Improved Nutritional Knowledge in the Obese Adult Population Modifies Eating Habits and Serum and Anthropometric Markers
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Data Collection
2.3. Nutritional Assessment
2.4. Nutritional Knowledge
2.5. Eating Habits
2.5.1. Food Frequency
2.5.2. Easy Diet®
2.6. Intervention
2.7. Data Analysis
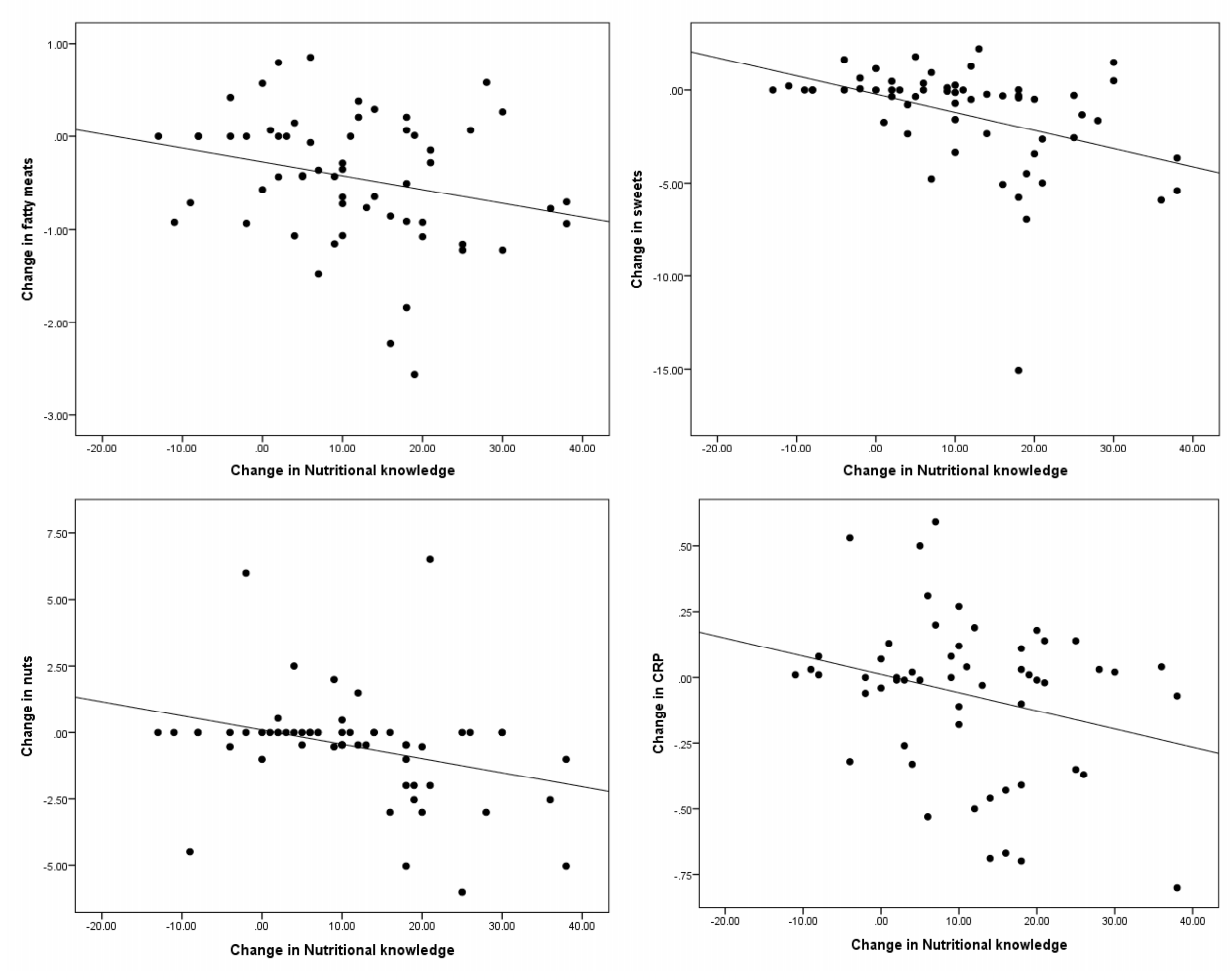
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chooi, Y.C.; Ding, C.; Magkos, F. The epidemiology of obesity. Metab. Clin. Exp. 2019, 92, 6–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef] [Green Version]
- Hernáez, A.; Zomeño, M.D.; Dégano, I.R.; Pérez-Fernández, S.; Goday, A.; Vila, J.; Civeira, F.; Moure, R.; Marrugat, J. Excess Weight in Spain: Current Situation, Projections for 2030, and Estimated Direct Extra Cost for the Spanish Health System. Rev. Esp. Cardiol. Engl. Ed. 2019, 72, 916–924. [Google Scholar] [CrossRef]
- Blüher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Prados-Bo, A.; Gomez-Martínez, S.; Nova, E.; Marcos, A. El papel de los probióticos en el manejo de la obesidad. Nutr. Hosp. 2015, 10–18. [Google Scholar] [CrossRef]
- Hruby, A.; Hu, F.B. The Epidemiology of Obesity: A Big Picture. Pharmacoeconomics 2015, 33, 673–689. [Google Scholar] [CrossRef]
- Arroyo-Johnson, C.; Mincey, K.D. Obesity epidemiology trends by race/ethnicity, gender, and education: National Health Interview Survey, 1997–2012. Gastroenterol. Clin. N. Am. 2016, 45, 571–579. [Google Scholar] [CrossRef] [Green Version]
- Hebebrand, J.; Holm, J.-C.; Woodward, E.; Baker, J.L.; Blaak, E.; Schutz, D.D.; Farpour-Lambert, N.J.; Frühbeck, G.; Halford, J.G.C.; Lissner, L.; et al. A Proposal of the European Association for the Study of Obesity to Improve the ICD-11 Diagnostic Criteria for Obesity Based on the Three Dimensions Etiology, Degree of Adiposity and Health Risk. Obes. Facts 2017, 10, 284–307. [Google Scholar] [CrossRef] [PubMed]
- Vos, T.; Allen, C.; Arora, M.; Barber, R.M.; Bhutta, Z.A.; Brown, A.; Carter, A.; Cassey, D.C.; Charlson, F.J. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1545–1602. [Google Scholar] [CrossRef] [Green Version]
- Wharton, S.; Lau, D.C.W.; Vallis, M.; Sharma, A.M.; Biertho, L.; Campbell-Scherer, D.; Adamo, K.; Alberga, A.; Bell, R.; Boulé, N.; et al. Obesity in adults: A clinical practice guideline. Can. Med. Assoc. J. 2020, 192, E875–E891. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, T.; Haboubi, N. Assessment and management of nutrition in older people and its importance to health. Clin. Interv. Aging 2010, 5, 207–216. [Google Scholar] [PubMed] [Green Version]
- Pérez-Ros, P.; Vila-Candel, R.; Adler, L.; Martínez-Arnau, F.M. Nutritional Status and Risk Factors for Frailty in Community-Dwelling Older People: A Cross-Sectional Study. Nutrients 2020, 12, 1041. [Google Scholar] [CrossRef]
- Bezerra, L.; Lima, S.M.; Correia, L.; Costa, R. Nutrition knowledge assessment studies in adults: A systematic review. Cien. Saude Colet. 2016, 21, 449–462. [Google Scholar] [CrossRef] [Green Version]
- Laxer, R.E.; Brownson, R.C.; Dubin, J.A.; Cooke, M.; Chaurasia, A.; Leatherdale, S.T. Clustering of risk-related modifiable behaviours and their association with overweight and obesity among a large sample of youth in the COMPASS study. BMC Public Health 2017, 17, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, J.; Masters, W.A.; Bai, Y.; Mozaffarian, D.; Naumova, E.N.; Singh, G.M. The International Diet-Health Index: A novel tool to evaluate diet quality for cardiometabolic health across countries. BMJ Glob. Health 2020, 5. [Google Scholar] [CrossRef]
- Balani, R.; Herrington, H.; Bryant, E.; Lucas, C.; Kim, S.C. Nutrition knowledge, attitudes, and self-regulation as predictors of overweight and obesity. J. Am. Assoc. Nurse Pr. 2019, 31, 502–510. [Google Scholar] [CrossRef]
- D’Innocenzo, S.; Biagi, C.; Lanari, M. Obesity and the Mediterranean Diet: A Review of Evidence of the Role and Sustainability of the Mediterranean Diet. Nutrients 2019, 11, 1306. [Google Scholar] [CrossRef] [Green Version]
- Meslier, V.; Abid, M.; Roager, H.M.; Filippis, F.; Roume, H.; Quinquis, B.; Giacco, R.; Mennella, I.; Ferracane, R.; Pons, N.; et al. Mediterranean diet intervention in overweight and obese subjects lowers plasma cholesterol and causes changes in the gut microbiome and metabolome independently of energy intake. Gut 2020, 69, 1258–1268. [Google Scholar] [CrossRef] [Green Version]
- Jensen, M.D.; Ryan, D.H.; Apovian, C.M.; Ard, J.D.; Comuzzie, A.G.; Donato, K.A.; Hu, F.B.; Hubbard, V.S.; Jakicic, J.M.; Kushner, R.F.; et al. Guideline for the Management of Overweight and Obesity in Adults. J. Am. Coll. Cardiol. 2014, 63, 2985–3023. [Google Scholar] [CrossRef] [Green Version]
- Australia National Health and Medical Research Council (Ed.) Clinical Practice Guidelines for the Management of Overweight and Obesity in Adults, Adolescents and Children in Australia: Systematic Review; National Health and Medical Research Council: Canberra, Australia, 2013; ISBN 9781864965933. [Google Scholar]
- Kirk, S.F.L.; Penney, T.L.; McHugh, T.-L.; Sharma, A.M. Effective weight management practice: A review of the lifestyle intervention evidence. Int. J. Obes. 2012, 36, 178–185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shaw, K.A.; Kenardy, J.; O’Rourke, P.K.; Del Mar, C.B. Psychological interventions for overweight or obesity. Cochrane Database Syst. Rev. 2005, 18, 1–23. [Google Scholar] [CrossRef] [Green Version]
- Thomson, M.; Martin, A.; Logue, J.; Wells, V.; Simpson, S.A. Barriers and facilitators of successful weight loss during participation in behavioural weight management programmes: A protocol for a systematic review. Syst. Rev. 2020, 9, 1–8. [Google Scholar] [CrossRef]
- Lim, S.; Smith, C.A.; Costello, M.F.; MacMillan, F.; Moran, L.; Ee, C. Barriers and facilitators to weight management in overweight and obese women living in Australia with PCOS: A qualitative study. BMC Endocr. Disord. 2019, 19, 106. [Google Scholar] [CrossRef] [PubMed]
- Salvador, J.; Vilarrasa, N.; Poyato, F.; Rubio, M.A. Perceptions, Attitudes, and Barriers to Obesity Management in Spain: Results from the Spanish Cohort of the International ACTION-IO Observation Study. J. Clin. Med. 2020, 9, 2834. [Google Scholar] [CrossRef]
- Miles, J.; Petrie, C.; Steel, M. Slimming on the Internet. J. R. Soc. Med. 2000, 93, 254–257. [Google Scholar] [CrossRef] [Green Version]
- Andrade, J.; Vasconcellos-Silva, P.R.; Da Silva, L.A. Cycles of attention to fad diets and internet search trends by Google trends. Cien. Saude Colet. 2020, 25, 2615–2631. [Google Scholar] [CrossRef]
- Murimi, M.W.; Kanyi, M.; Mupfudze, T.; Amin, M.R.; Mbogori, T.; Aldubayan, K. Factors Influencing Efficacy of Nutrition Education Interventions: A Systematic Review. J. Nutr. Educ. Behav. 2017, 49, 142–165.e1. [Google Scholar] [CrossRef]
- Calderón-García, A.; Marrodán, M.D.; Villarino, A.; Martínez-Álvarez, J. Assessment of nutritional status, and habits and food preferences in a child-youth population (7 to 16 years) of the Community of Madrid. Nutr. Hosp. 2019, 36, 394–404. [Google Scholar] [CrossRef]
- Johns, D.J.; Hartmann-Boyce, J.; Jebb, S.A.; Aveyard, P. Diet or exercise interventions vs. combined behavioral weight management programs: A systematic review and meta-analysis of direct comparisons. J. Acad. Nutr. Diet. 2014, 114, 1557–1568. [Google Scholar] [CrossRef] [Green Version]
- Gilardini, L.; Cancello, R.; Caffetto, K.; Cottafava, R.; Gironi, I.; Invitti, C. Nutrition knowledge is associated with greater weight loss in obese patients following a multidisciplinary rehabilitaiton program. Minerva Endocrinol. 2020. [Google Scholar] [CrossRef]
- Blomfield, R.L.; Collins, C.E.; Hutchesson, M.J.; Young, M.D.; Jensen, M.E.; Callister, R.; Morgan, P.J. Impact of self-help weight loss resources with or without online support on the dietary intake of overweight and obese men: The SHED-IT randomised controlled trial. Obes. Res. Clin. Pr. 2014, 8, e476–e487. [Google Scholar] [CrossRef]
- OMS Recomendaciones Mundiales Sobre la Actividad Física Para la Salud. Available online: http://www.who.int/dietphysicalactivity/factsheet_recommendations/es/ (accessed on 9 February 2016).
- Deurenberg, P.; Weststrate, J.A.; Seidell, J.C. Body mass index as a measure of body fatness: Age- and sex-specific prediction formulas. Br. J. Nutr. 1991, 65, 105–114. [Google Scholar] [CrossRef] [Green Version]
- Bach, L. Conocimiento nutricional y conductas de control del peso. Ph.D. Thesis, Universidad de Barcelona, Barcelona, Spain, 2002. [Google Scholar]
- Feskanich, D.; Rimm, E.B.; Giovannucci, E.L.; Colditz, G.A.; Stampfer, M.J.; Litin, L.B.; Willett, W.C. Reproducibility and validity of food intake measurements from a semiquantitative food frequency questionnaire. J. Am. Diet. Assoc. 1993, 93, 790–796. [Google Scholar] [CrossRef]
- Jeffery, R.W.; Levy, R.L.; Langer, S.L.; Welsh, E.M.; Flood, A.P.; Jaeb, M.A.; Laqua, P.S.; Hotop, A.M.; Finch, E.A. A comparison of maintenance-tailored therapy (MTT) and standard behavior therapy (SBT) for the treatment of obesity. Prev. Med. 2009, 49, 384–389. [Google Scholar] [CrossRef] [Green Version]
- Moreiras, O.; Carbajal, A.; Cabrera, L.; Cuadrado, C. Tablas de Composición de Alimentos: Guía de Practices, 19th ed.; Piramide: Madrid, Spain, 2018; ISBN 978-84-368-3947-0. [Google Scholar]
- Healthy Diet. Available online: https://www.who.int/news-room/fact-sheets/detail/healthy-diet (accessed on 19 October 2020).
- Zhou, L.; Zeng, Q.; Jin, S.; Cheng, G. The impact of changes in dietary knowledge on adult overweight and obesity in China. PLoS ONE 2017, 12. [Google Scholar] [CrossRef] [Green Version]
- Partearroyo, T.; Samaniego-Vaesken, M.L.; Ruiz, E.; Aranceta-Bartrina, J.; Gil, Á.; González-Gross, M.; Ortega, R.M.; Serra-Majem, L.; Varela-Moreiras, G. Current Food Consumption amongst the Spanish ANIBES Study Population. Nutrients 2019, 11, 2663. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arroyo-Olivares, R.; Alonso, R.; Quintana-Navarro, G.; Fuentes-Jiménez, F.; Mata, N.; Muñiz-Grijalvo, O.; Díaz-Díaz, J.L.; Zambón, D.; Arrieta, F.; García-Cruces, J.; et al. Adults with familial hypercholesterolaemia have healthier dietary and lifestyle habits compared with their non-affected relatives: The SAFEHEART study. Public Health Nutr. 2019, 22, 1433–1443. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shimokawa, S. When does dietary knowledge matter to obesity and overweight prevention? Food Policy 2013, 38, 35–46. [Google Scholar] [CrossRef]
- McKeown, N.M.; Troy, L.M.; Jacques, P.F.; Hoffmann, U.; O’Donnell, C.J.; Fox, C.S. Whole- and refined-grain intakes are differentially associated with abdominal visceral and subcutaneous adiposity in healthy adults: The Framingham Heart Study. Am. J. Clin. Nutr. 2010, 92, 1165–1171. [Google Scholar] [CrossRef] [Green Version]
- Ortega, R.M.; Aparicio, A.; Jiménez-Ortega, A.I.; Rodríguez-Rodríguez, E. Cereales de grano completo y sus beneficios sanitarios. Nutr. Hosp. 2015, 32, 25–31. [Google Scholar] [CrossRef]
- Urrialde, R. Update about reformulated beverages with less and free sugars for Spain and Portugal. Nutr. Hosp. 2020. [Google Scholar] [CrossRef]
- Brimblecombe, J.; McMahon, E.; Ferguson, M.; De Silva, K.; Peeters, A.; Miles, E.; Wycherley, T.; Minaker, L.; Greenacre, L.; Gunther, A.; et al. Effect of restricted retail merchandising of discretionary food and beverages on population diet: A pragmatic randomised controlled trial. Lancet Planet Health 2020, 4, e463–e473. [Google Scholar] [CrossRef]
- Klohe-Lehman, D.; Freeland-Graves, J.; Anderson, E.R.; McDowell, T.; Clarke, K.K.; Hanss-Nuss, H.; Cai, G.; Puri, D.; Milani, T.J. Nutrition Knowledge Is Associated with Greater Weight Loss in Obese and Overweight Low-Income Mothers. J. Am. Diet. Assoc. 2006, 106, 65–75. [Google Scholar] [CrossRef]
- Moore, T.; Alsabeeh, N.; Apovian, C.; Murphy, M.; Coffman, G.; Cabral, H. Weight, Blood Pressure, and Dietary Benefits After 12 Months of a Web-based Nutrition Education Program (DASH for Health): Longitudinal Observational Study. J. Med. Internet Res. 2008, 10, e52. [Google Scholar] [CrossRef]
- Gajewska, D.; Kucharska, A.; Kozak, M.; Wunderlich, S.; Niegowska, J. Effectiveness of Individual Nutrition Education Compared to Group Education, in Improving Anthropometric and Biochemical Indices among Hypertensive Adults with Excessive Body Weight: A Randomized Controlled Trial. Nutrients 2019, 11, 2921. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hooper, L.; Abdelhamid, A.; Bunn, D.; Brown, T.; Summerbell, C.D.; Skeaff, C.M. Effects of total fat intake on body weight. Cochrane Database Syst. Rev. 2015, CD011834. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chait, A.; Den Hartigh, L.J. Adipose Tissue Distribution, Inflammation and Its Metabolic Consequences, Including Diabetes and Cardiovascular Disease. Front. Cardiovasc. Med. 2020, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thiriet, M. Hyperlipidemias and Obesity. Vasculopathies 2019, 8, 331–548. [Google Scholar] [CrossRef]
- Sun, M.; Zhang, L.; Chen, S.; Liu, X.; Shao, X.; Zou, H. Association of C-Reactive Protein and Metabolic Disorder in a Chinese Population. Int. J. Environ. Res. Public Health 2015, 12, 8228–8242. [Google Scholar] [CrossRef]
- Abbey, E.L.; González-Becerra, K.; Rosales-Chávez, G.; Mora-Jiménez, A.; Hernández-Cañaveral, I.; Martínez-López, E. Low-grade chronic inflammation is attenuated by exercise training in obese adults through down-regulation of ASC gene in peripheral blood: A pilot study. Genes Nutr. 2020, 15, 15. [Google Scholar] [CrossRef]
- Leung, A.W.Y.; Chan, R.S.M.; Sea, M.M.M.; Woo, J. Psychological Factors of Long-Term Dietary and Physical Activity Adherence among Chinese Adults with Overweight and Obesity in a Community-Based Lifestyle Modification Program: A Mixed-Method Study. Nutrients 2020, 12, 1379. [Google Scholar] [CrossRef] [PubMed]
| Variable | Mean (SD)/n (%) |
|---|---|
| Age, years | 50.23 (11.9) |
| Sex, % | |
| Female | 56 (84.8) |
| Male | 10 (15.2) |
| Marital status, N, % | |
| Partner | 12 (18.2) |
| No partner | 54 (81.8) |
| Educational level, N, % | |
| Illiterate | 6 (9.1) |
| Primary | 39 (59) |
| Higher | 21 (31.8) |
| Physical activity | |
| Sedentary | 26 (39.4) |
| Moderate | 40 (60.6) |
| Pre Mean (SD) | Post Mean (SD) | MD | 95%CI (Lower) | 95%CI (Upper) | p-Value | |
|---|---|---|---|---|---|---|
| Weight (kg) | 87.24 (16.45) | 84.51 (16.81) | 2.73 | 1.78 | 3.68 | <0.001 |
| BMI (kg/m2) | 32.87 (5.60) | 31.79 (5.69) | 1.08 | 0.71 | 1.45 | <0.001 |
| Waist-hip index | 0.98 (0.08) | 0.97 (0.07) | 0.01 | 0.00 | 0.03 | 0.009 |
| Waist circumference (cm) | 109.02 (12.99) | 105.32 (13.54) | 3.70 | 2.21 | 5.18 | <0.001 |
| Waist-height ratio | 0.67 (0.08) | 0.65 (0.08) | 0.02 | 0.01 | 0.03 | <0.001 |
| Fat (%) | 41.22 (8.18) | 39.68 (7.54) | 1.54 | 0.23 | 2.85 | 0.022 |
| Glucose(mg/dl) | 100.14 (25.96) | 99.70 (25.91) | 0.44 | −2.53 | 3.40 | 0.769 |
| Total cholesterol (mg/dl) | 212.30 (24.50) | 207.20 (32.03) | 5.10 | −1.68 | 11.87 | 0.137 |
| HDL-cholesterol (mg/dl) | 55.51 (13.21) | 53.18 (11.93) | 2.33 | 0.92 | 3.74 | 0.002 |
| LDL-cholesterol (mg/dl) | 128.39 (22.93) | 126.92 (29.40) | 1.47 | −4.97 | 7.90 | 0.650 |
| Triglycerides (mg/dl) | 142.93 (65.41) | 135.93 (55.06) | 7.00 | −4.81 | 18.81 | 0.240 |
| CRP (mg/dl) | 0.59 (0.59) | 0.52 (0.51) | 0.07 | −0.01 | 0.15 | 0.084 |
| Pre Mean (SD) | Post Mean (SD) | MD | 95%CI (lower) | 95%CI (upper) | p-Value | ||
|---|---|---|---|---|---|---|---|
| Fish and seafood | 3–4 s/week | 6.91(3.55) | 7.24 (5.34) | −0.33 | −1.56 | 0.90 | 0.596 |
| Lean meat and poultry | 3–4 s/week | 3.20 (1.58) | 4.23 (3.26) | −1.03 | −1.82 | −0.24 | 0.011 |
| Eggs | 3–4 s/week | 2.52 (1.20) | 2.40 (1.08) | 0.13 | −0.19 | 0.44 | 0.427 |
| Legumes | 2–4 s/week | 2.11 (1.46) | 2.30 (2.33) | −0.19 | −0.82 | 0.44 | 0.547 |
| Nuts and seeds | 3–7 s/week | 1.50 (1.78) | 1.00 (1.80) | 0.51 | 0.00 | 1.01 | 0.048 |
| Dairy products | 2–4 s/day | 2.85 (1.48) | 2.74 (2.14) | 0.11 | −0.38 | 0.59 | 0.669 |
| Olive oil | 2–6 s/d | 2.37 (1.13) | 1.79 (1.25) | 0.58 | 0.25 | 0.92 | 0.001 |
| Vegetables | More than 2 s/day | 4.67(2.12) | 5.11 (3.42) | −0.44 | −1.26 | 0.39 | 0.296 |
| Fruits | More than 2 s/day | 4.18 (4.19) | 3.86 (3.38) | 0.32 | −0.53 | 1.17 | 0.456 |
| Cereals | 4–6 s/day | 2.81 (1.37) | 2.21(1.31) | 0.61 | 0.24 | 0.97 | 0.001 |
| Water | 4–8 s/day | 1.70 (1.02) | 1.87 (1.44) | −0.17 | −0.49 | 0.15 | 0.295 |
| Wine and beer | Sparingly | 0.21 (0.36) | 0.31 (0.58) | −0.10 | −0.23 | 0.02 | 0.114 |
| Fats | Sparingly | 0.52 (0.75) | 0.46 (0.75) | 0.07 | −0.13 | 0.27 | 0.494 |
| Sweets | Sparingly | 2.98 (3.16) | 1.74 (1.69) | 1.23 | 0.55 | 1.92 | 0.001 |
| Soft drinks | Sparingly | 0.52 (0.80) | 0.29 (0.45) | 0.23 | 0.10 | 0.37 | 0.001 |
| High-fat and processed meats | Sparingly | 1.37 (0.67) | 0.93 (0.53) | 0.43 | 0.26 | 0.61 | <0.001 |
| Macronutrients | Recommendation | Pre Mean (SD)/% cal/Day | Post Mean (SD)/% cal/Day | MD | 95CI% (Lower) | 95%CI (Upper) | P-Value |
|---|---|---|---|---|---|---|---|
| Energy, kcal/day | 2200–2900 | 2519.29 (759.67) | 2118.66 (681.05) | 400.63 | 220.33 | 580.93 | <0.001 |
| Proteins, g/day | 80–110 | 111.33 (32.21)/19.5 | 105.80(40.14)/21.2 | 5.53 | −4.14 | 15.21 | 0.26 |
| Carbohydrates, g/day | 300–400 | 245.51 (100.11)/39.5 | 209.27 (80.50)/41 | 36.25 | 14.13 | 58.36 | <0.001 |
| Fiber, g/day | 25–38 | 35.68(14.79) | 35.73 (18.83) | −0.05 | −4.79 | 4.69 | 0.98 |
| Total fats, g/day | 73–97 | 112.43(36.03)/41 | 85.70 (33.67)/37.8 | 26.72 | 16.92 | 36.52 | <0.001 |
| Saturated fatty acids, g/day | <22 | 32.22 (11.97)/12.91 | 24.23 (11.40)/11.8 | 7.99 | 4.85 | 11.14 | <0.001 |
| Monounsaturated, g/day | 27–49 | 53.08 (18.24)/19.96 | 39.26 (16.58)/18.2 | 13.83 | 8.90 | 18.75 | <0.001 |
| Polyunsaturated, g/day | <26 | 18.38 (7.43)/7.96 | 14.97 (8.10)/7.8 | 3.41 | 1.17 | 5.64 | <0.001 |
| Cholesterol, mg/day | 300 | 315.92 (99.11) | 298.93 (145.44) | 16.99 | −16.78 | 50.77 | 0.32 |
| Micronutrients | Recommendation | Pre Mean (SD) | Post Mean (SD) | MD | 95CI% (Lower) | 95%CI (Upper) | p-Value |
| Calcium, mg | 1000–1200 | 1148.56 (438.85) | 1096.52 (544.92) | 52.04 | −75.57 | 179.66 | 0.42 |
| Iron, mg | 10–18 | 18.41 (5.61) | 18.52 (8.83) | −0.12 | −2.27 | 2.04 | 0.91 |
| Iodine, μg | 120–140 | 133.18 (40.22) | 134.73 (60.84) | −1.55 | −15.78 | 12.68 | 0.83 |
| Magnesium, mg | 300–350 | 473.56 (153.47) | 460.31 (186.91) | 13.25 | −33.96 | 60.46 | 0.58 |
| Zinc, mg | 15 | 12.50 (3.66) | 11.58 (4.42) | 0.92 | −0.13 | 1.97 | 0.09 |
| Selenium, μg | 55 | 64.65 | 52.69 | 12.96 | 2.42 | 25.03 | 0.02 |
| Sodium, mg | 1000–5000 | 5340.68 (1763.24) | 3885.29 (1556.03) | 1455.38 | 943.53 | 1967.23 | <0.001 |
| Potassium, mg | 3500 | 5120.20 (1819.96) | 5189.10 (2370.53) | −68.89 | −657.19 | 519.41 | 0.82 |
| Phosphorus, mg | 700 | 2001.42 (631.76) | 1887.43 (815.46) | 114.00 | −66.00 | 294.00 | 0.21 |
| Vitamin B1, mg (Thiamine) | 1–1.2 | 2.06 (0.67) | 1.97 (0.77) | 0.09 | −0.10 | 0.28 | 0.35 |
| Vitamin B2, mg (Riboflavin) | 1.3–1.6 | 2.29 (0.68) | 2.30 (1.01) | −0.01 | −0.23 | 0.21 | 0.94 |
| Vitamin B3, mg (Niacin) | 14–17 | 45.30 (13.64) | 42.74 (17.13) | 2.56 | −1.70 | 6.81 | 0.23 |
| Vitamin B6, mg (Pyridoxine) | 1.2–1.6 | 2.80 (0.86) | 2.90 (1.31) | −0.09 | −0.40 | 0.22 | 0.56 |
| Vitamin B9, μg (Folic acid) | 400 | 563.12 (235.81) | 612.59 (374.31) | −49.48 | −142.76 | 43.81 | 0.29 |
| Vitamin B12, μg | 2 | 15.70 (9.61) | 13.73 (15.31) | 1.97 | −2.12 | 6.06 | 0.34 |
| Vitamin C, mg | 60 | 38.88 (23.19) | 42.36 (27.56) | −3.47 | −10.05 | 3.1 | 0.30 |
| Retinol, μg | 600–700 | 733.18 (77.44) | 579.63 (86.31) | 153.55 | −87.95 | 395.04 | 0.21 |
| Carotenes, μg | 800–1000 | 8388.86 (4288.4) | 9505.68 (7325.5) | −1116.82 | −3048.24 | 814.60 | 0.25 |
| Vitamin A, mg | 1000–2000 | 2087.35 (934.65) | 2128.41 (1491.2) | −41.07 | −399.31 | 317.18 | 0.82 |
| Vitamin D, μg | 5 | 2.40 (1.41) | 2.47 (1.65) | −0.06 | −0.49 | 0.36 | 0.76 |
| Vitamin E, mg6 | 15 | 17.25 (7.72) | 15.71 (9.18) | 1.54 | −0.83 | 3.91 | 0.20 |
| Alcohol, s/day | 1–2 | 2.07 (3.74) | 2.97 (5.60) | −0.90 | −2.09 | 0.29 | 0.13 |
| Water, mL | 2700–3700 | 1981.63 (690.57) | 2064.88 (913.19) | −83.24 | −301.89 | 135.40 | 0.45 |
| Beta | 95%CI (Lower) | 95%CI (Upper) | p-Value | |
|---|---|---|---|---|
| Moderate physical activity | 8.67 | 3.23 | 14.10 | 0.003 |
| Change in vegetables | 1.17 | 0.37 | 1.98 | 0.005 |
| Change in water | 1.8 | −0.08 | 3.69 | 0.061 |
| Change in CRP | −4.88 | −13.22 | 3.5 | 0.245 |
| Change in dairy products | −0.92 | −1.79 | 0.27 | 0.157 |
| Change in nuts | −1.5 | −3.22.66 | −0.35 | 0.12 |
| Change in sweets | −1.56 | −2.49 | −0.64 | 0.001 |
| Change in high-fat and processed meats | −0.88 | −1.68 | −0.08 | 0.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Hernández, L.; Martínez-Arnau, F.M.; Pérez-Ros, P.; Drehmer, E.; Pablos, A. Improved Nutritional Knowledge in the Obese Adult Population Modifies Eating Habits and Serum and Anthropometric Markers. Nutrients 2020, 12, 3355. https://0-doi-org.brum.beds.ac.uk/10.3390/nu12113355
López-Hernández L, Martínez-Arnau FM, Pérez-Ros P, Drehmer E, Pablos A. Improved Nutritional Knowledge in the Obese Adult Population Modifies Eating Habits and Serum and Anthropometric Markers. Nutrients. 2020; 12(11):3355. https://0-doi-org.brum.beds.ac.uk/10.3390/nu12113355
Chicago/Turabian StyleLópez-Hernández, Lourdes, Francisco Miguel Martínez-Arnau, Pilar Pérez-Ros, Eraci Drehmer, and Ana Pablos. 2020. "Improved Nutritional Knowledge in the Obese Adult Population Modifies Eating Habits and Serum and Anthropometric Markers" Nutrients 12, no. 11: 3355. https://0-doi-org.brum.beds.ac.uk/10.3390/nu12113355





