google Scholar]
- Taylor, R; Chey, T; Bauman, A; Webster, I. Socio-economic, migrant and geographic differentials in coronary heart disease occurrence in New South Wales. Aust. N Z. J. Public Health 1999, 23, 20–26. [Google Scholar]
- NCCH ICD10AM second edition browser V1.1 internet based software. http://nis-web.fhs.usyd.edu.au/ncch_new/ (accessed on 12 March 2008).
- MacIntyre, CR. Accuracy of ICD-9CM codes in hospital morbidity data, Victoria: Implications for public health research. Aust. N Z. J. Public Health 1997, 21, 477–482. [Google Scholar]
- AIHW: Waters, A.M.; Armstrong, T.; Senes, S. Medical Care of Cardiovascular Disease in Australia, CVD Cat No. 4, Cardiovascular Disease Series No. 7, Australian Institute of Health and Welfare: Canberra, Australia, 1998.
- Rentoukas, EI; Lazaros, GA; Arapi, SM; Koulouris, SA; Zacharoulis, AA. Coronary artery revascularization in the elderly: Percutaneous coronary angioplasty or bypass grafting? Hellenic J. Cardiol 2003, 44, 125–135. [Google Scholar]
- Malenka, DJ; O’Rourke, D; Miller, MA; Hearne, MJ; Shubrooks, S; Kellett, MAJ; Robb, JF; O’Meara, JR; VerLee, P; Bradley, WA; Wennberg, D; Ryan, TJ; Vaitkus, PT; Hettleman, B; Watkins, MW; McGrath, PD; O’Connor, GT. Cause of in-hospital death in 12,232 consecutive patients undergoing percutaneous transluminal coronary angioplasty: The Northern New England Cardiovascular Disease Study Group. Am. Heart J 1999, 137, 632–638. [Google Scholar]
- Schunkert, H; Harrel, L; Palacios, IF. Implications of small reference vessel diameter in patients undergoing percutaneous coronary revascularization. J. Am. Coll. Cardiol 1999, 34, 40–48. [Google Scholar]
- Tseng, CD; Chen, CY; Chiang, FT; Hsu, KL; Lo, HM; Tseng, YZ; Tsai, CH. Coronary artery perforation and delayed cardiac tamponade following balloon coronary angioplasty. J. Formos. Med. Assoc 1996, 95, 789–792. [Google Scholar]
- Bozinovski, J; Wang, S; Nakai, S. Delayed cardiac tamponade after coronary artery laceration. Ann. Thorac. Surg 2002, 73, 1314–1315. [Google Scholar]
- Fejka, M; Kahn, JK. Diagnosis, management, and clinical outcome of cardiac tamponade complicating percutaneous coronary intervention. Cardiovasc. Rev. Rep 2003, 24, 416–420. [Google Scholar]
- Stankovic, G; Orlic, D; Corvaja, N; Airoldi, F; Chieffo, A; Spanos, V; Montorfano, M; Carlino, M; Finci, L; Sangiorgi, G; Colombo, A. Incidence, predictors, in-hospital, and late outcomes of coronary artery perforations. Am. J. Cardiol 2004, 93, 213–216. [Google Scholar]
- Ellis, SG; Ajluni, S; Arnold, AZ; Popma, JJ; Bittl, JA; Eigler, NL; Cowley, MJ; Raymond, RE; Safian, RD; Whitlow, PL. Increased coronary perforation in the new device era: Incidence, classification, management, and outcome. Circulation 1994, 90, 2725–2730. [Google Scholar]
- Weerasinghe, DP; Wolfenden, HD; Yusuf, F. Coronary artery bypass graft surgery trends in New South Wales, Australia. Public Health 2008, 122, 151–160. [Google Scholar]
- AIHW: Davies, J.; Senes, S. Cardiac Surgery in Australia 1998, AIHW Cat. No. CVD 16; Australian Institute of Health and Welfare and National Heart Foundation of Australia: Canberra, Australia, 2001.
- NSW Department of Health The Health of the People of New South Wales - 2000, Report of The Chief Health Officer, State Health Publication No. (PHD) 000053, December; Population Health Division, NSW Department of Health: Sydney, Australia, 2000.
- Hobbs, MST; McCaul, KA; Knuiman, MW; Rankin, JM; Gilfillan, I. Trends in coronary artery revascularisation procedures in Western Australia, 1980–2001. Heart 2004, 90, 1036–1041. [Google Scholar]
- Ulrich, MR; Brock, DM; Ziskind, AA. Analysis of trends in coronary artery bypass grafting and percutaneous coronary intervention rates in Washington state from 1987 to 2001. Am. J. Cardiol 2003, 92, 836–839. [Google Scholar]
- EOHCS: Healy, J. Health Care Systems in Eight Countries: Trends and Challenges: Australia, Dixon, A; Mossialos, E (Eds.) The European Observatory on Health Care Systems, London School of Economics and Political Science: London, UK, 2002.
- Elliot, A. The Decline in Bulk Billing: Explanations and Implications. http://www.aph.gov.au/library/pubs/cib/2002-03/03CIB03.htm (accessed on 11 December 2007).
- Doran, E; Henry, DA. The PBS community awareness campaign: How helpful is blaming patients? Med. J. Aust 2003, 179, 544–545. [Google Scholar]
- Adams, MR; Orford, JL; Blake, GJ; Wainstein, MV; Byrne, JG; Selwyn, AP. Rescue percutaneous coronary intervention following coronary artery bypass graft - a descriptive analysis of the changing interface between interventional cardiologist and cardiac surgeon. Clin. Cardiol 2002, 25, 280–286. [Google Scholar]
- Murphy, GJ; Bryan, AJ; Angelini, GD. Hybrid coronary revascularization in the era of drug-eluting stents. Ann. Thorac. Surg 2004, 78, 1861–1867. [Google Scholar]


| Financial year | Percentages of coexisting conditionsa | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Diabetes | ARF | CRF | AMI | CHF | Hypertension | PVD | CVD | PD | |
| 1990–91 | 8.2 | 0.1 | 1.0 | 8.0 | 2.0 | 25.1 | 2.8 | 1.5 | 3.6 |
| 1991–92 | 9.3 | 0.2 | 0.9 | 12.5 | 3.1 | 30.8 | 2.5 | 1.7 | 5.3 |
| 1992–93 | 8.4 | 0.1 | 0.7 | 12.6 | 3.7 | 28.6 | 3.0 | 1.1 | 4.6 |
| 1993–94 | 9.6 | 0.3 | 0.7 | 11.6 | 2.7 | 29.0 | 4.0 | 1.4 | 5.0 |
| 1994–95 | 10.0 | 0.2 | 0.5 | 13.9 | 2.8 | 28.8 | 3.0 | 1.3 | 4.8 |
| 1995–96 | 11.8 | 0.4 | 0.8 | 14.5 | 2.2 | 31.1 | 3.6 | 1.5 | 5.8 |
| 1996–97 | 12.3 | 0.3 | 1.1 | 19.4 | 2.1 | 35.7 | 3.6 | 1.2 | 7.0 |
| 1997–98 | 12.2 | 0.4 | 1.3 | 17.7 | 2.2 | 31.4 | 3.8 | 1.1 | 6.5 |
| 1998–99 | 13.6 | 0.4 | 1.4 | 20.1 | 2.8 | 35.0 | 3.5 | 1.3 | 7.0 |
| 1999–00 | 14.1 | 0.5 | 1.8 | 22.1 | 3.2 | 35.4 | 3.5 | 1.3 | 5.7 |
| 2000–01 | 16.4 | 0.6 | 1.7 | 26.2 | 3.5 | 39.7 | 3.1 | 1.0 | 4.8 |
| 2001–02 | 16.8 | 0.8 | 2.6 | 29.1 | 3.5 | 43.0 | 4.3 | 1.5 | 4.3 |
| Overall | 13.4 | 0.4 | 1.4 | 20.2 | 3.0 | 35.5 | 3.6 | 1.3 | 5.7 |
| t value | 11.4 | 7.0 | 3.1 | 8.6 | 1.0 | 5.3 | 1.5 | –0.4 | 0.5 |
| p value | <0.001 | <0.001 | 0.011 | <0.001 | 0.335 | 0.004 | 0.177 | 0.701 | 0.654 |
| Independent variable | Logistic regression models by complications
| |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diabetes | RF | AMI | CHF | PVD | CVD | PD | ||||||||
| OR | CI | OR | CI | OR | CI | OR | CI | OR | CI | OR | CI | OR | CI | |
| Asia | 1.90 1.67–2.15 | 1.64 1.19 2.27 | 1.32 1.18 1.49 | 1.23 0.91 1.65 | 0.38 0.24 0.59 | 0.88 0.54 1.43 | 0.68 0.53 0.87 | |||||||
| Europe | 1.59 1.48–1.70 | 1.07 0.89 1.29 | 1.00 0.94 1.07 | 1.45 1.27 1.65 | 1.03 0.90 1.18 | 0.89 0.71 1.11 | 0.71 0.63 0.81 | |||||||
| UK | 0.72 0.65–0.81 | 0.78 0.59 1.02 | 0.83 0.76 0.91 | 0.81 0.65 1.00 | 1.21 1.03 1.41 | 0.73 0.53 1.00 | 0.85 0.73 0.98 | |||||||
| Middle East | 2.45 2.18–2.76 | 1.67 1.20 2.31 | 1.34 1.19 1.50 | 1.58 1.21 2.06 | 0.91 0.68 1.23 | 1.25 0.82 1.90 | 0.66 0.51 0.85 | |||||||
| Pacific | 3.02 2.43–3.75 | 1.75 0.92 3.30 | 1.37 1.10 1.71 | 1.29 0.72 2.30 | 0.99 0.56 1.77 | 1.36 0.60 3.06 | 0.61 0.36 1.04 | |||||||
| Other | 1.19 1.02–1.39 | 1.20 0.80 1.78 | 1.35 1.19 1.52 | 0.87 0.60 1.26 | 0.77 0.54 1.08 | 0.98 0.59 1.62 | 0.78 0.60 1.01 | |||||||
| Australia | ||||||||||||||
| Sex - Male Female | 0.77 0.73–0.81 | 0.96 0.83 1.10 | 0.99 0.95 1.05 | 0.73 0.66 0.81 | 0.86 0.78 0.95 | 0.77 0.66 0.90 | 0.84 0.77 0.91 | |||||||
| Age 30–59 60–74 | 0.83 0.78–0.87 | 0.43 0.36 0.51 | 1.54 1.47 1.61 | 0.51 0.45 0.58 | 0.40 0.36 0.45 | 0.33 0.27 0.41 | 0.64 0.58 0.69 | |||||||
| >=75 | 0.90 0.83–0.97 | 2.71 2.35 3.12 | 1.26 1.18 1.35 | 2.27 2.02 2.55 | 1.63 1.46 1.82 | 1.48 1.24 1.77 | 1.27 1.15 1.40 | |||||||
| c statistic | 0.585 | 0.675 | 0.564 | 0.661 | 0.645 | 0.659 | 0.591 | |||||||
| Independent variable | % * | Bivariate
| Multivariate
| |||
|---|---|---|---|---|---|---|
| χ2 | p value | OR (95% CI) | p value | |||
| Sex (female) | 29.0 | 4.8 | 0.027 | 1.098 (0.943–1.279) | 0.226 | |
| Age | 30–59 | 37.7 | 2.9 | 0.083 | 0.875 (0.755–1.014) | 0.076 |
| 60–74 | 49.5 | 3.7 | 0.052 | |||
| >=75 | 12.8 | 0.12 | 0.724 | 1.037 (0.836–1.287) | 0.741 | |
| Year of PCIs (continuous variable) | 1.011 (0.984–1.040) | 0.424 | ||||
| Emergency admissions | 52.9 | 112.5 | <0.001 | 1.745 (1.509–2.018) | <0.001 | |
| PTCA only | 73.6 | 381.9 | <0.001 | 7.476 (5.947–9.398) | <0.001 | |
| PTCA & Stent combined and Stent only | 26.4 | 121.7 | <0.001 | |||
| Cardiac tamponade | 0.68 | 20.2 | <0.001 | 4.298 (1.719–10.74) | 0.001 | |
| Perforation | 7.8 | 418.9 | <0.001 | 11.261 (8.506–14.91) | <0.001 | |
| Hypotension | 3.5 | 60.9 | <0.001 | 0.778 (0.105–5.786) | 0.806 | |
| Multi-vessel disease | 16.8 | 26.2 | 0.067 | 5.522 (4.340–7.027) | <0.001 | |
Share and Cite
Weerasinghe, D.P.; Yusuf, F.; Parr, N.J. Trends in Percutaneous Coronary Interventions in New South Wales, Australia. Int. J. Environ. Res. Public Health 2009, 6, 232-245. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph6010245
Weerasinghe DP, Yusuf F, Parr NJ. Trends in Percutaneous Coronary Interventions in New South Wales, Australia. International Journal of Environmental Research and Public Health. 2009; 6(1):232-245. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph6010245
Chicago/Turabian StyleWeerasinghe, Daminda P., Farhat Yusuf, and Nicholas J. Parr. 2009. "Trends in Percutaneous Coronary Interventions in New South Wales, Australia" International Journal of Environmental Research and Public Health 6, no. 1: 232-245. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph6010245




