The Impact of Measures Recommended by the Government to Limit the Spread of Coronavirus (COVID-19) on Physical Activity Levels, Quality of Life, and Mental Health of Brazilians
Abstract
:1. Introduction
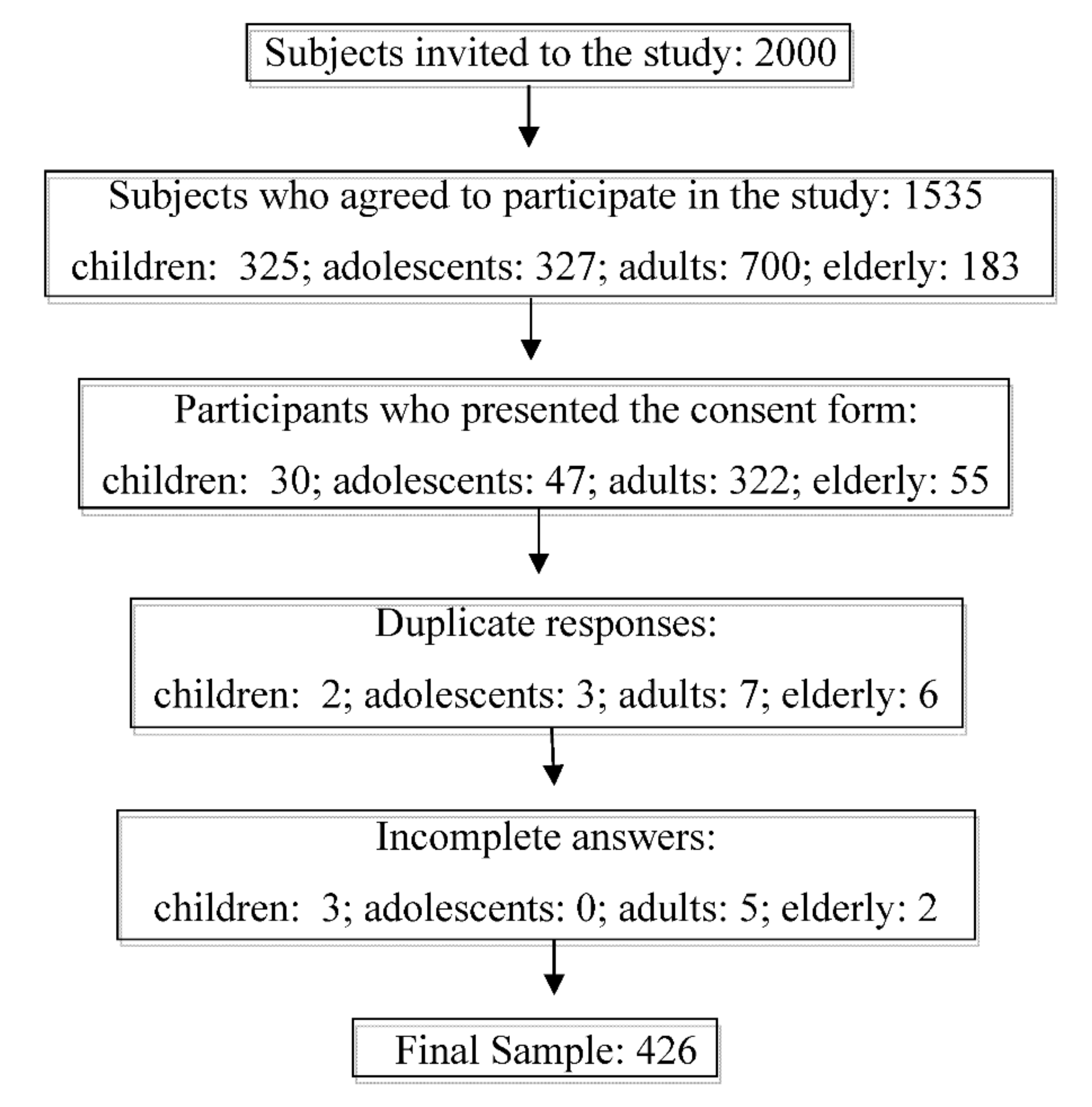
2. Methods
3. Sample
4. Questionnaire
International Physical Activity Questionnaire (IPAQ)
5. Short form Survey-36 (SF-36)
6. Stress Perception Scale
7. Basal Metabolic Rate (BMR)
8. Analyses
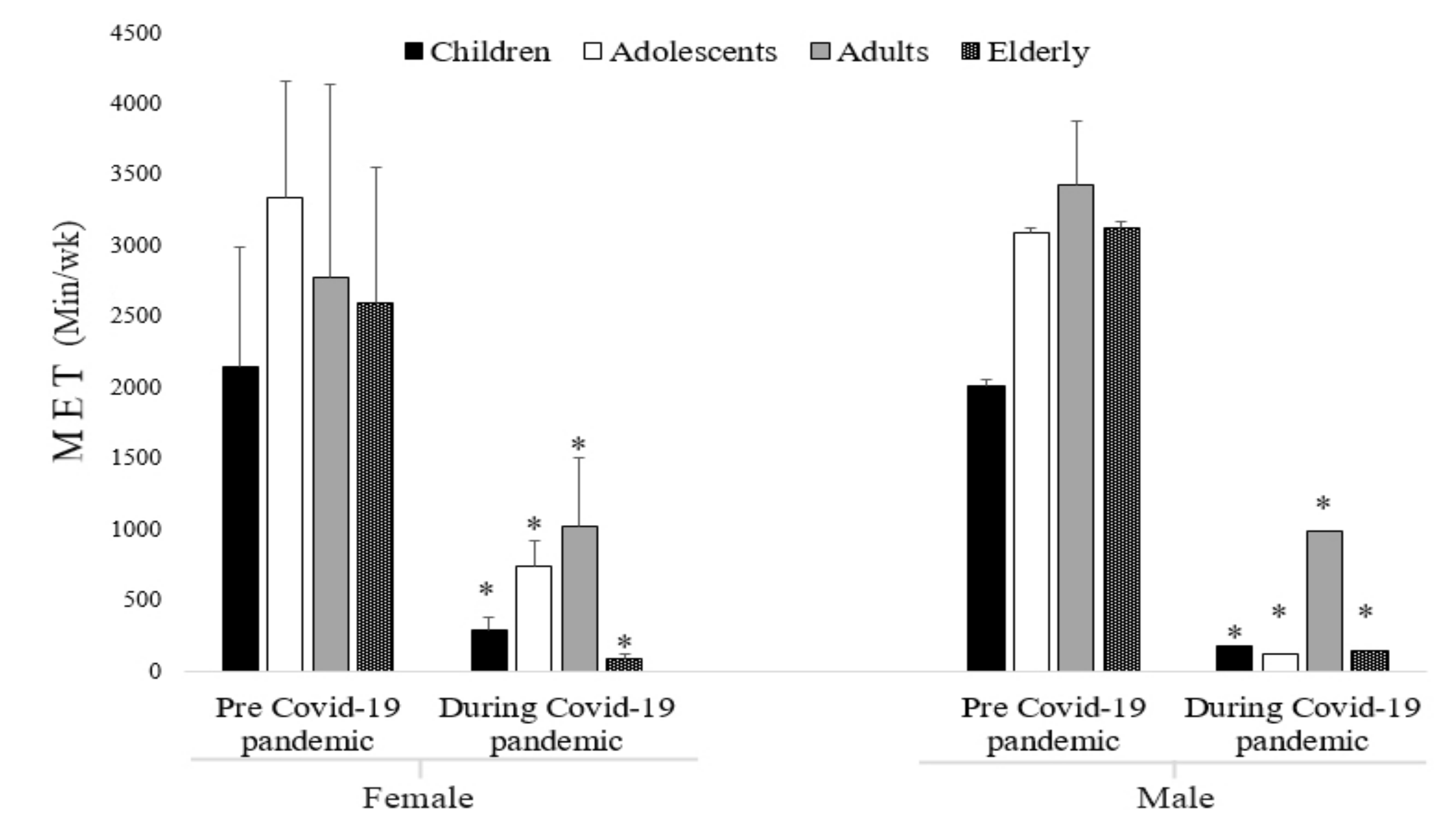
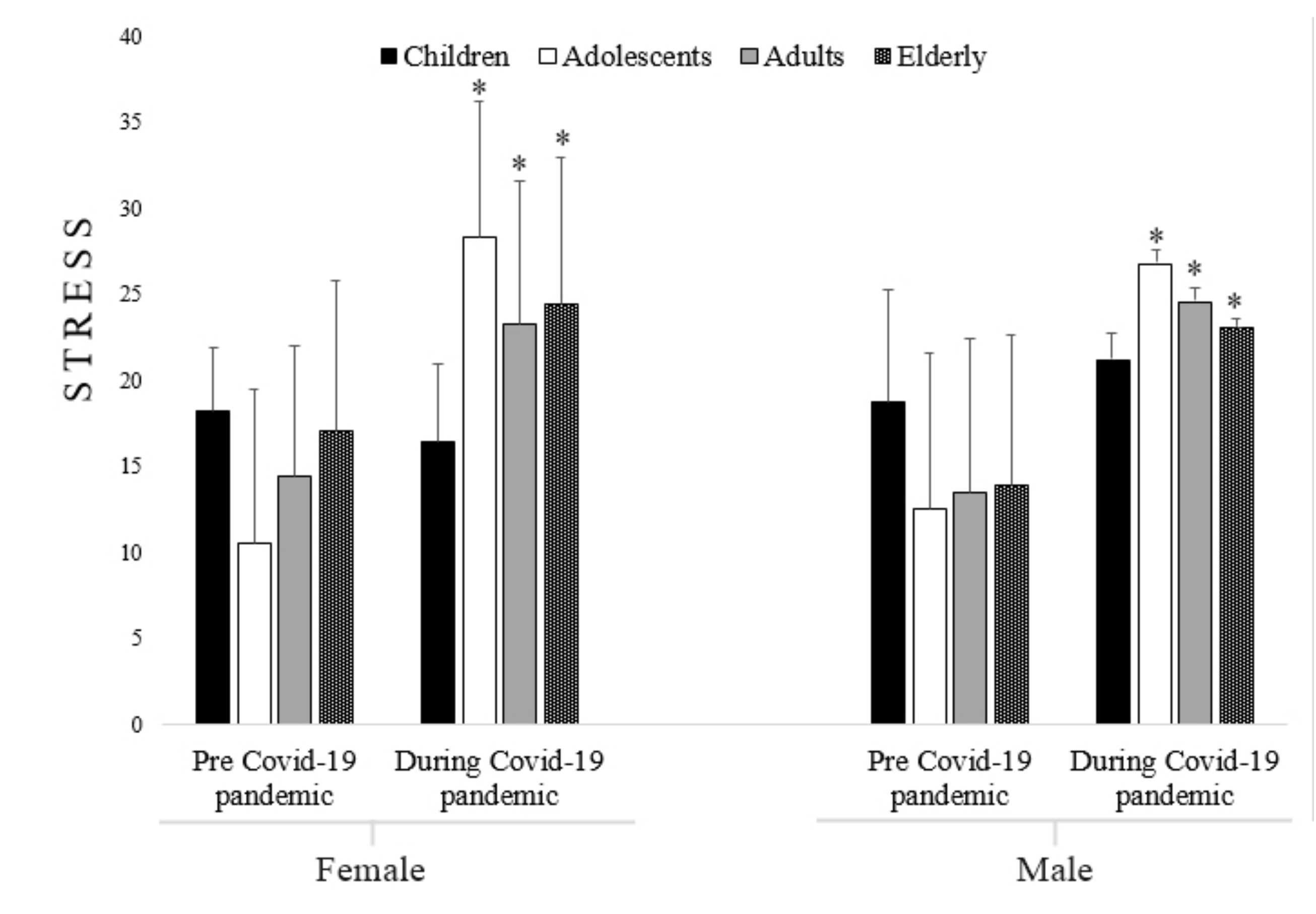
9. Results
10. Discussion
11. Mitigation Strategies to Keep Active
12. Children and Adolescents
13. Adults and Elderly
14. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Coronavirus Disease 2019 (COVID-19) Situation Report—23; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Gorbalenya, A.E.; Baker, S.C.; Baric, R.; Groot, R.J.D.; Drosten, C.; Gulyaeva, A.A.; Penzar, D. Severe acute respiratory syndrome-related coronavirus: The species and its viruses–a statement of the Coronavirus Study Group. bioRxiv 2020, 10, 07-937862. [Google Scholar]
- Hopmeyer, A.; Medovoy, T. Emerging adults’ self-identified peer crowd affiliations, risk behavior, and social–emotional adjustment in college. Emerg. Adulthood 2017, 5, 143–148. [Google Scholar] [CrossRef]
- Peçanha, T.; Goessler, K.F.; Roschel, H.; Gualano, B. Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. Am. J. Physiol. Heart Circ. Physiol. 2020, 318, H1441–H1446. [Google Scholar] [CrossRef] [PubMed]
- Fitbit, Inc. The Impact of Coronavirus on Global Activity (Online). Available online: https://blog.fitbit.com/covid-19-global-activity/ (accessed on 25 June 2020).
- Belavý, D.L.; Gast, U.; Daumer, M.; Fomina, E.; Rawer, R.; Schießl, H.; Felsenberg, D. Progressive adaptation in physical activity and neuromuscular performance during 520d confinement. PLoS ONE 2013, 8, e60090. [Google Scholar] [CrossRef] [Green Version]
- Herbolsheimer, F.; Ungar, N.; Peter, R. Why is social isolation among older adults associated with depressive symptoms? The mediating role of out-of-home physical activity. Int. J. Behav. Med. 2018, 25, 649–657. [Google Scholar] [CrossRef]
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef] [Green Version]
- Hallal, P.C.; Victora, C.G. Reliability and validity of the International Physical Activity Questionnaire (IPAQ). Med. Sci. Sports Exerc. 2004, 36, 556. [Google Scholar] [CrossRef]
- Ainsworth, B.E.; Haskell, W.L.; Leon, A.S.; Jacobs, D.R., Jr.; Montoye, H.J.; Sallis, J.F.; Paffenbarger, R.S., Jr. Compendium of physical activities: Classification of energy costs of human physical activities. Med. Scie Sports Exer. 1993, 25, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Nithyashri, J.; Kulanthaivel, G. Classification of human age based on Neural Network using FG-NET Aging database and Wavelets. In Proceedings of the 2012 Fourth International Conference on Advanced Computing (ICoAC), Chennai, India, 13–15 December 2012. [Google Scholar]
- Matsudo, S.; Araújo, T.; Marsudo, V.; Andrade, D.; Andrade, E.; Braggion, G. International Physical Activity Questionnaire (IPAQ): Study of validity and reproducibility in Brazil. Braz. J. Phys. Act. Health (Rev Bras AtivFisSaúde) 2001, 6, 5–18. [Google Scholar]
- de Souza, B.V.; Dias, R.; Correa, D.A. The use of the international physical activity questionnaire (IPAQ) as a diagnostic tool for the level of physical fitness: A review in Brazil. Saúde Rev. 2012, 12, 49–54. [Google Scholar]
- Ciconelli, R.M.; Ferraz, M.B.; Santos, W.; Meinão, I.; Quaresma, M.R. Translation into Portuguese and validation of the generic SF-36 quality of life assessment questionnaire (Brazil SF-36). Rev. Bras. Reumatol. 1999, 39, 143–150. [Google Scholar]
- Stanghelle, B.; Bentzen, H.; Giangregorio, L.; Pripp, A.H.; Skelton, D.; Bergland, A. Effects of a resistance and balance exercise programme on physical fitness, health-related quality of life and fear of falling in older women with osteoporosis and vertebral fracture: A randomized controlled trial. Osteoporos. Intern. 2020, 31, 1069–1078. [Google Scholar] [CrossRef]
- Lopez-Nava, G.; Asokkumar, R.; Lacruz, T.; Rull, A.; Beltran, L.; Bautista-Castaño, I. The effect of weight loss and exercise on Health-Related Quality of Life (HRQOL) following Endoscopic Bariatric Therapies (EBT) for obesity. Health Q. Life Outcomes 2020, 18, 1–9. [Google Scholar]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.A.; Benedict, F.G. A biometric study of human basal metabolism. PNAS 1918, 4, 370. [Google Scholar] [CrossRef] [Green Version]
- Espirito-Santo, H.; Daniel, F. Calculating and reporting effect sizes on scientific papers (1): p<0.05 limitations in the analysis of mean differences of two groups. Rev. Port. Investig. Comport. Soc. 2015, 1, 3–16. [Google Scholar]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Costa, C.L.A.; Costa, T.M.; Barbosa-Filho, V.C.; Bandeira, P.F.R.; Siqueira, R.C.L. Influência do distanciamento social no nível de atividade física durante a pandemia do COVID-19. Rev. Bras. Ativ. Fís. Saúde 2020, 25, 1–6. [Google Scholar] [CrossRef]
- Pinto, A.J.; Dunstan, D.W.; Owen, N.; Bonfá, E.; Gualano, B. Combating physical inactivity during the COVID-19 pandemic. Nat. Rev. Rheumat. 2020, 16, 347–348. [Google Scholar] [CrossRef]
- Reis, R.S.; Salvo, D.; Ogilvie, D.; Lambert, E.V.; Goenka, S.; Brownson, R.C. Lancet Physical Activity Series 2 Executive Committee. Scaling up physical activity interventions worldwide: Stepping up to larger and smarter approaches to get people moving. Lancet 2016, 388, 1337–1348. [Google Scholar] [CrossRef] [Green Version]
- Brazendale, K.; Beets, M.W.; Weaver, R.G.; Pate, R.R.; Turner-McGrievy, G.M.; Kaczynski, A.T.; von Hippel, P.T. Understanding differences between summer vs. school obesogenic behaviors of children: The structured days hypothesis. Intern. J. Behav. Nut. Phys. Activ. 2017, 14, 100. [Google Scholar] [CrossRef] [PubMed]
- Ekelund, U.; Steene-Johannessen, J.; Brown, W.J.; Fagerland, M.W.; Owen, N.; Powell, K.E. Lancet Sedentary Behaviour Working Group. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016, 388, 1302–1310. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. More Active People for a Healthier World: Global Action Plan on Physical Activity 2018–2030; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Wang, G.; Zhang, Y.; Zhao, J.; Zhang, J.; Jiang, F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet 2020, 395, 945–947. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult in patients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Marković, B.; Arsovski, S. Emotional design and quality of life. Center Qual. 2007, 20, 141. [Google Scholar] [CrossRef] [Green Version]
- Dubey, S.; Biswas, P.; Ghosh, R.; Chatterjee, S.; Dubey, M.J.; Chatterjee, S.; Lavie, C.J. Psychosocial impact of COVID-19. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 779–788. [Google Scholar] [CrossRef]
- Imran, N.; Zeshan, M.; Pervaiz, Z. Mental health considerations for children & adolescents in COVID-19 Pandemic. Pakistan J. Med. Scie. 2020, 36. [Google Scholar] [CrossRef]
- Li, S.; Wang, Y.; Xue, J.; Zhao, N.; Zhu, T. The impact of COVID-19 epidemic declaration on psychological consequences: A study on active Weibo users. Int. J. Environ. Res. Public Health 2020, 17, 2032. [Google Scholar] [CrossRef] [Green Version]
- Schmidt, B.; Crepaldi, M.A.; Bolze, S.D.A.; Neiva-Silva, L.; Demenech, L.M. Impacts on Mental Health and Psychological Interventions Faced with the New Coronavirus Pandemic (COVID-19). Estudos Psicol. 2020, 37, 1–13. [Google Scholar]
- Chwaszcz, J.; Palacz-Chrisidis, A.; Wiechetek, M.; Bartczuk, R.P.; Niewiadomska, I.; Sławska, P. Quality of life and its factors in the COVID19 pandemic situation. Results of Stage 1 studies during the pandemic growth period. arXiv 2020, arXiv:10.31234. [Google Scholar]
- World Health Organization. Be Active during COVID-19; WHO: Geneva, Switzerland, 2020; Available online: https://www.who.int/news-room/q-a-detail/be-active during-covid-19 (accessed on 25 June 2020).
- Bezerra, A.C.V. Factors associated with population behavior during social isolation in the COVID-19 pandemic. CiênciaSaúdeColetivo 2020, 25, 2411–2421. [Google Scholar]
- Burtscher, J.; Burtscher, M.; Millet, G.P. (Indoor) isolation, stress and physical inactivity: Vicious circles accelerated by Covid-19? Scand. J. Med. Sci. Sports 2020. [Google Scholar] [CrossRef]
- Haney, C.; Weill, J.; Bakhshay, S.; Lockett, T. Examining jail isolation. Prison J. 2015, 96, 126–152. [Google Scholar] [CrossRef]
- Bao, Y.; Sun, Y.; Meng, S.; Shi, J.; Lu, L. 2019-nCoV epidemic: Address mental health care to empower society. Lancet 2020, 395, e37–e38. [Google Scholar] [CrossRef] [Green Version]
- Cinelli, M.; Quattrociocchi, W.; Galeazzi, A.; Valensise, C.M.; Brugnoli, E.; Scala, A. The covid-19 social media infodemic. arXiv 2020, arXiv:2003.05004. [Google Scholar]
- Kowal, M.; Coll-Martín, T.; Ikizer, G.; Rasmussen, J.; Eichel, K.; Studzinska, A.; Lieberoth, A. Who Is the Most Stressed During COVID-19 Isolation? Data from 27 Countries. 2020. [Google Scholar] [CrossRef]
- Riebe, D.; Ehrman, J.K.; Liguori, G.; Magal, M. organizadores. ACSM’s Guidelines for Exercise Testing and Prescription, 10th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2018. [Google Scholar]
- Matias, G.H.L.; Guerra, A.C.; Souza Filho, B.A.B.; Lima, J.T.O.; Carmo, C.N.; Mattos, I.E. Repeatability and reproducibility of a home exercise manual. Fisioter. Pesq. 2018, 25, 209–216. [Google Scholar] [CrossRef]
- American College of Sports Medicine (ACSM). Staying Active during the Coronavirus Pandemic. 2020. Available online: https://www.exerciseismedicine.org/assets/page_documents/EIM_Rx% (accessed on 16 September 2020).
| Variables | Children’s | Adolescents | ||
|---|---|---|---|---|
| Sample (N° (%)) | 25 (100%) | 44 (100%) | ||
| Female (N° (%)) | 10 (40%) | 25 (57%) | ||
| Male (N° (%)) | 15 (60%) | 19 (43%) | ||
| Age (Yrs) | 9.56 ± 1.47 | 16.3 ± 1.67 | ||
| Stature (cm) | 138.0 ± 8.18 | 159.8 ± 13.7 | ||
| Male | Male | |||
| Pandemic Moments | ||||
| Pré | During | Pré | During | |
| Weight (Kg) | 34.0 ± 9.18 | *38.8 ± 8.61 | 52.6 ± 15.8 | *58.4 ± 15.5 |
| BMI (kg/m²) | 18.5 ± 7.00 | *21.2 ± 7.10 | 21.2 ± 3.45 | 23.6 ± 2.97 |
| BMR (Kcal) | 1328.4 ± 326.0 | 1384.5 ± 302.3 | 1430.5 ± 265.3 | 1497.9 ± 252.6 |
| Female | Female | |||
| Weight (Kg) | 32.0 ± 5.79 | *36.2 ± 4.34 | 60.4 ± 15.0 | *65.8 ± 14.0 |
| BMI (kg/m²) | 16.5± 3.52 | 18.7 ± 3.13 | 22.4 ± 3.72 | 24.4 ± 3.05 |
| BMR (Kcal) | 1167.6 ± 54.6 | 1207.5 ± 39.0 | 1450.9 ± 158.9 | 1502.3 ± 150.4 |
| Adults | Elderly | |||
| Sample (N° (%)) | 310 (100%) | 47 (100%) | ||
| Female (N° (%)) | 159 (51%) | 15 (31%) | ||
| Male (N° (%)) | 151 (49%) | 32 (69%) | ||
| Age (Yrs) | 36.5 ± 11.4 | 66.3 ± 5.07 | ||
| Stature (cm) | 164.4 ± 12.7 | 174.0 ± 8.91 | ||
| Male | Male | |||
| Weight (Kg) | 67.9 ± 18.1 | *72.3 ± 17.4 | 79.0 ± 9.68 | *83.7 ± 9.06 |
| BMI (kg/m²) | 24.1 ± 3.72 | *26.9 ± 8.23 | 25.7 ± 2.59 | 27.3 ± 0.54 |
| BMR (Kcal) | 1550.7 ± 294.8 | 1614.9 ± 275.6 | 1588.5 ± 239.0 | 1654.9 ± 248.1 |
| Female | Female | |||
| Weight (Kg) | 64.6 ± 13.9 | *68.1 ± 13.8 | 77.6 ± 7.72 | *81.9 ± 7.88 |
| BMI (kg/m²) | 24.1 ± 3.58 | 25.6 ± 3.57 | 28.2 ± 2.63 | 27.6 ± 2.19 |
| BMR (Kcal) | 1394.6 ± 139.5 | 1428.6 ± 139.9 | 1391.1 ± 81.4 | 1432.7 ± 88.9 |
| Domain—Raw Scale | Children’s | Adolescents | ||
|---|---|---|---|---|
| Pandemic Moments | ||||
| Male | Male | |||
| Pre | During | Pre | During | |
| FC | 90.33 ± 5.81 | *30.9 ± 21.6 | 91.3 ± 3.26 | *24.2 ± 8.10 |
| LPA | 96.6 ± 12.9 | *6.45 ± 1.66 | 100.0 ± 0.00 | *0.00 ± 0.00 |
| Pain | 76.5 ± 30.6 | *38.3 ± 46.1 | 78.9 ± 27.9 | *40.8 ± 24.3 |
| GHS | 61.2 ± 8.96 | *49.8 ± 12.5 | 66.4 ± 17.5 | *50.7 ± 14.2 |
| VIT | 66.0 ± 17.7 | *47.0 ± 19.3 | 62.6 ± 18.0 | *40.5 ± 16.1 |
| AS | 57.5 ± 28.2 | *32.8 ± 18.3 | 75.0 ± 28.8 | *28.2 ± 13.5 |
| EA | 97.7 ± 8.60 | *8.60 ± 2.22 | 94.7 ± 16.7 | *15.2 ± 3.50 |
| MH | 68.2 ± 14.7 | *33.0 ± 23.0 | 68.2 ± 17.7 | *35.3 ± 15.8 |
| Female | Female | |||
| FC | 79.0 ± 9.36 | *28.0 ± 14.6 | 86.2 ± 22.5 | *25.8 ± 9.90 |
| LPA | 95.0 ± 15.8 | *0.00 ± 0.00 | 100.0 ± 0.00 | *27.6 ± 8.00 |
| Pain | 65.9 ± 21.2 | 54.2 ± 20.0 | 77.0 ± 35.8 | *21.6 ± 9.80 |
| GHS | 69.1 ± 55.9 | *69.1 ± 14.7 | 68.3 ± 12.8 | *47.4 ± 10.6 |
| VIT | 56.5 ± 18.4 | 56.5 ± 12.2 | 63.2 ± 20.5 | *35.8 ± 11.1 |
| AS | 56.2 ± 14.7 | 48.7 ± 16.0 | 75.0 ± 35.1 | *25.0 ± 9.00 |
| EA | 96.6 ± 10.5 | *21.0 ± 6.66 | 97.33 ± 9.22 | *15.7 ± 5.33 |
| MH | 60.8 ± 15.1 | *40.4 ± 11.8 | 67.5 ± 16.7 | *21.6 ± 6.30 |
| Adults | Elderly | |||
| Male | Male | |||
| FC | 89.6 ± 10.0 | *29.6 ± 5.19 | 86.2 ± 10.7 | *17.1 ± 7.96 |
| LPA | 94.3 ± 18.5 | *18.2 ± 5.62 | 97.6 ± 13.2 | *4.41 ± 0.78 |
| Pain | 73.3 ± 25.3 | *49.4 ± 9.34 | 79.5 ± 25.2 | *33.2 ± 1.06 |
| GHS | 63.5 ± 16.1 | *55.11 ± 18.7 | 63.6 ± 15.3 | *53.6 ± 10.4 |
| VIT | 55.5 ± 20.2 | *46.5 ± 15.7 | 58.1 ± 21.0 | *40.3 ± 18.0 |
| AS | 66.6 ± 32.4 | *36.3 ± 9.37 | 64.4 ± 32.5 | *28.9 ± 7.39 |
| EA | 89.1 ± 23.2 | *19.2 ± 6.62 | 94.7 ± 19.1 | *8.19 ± 2.08 |
| MH | 65.0 ± 14.5 | *36.4 ± 3.26 | 67.2 ± 13.2 | 25.0 ± 6.31 |
| Female | Female | |||
| FC | 86.3 ± 15.1 | *31.1 ± 3.23 | 82.6 ± 21.1 | *29.1 ± 19.6 |
| LPA | 90.8 ± 23.6 | *26.3 ± 12.1 | 93.3 ± 25.8 | *6.45 ± 166 |
| Pain | 75.6 ± 25.8 | *49.5 ± 9.97 | 67.2 ± 23.8 | *48.2 ± 5.66 |
| GHS | 63.3 ± 16.5 | *57.4 ± 17.1 | 56.8 ± 14.2 | *43.2 ± 10.0 |
| VIT | 56.4 ± 19.3 | *47.1 ± 16.5 | 49.0 ± 19.8 | 48.0 ± 20.4 |
| AS | 67.3 ± 33.0 | *38.2 ± 3.81 | 61.6 ± 31.1 | *25.0 ± 7.54 |
| EA | 87.4 ± 22.7 | *27.6 ± 14.2 | 95.5 ± 11.7 | *0.00 ± 0.00 |
| MH | 65.4 ± 13.8 | *40.4 ± 16.22 | 60.2 ± 19.4 | *33.3 ± 13.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Matos, D.G.; Aidar, F.J.; Almeida-Neto, P.F.d.; Moreira, O.C.; Souza, R.F.d.; Marçal, A.C.; Marcucci-Barbosa, L.S.; Martins Júnior, F.d.A.; Lobo, L.F.; dos Santos, J.L.; et al. The Impact of Measures Recommended by the Government to Limit the Spread of Coronavirus (COVID-19) on Physical Activity Levels, Quality of Life, and Mental Health of Brazilians. Sustainability 2020, 12, 9072. https://0-doi-org.brum.beds.ac.uk/10.3390/su12219072
de Matos DG, Aidar FJ, Almeida-Neto PFd, Moreira OC, Souza RFd, Marçal AC, Marcucci-Barbosa LS, Martins Júnior FdA, Lobo LF, dos Santos JL, et al. The Impact of Measures Recommended by the Government to Limit the Spread of Coronavirus (COVID-19) on Physical Activity Levels, Quality of Life, and Mental Health of Brazilians. Sustainability. 2020; 12(21):9072. https://0-doi-org.brum.beds.ac.uk/10.3390/su12219072
Chicago/Turabian Stylede Matos, Dihogo Gama, Felipe J. Aidar, Paulo Francisco de Almeida-Neto, Osvaldo Costa Moreira, Raphael Fabrício de Souza, Anderson Carlos Marçal, Lucas Soares Marcucci-Barbosa, Francisco de Assis Martins Júnior, Lazaro Fernandes Lobo, Jymmys Lopes dos Santos, and et al. 2020. "The Impact of Measures Recommended by the Government to Limit the Spread of Coronavirus (COVID-19) on Physical Activity Levels, Quality of Life, and Mental Health of Brazilians" Sustainability 12, no. 21: 9072. https://0-doi-org.brum.beds.ac.uk/10.3390/su12219072









