Single Amino Acid Substitutions Surrounding the Icosahedral Fivefold Symmetry Axis Are Critical for Alternative Receptor Usage of Foot-and-Mouth Disease Virus
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cell Lines, Viruses and Plasmids
2.2. Site-Directed Mutagenesis and Transfection
2.3. Propagation of Virus Progeny and Sequencing of the Capsid-Coding Regions
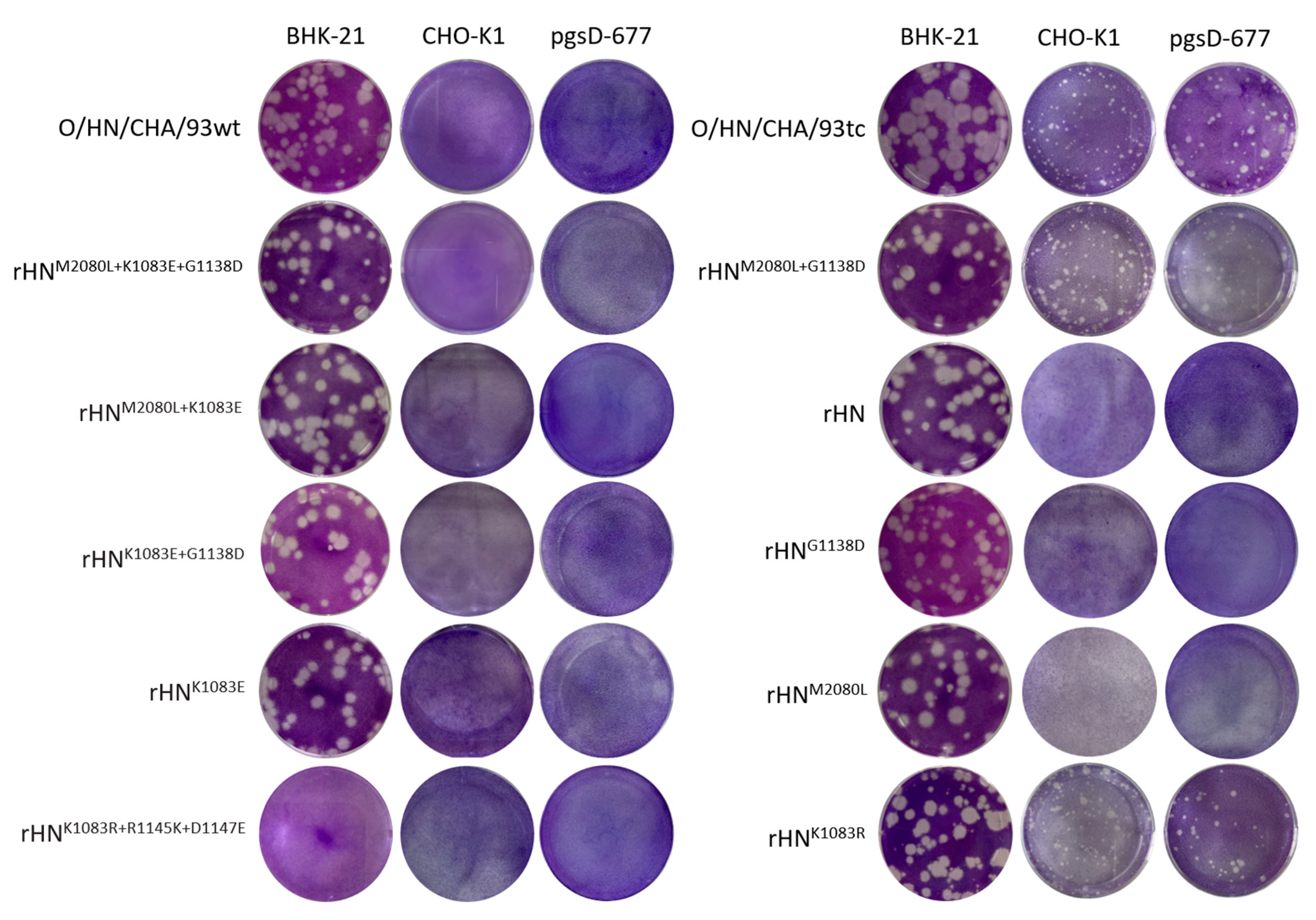
2.4. Plaque Assays
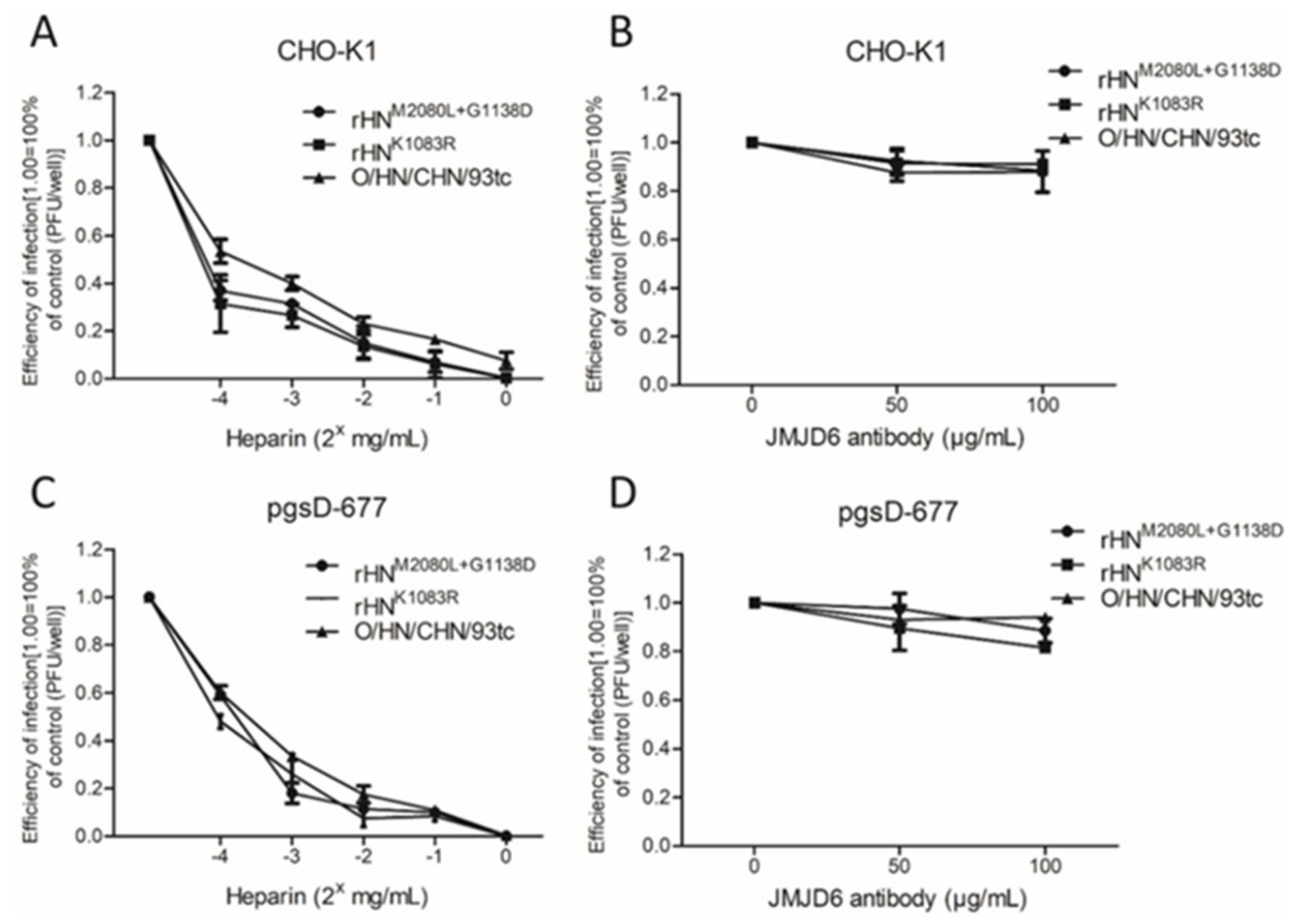
2.5. Plaque Reduction Assays
2.6. Confocal Microscopy
3. Results
3.1. E83K in VP1 is Responsible for the Alteration in Cellular Receptor Recognition of O/HN/CHA/93tc to Establish an Efficient Infection in Integrin-Negative CHO Cell Lines
3.2. L80 in VP2 is Involved in the Occurrence of E83K in VP1 during the Adaptation of O/HN/CHA/93wt to BHK-21 Cells
3.3. Both L80M in VP2 and D138G in VP1 Are Detrimental for the Infection of rHN in Two CHO Cell Lines
3.4. K83R in VP1 of rHN Plays a Functional Role to Expand Virus Tropism to Cell Types
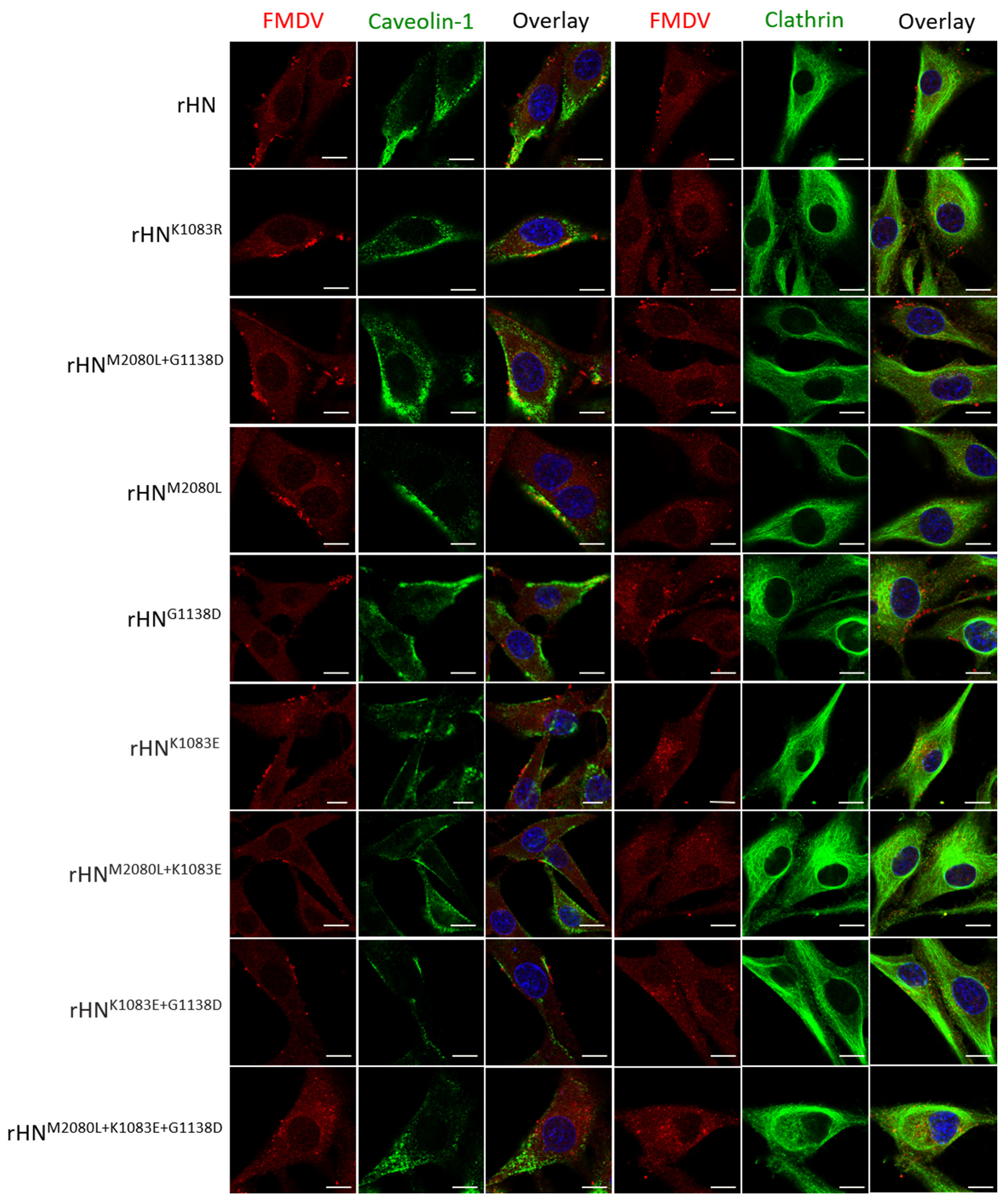
3.5. The Site-Directed Mutants of rHN with a High Affinity for Heparin Allow Caveolin-Mediated Endocytosis in Cultured Cells
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Knight-Jones, T.J.D.; Robinson, L.; Charleston, B.; Rodriguez, L.L.; Gay, C.; Sumption, K.J.; Vosloo, W. Global foot-and-mouth disease research update and gap analysis: Epidemiology, wildlife and economics. Transbound. Emerg. Dis. 2016, 63, 14–29. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, D.; Perrings, C. Foot and mouth disease: The risks of the international trade in live animals. Rev. Sci. Tech. l’OIE 2017, 36, 839–865. [Google Scholar] [CrossRef] [PubMed]
- Freimanis, G.; Di Nardo, A.; Bankowska, K.; King, D.; Wadsworth, J.; Knowles, N.; King, D. Genomics and outbreaks: Foot and mouth disease. Rev. Sci. Tech. l’OIE 2016, 35, 175–189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brito, B.P.; Rodriguez, L.L.; Hammond, J.M.; Pinto, J.; Perez, A.M. Review of the global distribution of foot-and-mouth disease virus from 2007 to 2014. Transbound. Emerg. Dis. 2015, 64, 316–332. [Google Scholar] [CrossRef]
- Martinez-Salas, E.; Belsham, G.J. Genome organization, translation and replication of foot-and-mouth disease virus RNA. In Foot-and-Mouth Disease Virus: Current Research and Emerging Trends; Sobrino, F., Domingo, E., Eds.; Caister Academic Press: Norfolk, UK, 2017. [Google Scholar]
- Herod, M.R.; Gold, S.; Lasecka-Dykes, L.; Wright, C.; Ward, J.C.; McLean, T.C.; Forrest, S.; Jackson, T.; Tuthill, T.J.; Rowlands, D.J.; et al. Genetic economy in picornaviruses: Foot-and-mouth disease virus replication exploits alternative precursor cleavage pathways. PLoS Pathog. 2017, 13, e1006666. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, P.; Liu, Y.; Ma, H.-C.; Paul, A.V.; Wimmer, E. Picornavirus morphogenesis. Microbiol. Mol. Biol. Rev. 2014, 78, 418–437. [Google Scholar] [CrossRef] [Green Version]
- Ruiz-Saenz, J.; Goez, Y.; Tabares, W.; López-Herrera, A. Cellular receptors for foot and mouth disease virus. Intervirology 2009, 52, 201–212. [Google Scholar] [CrossRef]
- Berinstein, A.; Roivainen, M.; Hovi, T.; Mason, P.W.; Baxt, B. Antibodies to the vitronectin receptor (integrin alpha V beta 3) inhibit binding and infection of foot-and-mouth disease virus to cultured cells. J. Virol. 1995, 69, 2664–2666. [Google Scholar] [CrossRef] [Green Version]
- Jackson, T.; Sheppard, D.; Denyer, M.; Blakemore, W.; King, A.M. The epithelial integrin alphavbeta6 is a receptor for foot-and-mouth disease virus. J. Virol. 2000, 74, 4949–4956. [Google Scholar] [CrossRef]
- Jackson, T.; Mould, A.P.; Sheppard, D.; King, A.M. Integrin alphavbeta1 is a receptor for foot-and-mouth disease virus. J. Virol. 2002, 76, 935–941. [Google Scholar] [CrossRef] [Green Version]
- Jackson, T.; Clark, S.; Berryman, S.; Burman, A.; Cambier, S.; Mu, D.; Nishimura, S.; King, A.M. Integrin alphavbeta8 functions as a receptor for foot-and-mouth disease virus: Role of the beta-chain cytodomain in integrin-mediated infection. J. Virol. 2004, 78, 4533–4540. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Donnell, V.; Larocco, M.; Duque, H.; Baxt, B. Analysis of foot-and-mouth disease virus internalization events in cultured cells. J. Virol. 2005, 79, 8506–8518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berryman, S.; Clark, S.; Monaghan, P.; Jackson, T. Early events in integrin alphavbeta6-mediated cell entry of foot-and-mouth disease virus. J. Virol. 2005, 79, 8519–8534. [Google Scholar] [CrossRef] [Green Version]
- Martín-Acebes, M.A.; González-Magaldi, M.; Sandvig, K.; Sobrino, F.; Armas-Portela, R. Productive entry of type C foot-and-mouth disease virus into susceptible cultured cells requires clathrin and is dependent on the presence of plasma membrane cholesterol. Virology 2007, 369, 105–118. [Google Scholar] [CrossRef] [Green Version]
- Neff, S.; Sá-Carvalho, D.; Rieder, E.; Mason, P.W.; Blystone, S.D.; Brown, E.J.; Baxt, B. Foot-and-mouth disease virus virulent for cattle utilizes the integrin αvβ3 as its receptor. J. Virol. 1998, 72, 3587–3594. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jackson, T.; Ellard, F.M.; Ghazaleh, R.A.; Brookes, S.M.; Blakemore, W.E.; Corteyn, A.H.; Stuart, D.I.; Newman, J.W.; King, A.M. Efficient infection of cells in culture by type O foot-and-mouth disease virus requires binding to cell surface heparan sulfate. J. Virol. 1996, 70, 5282–5287. [Google Scholar] [CrossRef] [Green Version]
- O׳donnell, V.; Larocco, M.; Baxt, B. Heparan sulfate-binding foot-and-mouth disease virus enters cells via caveola-mediated endocytosis. J. Virol. 2008, 82, 9075–9085. [Google Scholar] [CrossRef] [Green Version]
- Lawrence, P.; Rai, D.; Conderino, J.S.; Uddowla, S.; Rieder, E. Role of Jumonji C-domain containing protein 6 (JMJD6) in infectivity of foot-and-mouth disease virus. Virology 2016, 492, 38–52. [Google Scholar] [CrossRef]
- Lawrence, P.; Pacheco, J.M.; Stenfeldt, C.; Arzt, J.; Rai, D.K.; Rieder, E. Pathogenesis and micro-anatomic characterization of a cell-adapted mutant foot-and-mouth disease virus in cattle: Impact of the Jumonji C-domain containing protein 6 (JMJD6) and route of inoculation. Virology 2016, 492, 108–117. [Google Scholar] [CrossRef]
- Mason, P.W.; Rieder, E.; Baxt, B. RGD sequence of foot-and-mouth disease virus is essential for infecting cells via the natural receptor but can be bypassed by an antibody-dependent enhancement pathway. Proc. Natl. Acad. Sci. USA 1994, 91, 1932–1936. [Google Scholar] [CrossRef] [Green Version]
- Baxt, B.; Mason, P.W. Foot-and-mouth disease virus undergoes restricted replication in macrophage cell cultures following fc receptor-mediated adsorption. Virology 1995, 207, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Mason, P.; Berinstein, A.; Baxt, B.; Parsells, R.; Kang, A.; Rieder, E. Cloning and expression of a single-chain antibody fragment specific for foot-and-mouth disease virus. Virology 1996, 224, 548–554. [Google Scholar] [CrossRef] [Green Version]
- Rieder, E.; Berinstein, A.; Baxt, B.; Kang, A.; Mason, P.W. Propagation of an attenuated virus by design: Engineering a novel receptor for a noninfectious foot-and-mouth disease virus. Proc. Natl. Acad. Sci. USA 1996, 93, 10428–10433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Han, S.-C.; Guo, H.-C.; Sun, S.-Q.; Jin, Y.; Wei, Y.-Q.; Feng, X.; Yao, X.-P.; Cao, S.-Z.; Liu, D.X.; Liu, X.-T. Productive entry of foot-and-mouth disease virus via macropinocytosis independent of phosphatidylinositol 3-kinase. Sci. Rep. 2016, 6, srep19294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fry, E.E.; Lea, S.M.; Jackson, T.; Newman, J.W.; Ellard, F.M.; Blakemore, W.E.; Abu-Ghazaleh, R.; Samuel, A.; King, A.M.; Stuart, D.I. The structure and function of a foot-and-mouth disease virus-oligosaccharide receptor complex. EMBO J. 1999, 18, 543–554. [Google Scholar] [CrossRef] [Green Version]
- Fry, E.E.; Newman, J.W.I.; Curry, S.; Najjam, S.; Jackson, T.; Blakemore, W.; Lea, S.M.; Miller, L.; Burman, A.; King, A.M.Q.; et al. Structure of foot-and-mouth disease virus serotype A1061 alone and complexed with oligosaccharide receptor: Receptor conservation in the face of antigenic variation. J. Gen. Virol. 2005, 86, 1909–1920. [Google Scholar] [CrossRef]
- Dill, V.; Eschbaumer, M. Cell culture propagation of foot-and-mouth disease virus: Adaptive amino acid substitutions in structural proteins and their functional implications. Virus Genes 2019, 56, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Sa-Carvalho, D.; Rieder, E.; Baxt, B.; Rodarte, R.; Tanuri, A.; Mason, P.W. Tissue culture adaptation of foot-and-mouth disease virus selects viruses that bind to heparin and are attenuated in cattle. J. Virol. 1997, 71, 5115–5123. [Google Scholar] [CrossRef] [Green Version]
- Borca, M.; Pacheco, J.M.; Holinka, L.G.; Carrillo, C.; Hartwig, E.J.; Garriga, D.; Kramer, E.; Rodriguez, L.; Piccone, M.E. Role of arginine-56 within the structural protein VP3 of foot-and-mouth disease virus (FMDV) O1 Campos in virus virulence. Virology 2012, 422, 37–45. [Google Scholar] [CrossRef] [Green Version]
- Bai, X.; Bao, H.; Li, P.; Wei, W.; Zhang, M.; Sun, P.; Cao, Y.; Lu, Z.; Fu, Y.; Xie, B.; et al. Effects of two amino acid substitutions in the capsid proteins on the interaction of two cell-adapted PanAsia-1 strains of foot-and-mouth disease virus serotype O with heparan sulfate receptor. Virol. J. 2014, 11, 132. [Google Scholar] [CrossRef]
- Bai, X.-W.; Bao, H.-F.; Li, P.-H.; Ma, X.-Q.; Sun, P.; Bai, Q.-F.; Zhang, M.; Yuan, H.; Chen, D.-D.; Li, K.; et al. Engineering responses to amino acid substitutions in the VP0-and VP3-coding regions of PanAsia-1 strains of foot-and-mouth disease virus serotype O. J. Virol. 2019, 93, e02278-18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cao, Y.-M.; Lu, Z.-J.; Sun, P.; Fu, Y.; Tian, F.; Hao, X.; Bao, H.-F.; Liu, X.-T.; Liu, Z. A pseudotype baculovirus expressing the capsid protein of foot-and-mouth disease virus and a T-Cell immunogen shows enhanced immunogenicity in mice. Virol. J. 2011, 8, 77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, P.-H.; Bai, X.-W.; Sun, P.; Li, D.; Lu, Z.-J.; Cao, Y.-M.; Fu, Y.-F.; Bao, H.-F.; Chen, Y.-L.; Xie, B.-X.; et al. Evaluation of a genetically modified foot-and-mouth disease virus vaccine candidate generated by reverse genetics. BMC Veter. Res. 2012, 8, 57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cao, W.; Li, P.; Bai, X.; Lu, Z.; Sun, P.; Liu, Z. Rescue and identification of virus activity of foot-and-mouth disease virus strain O/HN/93 from full length cDNA clone. Acta Agric. Boreali-Sinica 2010, 25, 32–37. [Google Scholar]
- Knowles, N.; Samuel, A.R.; Davies, P.R.; Midgley, R.J.; Valarcher, J.-F. Pandemic strain of foot-and-mouth disease virus serotype O. Emerg. Infect. Dis. 2005, 11, 1887–1893. [Google Scholar] [CrossRef]
- Bai, X.; Bao, H.; Li, P.; Sun, P.; Kuang, W.; Cao, Y.; Lu, Z.; Liu, Z.; Liu, X. Genetic characterization of the cell-adapted PanAsia strain of foot-and-mouth disease virus O/Fujian/CHA/5/99 isolated from swine. Virol. J. 2010, 7, 208. [Google Scholar] [CrossRef] [Green Version]
- Lawrence, P.; Larocco, M.; Baxt, B.; Rieder, E. Examination of soluble integrin resistant mutants of foot-and-mouth disease virus. Virol. J. 2013, 10, 2. [Google Scholar] [CrossRef] [Green Version]
- Núñez, J.I.; Molina, N.; Baranowski, E.; Domingo, E.; Clark, S.; Burman, A.; Berryman, S.; Jackson, T.; Sobrino, F. Guinea pig-adapted foot-and-mouth disease virus with altered receptor recognition can productively infect a natural host. J. Virol. 2007, 81, 8497–8506. [Google Scholar] [CrossRef] [Green Version]
- Logan, D.; Abu-Ghazaleh, R.; Blakemore, W.; Curry, S.; Jackson, T.; King, A.; Lea, S.; Lewis, R.; Newman, J.; Parry, N.; et al. Structure of a major immunogenic site on foot-and-mouth disease virus. Nat. Cell Biol. 1993, 362, 566–568. [Google Scholar] [CrossRef]
- Ruiz-Jarabo, C.M.; Sevilla, N.N.; Dávila, M.; Gómez-Mariano, G.; Baranowski, E.; Domingo, E. Antigenic properties and population stability of a foot-and-mouth disease virus with an altered Arg-Gly-Asp receptor-recognition motif. J. Gen. Virol. 1999, 80, 1899–1909. [Google Scholar] [CrossRef] [Green Version]
- Baranowski, E.; Ruiz-Jarabo, C.M.; Sevilla, N.; Andreu, D.; Beck, E.; Domingo, E. Cell recognition by foot-and-mouth disease virus that lacks the RGD integrin-binding motif: Flexibility in aphthovirus receptor usage. J. Virol. 2000, 74, 1641–1647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baranowski, E.; Ruiz-Jarabo, C.M.; Domingo, E. Evolution of cell recognition by viruses. Science 2001, 292, 1102–1105. [Google Scholar] [CrossRef] [PubMed]
- Li, P.-H.; Lu, Z.-J.; Bao, H.-F.; Li, D.; King, D.P.; Sun, P.; Bai, X.-W.; Cao, W.; Gubbins, S.; Chen, Y.-L.; et al. In-vitro and in-vivo phenotype of type Asia 1 foot-and-mouth disease viruses utilizing two non-RGD receptor recognition sites. BMC Microbiol. 2011, 11, 154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mateu, M.G. The foot-and-mouth disease virion: Structure and function. Foot Mouth Dis. Virus Curr. Res. Emerg. Trends 2017, 61–106. [Google Scholar] [CrossRef] [Green Version]
- Kotecha, A.; Seago, J.; Scott, K.; Burman, A.; Loureiro, S.; Ren, J.; Porta, C.; Ginn, H.M.; Jackson, T.; Pérez-Martin, E.; et al. Structure-based energetics of protein interfaces guides foot-and-mouth disease virus vaccine design. Nat. Struct. Mol. Biol. 2015, 22, 788–794. [Google Scholar] [CrossRef]
- Kotecha, A.; Wang, Q.; Dong, X.; Ilca, S.L.; Ondiviela, M.; Zihe, R.; Seago, J.; Charleston, B.; Fry, E.E.; Abrescia, N.G.A.; et al. Rules of engagement between alphavbeta6 integrin and foot-and-mouth disease virus. Nat. Commun. 2017, 8, 15408. [Google Scholar] [CrossRef]
- Duque, H.; Baxt, B. Foot-and-mouth disease virus receptors: Comparison of bovine αv integrin utilization by type A and O viruses. J. Virol. 2003, 77, 2500–2511. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Sun, Y.; Yang, F.; Guo, J.; He, J.; Wu, Q.; Cao, W.; Lv, L.; Zheng, H.; Zhang, Z. Induction of partial protection against foot and mouth disease virus in guinea pigs by neutralization with the integrin beta6-1 subunit. Viruses 2013, 5, 1114–1130. [Google Scholar] [CrossRef] [Green Version]
- Miller, L.C.; Blakemore, W.; Sheppard, D.; Atakilit, A.; King, A.M.; Jackson, T. Role of the cytoplasmic domain of the beta-subunit of integrin alpha(v)beta6 in infection by foot-and-mouth disease virus. J. Virol. 2001, 75, 4158–4164. [Google Scholar] [CrossRef] [Green Version]
- Xu, X.; Nagarajan, H.; Lewis, N.E.; Pan, S.; Cai, Z.; Liu, X.; Chen, W.; Xie, M.; Wang, W.; Hammond, S.; et al. The genomic sequence of the Chinese hamster ovary (CHO)-K1 cell line. Nat. Biotechnol. 2011, 29, 735–741. [Google Scholar] [CrossRef] [Green Version]
- Lawrence, P.; Rieder, E. Insights into Jumonji C-domain containing protein 6 (JMJD6): A multifactorial role in foot-and-mouth disease virus replication in cells. Virus Genes 2017, 53, 340–351. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.; Hwang, J.-H.; Kim, A.; Park, J.-H.; Lee, M.J.; Kim, B.; Kim, S.-M. Analysis of amino acid mutations of the foot-and-mouth disease virus serotype O using both heparan sulfate and JMJD6 receptors. Viruses 2020, 12, 1012. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.; Pacheco, J.M.; Mason, P.W. Evaluation of genetically engineered derivatives of a Chinese strain of foot-and-mouth disease virus reveals a novel cell-binding site which functions in cell culture and in animals. J. Virol. 2003, 77, 3269–3280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maree, F.; Blignaut, B.; De Beer, T.A.; Visser, N.; Rieder, E.A. Mapping of amino acid residues responsible for adhesion of cell culture-adapted foot-and-mouth disease SAT type viruses. Virus Res. 2010, 153, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Dill, V.; Hoffmann, B.; Zimmer, A.; Beer, M.; Eschbaumer, M. Influence of cell type and cell culture media on the propagation of foot-and-mouth disease virus with regard to vaccine quality. Virol. J. 2018, 15, 46. [Google Scholar] [CrossRef] [PubMed]
- International Office of Epizooties. Outerbreaks during preceding months. OIE Bull. 1990, 102, 721–732. [Google Scholar]
- Li, P.; Lu, Z.; Bai, X.; Li, D.; Sun, P.; Bao, H.; Fu, Y.; Cao, Y.; Chen, Y.; Xie, B.; et al. Evaluation of a 3A-truncated foot-and-mouth disease virus in pigs for its potential as a marker vaccine. Veter. Res. 2014, 45, 51. [Google Scholar] [CrossRef] [Green Version]
- Yuan, H.; Li, P.; Bao, H.; Sun, P.; Bai, X.; Bai, Q.; Li, N.; Ma, X.; Cao, Y.; Fu, Y.; et al. Engineering viable foot-and-mouth disease viruses with increased acid stability facilitate the development of improved vaccines. Appl. Microbiol. Biotechnol. 2020, 104, 1683–1694. [Google Scholar] [CrossRef] [Green Version]
- Fu, Y.; Li, P.; Cao, Y.; Wang, N.; Sun, P.; Shi, Q.; Ji, X.; Bao, H.; Li, D.; Chen, Y.; et al. Development of a blocking ELISA using a monoclonal antibody to a dominant epitope in non-structural protein 3A of foot-and-mouth disease virus, as a matching test for a negative-marker vaccine. PLoS ONE 2017, 12, e0170560. [Google Scholar] [CrossRef]


| Genomic Region | Position b | Virus | ||
|---|---|---|---|---|
| O/HN/CHA/93wt | O/HN/CHA/93tc c | rHN d | ||
| S | (353) | (T) | (C) | (C) |
| (361) | (A) | (G) | (G) | |
| IRES | (1–5) | (A5) | (A5) | (A6) £ |
| (279) | (C) | (A/C) * | (C) | |
| Lpro | 24 | Arg (CGA) | Arg (CGA)/Gln (CAA) # | Arg (CGA) |
| 87 | Glu (GAA) | Glu (GAA)/Lys (AAA) # | Glu (GAA) | |
| 172 | Pro (CCA) | Pro (CCA) | Pro (CCG) | |
| 173 | Asp (GAC) | Asp (GAC) | Asp (GAT) | |
| VP2 | 80 | Leu (CTG) | Leu (CTG) | Met (ATG) |
| VP3 | 57 | Phe (TTC) | Phe (TTC/TTT) $ | Phe (TTC) |
| 138 | Ala (GCG) | Ala (GCG) | Ala (GCC) | |
| 153 | Asn (AAT) | Asn (AAT) | Asn (AAC) | |
| 201 | Val (GTG) | Val (GTG) | Val (GTT) | |
| VP1 | 83 | Glu (GAG) | Lys (AAG) | Lys (AAG) |
| 138 | Asp (GAC) | Asp (GAC) | Gly (GGC) | |
| 2B | 107 | Ile (ATC) | Ile (ATC) | Ile (ATA) |
| Virus a | Individual Amino Acid Residues b | Virus Titer (PFU/mL) c | Inhibition of Viral Infection in BHK-21 Cells d | ||||||
|---|---|---|---|---|---|---|---|---|---|
| VP2 | VP1 | BHK-21 | CHO-K1 | pgsD-677 | Heparin | VR-17 | |||
| 80 | 83–85 | 138 | 145–147 | ||||||
| * O/HN/CHN/93wt | L | EGD | D | RGD | 2.5 × 107 | <5 | <5 | 0.5 | 98 |
| # O/HN/CHN/93tc | L | KGD | D | RGD | 7.0 × 107 | 2.4 × 104 | 5.5 × 102 | 97 | 0.2 |
| rHN | M | KGD | G | RGD | 1.1 × 107 | <5 | <5 | 85 | 0.2 |
| rHNM2080L | L | KGD | G | RGD | 3.7 × 107 | <5 | <5 | 80 | 0.5 |
| rHNG1138D | M | KGD | D | RGD | 2.5 × 107 | <5 | <5 | 76 | 0.7 |
| # rHNM2080L+G1138D | L | KGD | D | RGD | 6.8 × 107 | 3.2 × 104 | 6.0 × 102 | 98 | 0.2 |
| rHNK1083E | M | EGD | G | RGD | 4.2 × 107 | <5 | <5 | 0.2 | 98 |
| rHNM2080L+K1083E | L | EGD | G | RGD | 1.8 × 107 | <5 | <5 | 0.4 | 86 |
| rHNK1083E+G1138D | M | EGD | D | RGD | 3.0 × 107 | <5 | <5 | 0.5 | 96 |
| * rHNM2080L+K1083E+G1138D | L | EGD | D | RGD | 5.2 × 107 | <5 | <5 | 0.3 | 96 |
| rHNK1083R | M | RGD | G | RGD | 5.0 × 107 | 1.5 × 103 | 1.2 × 102 | 95 | 0.4 |
| $ rHNK1083R+R1145K+D1147E | M | RGD | G | KGE | <5 | <5 | <5 | — | — |
| Virus | Original Mutation | Acquired Mutation b | No. of Passages | ||
|---|---|---|---|---|---|
| VP2 | VP1 | ||||
| rHN | — | — | — | NC | 20 |
| rHNM2080L | M80L | — | — | NC | 20 |
| rHNK1083E | — | K83E | — | NC | 20 |
| rHNK1083R | — | K83R | — | NC | 11 |
| rHNG1138D | — | — | G138D | NC | 20 |
| rHNM2080L+K1083E | M80L | K83E | — | E83K in VP1 | 8 |
| rHNM2080L+G1138D | M80L | — | G138D | NC | 20 |
| rHNK1083E+G1138D | — | K83E | G138D | NC | 20 |
| rHNM2080L+K1083E+G1138D | M80L | K83E | G138D | E83K in VP1 | 10 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gong, X.-H.; Bai, X.-W.; Li, P.-H.; Bao, H.-F.; Zhang, M.; Chen, Y.-L.; Sun, P.; Yuan, H.; Huang, L.; Ma, X.-Q.; et al. Single Amino Acid Substitutions Surrounding the Icosahedral Fivefold Symmetry Axis Are Critical for Alternative Receptor Usage of Foot-and-Mouth Disease Virus. Viruses 2020, 12, 1147. https://0-doi-org.brum.beds.ac.uk/10.3390/v12101147
Gong X-H, Bai X-W, Li P-H, Bao H-F, Zhang M, Chen Y-L, Sun P, Yuan H, Huang L, Ma X-Q, et al. Single Amino Acid Substitutions Surrounding the Icosahedral Fivefold Symmetry Axis Are Critical for Alternative Receptor Usage of Foot-and-Mouth Disease Virus. Viruses. 2020; 12(10):1147. https://0-doi-org.brum.beds.ac.uk/10.3390/v12101147
Chicago/Turabian StyleGong, Xiao-Hua, Xing-Wen Bai, Ping-Hua Li, Hui-Fang Bao, Meng Zhang, Ying-Li Chen, Pu Sun, Hong Yuan, Lei Huang, Xue-Qing Ma, and et al. 2020. "Single Amino Acid Substitutions Surrounding the Icosahedral Fivefold Symmetry Axis Are Critical for Alternative Receptor Usage of Foot-and-Mouth Disease Virus" Viruses 12, no. 10: 1147. https://0-doi-org.brum.beds.ac.uk/10.3390/v12101147




