1. Introduction
Implant restorations in the anterior zone are usually accompanied with patients’ higher aesthetic expectations and sufficient available bone volume. Slight deviations of the implant position may harm important anatomical structures such as adjacent teeth, or lead to a series of esthetic, biological and technical complications [
1,
2]. Therefore, how to avoid the occurrence of adverse events and achieve the precise placement of the optimal three-dimensional position of the implant is a challenge for every implantologist.
The wide usage of CBCT data in combination with implant planning software has made it possible to lead predictable outcomes. One possible technique that facilitates a more accurate implant positioning is computer-assisted, template-guided implantology [
3,
4]. Different from the traditional free-hand implant placement that overly relies on the clinician’s skill set and experience, computer-assisted, template-guided implantology is driven by final optimal restoration, according to which clinicians address considerations for the most optimal implant position prior to the surgery [
5,
6,
7]. The template has been postulated to provide higher precision [
8,
9,
10,
11], which can help to achieve better implant placement with the potential for reduced operative complications [
12,
13,
14]. Through digital designing software such as Simplant
® and Nobel Clinician
®, the patient’s cone-beam computed tomography (CBCT) data was overlapping with the intraoral or model three-dimensional data obtained by an optical scanner [
15], so that the clinicians can virtually plan the optimal three-dimensional implant position before the operation. Then, using the computer-aided design and computer-aided manufacturing (CAD-CAM) technology to fabricate the surgical template, and with the assistance of which we can transfer the preoperative virtual plan into the actual surgery.
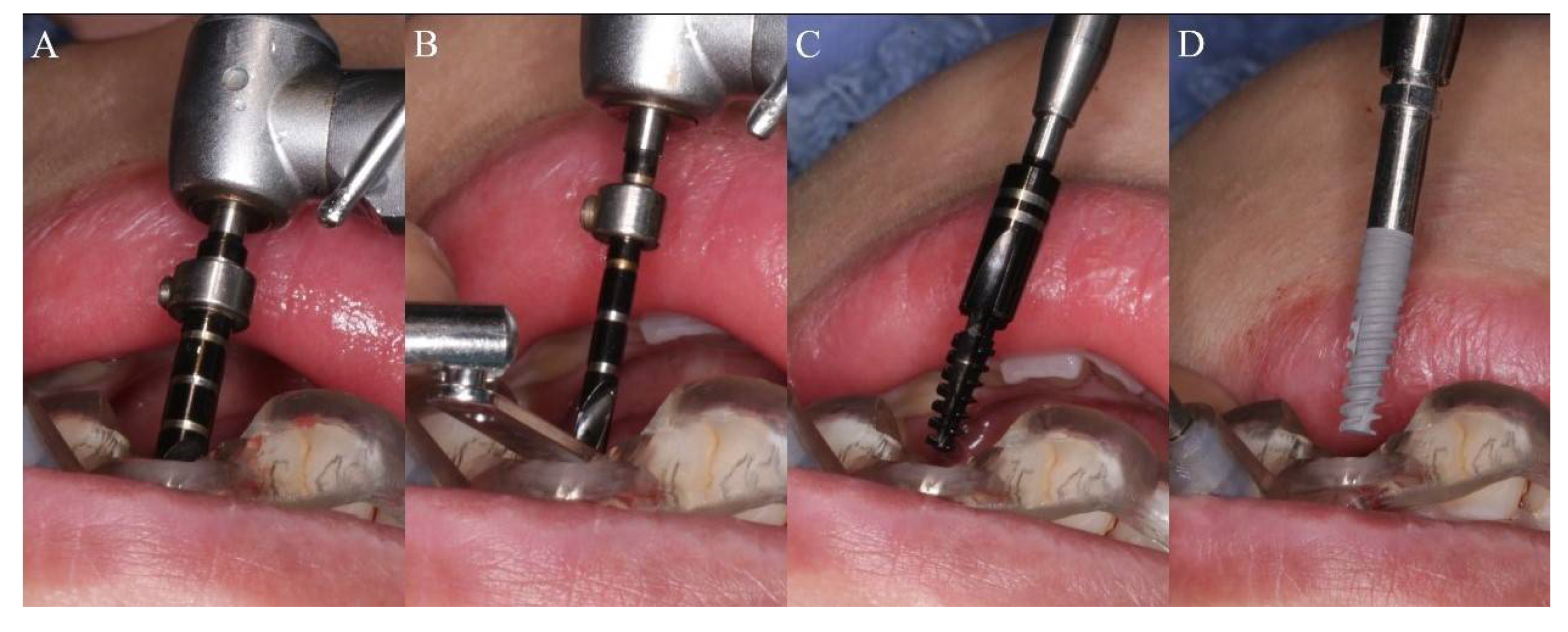
According to the surgical template and its effects on the accuracy of the surgical protocols, template guided surgery could principally be differentiated into fully guided and pilot-drill-guided protocols [
10]. Fully guided surgery is facilitated with a particular drill kit, inserting different drills through guiding sleeves in the template step by step, until the final insertion of the implant fixture. A pilot-drill-guided protocol is performed with a universal guide kit. After the pilot drill with the assistance of the template, with or without a drill stop ring, the template is removed, and subsequent drilling is performed by free-hand. Extensive research has shown that, compared with pilot-drill-guided surgery, fully guided protocol can better control the linear and angular deviations, and enables more accurate implant placement [
10,
13,
16,
17]. Nowadays, fully guided surgical templates are widely used in various surgeries for the purpose of improving surgical precision and safety. To date, however, most relevant research mainly focuses on the edentulous jaw and posterior zone [
17,
18,
19]; there have been very few discussions on the accuracy of anterior implant placement with fully guided surgery, and further verifications are still needed.
There are various factors that affect the accuracy of the guided template. In the entire process of computer-assisted, template-guided implant surgery, from preoperative data collection, data overlap, guided template production, to the operation, multiple links may have impact on the accuracy of implantation. The accumulation of a little error in each link will eventually lead to the significant positional deviation of the implant [
20]. Several studies have pointed out that bone density has a certain influence on the angle of implant placement. Lower bone density may cause greater implant angular deviation [
21]. In terms of bone density, the maxillary bone density is generally lower than that of the mandible. Yet, when a fully guided template is utilized, whether or not the disparities would still exist, leads to higher deviations in the maxillary guided surgery, or bias may be reduced due to its higher transferring accuracy. Further research on this would be valuable.
In order to reduce surgical interventions and shorten the treatment period [
22,
23,
24], immediate implantations are often applied in the anterior zone. Unlike the preparation of conventional implantation, in the implant site preparation after tooth extraction, the drill often drifts labially due to the resistance of the lingual bone wall of the extraction socket, which cause deviations in the final implant position.
To reduce the adverse impact of conventional open flap surgery, given sufficient vertical height, width and bone density of the alveolar ridge as well as adequate width and thickness of keratinized gingiva, fully guided flapless protocol can be conducted in the anterior zone. Schnutenhaus et al. [
25] found no statistical significance of the effect on implantation accuracy between open flap and flapless techniques. Behneke et al. [
26] pointed out that the implant position is shallow when the flap is not elevated. Hence, more studies related to discrepancies of the implant placement in the anterior zone with or without open flap techniques with tooth-borne surgical template need to be initiated.
In this study, a digital method is adopted to measure the transferring accuracy of the surgical template in the anterior zone. We can also clarify the influence among the arch difference, timing of implant placement and surgical techniques by comparing the accuracy of the fully guided template between the maxilla and mandible groups, immediate and delayed implantation groups, open flap and flapless technique groups. It aims to provide a theoretical basis and practical guidance for the application of the fully guided implantation.
4. Discussion
Limited by special anatomical locations and some exogenous factors, implantation in the anterior zone is frequently confronted with insufficient bone volume. Compared to posterior area, the available bone width in the anterior zone is thinner. In domestic and abroad investigations, the average thickness of the labial plate in the anterior zone is about 0.7–1.0 m [
27,
28,
29,
30]. With the loss of teeth, the labial bundle bone absorbs due to the lack of internal blood supply from periodontal ligament. Thus, the width of the alveolar bone will be further reduced. According to the research of Schropp et al. [
31], the alveolar bone width can be absorbed up to 50% within one year after tooth extraction. Fan Shengzi et al. [
32] measured the alveolar bone width of the anterior teeth after tooth loss, the results of which showed that after losing teeth for six month, the average bone width 4 mm below the top of the alveolar crest was only 4.10 ± 1.56 mm. One year after the loss, the average bone width was 3.28 ± 0.47 mm.
Performing operations under such limited bone volume conditions, the accuracy of implantation is particularly crucial. A few deviations may induce a series of undesirable consequences. When the implant is placed labially, the implant screw thread may be exposed due to the loss of the labial plate. In that way, additional bone augmentation is required to restore the missing bone during the surgery, which increases the difficulty and complexity of the operation as well as the implant treatment period. In the later stage of restoration, excessively labial inclination may result in later gingival recession, which will compromise the esthetics of the final restoration. When the implant is placed lingually, at the position of the central incisor in maxilla, it may enter into the incisive canal and damage the nasopalatine nerve, inducing paresthesia in the adjacent palatal mucosa. In mandible, the implant may puncture the lingual plate and damage the blood vessels, leading to life-threatening hemorrhage and hematoma [
33,
34]. Besides, the risk of implant osseointegration failure is increased. In the later stage of restoration, the labial protrusion of the crown is too large for daily oral hygiene maintenance. Whereas the cingulum of the crown is too thick to be comfortable. When the implant is placed mesially or distally, it may hurt adjacent natural teeth. When the distance between the implant and the natural tooth is less than 1.5 mm, the recession of the gingival papilla occurs and will detract the esthetics of the final restoration.
Through computer-assisted, template-guided implant surgery, patients’ information of hard and soft tissues can be visualized in the digital software before the operation. Follow the prosthetic-oriented principle to plan the optimal implant site and keep away from the adjacent anatomical structures. In addition, Koichiro, et al. revealed that the optimal implant position can also be determined through biomechanical considerations coming from stress analysis [
35]. Under the guidance of the fully guided template, the optimal three-dimensional position of the implant can come true in the anterior zone. The application of the template ensures a high positional precision, and effectively utilizes the available bone volume and reduces unnecessary bone loss. At the same time, it makes the operation more minimally invasive, increases the patients’ comfort and shortens the surgical time.
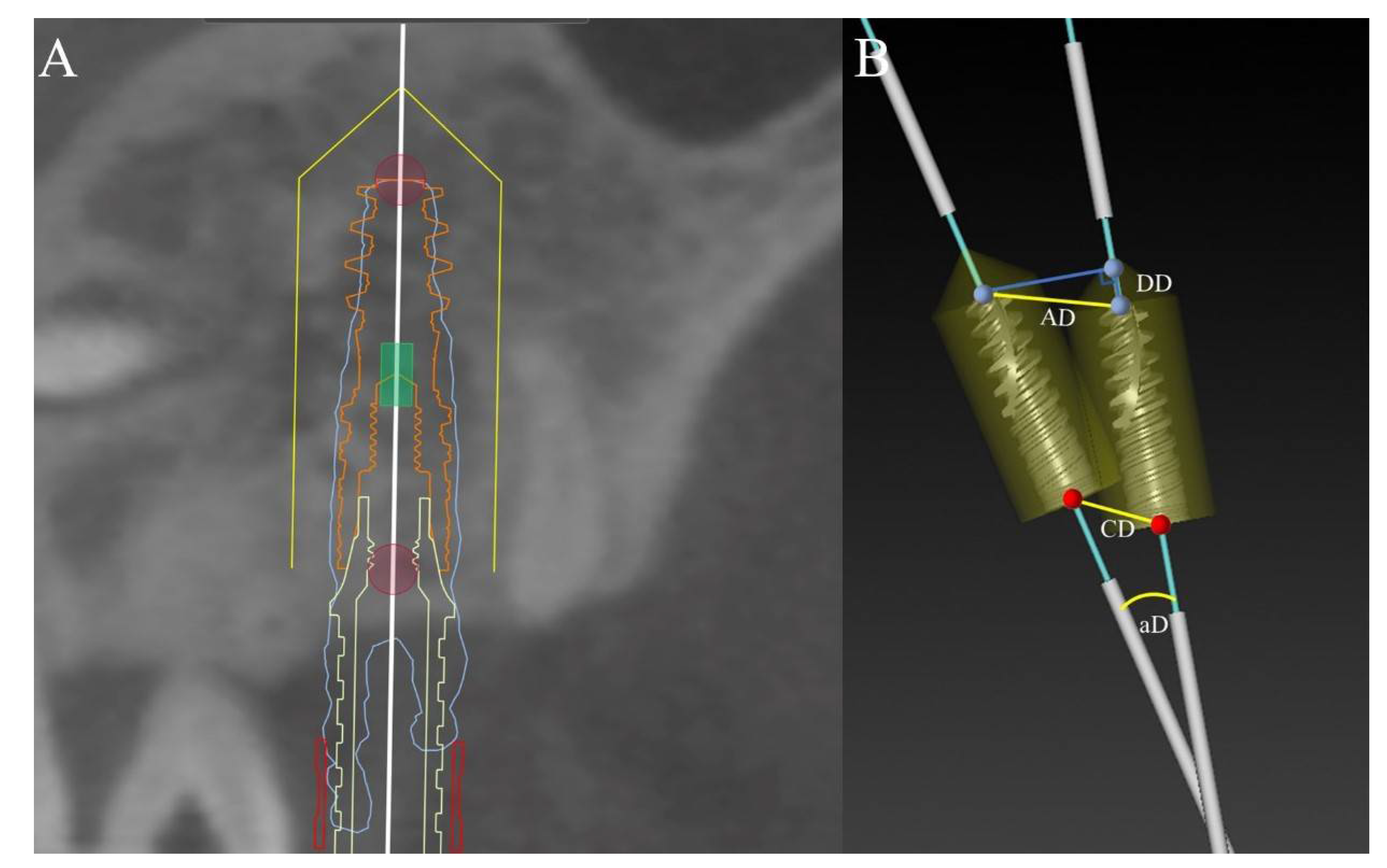
In this study, the apical, coronal, depth and angular deviations between the actual implant position and the planned position was 1.13 ± 0.39 mm, 0.86 ± 0.33 mm, 0.41 ± 0.66 mm and 3.32 ± 1.65° on average. These results are consistent with the findings of Dreiseidler, Van de Wiele, D’Haese. Dreiseidler et al. [
36] carried out an in vitro experiment with a total of 108 implants were inserted in partially edentulous models. The average deviations at shoulder level and apex level were 0.89 ± 0.44 mm and 1.09 ± 0.69 mm, respectively. Van de Wiele [
37] and D’Haese [
38] measured 75 and 77 implants placed in edentulous patients. The mean coronal deviations were 0.88 ± 0.50 mm and 0.91 ± 0.44 mm, and the mean apical deviations corresponded to 1.10 ± 0.53 mm and 1.13 ± 0.52 mm.
In some other reports, the average deviations of the fully guided template at the shoulder and apex can be as low as 0.32 ± 0.23 mm, 0.49 ± 0.29 mm [
39], and as high as 1.96 ± 0.23 mm, 2.29 ± 0.27 mm [
40]. One of the reasons for the inconsistency of these results may be the divergence in research models. Generally, in the case of in vitro experiments and cadaveric studies, better visibility makes the operation easier. However, in clinical situations, clinicians are usually faced with more complicated oral conditions, which may affect the final accuracy. On the other hand, different measurement methods will also contribute to different outcomes. For example, some researchers measured the linear distance of the apical and coronal center between the virtual planned implant and the actual implant. While others measure the horizontal distance between the two implants at shoulder level and apex level. So far, there is no standardized index to measure the accuracy of implant placement. Diverse methods come to disparate results, which makes different studies less comparable.
Although there are certain differences in the transferring accuracy of the fully guided template among different research studies, more and more studies believe that the overall accuracy of the fully guided surgery is better than that of the pilot-drill-guided and free-hand surgery. A retrospective study by Cassetta et al. [
13] pointed out that the fully guided template can provide better accuracy at shoulder level and depth than the pilot-drill-guided. At the 4th EAO Consensus Conference, the point of view that fully guided surgery has higher accuracy has been repeatedly raised [
41]. Furthermore, recently, Fernando et al. [
16] conducted a systematic review of computer-guided surgery and compared the accuracy of the pilot-drill-guided template and the fully guided template. The coronal, apical, depth and angular deviations of the full-course guide were 1.00 ± 0.08 mm, 1.23 ± 0.10 mm, 0.62 ± 0.08 mm, 3.13 ± 0.23°, which are similar to the results of this study. In contrast, the deviation of the half-course guide at each position has been increased, corresponding to 1.44 ± 0.18 mm, 1.91 ± 0.23 mm, 0.83 ± 0.23 mm, 4.30 ± 0.73°. The transferring accuracy of pilot-drill-guided template is worse than the fully guided template.
There is still some controversy about the influence of the implant site, that is, the maxilla and mandible on the accuracy of fully guided implantation. Some researchers argued that the accuracy of the maxillary guided template is higher than the mandibular one. For example, Lin [
42] and Behneke [
26] showed that the deviations at apex level of the mandibular guided template are significantly lower than those of the maxillary one, while Vasak et al. [
43] thought that the difference is mainly manifested at shoulder level. Christache et al. [
44] revealed that the coronal, apical and depth deviations of the mandibular guided implantation are smaller than those of the maxillary implantation. In this regard, the researchers analyzing the reasons for the difference may be related to the bone density of the jaw. The bone density of the upper jaw is lower than that of the lower jaw. The drill faced with less resistance is easier to deviate during preparation and implantation [
39]. However, some scholars hold different opinions. Valent [
3] and Erosy [
45] showed that the accuracy of the mandibular guided template is higher than that of the maxillary one, because the upper jaw provides a large-scale support to the guided template to obtain good stability [
46]. Zhou et al. [
47] conducted a systematic review of the factors that affect the accuracy of guided surgery, and analyzed that the maxillary and mandibular guided operations have no significant difference in the linear deviations, but the angular deviation. In our study, except that the depth deviation in maxilla group was slightly higher than that in mandible group, and the differences in the other three deviations were not statistically significant.
Analyze the possible reasons. First, tooth-supported template with retention of guided anchor pin determines good stability in the upper and lower jaws. The second is that the anterior zone supplies strong operability on better vision, easy operation, less interference from factors such as mouth opening, which is different from the posterior tooth area. Third, the entire surgical process from initial positioning to final implant placement is assisted by the guided template, which relatively weakens the interference of some unfavorable factors such as jaw bone density. Therefore, the accuracy appeared to be unaffected by the arch type and the bone density. The significant difference on depth deviation in this study may be caused by the surgeon’s habit of using a torque wrench to deepen one or two screw threads of the implant after the guided template is removed from the upper jaw.
Unlike conventional implantation, immediate implantation is to do the implant site preparation in the empty extraction socket. During the preparation process, the resistance from lingual side is greater than that from buccal side due to the existence of the lingual bone wall, so the drill easily deviates to the buccal side, which affects the accuracy of the implantation. Although the implant can be placed in a more optimal position under the guidance of the guided template, the drill may still slip and drift during preparation. Because it is impossible to restrict the drill in whole length due to the limited height of the guide sleeve, and there are tolerances between the guide sleeve and the drill. In this study, the accuracy of immediate implantation is similar to that of delayed implantation. And in terms of apical and angular deviations, immediate implantation group appeared higher precision, which is accordant to the results of Alzoubi et al. [
48], who compared the deviations in the three directions of shoulder level, apex level and angulation. Into the immediate implantation cases discrepancies of shoulder level, apex level and angulation were observed as 0.85 mm, 1.10 mm and 3.49°, respectively, while delayed implantation group corresponds to 0.88 mm, 1.59 mm and 4.29°, which are lower than the former group. It can be observed that by removing the resistance of the lingual bone wall in advance, and cooperating with the fully guided template, immediate implantation and conventional implantation can achieve similar accuracy. In this study, the average implant depth of the immediate implantation group was slightly deeper than that of the conventional implant group. The possible reason was that in this research group immediate load was usually performed during the operation, which required axial adjustment of the implant according to the corresponding marking points on the guided template, so that the temporary prosthesis could be accurately positioned, and the implant depth was deepened during this process.
Conventional implant surgery needs to elevate flaps, expose the implant site, and suture to seal the wounds, which have been obtained satisfactory healing and restoration. However, the open flap will reduce the blood supply of the periosteum, leading to the loss of alveolar bone mass, and postoperative bleeding, increasing the risk of infection and gingival recession [
49]. The flapless implant surgery assisted by surgical template can prevent from the adverse effects of conventional implant surgery, that is, reducing the patient’s swelling and pain, intraoperative bleeding and operation time, without sutures, and preserving the soft and hard tissues of the implant site as well as maintaining blood supply so that patients can return to normal oral hygiene as soon as possible [
50]. However, flapless surgery is appropriate for sufficient vertical height, width and bone density of the alveolar bone, at least 3 mm attached gum and at least 50 mm extent of mouth opening [
51].
Among the 52 implants in this study, there was no statistically significant difference in the measurement indexes between the open flap technique group and the flapless technique group. This is consistent with the reports of Schnutenhaus et al. [
25] and Ersoy et al. [
45] Most of the parameters in the study of Behneke et al. [
26] did not differ significantly during surgery. The only significant difference (
p = 0.027) is that the implant position of the flapless technique group is shallower than the actual implant position of the open flap technique group. In our study, the average implant depth of the flapless technique group was slightly shallower than that of the open flap technique group, but the difference was not statistically significant. A systematic review by Tahmaseb et al. [
52] pointed out that in clinical studies, the accuracy of open flap technique group is much lower than that of flapless technique group, because most open flap are performed under the guidance of bone-borne templates. Van Assche [
16] conducted a meta-analysis and found that bone-borne templates affect the accuracy of digital guided surgical. However, the angular and apical deviations of the tooth-borne guided template are significantly smaller than the mucosa-borne and bone-borne methods [
20]. It can be indicated that under the guidance of the tooth-borne, fully guided template, the surgical method does not affect the accuracy of implant placement.
Studies have shown that compared to the surgical stage, more deviations are related with the preoperative stage [
39]. In the process of preoperative data collection, although CBCT is currently a relatively reliable imaging method, factors such as metal restorations in the mouth and shaking of the patient during the shooting process may cause the final image to be distorted and inaccurate, which results in bias in the overlap and evaluation of the data [
53,
54]. In the process of oral scanning to collect information in the patient’s mouth, blood, saliva, the size of the scanning head, and improper operation methods may cause deviations in the final data [
55,
56]. In addition, the accuracy of the optical scanner and the digital design software will also affect the final precision [
57,
58]. At the stage of implant surgery, there is a certain tolerance between the guide sleeve and the drill. When the drill is drilling, there may be a certain extent of movement between them, which allows the preparation direction of the implant somewhat changed. Some scholars believe that by reducing the height from bottom of the guide sleeve to the bone surface and increasing the length of guide sleeve, the deviation can be reduced, and the accuracy can be improved [
59,
60]. The NobelGuide
® fully guided template and the matching kit used in this study have certain tolerances, although it can allow the surgeon to better perceive the implant placement, it may also have a certain impact on the accuracy of implant placement. Furthermore, in a recent study, Cassetta et al. [
61] found that the experience of the surgeon had almost no effect on the guided surgery.
This study merely focused on the transferring accuracy of the NobelGuide® templates in the anterior zone, and lacked the comparison of other systems, the conclusions of which had certain one-sidedness and limitations, and was unable to encompass the results of entire guided templates. Furthermore, as a retrospective cohort study, it only reported 40 patients, a total of 52 implants, the sample size of which was too insufficient to provide a strong evidence-based argument. Therefore, relevant randomized controlled trials and large numbers of samples are urgently needed to give further verifications of the findings.