Intermittent Fasting in Cardiovascular Disorders—An Overview
Abstract
:1. Introduction
2. The Impact of Intermittent Fasting on Lipid Metabolism
3. The Impact of Intermittent Fasting on Inflammatory Biomarkers
4. The Impact of Intermittent Fasting on Blood Pressure
5. The Impact of IF Diets on Other Important Factors in the Development of Cardiovascular Diseases
6. Importance of Food Quality in the “Eating Window”
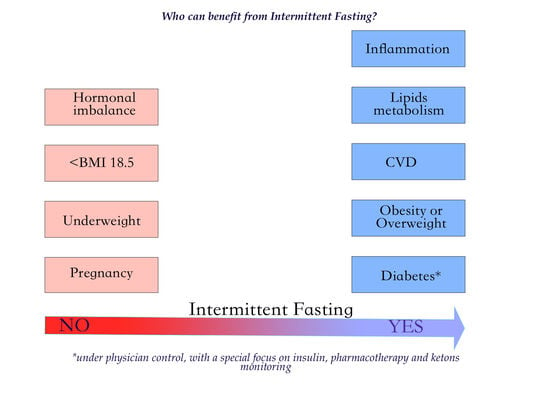
7. Advantages and Disadvantages of Using the IF Diet
8. Summary
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. Available online: https://www.who.int/cardiovascular_diseases/en/ (accessed on 1 February 2019).
- Cierniak-Piotrowska, M.; Marciniak, G.; Stańczak, J. GUS, Statystyka zgonów i umieralności z powodu chorób układu krążenia 2016. Available online: http://bip.stat.gov.pl/organizacja-statystyki-publicznej/rzadowa-rada ludnosciowa/publikacje-rzadowej-rady-ludnosciowej/ (accessed on 1 February 2019).
- Grodstein, F.; Manson, J.; Stampfer, M. Hormone therapy and coronary heart disease: The role oftime since menopause and age at hormone initiation. J. Womens Health 2006, 15, 35–44. [Google Scholar] [CrossRef]
- Matyjaszczyk, P.; Hoffmann, K.; Bryl, W. Epidemiology of selected risk factors for cardiovascular disease. Prz Kardiodiabet 2011, 6, 255–262. [Google Scholar]
- Jankowski, P. Principles of cardiovascular disease prophylaxis in 2018. Kardiol Inwazyjna 2017, 12, 42–48. [Google Scholar]
- Yusuf, S.; Hawken, S.; Ounpuu, S.; Dans, T.; Avezum, A.; Lanas, F.; McQueen, M.; Budaj, A.; Pais, P.; Varigos, J.; et al. INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries: Case-control study. Lancet 2004, 364, 937–952. [Google Scholar] [CrossRef]
- Sofi, F.; Abbate, R.; Gensini, G.F.; Casini, A. Accruing evidenceon benefits of adherence to the Mediterranean diet onhealth: An updated systematic review and meta-analysis. Am. J. Clin. Nutr. 2010, 92, 1189–1196. [Google Scholar] [CrossRef] [PubMed]
- Johnstone, A. Fasting for weight loss. An effective strategy or latest dieting trend? Int. J. Obes. 2014, 39, 727–733. [Google Scholar] [CrossRef]
- Barnosky, A.R.; Hoddy, K.K.; Unterman, T.G.; Varady, K.A. Intermittent fasting vs. daily calorie restriction for type 2 diabetes prevention: A review of human findings. Transl. Res. 2014, 164, 302–311. [Google Scholar] [CrossRef]
- Jane, L.; Atkinson, G.; Jaime, V.; Hamilton, S.; Waller, G.; Harrison, S. Intermittent fasting interventions for the treatment of overweight and obesity in adults aged 18 years and over. A systematic review protocol. JBI Database Syst. Rev. Implement. Rep. 2015, 13, 60–68. [Google Scholar] [CrossRef]
- Harvie, M.; Howell, A. Potential benefits and harms of intermittent energy restriction and intermittent fasting amongst obese, overweight, and normal weight subjects—A narrative review of human and animal evidence. Behav. Sci. 2017, 7, E4. [Google Scholar] [CrossRef]
- Carter, S.; Clifton, P.M.; Keogh, J.B. The effects of intermittent compared to continuous energy restriction on glycaemic control in type 2 diabetes; a pragmatic pilot trial. Diabetes Res. Clin. Pract. 2016, 122, 106–112. [Google Scholar] [CrossRef]
- Patterson, R.E.; Sears, D.D. Metabolic Effects of Intermittent Fasting. Annu. Rev. Nutr. 2017, 37, 371–393. [Google Scholar] [CrossRef] [PubMed]
- Heilbronn, L.K.; Smith, S.R.; Martin, C.K.; Anton, S.D.; Ravussin, E. Alternate-day fasting in nonobese subjects: Effects on body weight, body composition, and energy metabolism. Am. J. Clin. Nutr. 2005, 81, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Tatiana Moro, T.; Tinsley, G.; Bianco, A.; Marcolin, G.; Pacelli, Q.F.; Battaglia, G.; Palma, A.; Gentil, P.; Neri, M.; Paoli, A. Effects of eight weeks of time-restricted feeding (16/8) on basal metabolism, maximal strength, body composition, inflammation, and cardiovascular risk factors in resistance-trained males. J. Transl. Med. 2016, 14, 290. [Google Scholar] [CrossRef]
- Anastasiou, C.A.; Karfopoulou, E.; Yannakoulia, M. Weight regaining: From statistics and behaviors to physiology and metabolism. Metabolism 2015, 64, 1395–1407. [Google Scholar] [CrossRef] [PubMed]
- Wing, R.R.; Blair, E.H.; Bononi, P.; Marcus, M.D.; Watanabe, R.; Bergman, R.N. Caloric restriction per se is a significant factor in improvements in glycemic control and insulin sensitivity during weight loss in obese NIDDM patients. Diabetes Care 1994, 17, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Calixto, A. Life without food and the implications for neurodegeneration. Adv. Genet. 2015, 92, 53–74. [Google Scholar] [PubMed]
- Mattson, M.P.; Longo, V.D.; Harvie, M. Impact of intermittent fasting on health and disease processes. Ageing Res. Rev. 2017, 39, 46–58. [Google Scholar] [CrossRef]
- Vance, J.E.; Vance, D.E. Biochemistry of Lipids, Lipoproteins and Membranes. Elsevier 2008, 36, 648. [Google Scholar]
- Dąbrowska, M.; Zielińska, A.; Nowak, I. Lipid oxidation products as a potentialhealth and analytical problem. CHEMIK 2015, 69, 89–94. [Google Scholar]
- Toledo, F.W.; Grundler, F.; Bergouignan, A.; Drinda, S.; Michalsen, A. Safety, health improvement and well-being during a 4 to 21-day fasting period in an observational study including 1422 subjects. PLoS ONE 2019, 14, e0209353. [Google Scholar]
- Mattson, M.P.; Moehl, K.; Ghena, N.; Schmaedick, M.; Cheng, A. Intermittent metabolic switching, neuroplasticity and brain health. Nat. Rev. Neurosci. 2018, 19, 63–80. [Google Scholar] [CrossRef] [PubMed]
- Camandola, S.; Mattson, M.P. Brain metabolism in health, aging, and neurodegeneration. EMBO J. 2017, 36, 1474–1492. [Google Scholar] [CrossRef] [PubMed]
- Bhutani, S.; Klempel, M.C.; Kroeger, C.M.; Trepanowski, J.F.; Varady, K.A. Alternate day fasting and endurance exercise combine to reduce body weight and favorably alter plasma lipids in obese humans. Obesity (Silver Spring) 2013, 21, 1370–1379. [Google Scholar] [CrossRef] [PubMed]
- Wilson, R.A.; Deasy, W.; Stathis, C.G.; Hayes, A.; Cooke, M.B. Intermittent Fasting with or without Exercise Prevents Weight Gain and Improves Lipids in Diet-Induced Obese Mice. Nutrients 2018, 10, 346. [Google Scholar] [CrossRef]
- Harvie, M.N.; Pegington, M.; Mattson, M.P.; Frystyk, J.; Dillon, B.; Evans, G.; Cuzick, J.; Jebb, S.A.; Martin, B.; Cutler, R.G.; et al. The effects of intermittent or continuous energy restriction on weight loss and metabolic disease risk markers: A randomized trial in young overweight women. Int. J. Obes. (Lond.) 2011, 35, 714–727. [Google Scholar] [CrossRef] [PubMed]
- Varady, K.A.; Bhutani, S.; Klempel, M.C.; Kroeger, C.M.; Trepanowski, J.F.; Haus, J.M.; Hoddy, K.K.; Calvo, Y.L. Alternate day fasting for weight loss in normal weight and overweight subjects: A randomized controlled trial. Nutr. J. 2013, 12, 146. [Google Scholar] [CrossRef] [PubMed]
- Eshghinia, S.; Mohammadzadeh, F. The effects of modified alternate-day fasting diet on weight loss and CAD risk factors in overweight and obese women. J. Diabetes Metab. Disord. 2013, 12, 4. [Google Scholar] [CrossRef] [PubMed]
- Teng, N.I.M.F.; Shahar, S.; Rajab, N.F.; Manaf, Z.A.; Ngah, W.Z. Improvement of metabolic parameters inhealthy older adult men following a fasting calorie restriction intervention. Aging Male 2013, 16, 177–183. [Google Scholar] [CrossRef]
- Harvie, M.N.; Wright, C.; Pegington, M.; McMullan, D.; Mitchell, E.; Martin, B.; Cutler, R.G.; Evans, G.; Whiteside, S.; Maudsley, S.; et al. The effect of intermittent energy and carbohydrate restriction v. daily energy restriction on weight loss and metabolic disease risk markers in overweight women. Br. J. Nutr. 2013, 110, 1534–1547. [Google Scholar] [CrossRef]
- Chowdhury, E.A.; Richardson, J.D.; Holman, G.D.; Tsintzas, K.; Thompson, D.; Betts, J.A. The causal role of breakfast in energy balance and health: A randomized controlled trial in obese adults. Am. J. Clin. Nutr. 2016, 103, 747–756. [Google Scholar] [CrossRef]
- Herrington, W.; Lacey, B.; Sherliker, P.; Armitage, J.; Lewington, S. Epidemiology of atherosclerosis and the possibility of reducing the global burden of atherosclerosis disease. Circ. Res. 2016, 118, 535–546. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.T.; Lin, Y.H.; Chan, Y.W.; Li, K.H.; To, O.T.; Yan, B.P.; Liu, T.; Li, G.; Wong, W.T.; Keung, W.; et al. Mouse models of atherosclerosis: A historical perspective and recent advances. Lipids Health Dis. 2017, 16, 12. [Google Scholar] [CrossRef] [PubMed]
- Parthasarathy, S.; Quinn, M.T.; Steinberg, D. Is oxidized low density lipoprotein involved in the recruitment and retention of monocyte/macrophages in the artery wall during the initiation of atherosclerosis? Basic Life Sci. 1988, 49, 375–380. [Google Scholar] [PubMed]
- Braun, M.; Pietsch, P.; Felix, S.B.; Baumann, G. Modulation of intercellular adhesion molecule-1 and vascular cell adhesion molecule-1 on human coronary smooth muscle cells by cytokines. J. Mol. Cell. Cardiol. 1995, 27, 2571–2579. [Google Scholar] [CrossRef]
- Sano, H.; Sudo, T.; Yokode, M.; Murayama, T.; Kataoka, H.; Takakura, N.; Nishikawa, S.; Nishikawa, S.I.; Kita, T. Functional blockade of platelet-derived growth factor receptor-beta but not of receptor-alpha prevents vascular smooth muscle cell accumulation in fibrous cap lesions in apolipoprotein E-deficient mice. Circulation 2001, 103, 2955–2960. [Google Scholar] [CrossRef] [PubMed]
- Kozaki, K.; Kaminski, W.E.; Tang, J.; Hollenbach, S.; Lindahl, P.; Sullivan, C.; Yu, J.C.; Abe, K.; Martin, P.J.; Ross, R.; et al. Blockade of platelet-derived growth factor or its receptors transiently delays but does not prevent fibrous cap formation in ApoE null mice. Am. J. Pathol. 2002, 161, 1395–1407. [Google Scholar] [CrossRef]
- Bays, H.E. “Sick fat,” metabolic disease, and atherosclerosis. Am. J. Med. 2009, 22, 26–37. [Google Scholar] [CrossRef]
- Aksungar, F.B.; Topkaya, A.E.; Akyildiz, M. Interleukin-6, C-reactive protein and biochemical parameters during prolonged intermittent fasting. Ann. Nutr. Metab. 2007, 51, 88–95. [Google Scholar] [CrossRef]
- Kawano, J.; Arora, R. The role of adiponectin in obesity, diabetes, and cardiovascular disease. J. Cardiometab. Syndr. 2009, 4, 44–49. [Google Scholar] [CrossRef]
- Bhutani, S.; Klempel, M.C.; Berger, R.A.; Varady, K.A. Improvements in Coronary Heart Disease Risk Indicators by Alternate-Day Fasting Involve Adipose Tissue Modulations. Obesity 2010, 18, 2152–2159. [Google Scholar] [CrossRef]
- Cambuli, V.M.; Musiu, M.C.; Incani, M. Assessment of adiponectin and leptin as biomarkers of positive metabolic outcomes after lifestyle intervention in overweight and obese children. J. Clin. Endocrinol. Metab. 2008, 93, 3051–3057. [Google Scholar] [CrossRef]
- Achari, A.E.; Jain, S.K. Adiponectin, a Therapeutic Target for Obesity, Diabetes, and Endothelial Dysfunction. Int. J. Mol. Sci. 2017, 18, 1321. [Google Scholar] [CrossRef] [PubMed]
- Ouchi, N.; Kihara, S.; Arita, Y.; Maeda, K.; Kuriyama, H.; Okamoto, Y.; Hotta, K.; Nishida, M.; Takahashi, K.; Nakamura, T.; et al. Novel modulator for endothelial adhesion molecules: Adipocyte-derived plasma protein adiponectin. Circulation 1999, 100, 2473–2476. [Google Scholar] [CrossRef] [PubMed]
- Ouchi, N.; Kihara, S.; Arita, Y.; Okamoto, Y.; Maeda, K.; Kuriyama, H.; Hotta, K.; Nishida, M.; Takahashi, M.; Muraguchi, M.; et al. Adiponectin, an adipocyte-derived plasma protein, inhibits endothelial NF-kappaB signaling through a cAMP-dependent pathway. Circulation 2000, 102, 1296–1301. [Google Scholar] [CrossRef]
- Okamoto, Y.; Folco, E.J.; Minami, M.; Wara, A.K.; Feinberg, M.W.; Sukhova, G.K.; Colvin, R.A.; Kihara, S.; Funahashi, T.; Luster, A.D.; et al. Adiponectin inhibits the production of CXC receptor 3 chemokine ligands in macrophages and reduces T-lymphocyte recruitment in atherogenesis. Circ. Res. 2008, 102, 218–225. [Google Scholar] [CrossRef]
- Matsuda, M.; Shimomura, I.; Sata, M.; Arita, Y.; Nishida, M.; Maeda, N.; Kumada, M.; Okamoto, Y.; Nagaretani, H.; Nishizawa, H. Role of adiponectin in preventing vascular stenosis the missing link of adipo-vascular axis. J. Biol. Chem. 2002, 277, 37487–37491. [Google Scholar] [CrossRef]
- Wan, R.; Ahmet, I.; Brown, M.; Cheng, A.; Kamimura, N.; Talan, M.; Mattson, M.P. Cardioprotective Effect of Intermittent Fasting is Associated with an Elevation of Adiponectin Levels in Rats. J. Nutr. Biochem. 2010, 21, 413–417. [Google Scholar] [CrossRef] [PubMed]
- Sattar, N.; Wannamethee, G.; Sarwar, N.; Chernova, J.; Lawlor, D.A.; Kelly, A.; Wallace, A.M.; Danesh, J.; Whincup, P.H. Leptin and coronary heart disease: Prospective study and systematic review. J. Am. Coll. Cardiol. 2009, 53, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Bowman, J.D.; Bowman, C.D.; Bush, J.E.; Delheij, P.P.; Frankle, C.M.; Gould, C.R.; Haase, D.G.; Knudson, J.; Mitchell, G.E.; Penttila, S.; et al. Parity nonconservation for neutron resonances in 238U. Phys. Rev. Lett. 1990, 65, 1192–1195. [Google Scholar] [CrossRef]
- Burnett, M.S.; Lee, C.W.; Kinnaird, T.D.; Stabile, E.; Durrani, S.; Dullum, M.K.; Devaney, J.M.; Fishman, C.; Stamou, S.; Canos, D.; et al. The potential role of resistin in atherogenesis. Atherosclerosis 2005, 182, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Schmid, A.; Leszczak, S.; Ober, I.; Karrasch, T.; Schäffler, A. Short-term Regulation of Resistin in vivo by Oral Lipid Ingestion and in vitro by Fatty Acid Stimulation. Exp. Clin. Endocrinol. Diabetes 2015, 123, 553–560. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Park, D.W.; Tadie, J.M.; Gregoire, M.; Deshane, J.; Pittet, J.F.; Abraham, E.; Zmijewski, J.W. Human resistin promotes neutrophil proinflammatory activation and neutrophil extracellular trap formation and increases severity of acute lung injury. J. Immunol. 2014, 192, 4795–4803. [Google Scholar] [CrossRef] [PubMed]
- Hoddy, K.K.; Gibbons, C.; Kroeger, C.M.; Trepanowski, J.F.; Barnosky, A.; Buhtani, S.; Gabel, K.; Finlayson, G.; Varady, K.A. Changes in hunger and fullness in relation to gut peptides before and after 8 weeks of alternate day fasting. Clin. Nutr. 2016, 35, 1380–1385. [Google Scholar] [CrossRef]
- Safavi, E.; Rahbar, A.R. Effect of Intermittent Fasting during Ramadan on Visfatin, Adiponectin and Tumor Necrotizing Factor-Alpha In Healthy Muslim Individuals. J. Fasting Health 2017, 5, 50–55. [Google Scholar]
- Alexander, M.R.; Madhur, M.S.; Harrison, D.G.; Dreisbach, A.W.; Riaz, K.; Sander, G.E.; Yang, E.H. Hypertension: Practice Essentials, Background, Pathophysiology. Cardiology 2018. Available online: https://emedicine.medscape.com/article/241381-overview (accessed on 1 February 2019).
- Benjamin, E.J.; Virani, S.S.; Callaway, C.W.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Chiuve, S.E.; Cushman, M.; Delling, F.N.; Deo, R.; et al. Heart Disease and Stroke Statistics—2018 Update, A Report from the American Heart Association. Circulation 2018, 137, e67–e492. [Google Scholar] [CrossRef] [PubMed]
- Mager, D.E.; Wan, R.; Brown, M.; Cheng, A.; Wareski, P.; Abernethy, D.R.; Mattson, M.P. Caloric restriction and intermittent fasting alter spectral measures of heart rate and blood pressure variability in rats. FASEB J. 2006, 20, 631–637. [Google Scholar] [CrossRef]
- Wan, R.; Weigand, L.A.; Bateman, R.; Griffioen, K.; Mendelowitz, D.; Mattson, M.P. Evidence that BDNF regulates heart rate by a mechanism involving increased brainstem parasympathetic neuron excitability. J. Neurochem. 2014, 129, 573–580. [Google Scholar] [CrossRef]
- Yang, B.; Slonimsky, J.D.; Birren, S.J. A rapid switch in sympathetic neurotransmitter release properties mediated by the p75 receptor. Nat. Neurosci. 2002, 5, 539–545. [Google Scholar] [CrossRef]
- Wang, J.; Irnaten, M.; Neff, R.A.; Venkatesan, P.; Evans, C.; Loewy, A.D.; Mettenleiter, T.C.; Mendelowitz, D. Synaptic and neurotransmitter activation of cardiac vagal neurons in the nucleus ambiguus. Ann. N. Y. Acad. Sci. 2001, 940, 237–246. [Google Scholar] [CrossRef]
- Erdem, Y.; Ozkan, G.; Ulusoy, S.; Arici, M.; Derici, U.; Sengul, S.; Sindel, S.; Erturk, S. The effect of intermiitent fasting on blood pressure variability in patients with newly diagnosed hypertension or prehypertension. J. Am. Soc. Hypertens. 2018, 12, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Colditz, G.A.; Willett, W.C.; Rotnitzky, A.; Manson, J.E. Weight gain as a risk factor for clinical diabetes mellitus in women. Ann. Intern. Med. 1995, 122, 481–486. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.C.; Manson, J.E.; Stampfer, M.J.; Colditz, G.A.; Rosner, B.; Speizer, F.E.; Hennekens, C.H. Weight, weight change, and coronary heart disease in women. Risk within the ‘normal’ weight range. JAMA 1995, 273, 461–465. [Google Scholar] [CrossRef]
- Trepanowski, J.F.; Kroeger, C.M.; Barnosky, A.; Klempel, M.C.; Bhutani, S.; Hoddy, K.K.; Gabel, K.; Freels, S.; Rigdon, J.; Rood, J.; et al. Effect of Alternate-Day Fasting on Weight Loss, Weight Maintenance, and Cardioprotection Among Metabolically Healthy Obese Adults: A Randomized Clinical Trial. JAMA Intern. Med. 2017, 177, 930–938. [Google Scholar] [CrossRef]
- Schübel, R.; Nattenmüller, J.; Sookthai, D.; Nonnenmacher, T.; Graf, M.E.; Riedl, L.; Schlett, C.L.; von Stackelberg, O.; Johnson, T.; Nabers, D.; et al. Effects of intermittent and continuous calorie restriction on bodyweight and metabolism over 50 wk: A randomized controlled trial. Am. J. Clin. Nutr. 2018, 108, 933–945. [Google Scholar] [CrossRef] [PubMed]
- Sutton, E.F.; Beyl, R.; Early, K.S.; Cefalu, W.T.; Ravussin, E.; Peterson, C.M. Early Time-Restricted Feeding Improves Insulin Sensitivity, Blood Pressure, and Oxidative Stress Even without Weight Loss in Men with Prediabetes. Cell Metab. 2018, 27, 1212–1221. [Google Scholar] [CrossRef]
- Gotthardt, J.D.; Verpeut, J.L.; Yeomans, B.L.; Yang, J.A.; Yasrebi, A.; Roepke, T.A.; Bello, N.T. Intermittent Fasting Promotes Fat Loss With Lean Mass Retention, Increased Hypothalamic Norepinephrine Content, and Increased Neuropeptide Y Gene Expression in Diet-Induced Obese Male Mice. Endocrinology 2016, 157, 679–691. [Google Scholar] [CrossRef]
- Arnason, T.G.; Bowen, M.W.; Mansell, K.D. Effects of intermittent fasting on health markers in those with type 2 diabetes: A pilot study. World J. Diabetes 2017, 8, 154–164. [Google Scholar] [CrossRef]
- Leslie, W.S.; Ford, I.; Sattar, N.; Hollingsworth, K.G.; Adamson, A.; Sniehotta, F.F.; McCombie, L.; Brosnahan, N.; Ross, H.; Mathers, J.C.; et al. The Diabetes Remission Clinical Trial (DiRECT): Protocol for a cluster randomised trial. BMC Fam. Pract. 2016, 17, 20. [Google Scholar] [CrossRef]
- Furmli, S.; Elmasry, R.; Ramos, M.; Fung, J. Therapeutic use of intermittent fasting for people with type 2 diabetes as an alternative to insulin. BMJ Case Rep. 2018, 2018, brc-2017. [Google Scholar] [CrossRef]
- Sequea, D.A.; Sharma, N.; Arias, E.B.; Cartee, G.D. Calorie restriction enhances insulin-stimulated glucose uptake and Akt phosphorylation in both fast-twitch and slow-twitch skeletal muscle of 24-month-old rats. J. Gerontol. A Biol. Sci. Med. Sci. 2012, 67, 1279–1285. [Google Scholar] [CrossRef]
- Belkacemi, L.; Selselet-Attou, G.; Hupkens, E.; Nguidjoe, E.; Louchami, K.; Sener, A.; Malaisse, W.J. Intermittent Fasting Modulation of the Diabetic Syndrome in Streptozotocin-Injected Rats. Int. J. Endocrinol. 2012, 2012, 962012. [Google Scholar] [CrossRef] [PubMed]
- Wei, S.; Han, R.; Zhao, J.; Wang, S.; Huang, M.; Wang, Y.; Chen, Y. Intermittent administration of a fasting-mimicking diet intervenes in diabetes progression, restores β cells and reconstructs gut microbiota in mice. Nutr. Metab. (Lond.) 2018, 15, 80. [Google Scholar] [CrossRef]
- Liu, H.; Javaheri, A.; Godar, R.J.; Murphy, J.; Ma, X.; Rohatgi, N.; Mahadevan, J.; Hyrc, K.; Saftig, P.; Marshall, C.; et al. Intermittent fasting preserves beta-cell mass in obesity-induced diabetes via the autophagy-lysosome pathway. Autophagy 2017, 13, 1952–1968. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.R.; Willing, A. Enhancing endogenous capacity to repair a stroke-damaged brain: An evolving field for stroke research. Prog. Neurobiol. 2018, 163–164, 5–26. [Google Scholar] [CrossRef] [PubMed]
- Fann, D.Y.; Ng, G.Y.; Poh, L.; Arumugam, T.V. Positive effects of intermittent fasting in ischemic stroke. Exp. Gerontol. 2017, 89, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Li, L.; Zhao, H.; Peng, S.; Zuo, Z. Chronic high fat diet induces cardiac hypertrophy and fibrosis in mice. Metabolism 2015, 64, 917–925. [Google Scholar] [CrossRef] [PubMed]
- Scicchitano, P.; Cameli, M.; Maiello, M.; Modesti, P.A.; Muiesan, M.L.; Novo, S.; Palmiero, P.; Sergio Saba, P.; Pedrinelli, R.; Ciccone, M.M. Nutraceuticals and dyslipidaemia: Beyondthe commontherapeutics. J. Funct. Food 2014, 6, 11–32. [Google Scholar] [CrossRef]
- Giordano, P.; Scicchitano, P.; Locorotondo, M.; Mandurino, C.; Ricci, G.; Carbonara, S.; Gesualdo, M.; Zito, A.; Dachille, A.; Caputo, P.; et al. Carotenoids and cardiovascular risk. Curr. Pharm. Des. 2012, 18, 5577–5589. [Google Scholar] [CrossRef]
- Wiciński, M.; Malinowski, B.; Węclewicz, M.M.; Grześk, E.; Grześk, G. Resveratrol increases serum BDNF concentrations and reduces vascular smooth muscle cells contractility via a NOS-3-independent mechanism. Biomed. Res. Int. 2017, 2017, 9202954. [Google Scholar] [CrossRef]
- Wiciński, M.; Malinowski, B.; Węclewicz, M.M.; Grześk, E.; Grześk, G. Anti-athergoenic properties of resveratrol: 4-week resveratrol administration associated with serum concentrations of SIRT1, adiponectin, S100A8/9 and VSMCs contractility in a rat model. Exp. Ther. Med. 2017, 13, 2071–2078. [Google Scholar] [CrossRef]
- Chen, Q.; Wang, E.; Ma, L.; Zhai, P. Dietary resveratrol increases the expression of hepatic 7a-hydroxylase and ameliorates hypercholesterolemia in high-fat fed C57BL/6J mice. Lipids Health Dis. 2012, 11, 56. [Google Scholar] [CrossRef]
- Sahebkar, A. Effects of resveratrol supplementation on plasma lipids: A systematic review and meta-analysis of randomized controlled trials. Nutr. Rev. 2013, 71, 822–835. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.H.; Chen, S.C.; Ou, T.T.; Chyau, C.C.; Chang, Y.C.; Wang, C.J. Mulberry leaf polyphenol extracts reduced hepatic lipid accumulation involving regulation of adenosine monophosphate activated protein kinase and lipogenic enzymes. J. Funct. Foods 2013, 5, 1620–1632. [Google Scholar] [CrossRef]
- Jin, D.; Xua, Y.; Meia, X. Antiobesity and lipid lowering effects of theaflavins on high-fat diet induced obese rats. J. Funct. Foods 2013, 5, 1142–1150. [Google Scholar] [CrossRef]
- Gunathilake, K.D.P.P.; Wang, Y.; Vasantha Rupasinghea, H.P. Hypocholesterolemic and hypotensive effects of a fruitbased functional beverage in spontaneously hypertensive rats fed with cholesterol-rich diet. J. Funct. Foods 2013, 5, 1392–1401. [Google Scholar] [CrossRef]
- Ciccone, M.M.; Scicchitano, P.; Gesualdo, M.; Zito, A.; Carbonara, S.; Ricci, G.; Cortese, F.; Giordano, P. The role of omega-3 polyunsaturated fatty acids supplementation in childhood: A review. Recent Patents Cardiovasc. Drug Discov. 2013, 8, 42–55. [Google Scholar] [CrossRef]
- Kris-Etherton, P.M.; Harris, W.S.; Appel, L.J. American Heart Association Nutrition Committee. Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Circulation 2002, 106, 2747–2757. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, S.; Willers, J.; Stahl, F.; Dardano, A.; Penno, G.; Del Prato Mutz, K.O.; Scheper, T.; Hahn, A.; Schuchardt, J.P. Regulation of lipid metabolism-related gene expression in whole blood cells of normo- and dyslipidemic men after fish oil supplementation. Lipids Health Dis. 2012, 11, 172. [Google Scholar] [CrossRef]
- Zhao, J.F.; Ching, L.C.; Huang, Y.C.; Chen, C.Y.; Chiang, A.N.; Kou, Y.R.; Shyue, S.K.; Lee, T.S. Molecular mechanism of curcumin on the suppression of cholesterol accumulation in macrophage foam cells and atherosclerosis. Mol. Nutr. Food Res. 2012, 56, 691–701. [Google Scholar] [CrossRef]
- Rahimi-Ardabili, B.; Argani, H.; Ghorbanihaghjo, A.; Rashtchizadeh, N.; Naghavi-Behzad, M.; Ghorashi, S.; Nezami, N. Paraoxonase enzyme activity is enhanced by zinc supplementation in hemodialysis patients. Renal Failure 2012, 34, 1123–1128. [Google Scholar] [CrossRef]
- Li, H.L.; Liu, D.P.; Liang, C.C. Paraoxonase gene polymorphisms, oxidative stress, and diseases. J. Mol. Med. (Berlin) 2003, 81, 766–779. [Google Scholar] [CrossRef]
- Bronwen, M.; Mattson, M.P.; Maudsleya, S. Caloric restriction and intermittent fasting: Two potential diets for successful brain aging. Ageing Res. Rev. 2006, 5, 332–353. [Google Scholar]
- Beshyah, S.A.; Hassanein, M.; Ahmedani, M.Y.; Shaikh, S.; Ba-Essa, E.M.; Megallaa, M.H.; Afandi, B.; Ibrahim, F.; Al-Muzaffar, T. Diabetic Hypoglycaemia during Ramadan Fasting: A Trans-National Observational Real-World Study. Diabetes Res. Clin. Pract. 2019, 18, 31843–31846. [Google Scholar] [CrossRef]
- Dardano, A.; Penno, G.; Del Prato, S.; Miccoli, R. Optimal therapy of type 2 diabetes: A controversial challenge. Aging (Albany NY) 2014, 6, 187–206. [Google Scholar] [CrossRef]
- Miller, M.E.; Williamson, J.D.; Gerstein, H.C.; Byington, R.P.; Cushman, W.C.; Ginsberg, H.N.; Ambrosius, W.T.; Lovato, L.; Applegate, W.B.; ACCORD Investigators. Effects of randomization to intensive glucose control on adverse events, cardiovascular disease, and mortality in older versus younger adults in the ACCORD Trial. Diabetes Care 2014, 37, 634–643. [Google Scholar] [CrossRef]
- Ganesan, K.; Habboush, Y.; Sultan, S. Intermittent Fasting: The Choice for a Healthier Lifestyle. Cureus 2018, 10, e2947. [Google Scholar] [CrossRef]
| Energy restriction for two nonconsecutive days and ad libidum intake for other five days. | Eating days—ad libidum food intake. Fasting days—Low or no-energy food intake. | Ad libitum food intake in specific timeframe (~12-h). Night fasting period according to circadian rhythm. | |
| 5:2 Protocol | ADF Protocol | TRF Protocol | Days of the Week |
| Fast | Eat | ~12-h | Monday |
| Fast | Fast | ~12-h | Tuesday |
| Eat | Eat | ~12-h | Wednesday |
| Eat | Fast | ~12-h | Thursday |
| Eat | Eat | ~12-h | Friday |
| Fast | Fast | ~12-h | Saturday |
| Fast | Eat | ~12-h | Sunday |
| First Author and Reference Number | Number of Enrolled | Participants Description | Time | Lipids | NCT Number |
|---|---|---|---|---|---|
| Harvie et al., 2011 [27] | 107 | Overweight or obese premenopausal women | 6 months | NS (LDL, TGs, HDL) | NCT02679989 |
| Varady et al., 2013 [28] | 15 | Overweight individuals BMI 20–29.9 kg/m2 | 12 weeks | ↓TC (p < 0.01) ↓LDL (p < 0.01) NS HDL ↓TGs (p < 0.01) | NCT00960505 |
| Bhutani et al., 2013 [25] | 83 | Obese individuals BMI 30–39.9 kg/m2 | 12 weeks | NS TC ↓LDL (p < 0.05) NS TGs ↑HDL (p < 0.05) | NCT00960505 |
| Eshghinia et al., 2013 [29] | 15 | Overweight or obese women BMI ≥ 25 kg/m2 | 8 weeks | NS (LDL, TGs, HDL) | - |
| Teng et al., 2013 [30] | 28 | Malay Men BMI 23–29.9 kg/m2 | 12 weeks | ↓TC (p < 0.001) ↓LDL (p < 0.05) NS HDL NS TGs | NCT01665482 |
| Harvie et al., 2013 [31] | 77 | Overweight or obese women | 3 months | NS (LDL, TGs, HDL) | NCT00869466 |
| Chowdhury et al., 2016 [32] | 23 | Obese individuals BMI 30–39.9 kg/m2 | 6 weeks | NS (LDL, TGs, HDL) ↑TC | - |
| First Author and Reference Number | Number of Enrolled | Participants Description | Time | Inflammatory Biomarkers | NCT Number |
|---|---|---|---|---|---|
| Harvie et al., 2013 [31] | 77 | Overweight or obese women | 3 months | NS (IL6, TNFα, leptin, adiponectin) | NCT00869466 |
| Varady et al., 2013 [28] | 15 | Overweight individuals BMI 20–29.9 kg/m2 | 12 weeks | ↓CRP (p = 0.01) ↓Leptin (p = 0.03) ↑Adiponectin (p < 0.01) | NCT00960505 |
| Bhutani et al., 2013 [25] | 83 | Obese individuals BMI 30–39.9 kg/m2 | 12 weeks | NS CRP | NCT00960505 |
| Hoddy et al., 2016 [55] | 59 | Obese individuals BMI 30–39.9 kg/m2 | 10 weeks | ↓Leptin (p < 0.05) | - |
| Chowdhury et al., 2016 [32] | 23 | Obese individuals BMI 30–39.9 kg/m2 | 6 weeks | NS (IL6, CRP, leptin, adiponectin) | - |
| Safavi et al., 2017 [56] | 34 | Male individuals 16–64 years old (Ramadan) | 4 weeks | NS (adiponectin, TNFα) | - |
| First Author and Reference Number | Number of Enrolled | Participants Description | Time | Blood Pressure | BDNF | NCT Number |
|---|---|---|---|---|---|---|
| Harvie et al., 2011 [27] | 107 | Overweight or obese premenopausal women | 6 months | ↓Systolic (p = 0.99) ↓Diastolic (p = 0.84) | NS | NCT02679989 |
| Varady et al., 2013 [28] | 15 (5 M/10 F) | Overweight individuals BMI 20–29.9 kg/m2 | 12 weeks | ↓(p = 0.51) | - | NCT00960505 |
| Bhutani et al., 2013 [25] | 83 (3 M/80 F) | Obese individuals BMI 30–39.9 kg/m2 | 12 weeks | ↓Systolic (p = 0.254) ↓Diastolic (p = 0.570) | - | NCT00960505 |
| Eshghinia et al., 2013 [29] | 15 F | Overweight or obese women BMI ≥25 kg/m2 | 8 weeks | ↓Systolic (p < 0.001) ↓Diastolic (p < 0.05) | - | - |
| Teng et al., 2013 [30] | 28 M | Malay Men BMI 23–29.9 kg/m2 | 12 weeks | ↓Systolic (p < 0.05) ↓Diastolic (p < 0.05) | - | NCT01665482 |
| Erdem et al., 2018 [63] | 60 | Individuals from the Cappadocia cohort with prehypertension and hypertension SBP 12—139 and ≥140; DBP 80–89 and ≥90 mmHg | ↓Systolic (p < 0.001) ↓Diastolic (p < 0.039) | - |
| First Author and Reference Number | Number of Enrolled | Participants Description | Time | Weight Changes | Glycemic Profile | NCT Number |
|---|---|---|---|---|---|---|
| Harvie et al., 2011 [27] | 107 | Overweight or obese premenopausal women | 6 months | NS | ↓insulin NS glucose | NCT02679989 |
| Harvie et al., 2013 [31] | 77 | Overweight or obese women | 3 months | NS | ↓insulin NS (HbA1C, glucose) | NCT00869466 |
| Varady et al., 2013 [28] | 15 | Overweight individuals BMI 20–29.9 kg/m2 | 12 weeks | ↓(p < 0.001) | - | NCT00960505 |
| Bhutani et al., 2013 [25] | 83 | Obese individuals BMI 30–39.9 kg/m2 | 12 weeks | ↓(p < 0.05) | NS (insulin, glucose) | NCT00960505 |
| Hoddy et al., 2016 [55] | 59 | Obese individuals BMI 30–39.9 kg/m2 | 10 weeks | ↓(p < 0.0001) | ↓(insulin, glucose) | - |
| Chowdhury et al., 2016 [32] | 23 | Obese individuals BMI 30–39.9 kg/m2 | 6 weeks | ↑(NS) | NS (insulin, glucose) | - |
| Safavi et al., 2017 [56] | 34 | Male individuals 16–64 years old (Ramadan) | 4 weeks | NS | - | - |
| Trepanowski et al., 2017 [66] | 100 | Obese individuals BMI 34 | 12 months | ↓(comparing to control group) | ↓(insulin, glucose) comparing to control group | NCT00960505 |
| Schubel et al., 2018 [67] | 150 | Obese and overweight BMI ≥ 25 | 50 weeks | ↓(comparing to control group) | NS (insulin, glucose) comparing to control group | NCT02449148 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malinowski, B.; Zalewska, K.; Węsierska, A.; Sokołowska, M.M.; Socha, M.; Liczner, G.; Pawlak-Osińska, K.; Wiciński, M. Intermittent Fasting in Cardiovascular Disorders—An Overview. Nutrients 2019, 11, 673. https://0-doi-org.brum.beds.ac.uk/10.3390/nu11030673
Malinowski B, Zalewska K, Węsierska A, Sokołowska MM, Socha M, Liczner G, Pawlak-Osińska K, Wiciński M. Intermittent Fasting in Cardiovascular Disorders—An Overview. Nutrients. 2019; 11(3):673. https://0-doi-org.brum.beds.ac.uk/10.3390/nu11030673
Chicago/Turabian StyleMalinowski, Bartosz, Klaudia Zalewska, Anna Węsierska, Maya M. Sokołowska, Maciej Socha, Grzegorz Liczner, Katarzyna Pawlak-Osińska, and Michał Wiciński. 2019. "Intermittent Fasting in Cardiovascular Disorders—An Overview" Nutrients 11, no. 3: 673. https://0-doi-org.brum.beds.ac.uk/10.3390/nu11030673