Nanostructured Lipid Carriers for Delivery of Chemotherapeutics: A Review
Abstract
:1. Introduction
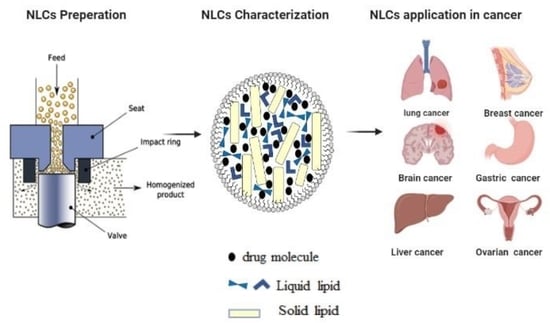
2. Structure and Classification of NLCs
3. Composition and Methods of Preparation of NLCs
3.1. Composition of NLCs
3.2. Methods of Preparation of NLCs
3.2.1. High Pressure Homogenization
3.2.2. Solvent Emulsification/Evaporation
3.2.3. Microemulsions
3.2.4. Ultra-Sonication or High-Speed Homogenization
3.2.5. Spray Drying
3.2.6. Microfluidics
4. Characterization of Drug Loaded NLCs
4.1. Particle Size and Morphology
4.2. Surface Charge
4.3. Degree of Crystallinity
4.4. Encapsulation Efficiency Percentage (EE %)
4.5. Stability
4.6. Drug Release from NLCs
5. Applications of NLCs in Delivery of Chemotherapeutic Agents
| Route of Administration | Drug Name | Uses | References |
|---|---|---|---|
| Parenteral injection | Bromocriptine | Brain targeting for treatment of Parkinson’s disease, neuroleptic malignant syndrome and pituitary tumors | [98] |
| Apomorphine | Brain targeting for treatment of Parkinson’s disease | [99,100] | |
| Baicalein | Brain targeting for prevention or therapy of ischemic brain damage and neurodegenerative diseases | [101,102] | |
| Silybin | Hepatotoxicity | [103,104] | |
| Bifendate | Hepatitis | [105,106] | |
| Buprenorphine | Analgesic treatment of chronic pain and opioid dependence. | [107,108] | |
| Dexamethasone acetate | Anti-inflammatory | [109] | |
| Topical | Cyproterone acetate | Acne vulgaris | [110] |
| Acitretin | Acne vulgaris and psoriasis | [73,111] | |
| Psoralen | Psoriasis | [29,112] | |
| Flurbiprofen | Rheumatoid arthritis, sunburn and gout | [113,114] | |
| Ketoprofen | Arthritis and skin inflammation | [30,115] | |
| Celastrol/Indomethacin | Arthritis and inflammatory pain | [116] | |
| Celecoxib | Anti-inflammatory | [43] | |
| Valdecoxib | Anti-inflammatory | [117] | |
| Fluticasone | Atopic dermatitis and psoriasis | [42] | |
| Lidocaine | Local anesthetic | [118] | |
| Benzocaine/Lidocaine | Local anesthetic | [119] | |
| Nanolipid Q 10 CL | Anti-aging/cellular antioxidant | [58,120,121,122] | |
| Lutein | Antioxidant, anti-stress, and blue light filter protect the skin from photo damage | [123,124] | |
| Meloxicam | Osteoarthritis and rheumatoid arthritis | [125] | |
| Clotrimazole | Antifungal | [26,126] | |
| Octyl-methoxycinnamate | UVB absorber, Sunscreen | [127,128] | |
| Donepezil | Alzheimer | [41] | |
| Oral | Repaglinide | Diabetes | [129,130,131] |
| Hydrochlorothiazide | Hypertension | [27] | |
| Simvastatin | Antihyperlipidemic | [132] | |
| Lovastatin | Antihyperlipidemic | [133] | |
| Ocular | Triamcinolone Acetonide | Inflammatory, edematous, and angiogenic ocular diseases | [134] |
| Mangiferin | Cataract | [135] | |
| Flurbiprofen | Anti-inflammatory | [63,136,137] | |
| Moxifloxacin | Treatment of endophthalmitis | [138] | |
| Pulmonary | Itraconazole | Fungal lung infections | [139] |
| Sildenafil | Pulmonary arterial hypertension | [140] | |
| Montelukast sodium | Prophylaxis and treatment of chronic asthma | [141] |
| Treatment | Control Drug | Cancer Type | In Vitro Cell Line | IC50 | In Vivo Tumor Inhibition Rate | References | |||
|---|---|---|---|---|---|---|---|---|---|
| Drug-NLCs | Free Drug | Blank NLCs | Drug-NLCs | Free Drug | |||||
| Docetaxel-NLC (DTX-NLC) | Duopafei® (polymeric micelles loaded with DTX) | Murine melanoma | B16 | 0.47 µg/mL | 0.96 µg/mL | 30.26 µg/mL | 62.69% (10 mg/kg) 90.36% (20 mg/kg) | 10 mg/kg: 42.74% | [16] |
| Hepatocellular carcinoma | HepG2 | 0.15 µg/mL | 0.74 µg/mL | 17.50 µg/mL | |||||
| Pulmonary adenocarcinoma | A549 | 0.02 µg/mL | 0.08 µg/mL | 10.11 µg/mL | |||||
| Ovarian carcinoma | SKOV3 | 0.44 µg/mL | 0.72 µg/mL | 26.34 µg/mL | |||||
| Paclitaxel-NLC (PTX-NLC) | Paclitaxel | Breast cancer | MCF-7 | 0.075 µg/mL | 0.29 µg/mL | 455.49 µg/mL | [17] | ||
| Multidrug-resistant breast cancer | MCF-7/ADR | 0.065 µg/mL | 8.61 µg/mL | 496.74 µg/mL | |||||
| Ovarian carcinoma | SKOV3 | 0.053 µg/mL | 0.16 µg/mL | 487.92 µg/mL | |||||
| Multidrug-resistant ovarian carcinoma | SKOV3-TR30 | 0.1 µg/mL | 9.35 µg/mL | 498.97 µg/mL | |||||
| Non-small cell lung carcinoma | H460 | 0.062 µM | 0.193 µM | - | 64% | 26% | [22] | ||
| Doxorubicin-NLC (DOX-NLC) | Doxorubicin | Breast cancer | MCF-7 | 0.15 µg/mL | 0.176 µg/mL | 455.49 µg/mL | [17] | ||
| Multidrug-resistant breast cancer | MCF-7/ADR | 0.83 µg/mL | 6.20 µg/mL | 496.74 µg/mL | |||||
| Ovarian carcinoma | SKOV3 | 0.33 µg/mL | 0.52 µg/mL | 487.92 µg/mL | |||||
| Multidrug-resistant ovarian carcinoma | SKOV3-TR30 | 0.52 µg/mL | 1.83 µg/mL | 498.97 µg/mL | |||||
| Non-small cell lung carcinoma | H460 | 0.059 µM | 0.176 µM | - | 65% | 26% | [22] | ||
| Hairy cell leukemia | HC2 20d2/c | 15.01 ± 0.5 | 17.81 ± 1.2 | - | [25] | ||||
| Quercetin-NLC (Q-NLC) | Quercetin | Breast cancer | MCF-7 | 15.8 µg/mL | >50 µg/mL | >50 µg/mL | [18] | ||
| MDA-MB-231 | 14.1 µg/mL | >50 µg/mL | >50 µg/mL | ||||||
| Etoposide-NLC (ETP-NLCs) | Etoposide | Gastric cancer | SGC7901 | 6.3 µg/mL | 56.5 µg/mL | - | Two-fold higher inhibition than control | [71] | |
| Cisplatin-NLC (DDP-NLC) | Cisplatin | Head and Neck cancer | FaDu | 4.7 µM | 46.5 µM | - | 41.7% | 9.3% | [142] |
| Curcumin-NLC (CUR-NLC) | Curcumin | Brain Cancer | A172 | 20 µg/mL | 80 µg/mL | - | 82.3% | 19.5% | [19] |
| Tamoxifen NLC (TAM-NLC) | Tamoxifen | Breast cancer | MCF-7 | 5.56 µg/mL | 2.72 µg/mL | - | [65] | ||
| 4T1 | 5.19 µg/mL | 5.13 µg/mL | - | ||||||
| Chemotherapeutic Agents | Target | Targeting Ligand | Linker | Reference |
|---|---|---|---|---|
| Doxorubicin (Dox)-loaded NLC | Epidermal growth factor receptor variant III (EGFRvIII) | EGFRvIII monoclonal antibody (MAb) | 3-(N-succinimidyloxyglutaryl)aminopropyl polyethylene glycol-carbamyl-distearoylphosphatidylethanolammine (DSPE-PEG2000-NHS) | [25] |
| Docetaxel (DTX)-loaded NLC | Vascular endothelial growth factor receptors (VEGFRs) which acts as double targets (tumor- and vascular targeting) | anti-VEGFR-2 antibody | 1,2-Distearoyl-sn-glycero-3-phosphoethanolamine-N-[amino(polyethylene glycol)-2000] (DSPE-PEG2000-NH2) | [74] |
| Hepsin (Hpn)-expressing prostate cancer cells | RIPL peptide (IPLVVPLRRRRRRRRC, 16-mer) | Distearoyl phosphatidylethanolamine-polyethylene glycol2000-maleimide (DSPE-PEG2000-Mal) | [93] | |
| Cisplatin (DDP) and (PTX)-loaded NLC | Folate receptors in head and neck cancer | Folate | 1,2-Distearoyl-sn-glycero-3-phosphoethanolamine-N-[amino(polyethylene glycol)-2000] (DSPE-PEG2000-NH2) | [142] |
| Temozolomide and vincristine-loaded NLC | Lactoferrin receptors in Glioblastoma multiforme | Lactoferrin | Distearoyl phosphatidylethanolamine-polyethylene glycol2000-maleimide (DSPE-PEG2000-Mal) | [143] |
| Gemcitabine (GEM) and (PTX)-loaded NLC | Glucose receptors in in non-small-cell lung cancer | N-acetyl-d-glucosamine | Hydrogen bonds between N-acetyl-d-glucosamine and sodium deoxycholate | [144] |
6. Toxicity and Biocompatibility
7. Conclusions
8. Future Directions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Belachew, S.A.; Erku, D.A.; Mekuria, A.B.; Gebresillassie, B.M. Pattern of chemotherapy-related adverse effects among adult cancer patients treated at Gondar University Referral Hospital, Ethiopia: A cross-sectional study. Drug. Healthc. Patient Saf. 2016, 8, 83–90. [Google Scholar] [CrossRef] [Green Version]
- Mehnert, W.; Mäder, K. Solid lipid nanoparticles: Production, characterization and applications. Adv. Drug Deliv. Rev. 2001, 47, 165–196. [Google Scholar] [CrossRef]
- De Jong, W.H.; Borm, P.J.A. Drug delivery and nanoparticles: Applications and hazards. Int. J. Nanomed. 2008, 3, 133–149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shidhaye, S.S.; Vaidya, R.; Sutar, S.; Patwardhan, A.; Kadam, V.J. Solid Lipid Nanoparticles and Nanostructured Lipid Carriers—Innovative Generations of Solid Lipid Carriers. Curr. Drug Deliv. 2008, 5, 324–331. [Google Scholar] [CrossRef] [PubMed]
- Sawant, K.; Dodiya, S. Recent Advances and Patents on Solid Lipid Nanoparticles. Recent Pat. Drug Deliv. Formul. 2008, 2, 120–135. [Google Scholar] [CrossRef] [PubMed]
- Müller, R.H.; Mäder, K.; Gohla, S. Solid lipid nanoparticles (SLN) for controlled drug delivery—A review of the state of the art. Eur. J. Pharm. Biopharm. 2000, 50, 161–177. [Google Scholar] [CrossRef]
- Muller, R.H.; Shegokar, R.; Keck, C.M. 20 Years of Lipid Nanoparticles (SLN & NLC): Present State of Development & Industrial Applications. Curr. Drug Discov. Technol. 2011, 8, 207–227. [Google Scholar]
- Jores, K.; Mehnert, W.; Mäder, K. Physicochemical investigations on solid lipid nanoparticles and on oil-loaded solid lipid nanoparticles: A nuclear magnetic resonance and electron spin resonance study. Pharm. Res. 2003, 20, 1274–1283. [Google Scholar] [CrossRef] [PubMed]
- Abdelbary, G.; Haider, M. In vitro characterization and growth inhibition effect of nanostructured lipid carriers for controlled delivery of methotrexate. Pharm. Dev. Technol. 2013, 18, 1159–1168. [Google Scholar] [CrossRef]
- Müller, R.H.; Radtke, M.; Wissing, S.A. Nanostructured lipid matrices for improved microencapsulation of drugs. Int. J. Pharm. 2002, 242, 121–128. [Google Scholar] [CrossRef]
- Müller, R.H.; Radtke, M.; Wissing, S.A. Solid lipid nanoparticles (SLN) and nanostructured lipid carriers (NLC) in cosmetic and dermatological preparations. Adv. Drug Deliv. Rev. 2002, 54 (Suppl. 1), S131–S155. [Google Scholar]
- Kasongo, K.W.; Jansch, M.; Müller, R.H.; Walker, R.B. Evaluation of the in vitro differential protein adsorption patterns of didanosine-loaded nanostructured lipid carriers (NLCs) for potential targeting to the brain. J. Liposome Res. 2011, 21, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Jenning, V.; Gohla, S.H. Encapsulation of retinoids in solid lipid nanoparticles (SLN®). J. Microencapsul. 2001, 18, 149–158. [Google Scholar] [PubMed]
- Khosa, A.; Reddi, S.; Saha, R.N. Nanostructured lipid carriers for site-specific drug delivery. Biomed. Pharmacother. 2018, 103, 598–613. [Google Scholar] [CrossRef]
- Ding, X.; Xu, X.; Zhao, Y.; Zhang, L.; Yu, Y.; Huang, F.; Yin, D.; Huang, H. Tumor targeted nanostructured lipid carrier co-delivering paclitaxel and indocyanine green for laser triggered synergetic therapy of cancer. RSC Adv. 2017, 7, 35086–35095. [Google Scholar] [CrossRef] [Green Version]
- Liu, D.; Liu, Z.; Wang, L.; Zhang, C.; Zhang, N. Nanostructured lipid carriers as novel carrier for parenteral delivery of docetaxel. Colloids Surf. B Biointerfaces 2011, 85, 262–269. [Google Scholar] [CrossRef]
- Zhang, X.-G.; Miao, J.; Dai, Y.-Q.; Du, Y.-Z.; Yuan, H.; Hu, F.-Q. Reversal activity of nanostructured lipid carriers loading cytotoxic drug in multi-drug resistant cancer cells. Int. J. Pharm. 2008, 361, 239–244. [Google Scholar] [CrossRef]
- Sun, M.; Nie, S.; Pan, X.; Zhang, R.; Fan, Z.; Wang, S. Quercetin-nanostructured lipid carriers: Characteristics and anti-breast cancer activities in vitro. Colloids Surf. B Biointerfaces 2014, 113, 15–24. [Google Scholar] [CrossRef]
- Chen, Y.; Pan, L.; Jiang, M.; Li, D.; Jin, L. Nanostructured lipid carriers enhance the bioavailability and brain cancer inhibitory efficacy of curcumin both in vitro and in vivo. Drug Deliv. 2016, 23, 1383–1392. [Google Scholar]
- Bondì, M.L.; Craparo, E.F.; Giammona, G.; Cervello, M.; Azzolina, A.; Diana, P.; Martorana, A.; Cirrincione, G. Nanostructured Lipid Carriers-Containing Anticancer Compounds: Preparation, Characterization, and Cytotoxicity Studies. Drug Deliv. 2007, 14, 61–67. [Google Scholar] [CrossRef]
- Fang, Y.-P.; Lin, Y.-K.; Su, Y.-H.; Fang, J.-Y. Tryptanthrin-Loaded Nanoparticles for Delivery into Cultured Human Breast Cancer Cells, MCF7: The Effects of Solid Lipid/Liquid Lipid Ratios in the Inner Core. Chem. Pharm. Bull. 2011, 59, 266–271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.; Zhang, H.; Hao, J.; Li, B.; Li, M.; Xiuwen, W. Lung cancer combination therapy: Co-delivery of paclitaxel and doxorubicin by nanostructured lipid carriers for synergistic effect. Drug Deliv. 2016, 23, 1398–1403. [Google Scholar] [CrossRef]
- Sabzichi, M.; Samadi, N.; Mohammadian, J.; Hamishehkar, H.; Akbarzadeh, M.; Molavi, O. Sustained release of melatonin: A novel approach in elevating efficacy of tamoxifen in breast cancer treatment. Colloids Surf. B Biointerfaces 2016, 145, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Sjöström, B.; Bergenståhl, B. Preparation of submicron drug particles in lecithin-stabilized o w emulsions: I. Model studies of the precipitation of cholesteryl acetate. Int. J. Pharm. 1992, 84, 107–116. [Google Scholar] [CrossRef]
- Abdolahpour, S.; Toliyat, T.; Omidfar, K.; Modjtahedi, H.; Wong, A.J.; Rasaee, M.J.; Kashanian, S.; Paknejad, M. Targeted delivery of doxorubicin into tumor cells by nanostructured lipid carriers conjugated to anti-EGFRvIII monoclonal antibody. Artif. Cells Nanomed. Biotechnol. 2018, 46, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Souto, E.B.; Müller, R.H. Investigation of the factors influencing the incorporation of clotrimazole in SLN and NLC prepared by hot high-pressure homogenization. J. Microencapsul. 2006, 23, 377–388. [Google Scholar] [CrossRef]
- Cirri, M.; Maestrini, L.; Maestrelli, F.; Mennini, N.; Mura, P.; Ghelardini, C.; Di Cesare Mannelli, L. Design, characterization and in vivo evaluation of nanostructured lipid carriers (NLC) as a new drug delivery system for hydrochlorothiazide oral administration in pediatric therapy. Drug Deliv. 2018, 25, 1910–1921. [Google Scholar] [CrossRef]
- Carvajal-Vidal, P.; Fábrega, M.J.; Espina, M.; Calpena, A.C.; García, M.L. Development of Halobetasol-loaded nanostructured lipid carrier for dermal administration: Optimization, physicochemical and biopharmaceutical behavior, and therapeutic efficacy. Nanomed. Nanotechnol. Biol. Med. 2019, 20. [Google Scholar] [CrossRef]
- Fang, J.Y.; Fang, C.L.; Liu, C.H.; Su, Y.H. Lipid nanoparticles as vehicles for topical psoralen delivery: Solid lipid nanoparticles (SLN) versus nanostructured lipid carriers (NLC). Eur. J. Pharm. Biopharm. 2008, 70, 633–640. [Google Scholar] [CrossRef]
- Cirri, M.; Bragagni, M.; Mennini, N.; Mura, P. Development of a new delivery system consisting in “drug—In cyclodextrin—In nanostructured lipid carriers” for ketoprofen topical delivery. Eur. J. Pharm. Biopharm. 2012, 80, 46–53. [Google Scholar] [CrossRef]
- Beloqui, A.; Solinís, M.Á.; Rodríguez-Gascón, A.; Almeida, A.J.; Préat, V. Nanostructured lipid carriers: Promising drug delivery systems for future clinics. Nanomed. Nanotechnol. Biol. Med. 2016, 12, 143–161. [Google Scholar] [CrossRef] [PubMed]
- Fang, C.-L.; Al-Suwayeh, S.; Fang, J.-Y. Nanostructured Lipid Carriers (NLCs) for Drug Delivery and Targeting. Recent Pat. Nanotechnol. 2013, 7, 41–55. [Google Scholar] [CrossRef] [PubMed]
- Ruktanonchai, U.; Bejrapha, P.; Sakulkhu, U.; Opanasopit, P.; Bunyapraphatsara, N.; Junyaprasert, V.; Puttipipatkhachorn, S. Physicochemical Characteristics, Cytotoxicity, and Antioxidant Activity of Three Lipid Nanoparticulate Formulations of Alpha-lipoic Acid. AAPS PharmSciTech 2009, 10, 227–234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iqbal, M.A.; Md, S.; Sahni, J.K.; Baboota, S.; Dang, S.; Ali, J. Nanostructured lipid carriers system: Recent advances in drug delivery. J. Drug Target. 2012, 20, 813–830. [Google Scholar] [CrossRef]
- Naseri, N.; Valizadeh, H.; Zakeri-Milani, P. Solid lipid nanoparticles and nanostructured lipid carriers: Structure preparation and application. Adv. Pharm. Bull. 2015, 5, 305–313. [Google Scholar] [CrossRef] [Green Version]
- Zhuang, C.Y.; Li, N.; Wang, M.; Zhang, X.N.; Pan, W.S.; Peng, J.J.; Pan, Y.S.; Tang, X. Preparation and characterization of vinpocetine loaded nanostructured lipid carriers (NLC) for improved oral bioavailability. Int. J. Pharm. 2010, 394, 179–185. [Google Scholar] [CrossRef]
- Vitorino, C.; Almeida, A.; Sousa, J.; Lamarche, I.; Gobin, P.; Marchand, S.; Couet, W.; Olivier, J.C.; Pais, A. Passive and active strategies for transdermal delivery using co-encapsulating nanostructured lipid carriers: In vitro vs. in vivo studies. Eur. J. Pharm. Biopharm. 2014, 86, 133–144. [Google Scholar] [CrossRef]
- Puglia, C.; Santonocito, D.; Ostacolo, C.; Sommella, E.M.; Campiglia, P.; Carbone, C.; Drago, F.; Pignatello, R.; Bucolo, C. Ocular formulation based on palmitoylethanolamide-loaded nanostructured lipid carriers: Technological and pharmacological profile. Nanomaterials 2020, 10, 287. [Google Scholar] [CrossRef] [Green Version]
- Bunjes, H.; Westesen, K.; Koch, M.H.J. Crystallization tendency and polymorphic transitions in triglyceride nanoparticles. Int. J. Pharm. 1996, 129, 159–173. [Google Scholar] [CrossRef]
- Liu, D.; Jiang, S.; Shen, H.; Qin, S.; Liu, J.; Zhang, Q.; Li, R.; Xu, Q. Diclofenac sodium-loaded solid lipid nanoparticles prepared by emulsion/solvent evaporation method. J. Nanopart. Res. 2011, 13, 2375–2386. [Google Scholar] [CrossRef]
- Mendes, I.T.; Ruela, A.L.M.; Carvalho, F.C.; Freitas, J.T.J.; Bonfilio, R.; Pereira, G.R. Development and characterization of nanostructured lipid carrier-based gels for the transdermal delivery of donepezil. Colloids Surf. B Biointerfaces 2019, 177, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Doktorovová, S.; Araújo, J.; Garcia, M.L.; Rakovský, E.; Souto, E.B. Formulating fluticasone propionate in novel PEG-containing nanostructured lipid carriers (PEG-NLC). Colloids Surf. B Biointerfaces 2010, 75, 538–542. [Google Scholar] [CrossRef] [PubMed]
- Joshi, M.; Patravale, V. Nanostructured lipid carrier (NLC) based gel of celecoxib. Int. J. Pharm. 2008, 346, 124–132. [Google Scholar] [CrossRef] [PubMed]
- Xia, Q.; Hao, X.; Lu, Y.; Xu, W.; Wei, H.; Ma, Q.; Gu, N. Production of drug-loaded lipid nanoparticles based on phase behaviors of special hot microemulsions. Colloids Surf. A Physicochem. Eng. Asp. 2008, 313–314, 27–30. [Google Scholar] [CrossRef]
- Esposito, E.; Drechsler, M.; Cortesi, R.; Nastruzzi, C. Encapsulation of cannabinoid drugs in nanostructured lipid carriers. Eur. J. Pharm. Biopharm. 2016, 102, 87–91. [Google Scholar] [CrossRef]
- Das, S.; Chaudhury, A. Recent Advances in Lipid Nanoparticle Formulations with Solid Matrix for Oral Drug Delivery. AAPS PharmSciTech 2011, 12, 62–76. [Google Scholar] [CrossRef] [Green Version]
- Kaur, P.; Mishra, V.; Shunmugaperumal, T.; Goyal, A.K.; Ghosh, G.; Rath, G. Inhalable spray dried lipidnanoparticles for the co-delivery of paclitaxel and doxorubicin in lung cancer. J. Drug Deliv. Sci. Technol. 2020, 56, 101502. [Google Scholar] [CrossRef]
- Freitas, C.; Müller, R.H. Spray-drying of solid lipid nanoparticles (SLN(TM)). Eur. J. Pharm. Biopharm. 1998, 46, 145–151. [Google Scholar] [CrossRef]
- Zhang, X.; Pan, W.; Gan, L.; Zhu, C.; Gan, Y.; Nie, S. Preparation of a dispersible PEGylate nanostructured lipid carriers (NLC) loaded with 10-hydroxycamptothecin by spray-drying. Chem. Pharm. Bull. 2008, 56, 1645–1650. [Google Scholar] [CrossRef] [Green Version]
- Xia, D.; Shrestha, N.; van de Streek, J.; Mu, H.; Yang, M. Spray drying of fenofibrate loaded nanostructured lipid carriers. Asian J. Pharm. Sci. 2016, 11, 507–515. [Google Scholar] [CrossRef] [Green Version]
- Zhong, Q.; Zhang, L. Nanoparticles fabricated from bulk solid lipids: Preparation, properties, and potential food applications. Adv. Colloid Interface Sci. 2019, 273, 102033. [Google Scholar] [CrossRef] [PubMed]
- Lababidi, N.; Sigal, V.; Koenneke, A.; Schwarzkopf, K.; Manz, A.; Schneider, M. Microfluidics as tool to prepare size-tunable PLGA nanoparticles with high curcumin encapsulation for efficient mucus penetration. Beilstein J. Nanotechnol. 2019, 10, 2280–2293. [Google Scholar] [CrossRef] [PubMed]
- Garg, S.; Heuck, G.; Ip, S.; Ramsay, E. Microfluidics: A transformational tool for nanomedicine development and production. J. Drug Target. 2016, 24, 821–835. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Liu, W.; Wan, J.; Cheng, X.; Gu, C.; Zhou, H.; Chen, S.; Zhao, X.; Tang, Y.; Yang, X. Preparation of Coenzyme Q10 nanostructured lipid carriers for epidermal targeting with high-pressure microfluidics technique. Drug Dev. Ind. Pharm. 2013, 39, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Üner, M. Characterization and imaging of solid lipid nanoparticles and nanostructured lipid carriers. In Handbook of Nanoparticles; Aliofkhazraei, M., Ed.; Springer: New York, NY, USA, 2015; pp. 117–141. ISBN 9783319153384. [Google Scholar]
- Peer, D.; Karp, J.M.; Hong, S.; Farokhzad, O.C.; Margalit, R.; Langer, R. Nanocarriers as an emerging platform for cancer therapy. Nat. Nanotechnol. 2007, 2, 751–760. [Google Scholar] [CrossRef] [PubMed]
- Danhier, F.; Feron, O.; Préat, V. To exploit the tumor microenvironment: Passive and active tumor targeting of nanocarriers for anti-cancer drug delivery. J. Control. Release 2010, 148, 135–146. [Google Scholar] [CrossRef]
- Teeranachaideekul, V.; Souto, E.B.; Junyaprasert, V.B.; Müller, R.H. Cetyl palmitate-based NLC for topical delivery of Coenzyme Q10—Development, physicochemical characterization and in vitro release studies. Eur. J. Pharm. Biopharm. 2007, 67, 141–148. [Google Scholar] [CrossRef]
- Moghimi, S.M.; Hunter, A.C.; Andresen, T.L. Factors Controlling Nanoparticle Pharmacokinetics: An Integrated Analysis and Perspective. Annu. Rev. Pharmacol. Toxicol. 2011, 52, 481–503. [Google Scholar] [CrossRef]
- Truong, N.P.; Whittaker, M.R.; Mak, C.W.; Davis, T.P. The importance of nanoparticle shape in cancer drug delivery. Expert Opin. Drug Deliv. 2015, 12, 129–142. [Google Scholar] [CrossRef]
- Tamjidi, F.; Shahedi, M.; Varshosaz, J.; Nasirpour, A. Nanostructured lipid carriers (NLC): A potential delivery system for bioactive food molecules. Innov. Food Sci. Emerg. Technol. 2013, 19, 29–43. [Google Scholar] [CrossRef]
- Xu, R. Progress in nanoparticles characterization: Sizing and zeta potential measurement. Particuology 2008, 6, 112–115. [Google Scholar] [CrossRef]
- Gonzalez-Mira, E.; Egea, M.A.; Souto, E.B.; Calpena, A.C.; García, M.L. Optimizing flurbiprofen-loaded NLC by central composite factorial design for ocular delivery. Nanotechnology 2011, 22, 045101. [Google Scholar] [CrossRef] [PubMed]
- Parveen, S.; Sahoo, S.K. Polymeric nanoparticles for cancer therapy. J. Drug Target. 2008, 16, 108–123. [Google Scholar] [CrossRef] [PubMed]
- How, C.W.; Rasedee, A.; Manickam, S.; Rosli, R. Tamoxifen-loaded nanostructured lipid carrier as a drug delivery system: Characterization, stability assessment and cytotoxicity. Colloids Surf. B Biointerfaces 2013, 112, 393–399. [Google Scholar] [CrossRef] [Green Version]
- Hu, F.Q.; Jiang, S.P.; Du, Y.Z.; Yuan, H.; Ye, Y.Q.; Zeng, S. Preparation and characteristics of monostearin nanostructured lipid carriers. Int. J. Pharm. 2006, 314, 83–89. [Google Scholar] [CrossRef]
- Han, F.; Li, S.; Yin, R.; Liu, H.; Xu, L. Effect of surfactants on the formation and characterization of a new type of colloidal drug delivery system: Nanostructured lipid carriers. Colloids Surf. A Physicochem. Eng. Asp. 2008, 315, 210–216. [Google Scholar] [CrossRef]
- Sanjula, B.; Shah, F.M.; Javed, A.; Alka, A. Effect of poloxamer 188 on lymphatic uptake of carvedilol-loaded solid lipid nanoparticles for bioavailability enhancement. J. Drug Target. 2009, 17, 249–256. [Google Scholar] [CrossRef]
- Jenning, V.; Gohla, S. Comparison of wax and glyceride solid lipid nanoparticles (SLN®). Int. J. Pharm. 2000, 196, 219–222. [Google Scholar] [CrossRef]
- Teeranachaideekul, V.; Müller, R.H.; Junyaprasert, V.B. Encapsulation of ascorbyl palmitate in nanostructured lipid carriers (NLC)-Effects of formulation parameters on physicochemical stability. Int. J. Pharm. 2007, 340, 198–206. [Google Scholar] [CrossRef]
- Jiang, H.; Pei, L.; Liu, N.; Li, J.; Li, Z.; Zhang, S. Etoposide-loaded nanostructured lipid carriers for gastric cancer therapy. Drug Deliv. 2016, 23, 1379–1382. [Google Scholar] [CrossRef] [Green Version]
- Emami, J.; Yousefian, H.; Sadeghi, H. Targeted nanostructured lipid carrier for brain delivery of artemisinin: Design, preparation, characterization, optimization and cell toxicity. J. Pharm. Pharm. Sci. 2018, 21, 225s–241s. [Google Scholar] [CrossRef] [PubMed]
- Sue Lee, C.; Koo, J. A review of acitretin, a systemic retinoid for the treatment of psoriasis. Expert Opin. Pharmacother. 2005, 6, 1725–1734. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Liu, F.; Liu, Z.; Wang, L.; Zhang, N. Tumor specific delivery and therapy by double-targeted nanostructured lipid carriers with anti-VEGFR-2 antibody. Mol. Pharm. 2011, 8, 2291–2301. [Google Scholar] [CrossRef] [PubMed]
- Castelli, F.; Puglia, C.; Sarpietro, M.G.; Rizza, L.; Bonina, F. Characterization of indomethacin-loaded lipid nanoparticles by differential scanning calorimetry. Int. J. Pharm. 2005, 304, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Zur Mühlen, A.; Schwarz, C.; Mehnert, W. Solid lipid nanoparticles (SLN) for controlled drug delivery—Drug release and release mechanism. Eur. J. Pharm. Biopharm. 1998, 45, 149–155. [Google Scholar] [CrossRef]
- El-Bahr, S.M. Effect of curcumin on hepatic antioxidant enzymes activities and gene expressions in rats intoxicated with aflatoxin B1. Phyther. Res. 2015, 29, 134–140. [Google Scholar] [CrossRef]
- Talegaonkar, S.; Bhattacharyya, A. Potential of Lipid Nanoparticles (SLNs and NLCs) in Enhancing Oral Bioavailability of Drugs with Poor Intestinal Permeability. AAPS PharmSciTech 2019, 20, 121. [Google Scholar] [CrossRef]
- Jansook, P.; Fülöp, Z.; Ritthidej, G.C. Amphotericin B loaded solid lipid nanoparticles (SLNs) and nanostructured lipid carrier (NLCs): Physicochemical and solid-solution state characterizations. Drug Dev. Ind. Pharm. 2019, 45, 560–567. [Google Scholar] [CrossRef]
- Müller, R.H.; Petersen, R.D.; Hommoss, A.; Pardeike, J. Nanostructured lipid carriers (NLC) in cosmetic dermal products. Adv. Drug Deliv. Rev. 2007, 59, 522–530. [Google Scholar] [CrossRef]
- Tikekar, R.V.; Nitin, N. Distribution of Encapsulated Materials in Colloidal Particles and Its Impact on Oxidative Stability of Encapsulated Materials. Langmuir 2012, 28, 9233–9243. [Google Scholar] [CrossRef]
- Riggs, B.L.; Hartmann, L.C. Selective estrogen-receptor modulators—Mechanisms of action and application to clinical practice. N. Engl. J. Med. 2003, 348, 1192. [Google Scholar] [CrossRef] [PubMed]
- Patil, P.H.; Belgamwar, V.S.; Patil, P.R.; Surana, S.J. Solubility Enhancement of Raloxifene Using Inclusion Complexes and Cogrinding Method. J. Pharm. 2013, 2013, 527380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shah, N.V.; Seth, A.K.; Balaraman, R.; Aundhia, C.J.; Maheshwari, R.A.; Parmar, G.R. Nanostructured lipid carriers for oral bioavailability enhancement of raloxifene: Design and in vivo study. J. Adv. Res. 2016, 7, 423–434. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Almousallam, M.; Moia, C.; Zhu, H. Development of nanostructured lipid carrier for dacarbazine delivery. Int. Nano Lett. 2015, 5, 241–248. [Google Scholar] [CrossRef] [Green Version]
- Breithaupt, H.; Dammann, A.; Aigner, K. Pharmacokinetics of dacarbazine (DTIC) and its metabolite 5-aminoimidazole-4-carboxamide (AIC) following different dose schedules. Cancer Chemother. Pharmacol. 1982, 9, 103–109. [Google Scholar] [CrossRef]
- Jia, T.; Zhang, L.; Duan, Y.; Zhang, M.; Wang, G.; Zhang, J.; Zhao, Z. The differential susceptibilities of MCF-7 and MDA-MB-231 cells to the cytotoxic effects of curcumin are associated with the PI3K/Akt-SKP2- Cip/Kips pathway. Cancer Cell Int. 2014, 14, 126. [Google Scholar] [CrossRef] [Green Version]
- Vecchi Brumatti, L.; Marcuzzi, A.; Tricarico, M.P.; Zanin, V.; Girardelli, M.; Bianco, M.A. Curcumin and Inflammatory Bowel Disease: Potential and Limits of Innovative Treatments. Molecules 2014, 19, 21127–21153. [Google Scholar] [CrossRef] [Green Version]
- Chen, Q.Y.; Jiao, D.M.; Wang, L.F.; Wang, L.; Hu, H.Z.; Song, J.; Yan, J.; Wu, L.J.; Shi, J.G. Curcumin inhibits proliferation-migration of NSCLC by steering crosstalk between a Wnt signaling pathway and an adherens junction via EGR-1. Mol. Biosyst. 2015, 11, 859–868. [Google Scholar] [CrossRef]
- Park, W.; Ruhul Amin, A.R.M.; Chen, Z.G.; Shin, D.M. New perspectives of curcumin in cancer prevention. Cancer Prev. Res. 2013, 6, 387–400. [Google Scholar] [CrossRef] [Green Version]
- Dong, X.; Wang, W.; Qu, H.; Han, D.; Zheng, J.; Sun, G. Targeted delivery of doxorubicin and vincristine to lymph cancer: Evaluation of novel nanostructured lipid carriers in vitro and in vivo. Drug Deliv. 2016, 23, 1374–1378. [Google Scholar] [CrossRef] [Green Version]
- Huang, Y.; He, L.; Liu, W.; Fan, C.; Zheng, W.; Wong, Y.-S.; Chen, T. Selective cellular uptake and induction of apoptosis of cancer-targeted selenium nanoparticles. Biomaterials 2013, 34, 7106–7116. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.G.; Kim, C.H.; Sung, S.W.; Lee, E.S.; Goh, M.S.; Yoon, H.Y.; Kang, M.J.; Lee, S.; Choi, Y.W. RIPL peptide-conjugated nanostructured lipid carriers for enhanced intracellular drug delivery to hepsin-expressing cancer cells. Int. J. Nanomed. 2018, 13, 3263–3278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Emami, J.; Rezazadeh, M.; Sadeghi, H.; Khadivar, K. Development and optimization of transferrin-conjugated nanostructured lipid carriers for brain delivery of paclitaxel using Box–Behnken design. Pharm. Dev. Technol. 2017, 22, 370–382. [Google Scholar] [CrossRef] [PubMed]
- Hu, C.M.J.; Fang, R.H.; Wang, K.C.; Luk, B.T.; Thamphiwatana, S.; Dehaini, D.; Nguyen, P.; Angsantikul, P.; Wen, C.H.; Kroll, A.V.; et al. Nanoparticle biointerfacing by platelet membrane cloaking. Nature 2015, 526, 118–121. [Google Scholar] [CrossRef] [PubMed]
- Bang, K.H.; Na, Y.G.; Huh, H.W.; Hwang, S.J.; Kim, M.S.; Kim, M.; Lee, H.K.; Cho, C.W. The delivery strategy of paclitaxel nanostructured lipid carrier coated with platelet membrane. Cancers 2019, 11, 807. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ong, Y.S.; Yazan, L.S.; Ng, W.K.; Abdullah, R.; Mustapha, N.M.; Sapuan, S.; Foo, J.B.; Tor, Y.S.; How, C.W.; Rahman, N.A.; et al. Thymoquinone loaded in nanostructured lipid carrier showed enhanced anticancer activity in 4T1 tumor-bearing mice. Nanomedicine 2018, 13, 1567–1582. [Google Scholar] [CrossRef] [Green Version]
- Esposito, E.; Mariani, P.; Ravani, L.; Contado, C.; Volta, M.; Bido, S.; Drechsler, M.; Mazzoni, S.; Menegatti, E.; Morari, M.; et al. Nanoparticulate lipid dispersions for bromocriptine delivery: Characterization and in vivo study. Eur. J. Pharm. Biopharm. 2012, 80, 306–314. [Google Scholar] [CrossRef]
- Subramony, J.A. Apomorphine in dopaminergic therapy. Mol. Pharm. 2006, 3, 380–385. [Google Scholar] [CrossRef]
- Hsu, S.H.; Wen, C.J.; Al-Suwayeh, S.A.; Chang, H.W.; Yen, T.C.; Fang, J.Y. Physicochemical characterization and in vivo bioluminescence imaging of nanostructured lipid carriers for targeting the brain: Apomorphine as a model drug. Nanotechnology 2010, 21, 405101. [Google Scholar] [CrossRef]
- Mu, X.; He, G.R.; Yuan, X.; Li, X.X.; Du, G.H. Baicalein protects the brain against neuron impairments induced by MPTP in C57BL/6 mice. Pharmacol. Biochem. Behav. 2011, 98, 286–291. [Google Scholar] [CrossRef]
- Tsai, M.J.; Wu, P.C.; Huang, Y.B.; Chang, J.S.; Lin, C.L.; Tsai, Y.H.; Fang, J.Y. Baicalein loaded in tocol nanostructured lipid carriers (tocol NLCs) for enhanced stability and brain targeting. Int. J. Pharm. 2012, 423, 461–470. [Google Scholar] [CrossRef]
- Gazak, R.; Walterova, D.; Kren, V. Silybin and Silymarin—New and Emerging Applications in Medicine. Curr. Med. Chem. 2007, 14, 315–338. [Google Scholar] [CrossRef]
- Jia, L.; Zhang, D.; Li, Z.; Duan, C.; Wang, Y.; Feng, F.; Wang, F.; Liu, Y.; Zhang, Q. Nanostructured lipid carriers for parenteral delivery of silybin: Biodistribution and pharmacokinetic studies. Colloids Surf. B Biointerfaces 2010, 80, 213–218. [Google Scholar] [CrossRef]
- Pan, S.-Y.; Yang, R.; Dong, H.; Yu, Z.; Ko, K.-M. Bifendate treatment attenuates hepatic steatosis in cholesterol/bile salt- and high-fat diet-induced hypercholesterolemia in mice. Eur. J. Pharmacol. 2006, 552, 170–175. [Google Scholar] [CrossRef]
- Feng, F.; Zheng, D.; Zhang, D.; Duan, C.; Wang, Y.; Jia, L.; Wang, F.; Liu, Y.; Gao, Q.; Zhang, Q. Preparation, characterization and biodistribution of nanostructured lipid carriers for parenteral delivery of bifendate. J. Microencapsul. 2011, 28, 280–285. [Google Scholar] [CrossRef]
- Ohtani, M. Basic pharmacology of buprenorphine. Eur. J. Pain Suppl. 2007, 1, 69–73. [Google Scholar] [CrossRef]
- Wang, J.J.; Liu, K.S.; Sung, K.C.; Tsai, C.Y.; Fang, J.Y. Lipid nanoparticles with different oil/fatty ester ratios as carriers of buprenorphine and its prodrugs for injection. Eur. J. Pharm. Sci. 2009, 38, 138–146. [Google Scholar] [CrossRef]
- Xu, X.; Zhao, C.; Yang, H.; Jian, Y.; Zhang, Z.; Huang, Y. Anti-inflammatory activity of injectable dexamethasone acetate-loaded nanostructured lipid carriers. Drug Deliv. 2011, 18, 485–492. [Google Scholar] [CrossRef]
- Štecová, J.; Mehnert, W.; Blaschke, T.; Kleuser, B.; Sivaramakrishnan, R.; Zouboulis, C.C.; Seltmann, H.; Korting, H.C.; Kramer, K.D.; Schäfer-Korting, M. Cyproterone acetate loading to lipid nanoparticles for topical acne treatment: Particle characterisation and skin uptake. Pharm. Res. 2007, 24, 991–1000. [Google Scholar] [CrossRef]
- Agrawal, Y.; Petkar, K.C.; Sawant, K.K. Development, evaluation and clinical studies of Acitretin loaded nanostructured lipid carriers for topical treatment of psoriasis. Int. J. Pharm. 2010, 401, 93–102. [Google Scholar] [CrossRef]
- Stern, R.S. Psoralen and Ultraviolet A Light Therapy for Psoriasis. N. Engl. J. Med. 2007, 357, 682. [Google Scholar] [CrossRef]
- González-Mira, E.; Nikolić, S.; García, M.L.; Egea, M.A.; Souto, E.B.; Calpena, A.C. Potential use of nanostructured lipid carriers for topical delivery of flurbiprofen. J. Pharm. Sci. 2011, 100, 242–251. [Google Scholar] [CrossRef]
- Han, F.; Li, S.; Yin, R.; Shi, X.; Jia, Q. Investigation of nanostructured lipid carriers for transdermal delivery of flurbiprofen. Drug Dev. Ind. Pharm. 2008, 34, 453–458. [Google Scholar] [CrossRef]
- Sütő, B.; Berkó, S.; Kozma, G.; Kukovecz, Á.; Budai-Szucs, M.; Erös, G.; Kemény, L.; Sztojkov-Ivanov, A.; Gáspár, R.; Csányi, E. Development of ibuprofen-loaded nanostructured lipid carrier-based gels: Characterization and investigation of in vitro and in vivo penetration through the skin. Int. J. Nanomed. 2016, 11, 1201–1212. [Google Scholar]
- Kang, Q.; Liu, J.; Zhao, Y.; Liu, X.; Liu, X.-Y.; Wang, Y.-J.; Mo, N.-L.; Wu, Q. Transdermal delivery system of nanostructured lipid carriers loaded with Celastrol and Indomethacin: Optimization, characterization and efficacy evaluation for rheumatoid arthritis. Artif. Cells, Nanomed. Biotechnol. 2018, 46, S585–S597. [Google Scholar] [CrossRef]
- Joshi, M.; Patravale, V. Formulation and Evaluation of Nanostructured Lipid Carrier (NLC)–based Gel of Valdecoxib. Drug Dev. Ind. Pharm. 2006, 32, 911–918. [Google Scholar] [CrossRef]
- Pathak, P.; Nagarsenker, M. Formulation and Evaluation of Lidocaine Lipid Nanosystems for Dermal Delivery. AAPS PharmSciTech 2009, 10, 985–992. [Google Scholar] [CrossRef]
- Puglia, C.; Sarpietro, M.G.; Bonina, F.; Castelli, F.; Zammataro, M.; Chiechio, S. Development, characterization, and in vitro and in vivo evaluation of benzocaine- and lidocaine-loaded nanostructrured lipid carriers. J. Pharm. Sci. 2011, 100, 1892–1899. [Google Scholar] [CrossRef]
- Junyaprasert, V.B.; Teeranachaideekul, V.; Souto, E.B.; Boonme, P.; Müller, R.H. Q10-loaded NLC versus nanoemulsions: Stability, rheology and in vitro skin permeation. Int. J. Pharm. 2009, 377, 207–214. [Google Scholar] [CrossRef]
- Graf, J. Antioxidants and skin care: The essentials. Plast. Reconstr. Surg. 2010, 125, 378–383. [Google Scholar] [CrossRef]
- Pardeike, J.; Schwabe, K.; Müller, R.H. Influence of nanostructured lipid carriers (NLC) on the physical properties of the Cutanova Nanorepair Q10 cream and the in vivo skin hydration effect. Int. J. Pharm. 2010, 396, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Roberts, R.L.; Green, J.; Lewis, B. Lutein and zeaxanthin in eye and skin health. Clin. Dermatol. 2009, 27, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Mitri, K.; Shegokar, R.; Gohla, S.; Anselmi, C.; Müller, R.H. Lipid nanocarriers for dermal delivery of lutein: Preparation, characterization, stability and performance. Int. J. Pharm. 2011, 414, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Khalil, R.M.; Abd-Elbary, A.; Kassem, M.A.; Ghorab, M.M.; Basha, M. Nanostructured lipid carriers (NLCs) versus solid lipid nanoparticles (SLNs) for topical delivery of meloxicam. Pharm. Dev. Technol. 2014, 19, 304–314. [Google Scholar] [CrossRef]
- Souto, E.B.; Wissing, S.A.; Barbosa, C.M.; Müller, R.H. Development of a controlled release formulation based on SLN and NLC for topical clotrimazole delivery. Int. J. Pharm. 2004, 278, 71–77. [Google Scholar] [CrossRef]
- Nikolić, S.; Keck, C.M.; Anselmi, C.; Müller, R.H. Skin photoprotection improvement: Synergistic interaction between lipid nanoparticles and organic UV filters. Int. J. Pharm. 2011, 414, 276–284. [Google Scholar] [CrossRef]
- Puglia, C.; Bonina, F.; Rizza, L.; Blasi, P.; Schoubben, A.; Perrotta, R.; Tarico, M.S.; Damiani, E. Lipid nanoparticles as carrier for octyl-methoxycinnamate: In vitro percutaneous absorption and photostability studies. J. Pharm. Sci. 2012, 101, 301–311. [Google Scholar] [CrossRef]
- Jain, S.K.; Agrawal, G.P.; Jain, N.K. A novel calcium silicate based microspheres of repaglinide: In vivo investigations. J. Control. Release 2006, 113, 111–116. [Google Scholar] [CrossRef]
- Qi, S.; Marchaud, D.; Craig, D.Q.M. An investigation into the mechanism of dissolution rate enhancement of poorly water-soluble drugs from spray chilled gelucire 50/13 microspheres. J. Pharm. Sci. 2010, 99, 262–274. [Google Scholar] [CrossRef]
- Date, A.A.; Vador, N.; Jagtap, A.; Nagarsenker, M.S. Lipid nanocarriers (GeluPearl) containing amphiphilic lipid Gelucire 50/13 as a novel stabilizer: Fabrication, characterization and evaluation for oral drug delivery. Nanotechnology 2011, 22, 275102. [Google Scholar] [CrossRef]
- Fathi, H.A.; Allam, A.; Elsabahy, M.; Fetih, G.; El-Badry, M. Nanostructured lipid carriers for improved oral delivery and prolonged antihyperlipidemic effect of simvastatin. Colloids Surf. B Biointerfaces 2018, 162, 236–245. [Google Scholar] [CrossRef]
- Chen, C.C.; Tsai, T.H.; Huang, Z.R.; Fang, J.Y. Effects of lipophilic emulsifiers on the oral administration of lovastatin from nanostructured lipid carriers: Physicochemical characterization and pharmacokinetics. Eur. J. Pharm. Biopharm. 2010, 74, 474–482. [Google Scholar] [CrossRef]
- Araújo, J.; Nikolic, S.; Egea, M.A.; Souto, E.B.; Garcia, M.L. Nanostructured lipid carriers for triamcinolone acetonide delivery to the posterior segment of the eye. Colloids Surf. B Biointerfaces 2011, 88, 150–157. [Google Scholar] [CrossRef]
- Liu, R.; Liu, Z.; Zhang, C.; Zhang, B. Nanostructured lipid carriers as novel ophthalmic delivery system for mangiferin: Improving in vivo ocular bioavailability. J. Pharm. Sci. 2012, 101, 3833–3844. [Google Scholar] [CrossRef]
- Gonzalez-Mira, E.; Sa, S.; C, N.; Calpena, A.C.; Egea, M.A.; Souto, E.B.; Luisa, M.; Ia, G. Improved and Safe Transcorneal Delivery of Flurbiprofen by NLC and NLC-Based Hydrogels. J. Pharm. Sci. 2011, 101, 707–725. [Google Scholar] [CrossRef]
- Tian, B.; Luo, Q.; Song, S.; Liu, D.; Pan, H.; Zhang, W.; He, L.; Ma, S.; Yang, X.; Pan, W. Novel surface-modified nanostructured lipid carriers with partially deacetylated water-soluble chitosan for efficient ocular delivery. J. Pharm. Sci. 2012, 101, 1040–1049. [Google Scholar] [CrossRef]
- Gade, S.; Patel, K.K.; Gupta, C.; Anjum, M.M.; Deepika, D.; Agrawal, A.K.; Singh, S. An Ex Vivo Evaluation of Moxifloxacin Nanostructured Lipid Carrier Enriched In Situ Gel for Transcorneal Permeation on Goat Cornea. J. Pharm. Sci. 2019, 108, 2905–2916. [Google Scholar] [CrossRef]
- Pardeike, J.; Weber, S.; Haber, T.; Wagner, J.; Zarfl, H.P.; Plank, H.; Zimmer, A. Development of an Itraconazole-loaded nanostructured lipid carrier (NLC) formulation for pulmonary application. Int. J. Pharm. 2011, 419, 329–338. [Google Scholar] [CrossRef]
- Nafee, N.; Makled, S.; Boraie, N. Nanostructured lipid carriers versus solid lipid nanoparticles for the potential treatment of pulmonary hypertension via nebulization. Eur. J. Pharm. Sci. 2018, 125, 151–162. [Google Scholar] [CrossRef]
- Patil-Gadhe, A.; Kyadarkunte, A.; Patole, M.; Pokharkar, V. Montelukast-loaded nanostructured lipid carriers: Part II Pulmonary drug delivery and in vitro–in vivo aerosol performance. Eur. J. Pharm. Biopharm. 2014, 88, 169–177. [Google Scholar] [CrossRef]
- Yang, J.; Ju, Z.; Dong, S. Cisplatin and paclitaxel co-delivered by folate-decorated lipid carriers for the treatment of head and neck cancer. Drug Deliv. 2017, 241, 792–799. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, J.; Xiao, X.; Zhu, J.; Gao, Z.; Lai, X.; Zhu, X.; Mao, G. Lactoferrin- and RGD-comodified, temozolomide and vincristine-coloaded nanostructured lipid carriers for gliomatosis cerebri combination therapy. Int. J. Nanomed. 2018, 13, 3039–3051. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liang, Y.; Tian, B.; Zhang, J.; Li, K.; Wang, L.; Han, J.; Wu, Z. Tumor-targeted polymeric nanostructured lipid carriers with precise ratiometric control over dual-drug loading for combination therapy in non-small-cell lung cancer. Int. J. Nanomed. 2017, 12, 1699–1715. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doktorovová, S.; Kovačević, A.B.; Garcia, M.L.; Souto, E.B. Preclinical safety of solid lipid nanoparticles and nanostructured lipid carriers: Current evidence from in vitro and in vivo evaluation. Eur. J. Pharm. Biopharm. 2016, 108, 235–252. [Google Scholar] [CrossRef]
- Akanda, M.H.; Rai, R.; Slipper, I.J.; Chowdhry, B.Z.; Lamprou, D.; Getti, G.; Douroumis, D. Delivery of retinoic acid to LNCap human prostate cancer cells using solid lipid nanoparticles. Int. J. Pharm. 2015, 493, 161–171. [Google Scholar] [CrossRef] [Green Version]
- Almeida, H.; Lobão, P.; Frigerio, C.; Fonseca, J.; Silva, R.; Sousa Lobo, J.M.; Amaral, M.H. Preparation, characterization and biocompatibility studies of thermoresponsive eyedrops based on the combination of nanostructured lipid carriers (NLC) and the polymer Pluronic F-127 for controlled delivery of ibuprofen. Pharm. Dev. Technol. 2017, 22, 336–349. [Google Scholar] [CrossRef]
- Hwang, T.-L.; Aljuffali, I.A.; Hung, C.-F.; Chen, C.-H.; Fang, J.-Y. The impact of cationic solid lipid nanoparticles on human neutrophil activation and formation of neutrophil extracellular traps (NETs). Chem. Biol. Interact. 2015, 235, 106–114. [Google Scholar] [CrossRef]
- Hwang, T.-L.; Aljuffali, I.A.; Lin, C.-F.; Chang, Y.-T.; Fang, J.-Y. Cationic additives in nanosystems activate cytotoxicity and inflammatory response of human neutrophils: Lipid nanoparticles versus polymeric nanoparticles. Int. J. Nanomed. 2015, 10, 371–385. [Google Scholar]
- Müller, R.H.; Rühl, D.; Runge, S.; Schulze-Forster, K.; Mehnert, W. Cytotoxicity of solid lipid nanoparticles as a function of the lipid matrix and the surfactant. Pharm. Res. 1997, 14, 458–462. [Google Scholar] [CrossRef]
- Schubert, M.A.; Müller-Goymann, C.C. Characterisation of surface-modified solid lipid nanoparticles (SLN): Influence of lecithin and nonionic emulsifier. Eur. J. Pharm. Biopharm. 2005, 61, 77–86. [Google Scholar] [CrossRef]
- Brugè, F.; Damiani, E.; Puglia, C.; Offerta, A.; Armeni, T.; Littarru, G.P.; Tiano, L. Nanostructured lipid carriers loaded with CoQ10: Effect on human dermal fibroblasts under normal and UVA-mediated oxidative conditions. Int. J. Pharm. 2013, 455, 348–356. [Google Scholar] [CrossRef]
- Lakkadwala, S.; Nguyen, S.; Lawrence, J.; Nauli, S.M.; Nesamony, J. Physico-chemical characterisation, cytotoxic activity, and biocompatibility studies of tamoxifen-loaded solid lipid nanoparticles prepared via a temperature-modulated solidification method. J. Microencapsul. 2014, 31, 590–599. [Google Scholar] [CrossRef] [PubMed]
- Doktorovova, S.; Souto, E.B.; Silva, A.M. Nanotoxicology applied to solid lipid nanoparticles and nanostructured lipid carriers—A systematic review of in vitro data. Eur. J. Pharm. Biopharm. 2014, 87, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Kyadarkunte, A.Y.; Patole, M.S.; Pokharkar, V.B. Cellular interactions and photoprotective effects of idebenone-loaded nanostructured lipid carriers stabilized using PEG-free surfactant. Int. J. Pharm. 2015, 479, 77–87. [Google Scholar] [CrossRef]
- Vallianou, N.G.; Evangelopoulos, A.; Schizas, N.; Kazazis, C. Potential anticancer properties and mechanisms of action of curcumin. Anticancer Res. 2015, 35, 645–651. [Google Scholar]
- Del Pozo-Rodríguez, A.; Delgado, D.; Gascón, A.R.; Solinís, M.Á. Lipid nanoparticles as drug/gene delivery systems to the retina. J. Ocul. Pharmacol. Ther. 2013, 29, 173–188. [Google Scholar] [CrossRef]
- Rao, M.P.; Manjunath, K.; Bhagawati, S.T.; Thippeswami, B.S. Bixin loaded solid lipid nanoparticles for enhanced hepatoprotection—Preparation, characterisation and in vivo evaluation. Int. J. Pharm. 2014, 473, 485–492. [Google Scholar] [CrossRef]
- Kasongo, K.W.; Pardeike, J.; Müller, R.H.; Walker, R.B. Selection and characterization of suitable lipid excipients for use in the manufacture of didanosine-loaded solid lipid nanoparticles and nanostructured lipid carriers. J. Pharm. Sci. 2011, 100, 5185–5196. [Google Scholar] [CrossRef]
- Han, Y.; Li, Y.; Zhang, P.; Sun, J.; Li, X.; Sun, X.; Kong, F. Nanostructured lipid carriers as novel drug delivery system for lung cancer gene therapy. Pharm. Dev. Technol. 2016, 21, 277–281. [Google Scholar] [CrossRef]
- Wang, H.; Liu, S.; Jia, L.; Chu, F.; Zhou, Y.; He, Z.; Guo, M.; Chen, C.; Xu, L. Nanostructured lipid carriers for MicroRNA delivery in tumor gene therapy. Cancer Cell Int. 2018, 18, 101. [Google Scholar] [CrossRef]





| Type | Name | References |
|---|---|---|
| Solid lipids | Glyceryl monostearate | [9,15,16,17] |
| Glyceryl tridecanoate | [18] | |
| Glyceryl tripalmitate | [18,19] | |
| Glyceryl behenate (Compritol® 888 ATO) | [20,21,22,23] | |
| Stearic acid | [16,24,25] | |
| Glyceryl distearate (Precirol® ATO 5) | [21,23,26,27,28] | |
| Liquid lipids | Oleic acid | [15,17,22,25] |
| Alpha-tocopheryl acetate | [18] | |
| Squalene | [21,29] | |
| Medium chain triglycerides (MCT)/caprylic and capric triglycerides | [20,23] | |
| PEG-8 caprylic/capric glycerides (Labrasol®) | [28,30] | |
| propylene glycol dicaprylocaprate (LabrafacTM PG) | [30] | |
| Soy lecithin (Epikuron™200) | [31] | |
| Surfactants | Soybean phosphatidylcholine | [18,20] |
| Hydrogenated soybean phosphatidylcholine | [21] | |
| Lecithin | [25] | |
| Solutol® HS 15 (poly-oxyethylene esters of 12-hydroxystearic acid) | [17] | |
| Soy lecithin (Epikuron™200) | [16,18,32] | |
| Pluronic® F-68 (Poloxamer 188) | [16,17,27,32] | |
| Pluronic F127 (poloxamer 407) | [9,23] | |
| Tween® 80 | [19,21,27] | |
| Cremophor® RH40 (PEG-40 Hydrogenated Castor Oil) | [9,23] | |
| Kolliphor® EL (Polyoxyl castor oil) | [9] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haider, M.; Abdin, S.M.; Kamal, L.; Orive, G. Nanostructured Lipid Carriers for Delivery of Chemotherapeutics: A Review. Pharmaceutics 2020, 12, 288. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics12030288
Haider M, Abdin SM, Kamal L, Orive G. Nanostructured Lipid Carriers for Delivery of Chemotherapeutics: A Review. Pharmaceutics. 2020; 12(3):288. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics12030288
Chicago/Turabian StyleHaider, Mohamed, Shifaa M. Abdin, Leena Kamal, and Gorka Orive. 2020. "Nanostructured Lipid Carriers for Delivery of Chemotherapeutics: A Review" Pharmaceutics 12, no. 3: 288. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics12030288