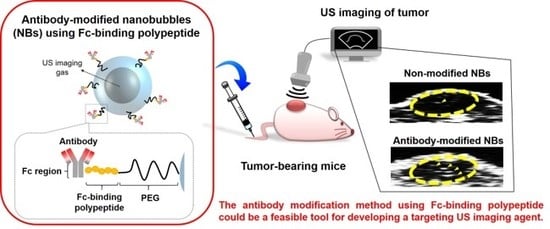
Development of Antibody-Modified Nanobubbles Using Fc-Region-Binding Polypeptides for Ultrasound Imaging
Abstract
:1. Introduction
2. Materials and Methods
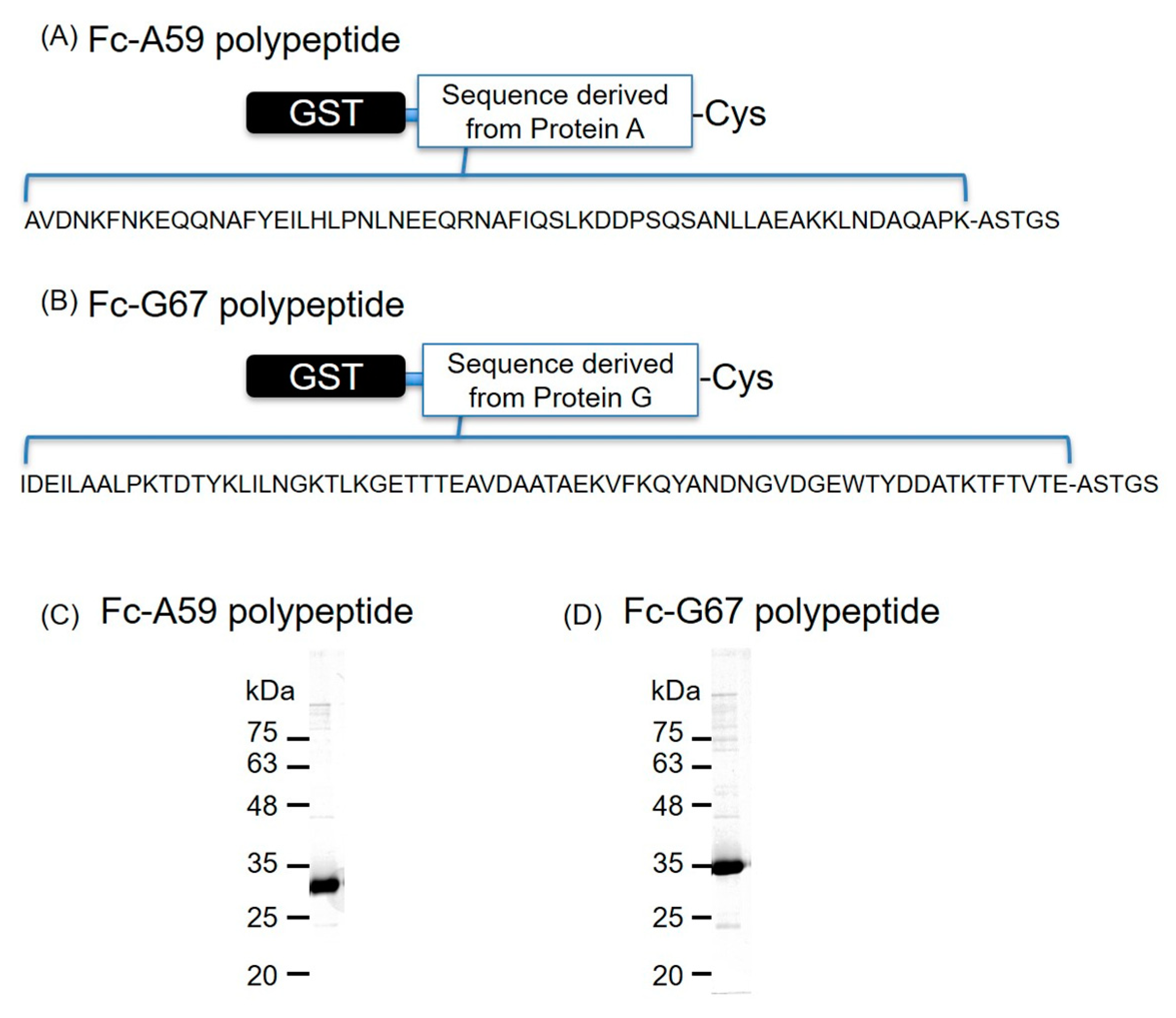
2.1. Production of Fc-Binding Polypeptides
2.2. Generation of an Antiserum for Mouse CD146 and 4D5-Fc Antibodies
2.3. Preparation of Antibody-Modified Liposomes and NBs
2.4. Cells and Tumor Model Mice
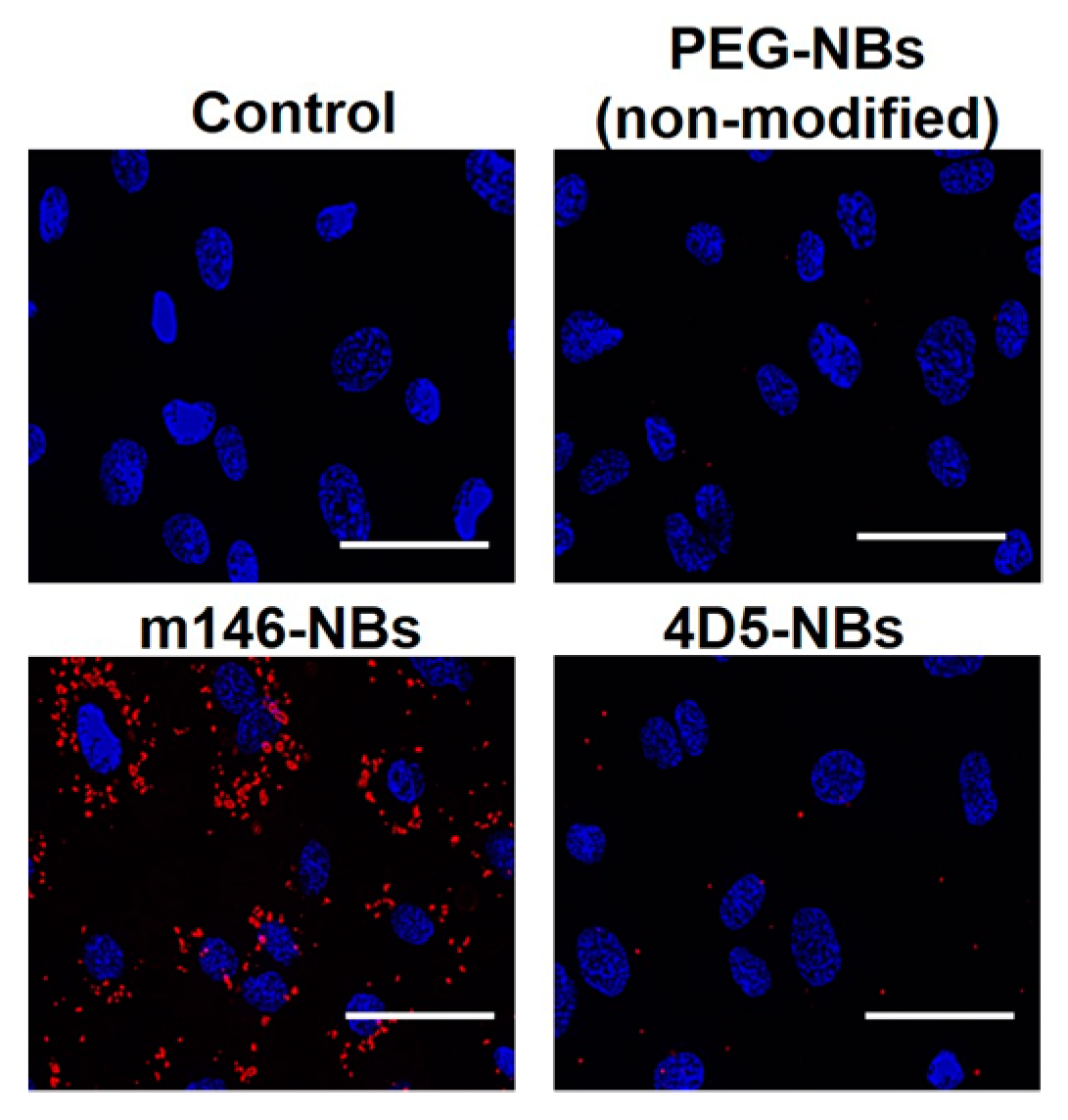
2.5. Fluorescent Microscopic Analysis
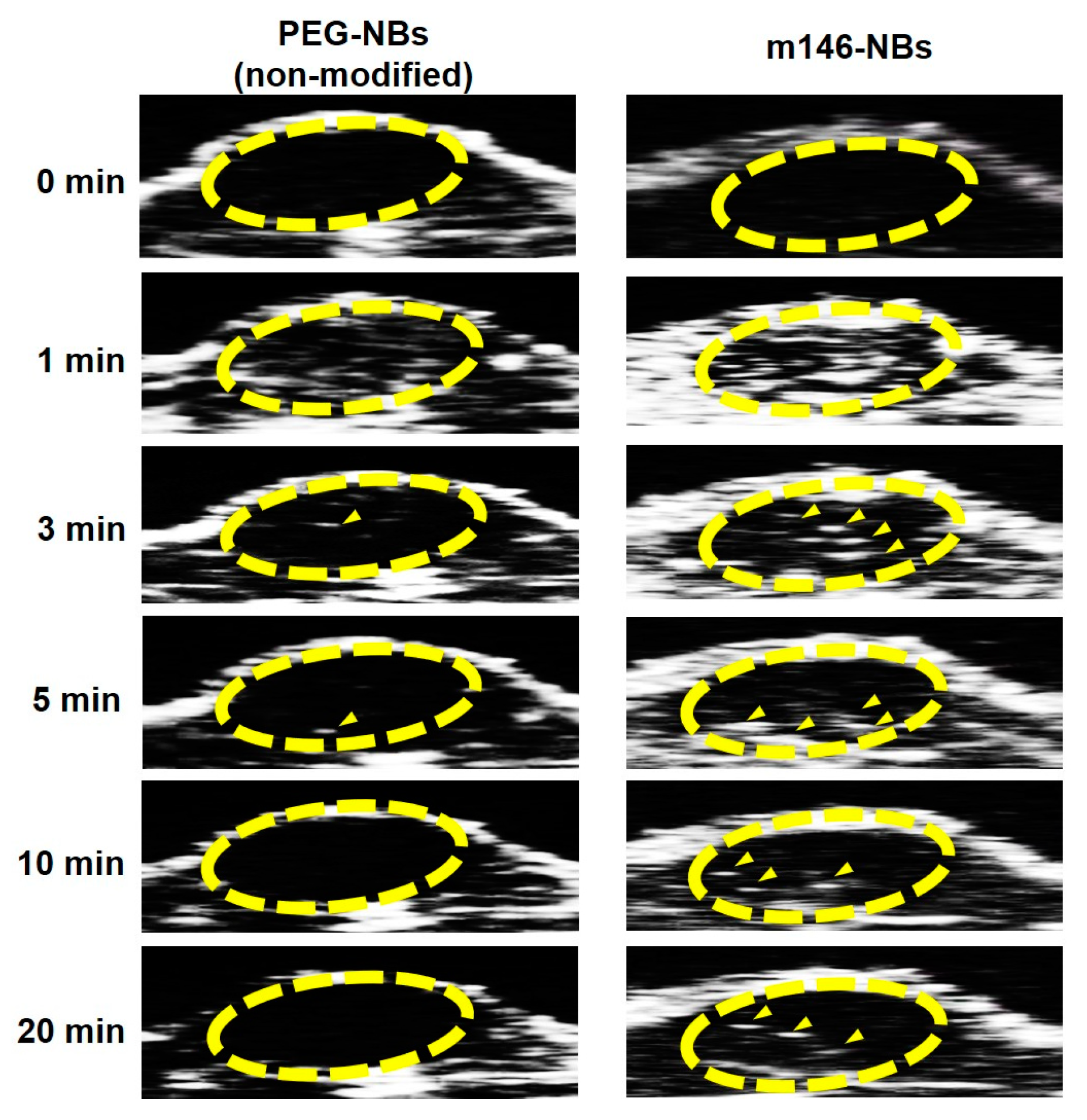
2.6. In Vivo US Imaging Analysis
3. Results and Discussion
3.1. Design and Purification of Fc-Binding Polypeptide
3.2. Characteristics of Antibody-Modified Liposomes/NBs using Fc-Binding Polypeptide
3.3. Specific Attachment of Anti-CD146 Antibody-Modified NBs
3.4. In Vivo US Imaging
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Willmann, J.K.; van Bruggen, N.; Dinkelborg, L.M.; Gambhir, S.S. Molecular imaging in drug development. Nat. Rev. Drug Discov. 2008, 7, 591–607. [Google Scholar] [CrossRef] [PubMed]
- Lindner, J.R. Microbubbles in medical imaging: current applications and future directions. Nat. Rev. Drug Discov. 2004, 3, 527–533. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.R.; Burns, P.N. Microbubble-enhanced US in Body Imaging: What Role? Radiology 2010, 257, 24–39. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, N.; Needles, A.; Willmann, J.K. Molecular ultrasound imaging: current status and future directions. Clin. Radiol. 2010, 65, 567–581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dănilă, M.; Popescu, A.; Sirli, R.; Sporea, I.; Martie, A.; Sendroiu, M. Contrast enhanced ultrasound (CEUS) in the evaluation of liver metastases. Med. Ultrason. 2010, 12, 233–237. [Google Scholar] [PubMed]
- Kim, T.K.; Noh, S.Y.; Wilson, S.R.; Kono, Y.; Piscaglia, F.; Jang, H.-J.; Lyshchik, A.; Dietrich, C.F.; Willmann, J.K.; Vezeridis, A.; et al. Contrast-enhanced ultrasound (CEUS) liver imaging reporting and data system (LI-RADS) 2017—A review of important differences compared to the CT/MRI system. Clin. Mol. Hepatol. 2017, 23, 280–289. [Google Scholar] [CrossRef]
- Fokong, S.; Theek, B.; Wu, Z.; Koczera, P.; Appold, L.; Jorge, S.; Resch-Genger, U.; van Zandvoort, M.; Storm, G.; Kiessling, F.; et al. Image-guided, targeted and triggered drug delivery to tumors using polymer-based microbubbles. J. Control. Release 2012, 163, 75–81. [Google Scholar] [CrossRef]
- Wu, W.; Feng, X.; Yuan, Y.; Liu, Y.; Li, M.; Bin, J.; Xiao, Y.; Liao, W.; Liao, Y.; Zhang, W.; et al. Comparison of Magnetic Microbubbles and Dual-modified Microbubbles Targeted to P-selectin for Imaging of Acute Endothelial Inflammation in the Abdominal Aorta. Mol. Imaging Biol. 2017, 19, 183–193. [Google Scholar] [CrossRef]
- Zhang, Y.-J.; Bai, D.-N.; Du, J.-X.; Jin, L.; Ma, J.; Yang, J.-L.; Cai, W.-B.; Feng, Y.; Xing, C.-Y.; Yuan, L.-J.; et al. Ultrasound-guided imaging of junctional adhesion molecule-A-targeted microbubbles identifies vulnerable plaque in rabbits. Biomaterials 2016, 94, 20–30. [Google Scholar] [CrossRef]
- Hirabayashi, F.; Iwanaga, K.; Okinaga, T.; Takahashi, O.; Ariyoshi, W.; Suzuki, R.; Sugii, M.; Maruyama, K.; Tominaga, K.; Nishihara, T. Epidermal growth factor receptor-targeted sonoporation with microbubbles enhances therapeutic efficacy in a squamous cell carcinoma model. PLoS ONE 2017, 12, e0185293. [Google Scholar] [CrossRef]
- Yeh, J.S.-M.; Sennoga, C.A.; McConnell, E.; Eckersley, R.; Tang, M.-X.; Nourshargh, S.; Seddon, J.M.; Haskard, D.O.; Nihoyannopoulos, P. A Targeting Microbubble for Ultrasound Molecular Imaging. PLoS ONE 2015, 10, e0129681. [Google Scholar] [CrossRef] [PubMed]
- Paganelli, G.; Magnani, P.; Zito, F.; Villa, E.; Sudati, F.; Lopalco, L.; Rossetti, C.; Malcovati, M.; Chiolerio, F.; Seccamani, E.; et al. Three-step monoclonal antibody tumor targeting in carcinoembryonic antigen-positive patients. Cancer Res. 1991, 51, 5960–5966. [Google Scholar] [PubMed]
- Carter, P. Improving the efficacy of antibody-based cancer therapies. Nat. Rev. Cancer 2001, 1, 118–129. [Google Scholar] [CrossRef] [PubMed]
- Safra, T.; Muggia, F.; Jeffers, S.; Tsao-Wei, D.D.; Groshen, S.; Lyass, O.; Henderson, R.; Berry, G.; Gabizon, A. Pegylated liposomal doxorubicin (doxil): Reduced clinical cardiotoxicity in patients reaching or exceeding cumulative doses of 500 mg/m2. Ann. Oncol. 2000, 11, 1029–1033. [Google Scholar] [CrossRef]
- Deutsch, Y.E.; Presutto, J.T.; Brahim, A.; Raychaudhuri, J.; Ruiz, M.A.; Sandoval-Sus, J.; Fernandez, H.F. Safety and Feasibility of Outpatient Liposomal Daunorubicin and Cytarabine (Vyxeos) Induction and Management in Patients with Secondary AML. Blood 2018, 132, 3559. [Google Scholar] [CrossRef]
- Gao, X.; Huang, L. Potentiation of Cationic Liposome-Mediated Gene Delivery by Polycations †. Biochemistry 1996, 35, 1027–1036. [Google Scholar] [CrossRef]
- Kawamura, K.; Kadowaki, N.; Suzuki, R.; Udagawa, S.; Kasaoka, S.; Utoguchi, N.; Kitawaki, T.; Sugimoto, N.; Okada, N.; Maruyama, K.; et al. Dendritic cells that endocytosed antigen-containing IgG-liposomes elicit effective antitumor immunity. J. Immunother. 2006, 29, 165–174. [Google Scholar] [CrossRef]
- Suzuki, R.; Takizawa, T.; Negishi, Y.; Hagisawa, K.; Tanaka, K.; Sawamura, K.; Utoguchi, N.; Nishioka, T.; Maruyama, K. Gene delivery by combination of novel liposomal bubbles with perfluoropropane and ultrasound. J. Control. Release 2007, 117, 130–136. [Google Scholar] [CrossRef]
- Endo-Takahashi, Y.; Negishi, Y.; Nakamura, A.; Ukai, S.; Ooaku, K.; Oda, Y.; Sugimoto, K.; Moriyasu, F.; Takagi, N.; Suzuki, R.; et al. Systemic delivery of miR-126 by miRNA-loaded Bubble liposomes for the treatment of hindlimb ischemia. Sci. Rep. 2015, 4, 3883. [Google Scholar] [CrossRef]
- Endo-Takahashi, Y.; Negishi, Y.; Nakamura, A.; Suzuki, D.; Ukai, S.; Sugimoto, K.; Moriyasu, F.; Takagi, N.; Suzuki, R.; Maruyama, K.; et al. pDNA-loaded Bubble liposomes as potential ultrasound imaging and gene delivery agents. Biomaterials 2013, 34, 2807–2813. [Google Scholar] [CrossRef]
- Endo-Takahashi, Y.; Negishi, Y.; Kato, Y.; Suzuki, R.; Maruyama, K.; Aramaki, Y. Efficient siRNA delivery using novel siRNA-loaded Bubble liposomes and ultrasound. Int. J. Pharm. 2012, 422, 504–509. [Google Scholar] [CrossRef] [PubMed]
- Negishi, Y.; Ishii, Y.; Shiono, H.; Akiyama, S.; Sekine, S.; Kojima, T.; Mayama, S.; Kikuchi, T.; Hamano, N.; Endo-Takahashi, Y.; et al. Bubble liposomes and ultrasound exposure improve localized morpholino oligomer delivery into the skeletal muscles of dystrophic mdx mice. Mol. Pharm. 2014, 11, 1053–1061. [Google Scholar] [CrossRef] [PubMed]
- Negishi, Y.; Hamano, N.; Tsunoda, Y.; Oda, Y.; Choijamts, B.; Endo-Takahashi, Y.; Omata, D.; Suzuki, R.; Maruyama, K.; Nomizu, M.; et al. AG73-modified Bubble liposomes for targeted ultrasound imaging of tumor neovasculature. Biomaterials 2013, 34, 501–507. [Google Scholar] [CrossRef] [PubMed]
- Choe, W.; Durgannavar, T.A.; Chung, S.J. Fc-Binding Ligands of Immunoglobulin G: An Overview of High Affinity Proteins and Peptides. Materials (Basel, Switzerland) 2016, 9, 994. [Google Scholar] [CrossRef] [PubMed]
- Jiang, T.; Zhuang, J.; Duan, H.; Luo, Y.; Zeng, Q.; Fan, K.; Yan, H.; Lu, D.; Ye, Z.; Hao, J.; et al. CD146 is a coreceptor for VEGFR-2 in tumor angiogenesis. Blood 2012, 120, 2330–2339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Braisted, A.C.; Wells, J.A. Minimizing a binding domain from protein A. Proc. Natl. Acad. Sci. USA 1996, 93, 5688–5692. [Google Scholar] [CrossRef] [PubMed]
- Guss, B.; Eliasson, M.; Olsson, A.; Uhlén, M.; Frej, A.K.; Jörnvall, H.; Flock, J.I.; Lindberg, M. Structure of the IgG-binding regions of streptococcal protein G. EMBO J. 1986, 5, 1567–1575. [Google Scholar] [CrossRef] [PubMed]
- Knappik, A.; Plückthun, A. Engineered turns of a recombinant antibody improve its in vivo folding. Protein Eng. 1995, 8, 81–89. [Google Scholar] [CrossRef]
- Carter, P.; Presta, L.; Gorman, C.M.; Ridgway, J.B.; Henner, D.; Wong, W.L.; Rowland, A.M.; Kotts, C.; Carver, M.E.; Shepard, H.M. Humanization of an anti-p185HER2 antibody for human cancer therapy. Proc. Natl. Acad. Sci. USA 1992, 89, 4285–4289. [Google Scholar] [CrossRef]
- Kikkawa, Y.; Enomoto-Okawa, Y.; Fujiyama, A.; Fukuhara, T.; Harashima, N.; Sugawara, Y.; Negishi, Y.; Katagiri, F.; Hozumi, K.; Nomizu, M.; et al. Internalization of CD239 highly expressed in breast cancer cells: a potential antigen for antibody-drug conjugates. 2018, 8. [Google Scholar] [CrossRef]
- Endo-Takahashi, Y.; Ooaku, K.; Ishida, K.; Suzuki, R.; Maruyama, K.; Negishi, Y. Preparation of Angiopep-2 Peptide-Modified Bubble Liposomes for Delivery to the Brain. Biol. Pharm. Bull. 2016, 39, 977–983. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Negishi, Y.; Hamano, N.; Sato, H.; Katagiri, F.; Takatori, K.; Endo-Takahashi, Y.; Kikkawa, Y.; Nomizu, M. Development of a Screening System for Targeting Carriers Using Peptide-Modified Liposomes and Tissue Sections. Biol. Pharm. Bull. 2018, 41, 1107–1111. [Google Scholar] [CrossRef] [PubMed]
- Hober, S.; Nord, K.; Linhult, M. Protein A chromatography for antibody purification. J. Chromatogr. B 2007, 848, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Saha, K.; Bender, F.; Gizeli, E. Comparative study of IgG binding to proteins G and A: nonequilibrium kinetic and binding constant determination with the acoustic waveguide device. Anal. Chem. 2003, 75, 835–842. [Google Scholar] [CrossRef] [PubMed]
- Ey, P.L.; Prowse, S.J.; Jenkin, C.R. Isolation of pure IgG1, IgG2a and IgG2b immunoglobulins from mouse serum using protein A-Sepharose. Immunochemistry 1978, 15, 429–436. [Google Scholar] [CrossRef]
- Bardin, N.; Anfosso, F.; Massé, J.M.; Cramer, E.; Sabatier, F.; Le Bivic, A.; Sampol, J.; Dignat-George, F. Identification of CD146 as a component of the endothelial junction involved in the control of cell-cell cohesion. Blood 2001, 98, 3677–3684. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Slamon, D.J.; Godolphin, W.; Jones, L.A.; Holt, J.A.; Wong, S.G.; Keith, D.E.; Levin, W.J.; Stuart, S.G.; Udove, J.; Ullrich, A.; et al. Studies of the HER-2/neu proto-oncogene in human breast and ovarian cancer. Science 1989, 244, 707–712. [Google Scholar] [CrossRef]
- Burns, P.N.; Wilson, S.R.; Simpson, D.H. Pulse inversion imaging of liver blood flow: improved method for characterizing focal masses with microbubble contrast. Invest. Radiol. 2000, 35, 58–71. [Google Scholar] [CrossRef]
- Sirsi, S.; Flexman, M.; Vlachos, F.; Huang, J.; Hernandez, S.L.; Kim, H.K.; Johung, T.J.; Gander, J.; Reichstein, A.; Lampl, B.S.; et al. Contrast Ultrasound Imaging for Identification of Early Responder Tumor Models to Anti-Angiogenic Therapy. Ultrasound Med. Biol. 2012, 38, 1019. [Google Scholar] [CrossRef]
- Borden, M.A.; Streeter, J.E.; Sirsi, S.R.; Dayton, P.A. In Vivo Demonstration of Cancer Molecular Imaging with Ultrasound Radiation Force and Buried-Ligand Microbubbles. Mol. Imaging 2013, 12. [Google Scholar] [CrossRef]
- Yan, P.; Chen, K.-J.; Wu, J.; Sun, L.; Sung, H.-W.; Weisel, R.D.; Xie, J.; Li, R.-K. The use of MMP2 antibody-conjugated cationic microbubble to target the ischemic myocardium, enhance Timp3 gene transfection and improve cardiac function. Biomaterials 2014, 35, 1063–1073. [Google Scholar] [CrossRef] [PubMed]
- Sirsi, S.R.; Borden, M.A. Advances in Ultrasound Mediated Gene Therapy Using Microbubble Contrast Agents. Theranostics 2012, 2, 1208–1222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwekkeboom, R.F.J.; Lei, Z.; Bogaards, S.J.P.; Aiazian, E.; Kamp, O.; Paulus, W.J.; Sluijter, J.P.G.; Musters, R.J.P. Ultrasound and Microbubble-Induced Local Delivery of MicroRNA-Based Therapeutics. Ultrasound Med. Biol. 2015, 41, 163–176. [Google Scholar] [CrossRef] [PubMed]
- Fujii, H.; Matkar, P.; Liao, C.; Rudenko, D.; Lee, P.J.; Kuliszewski, M.A.; Prud’homme, G.J.; Leong-Poi, H. Optimization of Ultrasound-mediated Anti-angiogenic Cancer Gene Therapy. Mol. Ther. Nucleic Acids 2013, 2, e94. [Google Scholar] [CrossRef] [PubMed]
- Dewitte, H.; Vanderperren, K.; Haers, H.; Stock, E.; Duchateau, L.; Hesta, M.; Saunders, J.H.; De Smedt, S.C.; Lentacker, I. Theranostic mRNA-loaded Microbubbles in the Lymphatics of Dogs: Implications for Drug Delivery. Theranostics 2015, 5, 97–109. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| NBs | Size (nm) ± SD |
|---|---|
| PEG-NBs (non-modified) | 529.3 ± 66.9 |
| m146-NBs (anti-mouse CD146 antibody-modified NBs) | 614.2 ± 96.2 |
| 4D5-NBs (anti-HER2 antibody-modified NBs) | 690.4 ± 106.1 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hamano, N.; Kamoshida, S.; Kikkawa, Y.; Yano, Y.; Kobayashi, T.; Endo-Takahashi, Y.; Suzuki, R.; Maruyama, K.; Ito, Y.; Nomizu, M.; et al. Development of Antibody-Modified Nanobubbles Using Fc-Region-Binding Polypeptides for Ultrasound Imaging. Pharmaceutics 2019, 11, 283. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics11060283
Hamano N, Kamoshida S, Kikkawa Y, Yano Y, Kobayashi T, Endo-Takahashi Y, Suzuki R, Maruyama K, Ito Y, Nomizu M, et al. Development of Antibody-Modified Nanobubbles Using Fc-Region-Binding Polypeptides for Ultrasound Imaging. Pharmaceutics. 2019; 11(6):283. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics11060283
Chicago/Turabian StyleHamano, Nobuhito, Sho Kamoshida, Yamato Kikkawa, Yusuke Yano, Tomomi Kobayashi, Yoko Endo-Takahashi, Ryo Suzuki, Kazuo Maruyama, Yuji Ito, Motoyoshi Nomizu, and et al. 2019. "Development of Antibody-Modified Nanobubbles Using Fc-Region-Binding Polypeptides for Ultrasound Imaging" Pharmaceutics 11, no. 6: 283. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics11060283