Affinity Effects on the Release of Non-Conventional Antifibrotics from Polymer Depots
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Molecular Docking Simulations
2.3. Surface Plasmon Resonance
2.4. Disk Synthesis
2.5. Microparticle Synthesis
2.6. Drug Loading and Release
2.7. Statistics
3. Results
3.1. In Silico Affinity Binding Predictions
3.2. In Vitro Affinity Measurements with Surface Plasmon Resonance
3.3. Drug Loading Efficiencies
3.4. Daily Drug Release Profiles
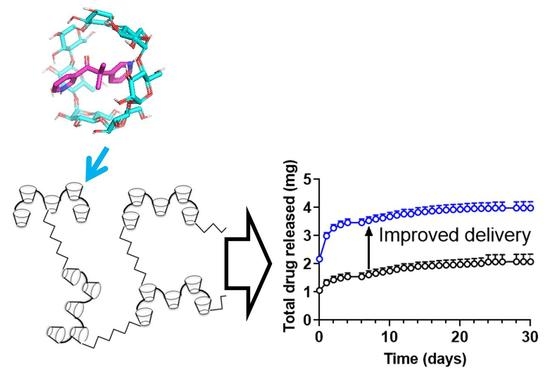
3.5. Cumulative Drug Release
3.6. Drug-Polymer Characteristics Juxtaposed with Release Data
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Ho, Y.Y.; Lagares, D.; Tager, A.M.; Kapoor, M. Fibrosis—A lethal component of systemic sclerosis. Nat. Rev. Rheumatol. 2014, 10, 390–402. [Google Scholar] [CrossRef] [PubMed]
- Cordero-Espinoza, L.; Huch, M. The balancing act of the liver: Tissue regeneration versus fibrosis. J. Clin. Investig. 2018, 128, 85–96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mitragotri, S.; Burke, P.A.; Langer, R. Overcoming the challenges in administering biopharmaceuticals: Formulation and delivery strategies. Nat. Rev. Drug Discov. 2014, 13, 655–672. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rohner, N.A.; Thomas, S.N. Melanoma growth effects on molecular clearance from tumors and biodistribution into systemic tissues versus draining lymph nodes. J. Control. Release 2016, 223, 99–108. [Google Scholar] [CrossRef] [Green Version]
- Suzuki, J.B.; Resnik, R.R. Wound Dehiscence: Incision Line Opening. In Misch’s Avoiding Complications in Oral Implantology; Resnik, R.R., Misch, C.E., Eds.; Mosby: St. Louis, MO, USA, 2018; pp. 402–439. [Google Scholar] [CrossRef]
- Remoué, N.; Bonod, C.; Fromy, B.; Sigaudo-Roussel, D. Animal Models in Chronic Wound Healing Research: For Innovations and Emerging Technologies in Wound Care. In Innovations and Emerging Technologies in Wound Care; Gefen, A., Ed.; Academic Press: Cambridge, MA, USA, 2020; pp. 197–224. [Google Scholar] [CrossRef]
- Mohammed-Saeid, W.; Karoyo, A.H.; Verrall, R.E.; Wilson, L.D.; Badea, I. Inclusion complexes of melphalan with gemini-conjugated β-cyclodextrin: Physicochemical properties and chemotherapeutic efficacy in in-vitro tumor models. Pharmaceutics 2019, 11, 427. [Google Scholar] [CrossRef] [Green Version]
- Argenziano, M.; Haimhoffer, A.; Bastiancich, C.; Jicsinszky, L.; Caldera, F.; Trotta, F.; Scutera, S.; Alotto, D.; Fumagalli, M.; Musso, T.; et al. In vitro enhanced skin permeation and retention of imiquimod loaded in β-cyclodextrin nanosponge hydrogel. Pharmaceutics 2019, 11, 138. [Google Scholar] [CrossRef] [Green Version]
- Mehenni, L.; Lahiani-Skiba, M.; Ladam, G.; Hallouard, F.; Skiba, M. Preparation and characterization of spherical amorphous solid dispersion with amphotericin B. Pharmaceutics 2018, 10, 235. [Google Scholar] [CrossRef] [Green Version]
- Cyphert, E.L.; Zuckerman, S.T.; Korley, J.N.; von Recum, H.A. Affinity interactions drive post-implantation drug filling, even in the presence of bacterial biofilm. Acta Biomater. 2017, 57, 95–102. [Google Scholar] [CrossRef]
- Haley, R.M.; von Recum, H.A. Localized and targeted delivery of NSAIDs for treatment of inflammation: A review. Exp. Biol. Med. 2019, 244, 433–444. [Google Scholar] [CrossRef]
- Thatiparti, T.R.; Shoffstall, A.J.; von Recum, H.A. Cyclodextrin-based device coatings for affinity-based release of antibiotics. Biomaterials 2010, 31, 2335–2347. [Google Scholar] [CrossRef]
- Rohner, N.A.; Purdue, L.; von Recum, H.A. Affinity-based polymers provide long-term immunotherapeutic drug delivery across particle size ranges optimal for macrophage targeting. bioRxiv 2019, 802801. [Google Scholar] [CrossRef] [Green Version]
- Cyphert, E.L.; von Recum, H.A. Emerging technologies for long-term antimicrobial device coatings: Advantages and limitations. Exp. Biol. Med. 2017, 242, 788–798. [Google Scholar] [CrossRef] [PubMed]
- Cyphert, E.L.; Learn, G.D.; Hurley, S.K.; Lu, C.-Y.; von Recum, H.A. Bone cements: An additive to PMMA bone cement enables postimplantation drug refilling, broadens range of compatible antibiotics, and prolongs antimicrobial therap. Adv. Healthc. Mater. 2018, 7, 18700812. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, G.S.; Maves, M.D.; McCormack, M.L. Deferoxamine decreases necrosis in dorsally based pig skin flaps. Otolaryngol.-Head Neck Surg. 1989, 101, 559–561. [Google Scholar] [CrossRef]
- Wahl, E.A.; Schenck, T.L.; Machens, H.-G.; Balmayor, E.R. VEGF released by deferoxamine preconditioned mesenchymal stem cells seeded on collagen-GAG substrates enhances neovascularization. Sci. Rep. 2016, 6, 36879. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ikeda, Y.; Ozono, I.; Tajima, S.; Imao, M.; Horinouchi, Y.; Izawa-Ishizawa, Y.; Kihira, Y.; Miyamoto, L.; Ishizawa, K.; Tsuchiya, K.; et al. Iron chelation by deferoxamine prevents renal interstitial fibrosis in mice with unilateral ureteral obstruction. PLoS ONE 2014, 9, e89355. [Google Scholar] [CrossRef] [Green Version]
- Stojadinovic, O.; Gordon, K.A.; Lebrun, E.; Tomic-Canic, M. Stress-induced hormones cortisol and epinephrine impair wound epithelization. Adv. Wound Care 2012, 1, 29–35. [Google Scholar] [CrossRef] [Green Version]
- Vukelic, S.; Stojadinovic, O.; Pastar, I.; Rabach, M.; Krzyzanowska, A.; Lebrun, E.; Davis, S.C.; Resnik, S.; Brem, H.; Tomic-Canic, M. Cortisol synthesis in epidermis is induced by IL-1 and tissue injury. J. Biol. Chem. 2011, 286, 10265–10275. [Google Scholar] [CrossRef] [Green Version]
- Espey, D.K.; Djomand, G.; Diomande, I.; Dosso, M.; Saki, M.Z.; Kanga, J.M.; Spiegel, R.A.; Marston, B.J.; Gorelkin, L.; Meyers, W.M.; et al. Pilot study of treatment of buruli ulcer with rifampin and dapsone. Int. J. Infect. Dis. 2002, 6, 60–65. [Google Scholar] [CrossRef] [Green Version]
- Bassi, L.; Bolzoni, G. Immunosuppression by Rifamycins; Springer: Berlin/Heidelberg, Germany, 1982. [Google Scholar]
- Bi, W.; Zhu, L.; Wang, C.; Liang, Y.; Liu, J.; Shi, Q.; Tao, E. Rifampicin inhibits microglial inflammation and improves neuron survival against inflammation. Brain Res. 2011, 1395, 12–20. [Google Scholar] [CrossRef]
- Bastakoty, D.; Saraswati, S.; Cates, J.; Lee, E.; Nanney, L.B.; Young, P.P. Inhibition of Wnt/beta-catenin pathway promotes regenerative repair of cutaneous and cartilage injury. FASEB J. 2015, 29, 4881–4892. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murakoshi, M.; Saiki, K.; Urayama, K.; Sato, T.N. An anthelmintic drug, pyrvinium pamoate, thwarts fibrosis and ameliorates myocardial contractile dysfunction in a mouse model of myocardial infarction. PLoS ONE 2013, 8, e79374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rohner, N.A.; Dogan, A.B.; Robida, O.A.; von Recum, H.A. Serum biomolecules unable to compete with drug refilling into cyclodextrin polymers regardless of the form. J. Mater. Chem. B 2019, 7, 5320–5327. [Google Scholar] [CrossRef] [PubMed]
- Rivera-Delgado, E.; Sadeghi, Z.; Wang, N.X.; Kenyon, J.; Satyanarayan, S.; Kavran, M.; Flask, C.; Hijaz, A.Z.; von Recum, H.A. Local release from affinity-based polymers increases urethral concentration of the stem cell chemokine CCL7 in rats. Biomed. Mater. 2016, 11, 025022. [Google Scholar] [CrossRef]
- Trott, O.; Olson, A.J. AutoDock Vina: Improving the speed and accuracy of docking with a new scoring function, efficient optimization, and multithreading. J. Comput. Chem. 2010, 31, 455–461. [Google Scholar] [CrossRef] [Green Version]
- Dallakyan, S.; Olson, A.J. Small-molecule library screening by docking with PyRx. Methods Mol. Biol. (Clifton, N. J.) 2015, 1263, 243–250. [Google Scholar] [CrossRef]
- Rivera-Delgado, E.; Nam, J.K.; von Recum, H.A. Localized affinity-based delivery of prinomastat for cancer treatment. ACS Biomater. Sci. Eng. 2017, 3, 238–242. [Google Scholar] [CrossRef]
- Thatiparti, T.R.; von Recum, H.A. Cyclodextrin complexation for affinity-based antibiotic delivery. Macromol. Biosci. 2009, 10, 82–90. [Google Scholar] [CrossRef]
- Grafmiller, K.T.; Zuckerman, S.T.; Petro, C.; Liu, L.; von Recum, H.A.; Rosen, M.J.; Korley, J.N. Antibiotic-releasing microspheres prevent mesh infection in vivo. J. Surg. Res. 2016, 206, 41–47. [Google Scholar] [CrossRef] [Green Version]
- Jhunjhunwala, S.; Balmert, S.C.; Raimondi, G.; Dons, E.; Nichols, E.E.; Thomson, A.W.; Little, S.R. Controlled release formulations of IL-2, TGF-β1 and rapamycin for the induction of regulatory T cells. J. Control. Release 2012, 159, 78–84. [Google Scholar] [CrossRef] [Green Version]
- Rivera-Delgado, E.; von Recum, H.A. Using affinity to provide long-term delivery of antiangiogenic drugs in cancer therapy. Mol. Pharm. 2017, 14, 899–907. [Google Scholar] [CrossRef] [PubMed]
- Rivera-Delgado, E.; Xin, A.; von Recum, H.A. Using QSARs for predictions in drug delivery. bioRxiv 2019. [Google Scholar] [CrossRef]
- Rohner, N.A.; Schomisch, S.J.; Marks, J.M.; von Recum, H.A. Cyclodextrin polymer preserves sirolimus activity and local persistence for antifibrotic delivery over the time course of wound healing. Mol. Pharm. 2019, 16, 1766–1774. [Google Scholar] [CrossRef] [PubMed]
- Fu, A.S.; Thatiparti, T.R.; Saidel, G.M.; von Recum, H.A. Experimental studies and modeling of drug release from a tunable affinity-based drug delivery platform. Ann. Biomed. Eng. 2011, 39, 2466–2475. [Google Scholar] [CrossRef]
- Fu, A.S.V.R.; Horst, A. Affinity-Based Drug Delivery. In Engineering Polymer Systems for Improved Drug Delivery; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2014. [Google Scholar] [CrossRef]
- Wang, N.X.; von Recum, H.A. Affinity-based drug delivery. Macromol. Biosci. 2010, 11, 321–332. [Google Scholar] [CrossRef]
- Cyphert, E.L.; Bil, M.; von Recum, H.A.; Święszkowski, W. Repurposing biodegradable tissue engineering scaffolds for localized chemotherapeutic delivery. J. Biomed. Mater. Res. Part A 2020. [Google Scholar] [CrossRef]
- Vasapollo, G.; Sole, R.D.; Mergola, L.; Lazzoi, M.R.; Scardino, A.; Scorrano, S.; Mele, G. Molecularly imprinted polymers: Present and future prospective. Int. J. Mol. Sci. 2011, 12, 5908–5945. [Google Scholar] [CrossRef] [Green Version]
- Juric, D.; Rohner, N.A.; von Recum, H.A. Molecular Imprinting of cyclodextrin supramolecular hydrogels improves drug loading and delivery. Macromol. Biosci. 2019, 19, 1800246. [Google Scholar] [CrossRef]
- Liechty, W.B.; Kryscio, D.R.; Slaughter, B.V.; Peppas, N.A. Polymers for drug delivery systems. Annu. Rev. Chem. Biomol. Eng. 2010, 1, 149–173. [Google Scholar] [CrossRef] [Green Version]
- Learn, G.D.; Lai, E.J.; von Recum, H.A. Using nonthermal plasma treatment to improve quality and durability of hydrophilic coatings on hydrophobic polymer surfaces. bioRxiv 2019, 868885. [Google Scholar] [CrossRef] [Green Version]
- Learn, G.D.; Lai, E.J.; Wilson, E.J.; von Recum, H.A. Nonthermal plasma treatment of polymers modulates biological fouling but can cause material embrittlement. bioRxiv 2019, 842260. [Google Scholar] [CrossRef]
- Cyphert, E.; Rivera, E.; Fu, A.S.; von Recum, H.A. Chemotherapeutic Delivery Based on Tumor ph Using an in Situ Affinity Change. In Proceedings of the Society for Biomaterials, Denver, CO, USA, 16–19 April 2014. [Google Scholar]
- Tellier, L.E.; Krieger, J.R.; Brimeyer, A.L.; Coogan, A.C.; Falis, A.A.; Rinker, T.E.; Schudel, A.; Thomas, S.N.; Jarrett, C.D.; Willett, N.J.; et al. Localized SDF-1α delivery increases pro-healing bone marrow-derived cells in the supraspinatus muscle following severe rotator cuff injury. Regen. Eng. Transl. Med. 2018, 4, 92–103. [Google Scholar] [CrossRef] [PubMed]
- Fu, A.S. Affinity-based Delivery and Reloading of Doxorubicin For Treatment of Glioblastoma Multiforme. Ph.D. Thesis, Case Western Reserve University School of Graduate Studies, Cleveland, OH, USA, 2013. [Google Scholar]
- Neves, B.J.; Braga, R.C.; Melo-Filho, C.C.; Moreira-Filho, J.T.; Muratov, E.N.; Andrade, C.H. QSAR-based virtual screening: Advances and applications in drug discovery. Front. Pharmacol. 2018, 9, 1275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cyphert, E.L.; Fu, A.S.; von Recum, H.A. Chemotherapeutic delivery using pH-responsive, affinity-based release. Exp. Biol. Med. 2017, 242, 692–699. [Google Scholar] [CrossRef] [PubMed]
- Dogan, A.B.; von Recum, H.A. Engineering selective molecular tethers to enhance suboptimal drug properties. bioRxiv 2020. [Google Scholar] [CrossRef]





| Drug | Conventional Use | Conventional Route | Wound Resolution Indications |
|---|---|---|---|
| Deferoxamine (DFOA) | Treating iron/aluminum toxicity | SQ, IM, IV | Decreases oxidative stress and necrosis [16] Enhances neovascularization [17] Reduces interstitial renal fibrosis [18] |
| Metyrapone (MTP) | Inhibition of adrenal steroidgenesis | PO | Enhances epithelialization [19,20] |
| Rifampicin (RIF) | Antibiotic activity | PO, IV | Ulcer resolution [21] Immunomodulatory [22,23] |
| Pyrvinium pamoate (PYR) | Anthelmintic activity | PO | Wnt inhibition [24] Inhibits fibroblast survival [25] |
| Drug | Mol. Wt.(g/mol) | Solubility (PBS, 25 °C, mg/mL) | β-CD/Dex Affinity Ratio | Max Total Release (mg) | Days of Release |
|---|---|---|---|---|---|
| Deferoxamine | 560.68 | 5.0 | 0.193 | 1.7 ± 0.92 | 30 |
| pCD-β-MP | Disks | ||||
| Metyrapone | 226.27 | 0.43 | 0.012 | 5.0 ± 0.53 | 30 |
| pCD-β-disk | All polymers | ||||
| Pyrvinium | 382.52 | 0.00029 | 0.022 | 1.6 ± 0.30 | 30 |
| pCD-β-MP | All polymers | ||||
| Rifampicin | 822.94 | 2.5 | 0.023 | 1.9 ± 0.21 | 30 |
| Dex-disk | Disks |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rohner, N.A.; Nguyen, D.; von Recum, H.A. Affinity Effects on the Release of Non-Conventional Antifibrotics from Polymer Depots. Pharmaceutics 2020, 12, 275. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics12030275
Rohner NA, Nguyen D, von Recum HA. Affinity Effects on the Release of Non-Conventional Antifibrotics from Polymer Depots. Pharmaceutics. 2020; 12(3):275. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics12030275
Chicago/Turabian StyleRohner, Nathan A., Dung Nguyen, and Horst A. von Recum. 2020. "Affinity Effects on the Release of Non-Conventional Antifibrotics from Polymer Depots" Pharmaceutics 12, no. 3: 275. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics12030275