Vitamin D Supplementation Improves the Effects of the Rehabilitation Program on Balance and Pressure Distribution in Patients after Anterior Cervical Interbody Fusion-Randomized Control Trial
Abstract
:1. Introduction
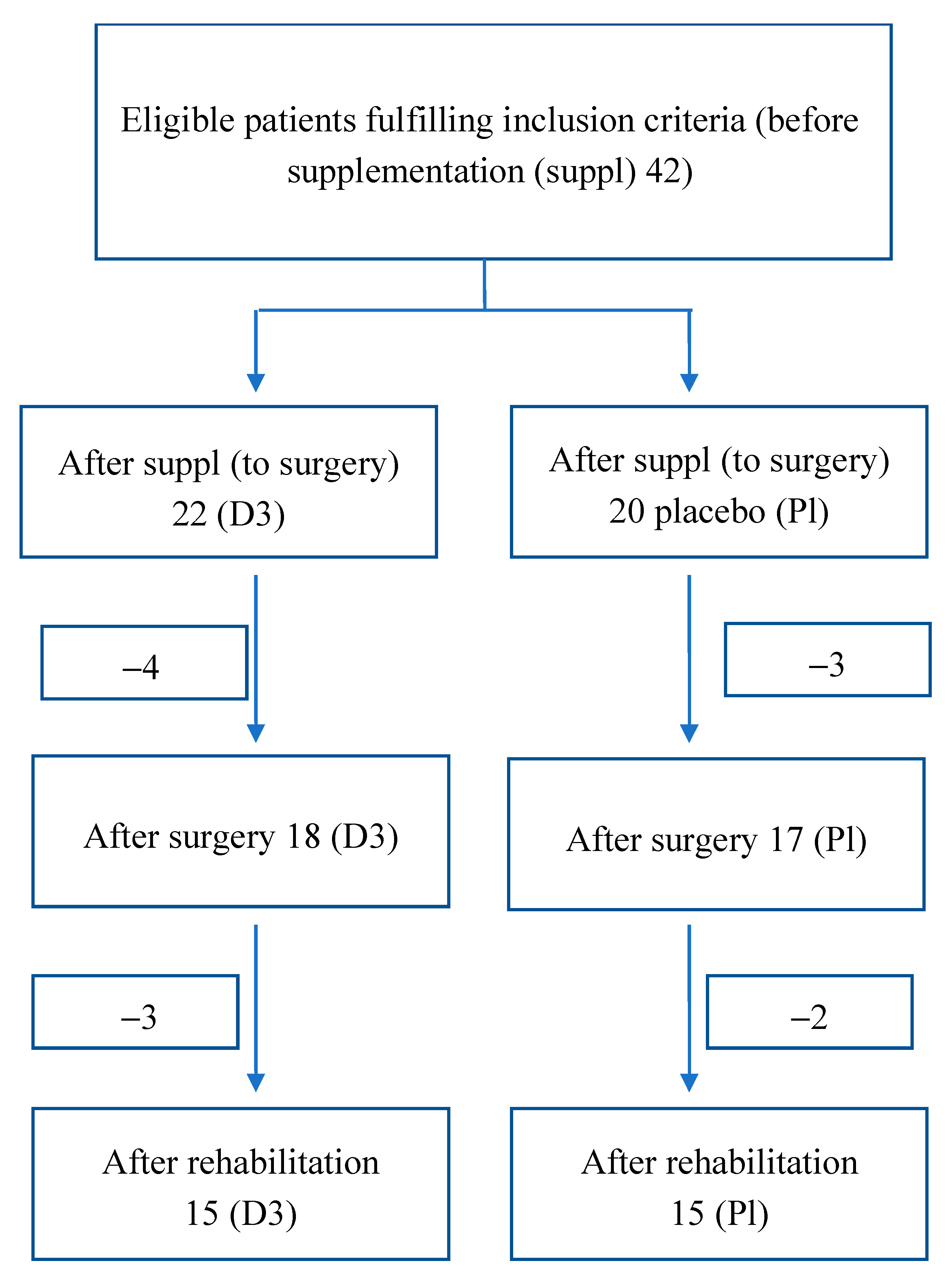
2. Materials and Methods
2.1. Participants, Therapists, and Centers
2.1.1. Including Criteria
2.1.2. Excluding Criteria
2.2. Functional Tests
2.3. Sample Collection
2.4. Postural Stability Test
2.5. Risk of Falls Test
2.6. Limits of Stability Test
2.7. Romberg Test
- (1)
- the ellipse sway area (mm2), defined as a 95% confidence ellipse area for the mean movements of the center of pressure (CoP) anterior, posterior, medial, and lateral coordinates.
- (2)
- the sway rate (mm/s), defined as the mean speed of movement of the CoP throughout the testing period.
- (3)
- the CoP path length (mm), defined as the absolute length of the CoP path movements throughout the testing period.
- (4)
- the average pressure distribution of the left and right feet expressed in body weight (%). Additionally, the bilateral pressure distribution asymmetry score was calculated as the absolute difference in pressure distribution between the legs. In a perfect symmetrical stance, this variable is zero [20].
2.8. Data Analysis
2.9. Rehabilitation Protocol
3. Results
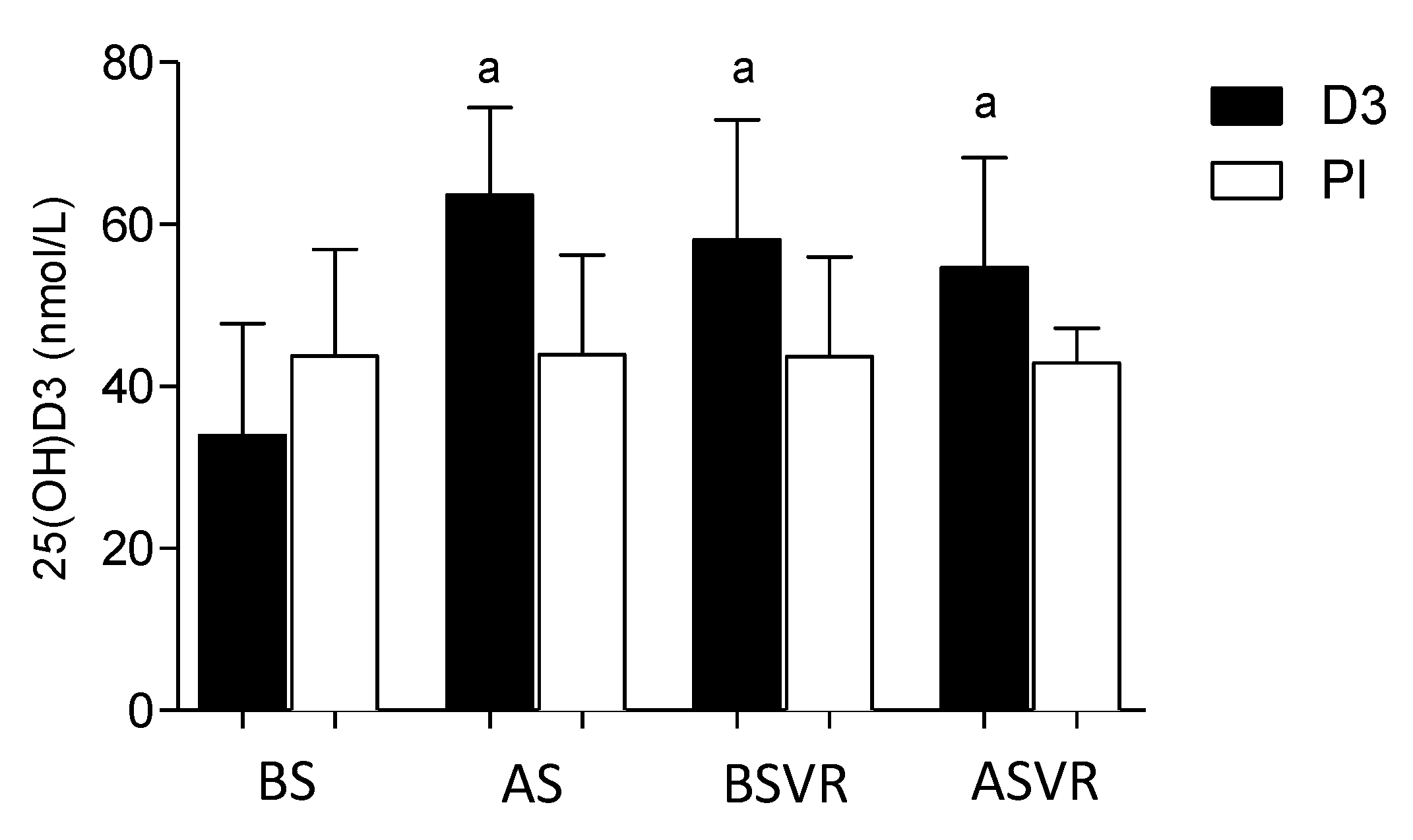
3.1. Vitamin D
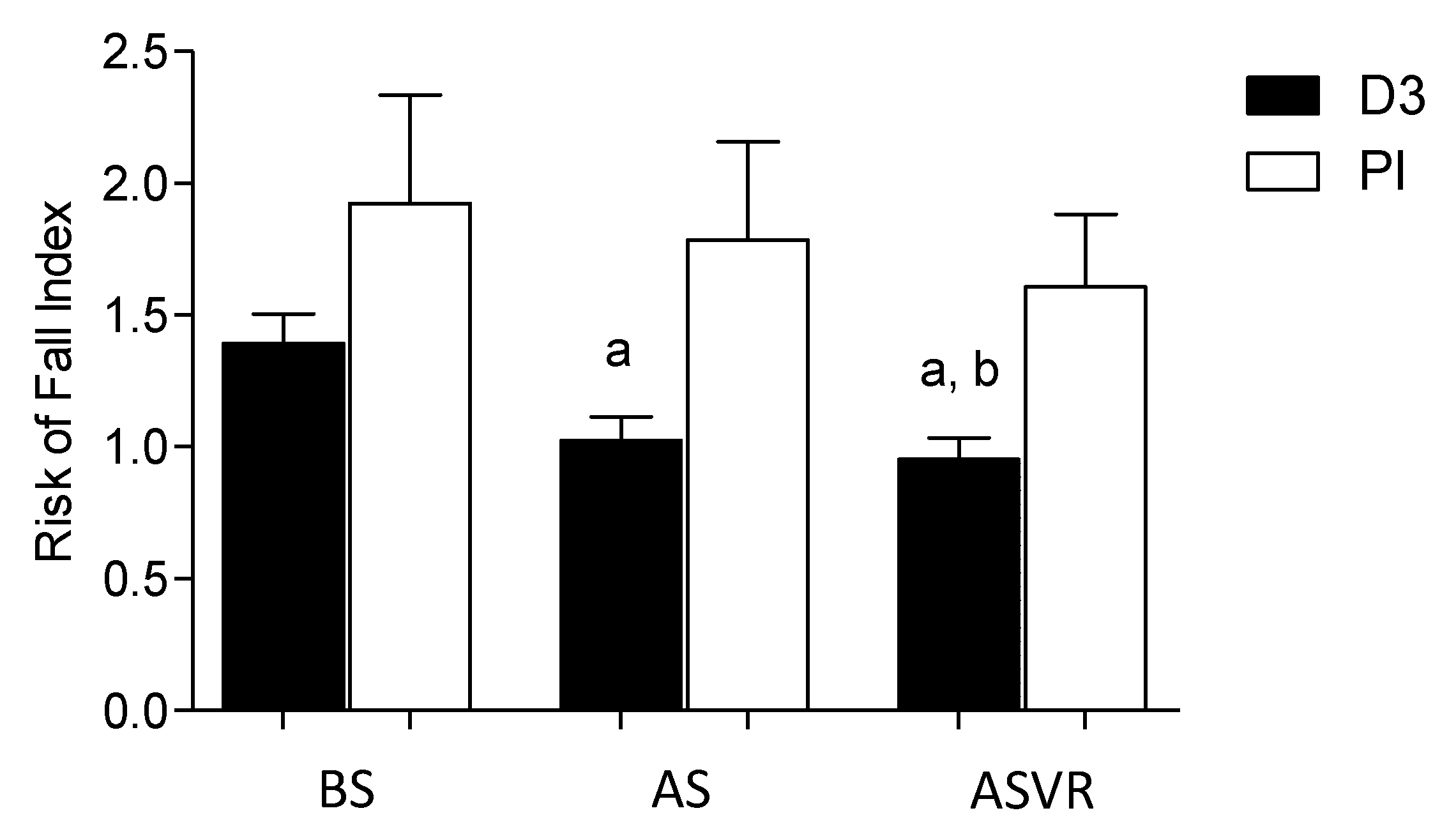
3.2. Risk of Falls
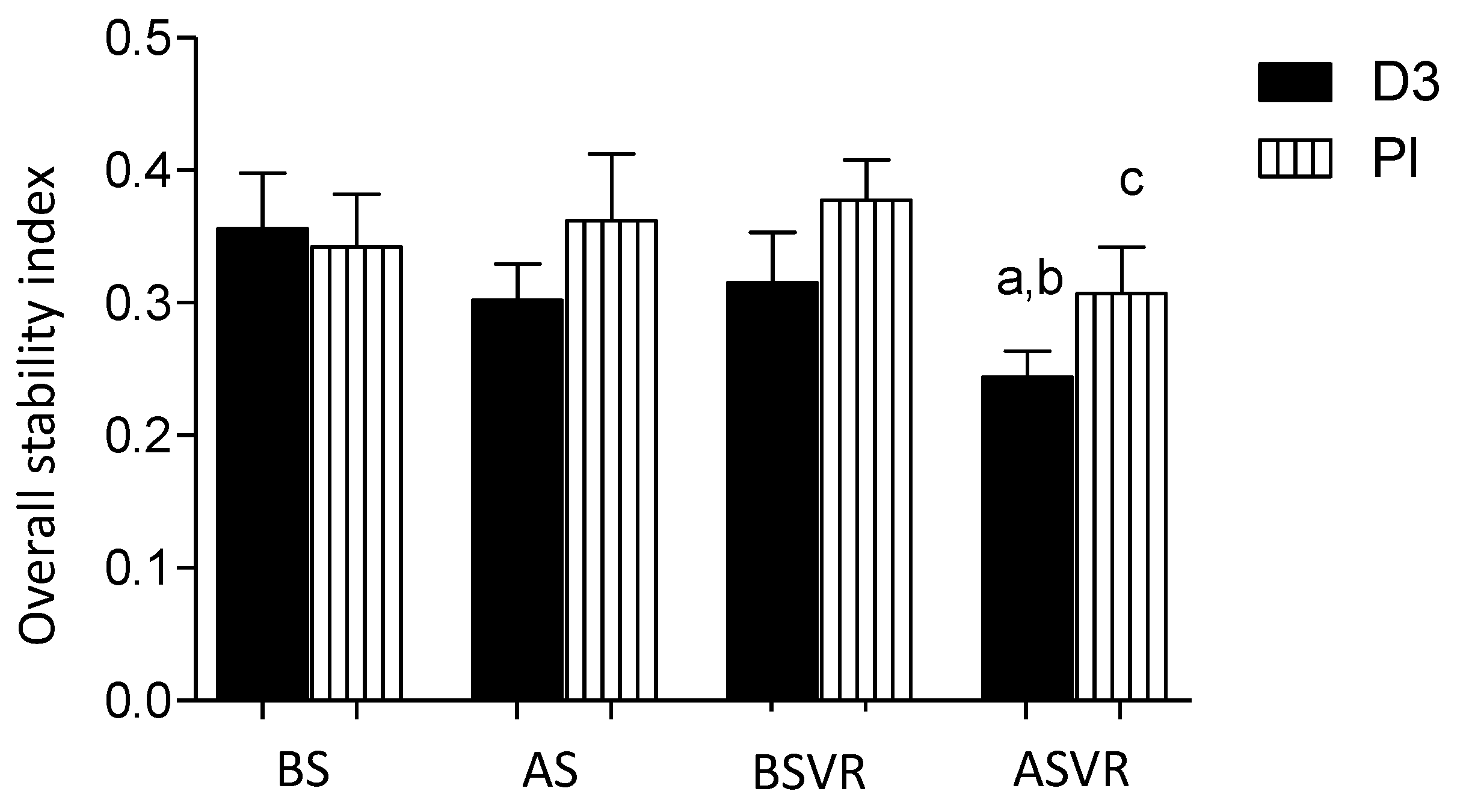
3.3. Postural Stability
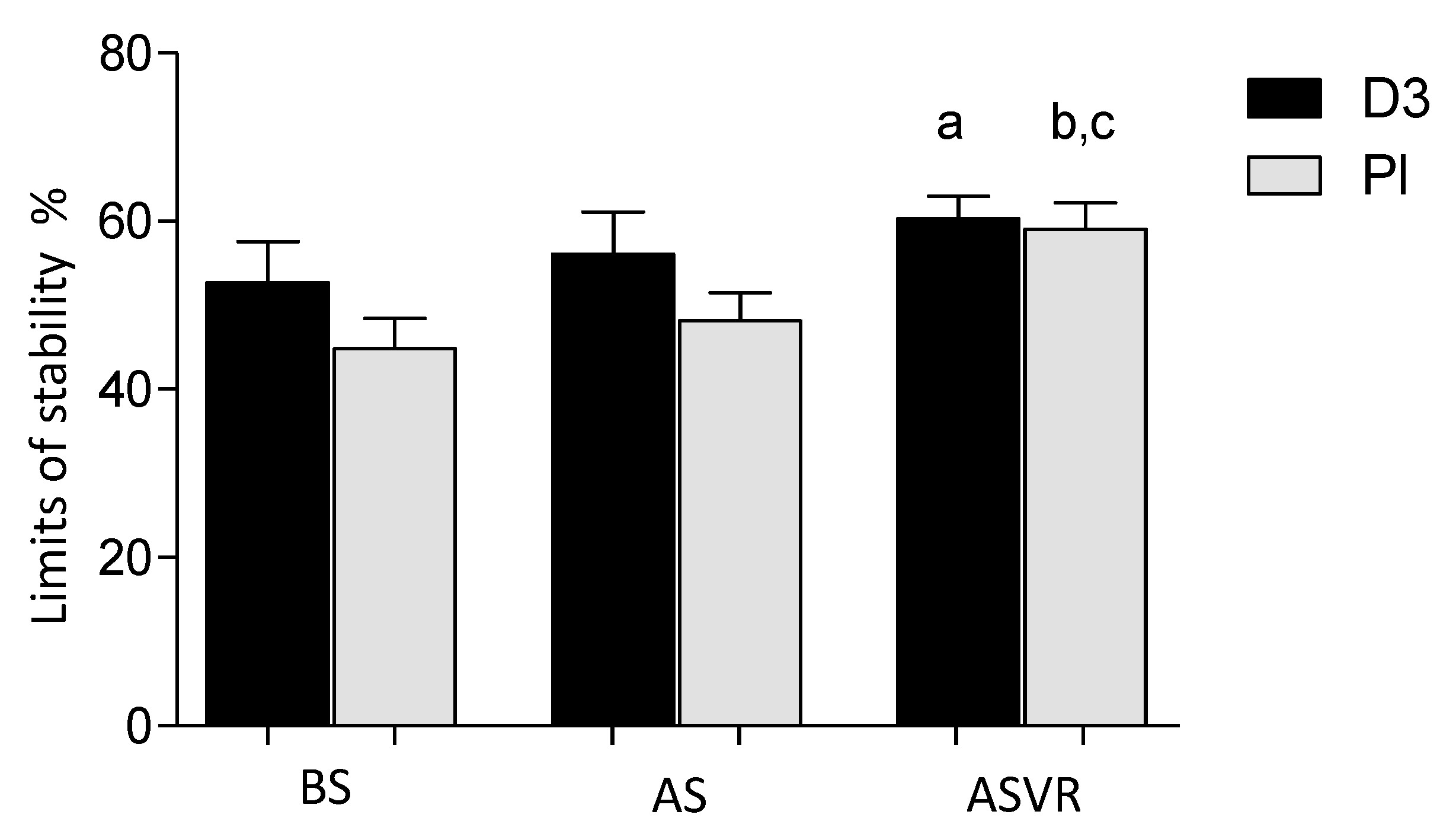
3.4. Limits of Stability
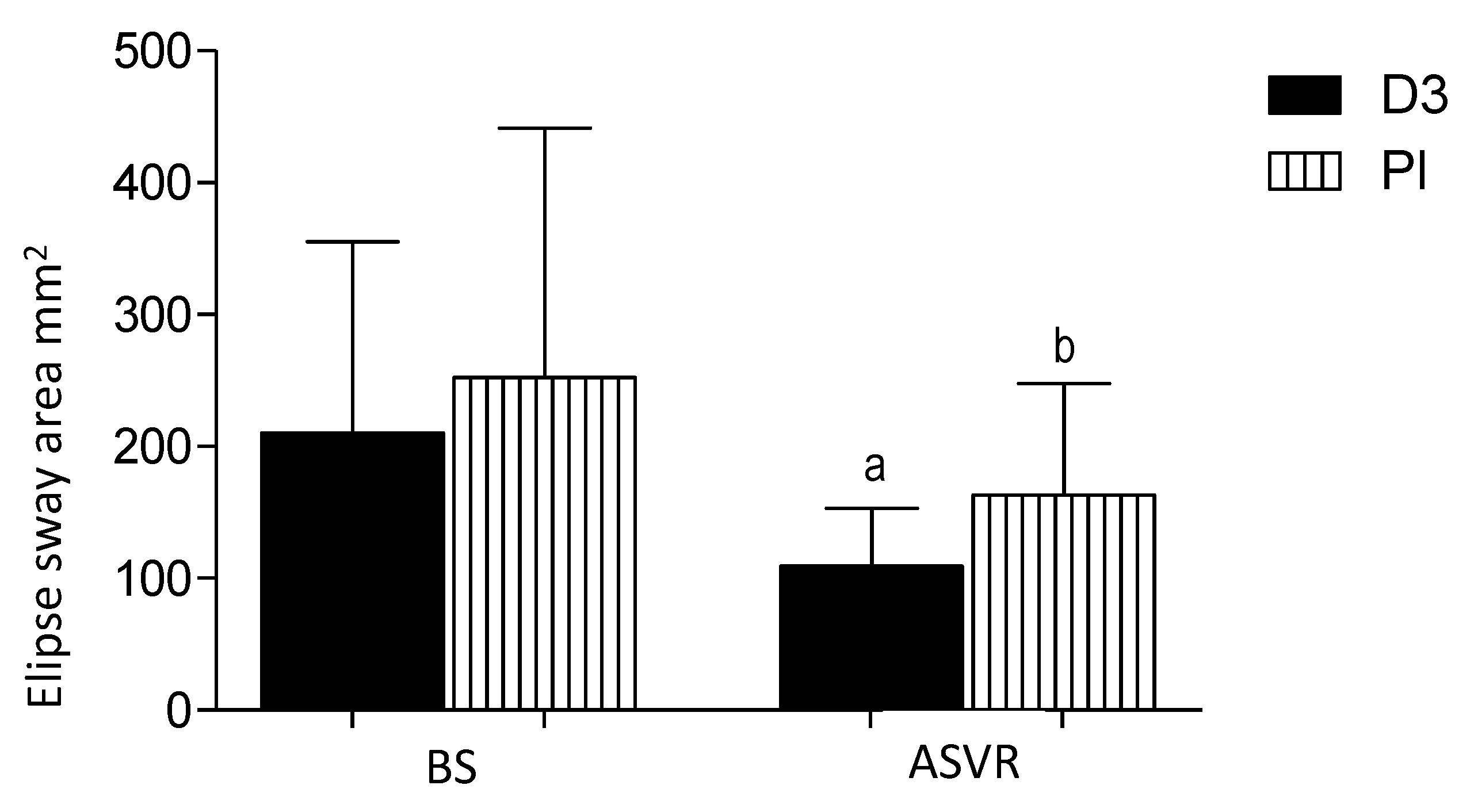
3.5. Ellipse Sway Area
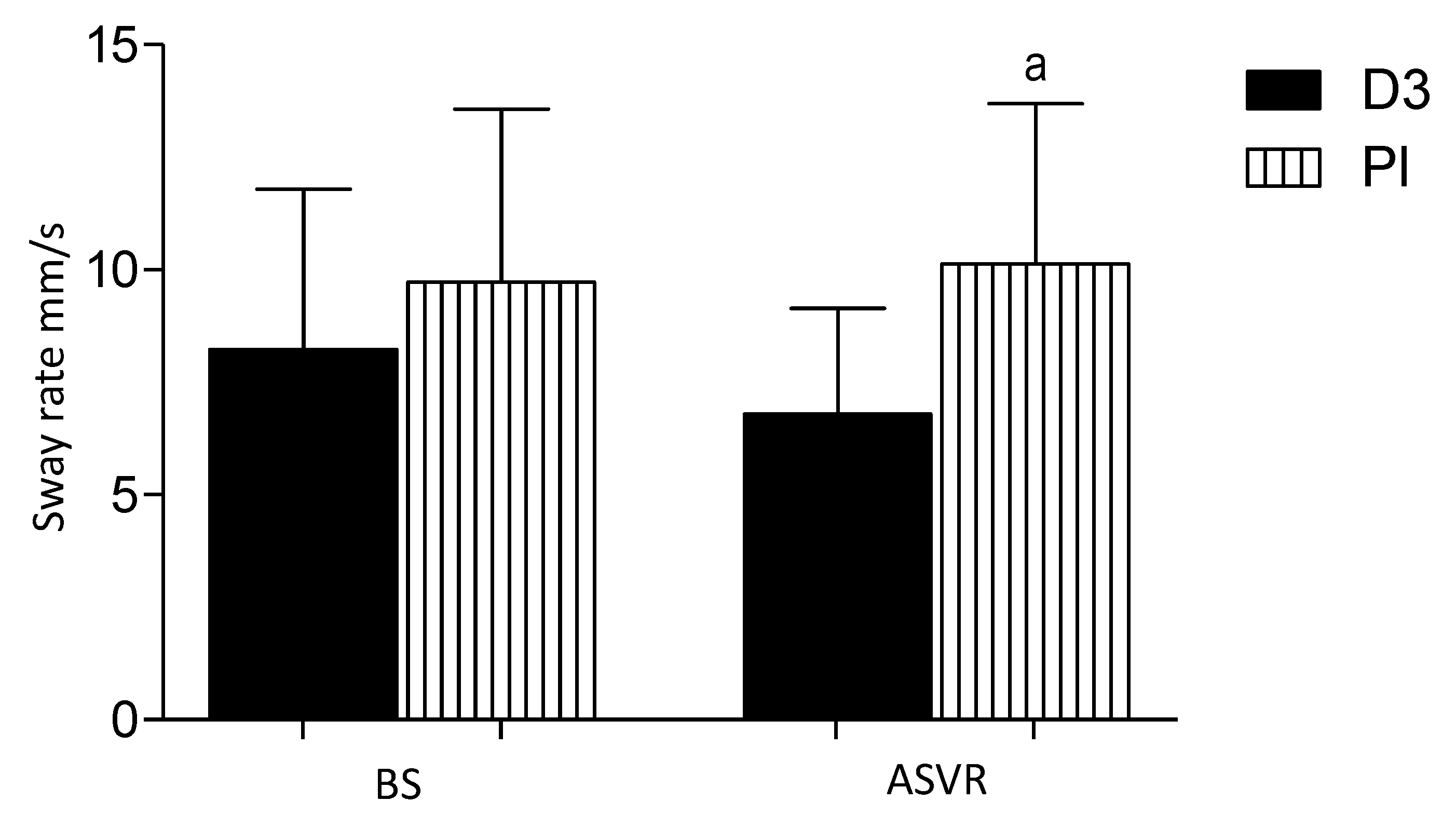
3.6. Sway Rate Center of Pressure (COP AV)
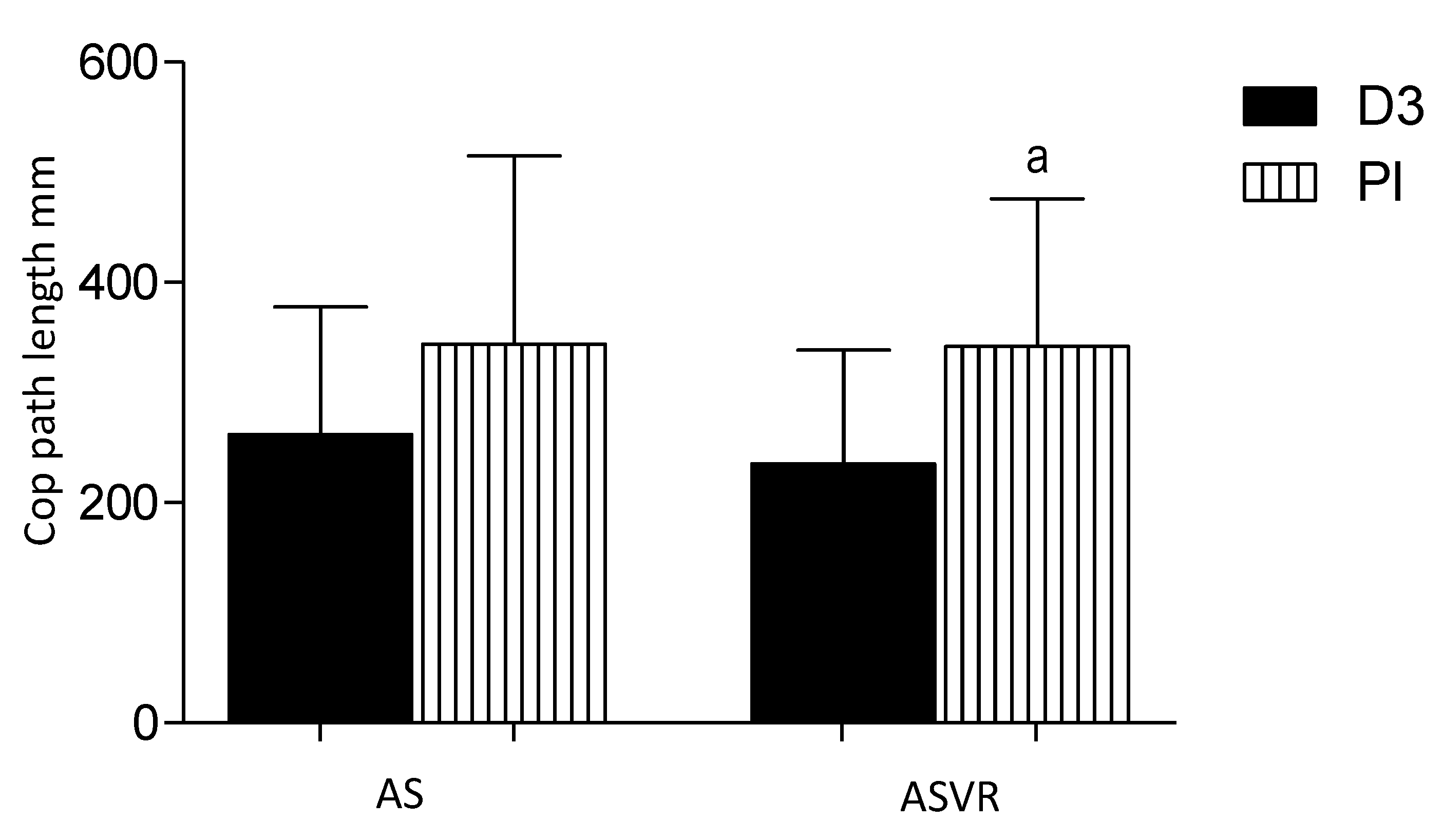
3.7. CoP Path Length
4. Discussion
Limitation of the Study
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ACIF | Anterior cervical interbody fusion |
| OSI | Overall postural stability index |
| Pl | Placebo |
| LOS | Limits of stability |
| RFT | Risk of falls |
| PST | Postural stability |
| BS | Before supplementation |
| AS | After supplementation |
| BSVR | After surgery—Before supervising rehabilitation |
| ASVR | After supervising rehabilitation |
| 25(OH)D3 | 25-hydroxy cholecalciferol |
| 1,25(OH)2D3 | 1,25-dihydroxycholecalciferol |
| VDR | Vitamin D receptor |
| MRI | Magnetic resonance imaging |
| BBS | Biodex Balance System |
| CVs | Coefficients of variability |
| APSI | Anterior-Posterior Stability Index |
| MLSI | Medial-Lateral Stability Index |
| EC | Eyes closed |
| CoP | Center of pressure |
| SDs | Standard deviations |
| CNS | Central Nervous System |
References
- Meleger, A.L.; Krivickas, L.S. Neck and back pain: Musculoskeletal disorders. Neurol. Clin. 2007, 25, 419–438. [Google Scholar] [CrossRef] [PubMed]
- Peolsson, A.; Oberg, B.; Wibault, J.; Dedering, A.; Zsigmond, P.; Bernfort, L.; Kammerlind, A.S.; Persson, L.C.G.; Lofgren, H. Outcome of physiotherapy after surgery for cervical disc disease: A prospective randomised multi-centre trial. BMC Musculoskel. Dis. 2014, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peolsson, A.; Soderlund, A.; Engquist, M.; Lind, B.; Lofgren, H.; Vavruch, L.; Holtz, A.; Winstrom-Christersson, A.; Isaksson, I.; Oberg, B. Physical Function Outcome in Cervical Radiculopathy Patients After Physiotherapy Alone Compared with Anterior Surgery Followed by Physiotherapy A Prospective Randomized Study With a 2-Year Follow-up. Spine 2013, 38, 300–307. [Google Scholar] [CrossRef]
- Coronado, R.A.; Devin, C.J.; Pennings, J.S.; Vanston, S.W.; Fenster, D.E.; Hills, J.M.; Aaronson, O.S.; Schwarz, J.P.; Stephens, B.F.; Archer, K.R. Early Self-directed Home Exercise Program after Anterior Cervical Discectomy and Fusion A Pilot Study. Spine 2020, 45, 217–225. [Google Scholar] [CrossRef]
- Pludowski, P.; Grant, W.B.; Bhattoa, H.P.; Bayer, M.; Povoroznyuk, V.; Rudenka, E.; Ramanau, H.; Varbiro, S.; Rudenka, A.; Karczmarewicz, E.; et al. Vitamin d status in central europe. Int. J. Endocrinol. 2014, 2014, 589587. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.T.; Tavera-Mendoza, L.E.; Laperriere, D.; Libby, E.; MacLeod, N.B.; Nagai, Y.; Bourdeau, V.; Konstorum, A.; Lallemant, B.; Zhang, R.; et al. Large-scale in silico and microarray-based identification of direct 1,25-dihydroxyvitamin D3 target genes. Mol. Endocrinol. 2005, 19, 2685–2695. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bischoff, H.A.; Borchers, M.; Gudat, F.; Duermueller, U.; Theiler, R.; Stahelin, H.B.; Dick, W. In situ detection of 1,25-dihydroxyvitamin D-3 receptor in human skeletal muscle tissue. Histochem. J. 2001, 33, 19–24. [Google Scholar] [CrossRef]
- Mieszkowski, J.; Niespodzinski, B.; Kochanowicz, A.; Gmiat, A.; Prusik, K.; Prusik, K.; Kortas, J.; Ziemann, E.; Antosiewicz, J. The Effect of Nordic Walking Training Combined with Vitamin D Supplementation on Postural Control and Muscle Strength in Elderly PeopleA Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2018, 15, 1951. [Google Scholar] [CrossRef] [Green Version]
- Rai, V.; Dietz, N.E.; Dilisio, M.F.; Radwan, M.M.; Agrawal, D.K. Vitamin D attenuates inflammation, fatty infiltration, and cartilage loss in the knee of hyperlipidemic microswine. Arthritis Res. Ther. 2016, 18, 203. [Google Scholar] [CrossRef] [Green Version]
- Pludowski, P.; Ducki, C.; Konstantynowicz, J.; Jaworski, M. Vitamin D status in Poland. Polskie Archiwum Medycyny Wewnȩtrznej 2016, 126, 530–539. [Google Scholar] [CrossRef] [Green Version]
- Stoker, G.E.; Buchowski, J.M.; Chen, C.T.; Kim, H.J.; Park, M.S.; Riew, K.D. Hypovitaminosis D and Cervical Disk Herniation among Adults Undergoing Spine Surgery. Glob. Spine J. 2013, 3, 231–236. [Google Scholar] [CrossRef] [Green Version]
- Warner, S.J.; Garner, M.R.; Nguyen, J.T.; Lorich, D.G. Perioperative vitamin D levels correlate with clinical outcomes after ankle fracture fixation. Arch. Orthop. Trauma Surg. 2016, 136, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Arnold, B.L.; Schmitz, R.J. Examination of Balance Measures Produced by the Biodex Stability System. J. Athl. Train. 1998, 33, 323–327. [Google Scholar]
- Siddiqi, F.A.; Masood, T. Training on Biodex balance system improves balance and mobility in the elderly. J. Pak. Med. Assoc. 2018, 68, 1655–1659. [Google Scholar]
- Stephenson, J.; Zesiewicz, T.; Gooch, C.; Wecker, L.; Sullivan, K.; Jahan, I.; Kim, S.H. Gait and balance in adults with Friedreich’s ataxia. Gait Posture 2015, 41, 603–607. [Google Scholar] [CrossRef]
- Black, F.O.; Wall, C., 3rd; Rockette, H.E., Jr.; Kitch, R. Normal subject postural sway during the Romberg test. Am. J. Otolaryngol. 1982, 3, 309–318. [Google Scholar] [CrossRef]
- Tjernstrom, F.; Bjorklund, M.; Malmstrom, E.M. Romberg ratio in quiet stance posturography--Test to retest reliability. Gait Posture 2015, 42, 27–31. [Google Scholar] [CrossRef] [Green Version]
- Scoppa, F.; Capra, R.; Gallamini, M.; Shiffer, R. Clinical stabilometry standardization: Basic definitions--acquisition interval--sampling frequency. Gait Posture 2013, 37, 290–292. [Google Scholar] [CrossRef]
- Kalron, A. The Romberg ratio in people with multiple sclerosis. Gait Posture 2017, 54, 209–213. [Google Scholar] [CrossRef]
- Kalron, A.; Achiron, A. Postural control, falls and fear of falling in people with multiple sclerosis without mobility aids. J. Neurol. Sci. 2013, 335, 186–190. [Google Scholar] [CrossRef]
- Maier, G.S.; Horas, K.; Seeger, J.B.; Roth, K.E.; Kurth, A.A.; Maus, U. Vitamin D insufficiency in the elderly orthopaedic patient: An epidemic phenomenon. Int. Orthop. 2015, 39, 787–792. [Google Scholar] [CrossRef] [PubMed]
- Maier, G.S.; Seeger, J.B.; Horas, K.; Roth, K.E.; Kurth, A.A.; Maus, U. The prevalence of vitamin D deficiency in patients with vertebral fragility fractures. Bone Joint J. 2015, 97, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Stemmle, J.; Marzel, A.; Chocano-Bedoya, P.O.; Orav, E.J.; Dawson-Hughes, B.; Freystaetter, G.; Egli, A.; Theiler, R.; Staehelin, H.B.; Bischoff-Ferrari, H.A. Effect of 800 IU Versus 2000 IU Vitamin D3 With or Without a Simple Home Exercise Program on Functional Recovery After Hip Fracture: A Randomized Controlled Trial. J. Am. Med. Dir. Assoc. 2019, 20, 530–536 e531. [Google Scholar] [CrossRef] [PubMed]
- Skrobot, W.; Liedtke, E.; Krasowska, K.; Dzik, K.P.; Flis, D.J.; Samoraj-Dereszkiewicz, A.; Libionka, W.; Kortas, J.; Kloc, W.; Antosiewicz, J.; et al. Early Rehabilitation Program and Vitamin D Supplementation Improves Sensitivity of Balance and the Postural Control in Patients after Posterior Lumbar Interbody Fusion: A Randomized Trial. Nutrients 2019, 11, 2202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krasowska, K.; Skrobot, W.; Liedtke, E.; Sawicki, P.; Flis, D.J.; Dzik, K.P.; Libionka, W.; Kloc, W.; Kaczor, J.J. The Preoperative Supplementation With Vitamin D Attenuated Pain Intensity and Reduced the Level of Pro-inflammatory Markers in Patients After Posterior Lumbar Interbody Fusion. Front. Pharmacol. 2019, 10. [Google Scholar] [CrossRef]
- Bischoff-Ferrari, H.A.; Conzelmann, M.; Dick, W.; Theiler, R.; Stahelin, H.B. Effect of vitamin D on muscle strength and relevance in regard to osteoporosis prevention. Z. Rheumatol. 2003, 62, 518–521. [Google Scholar] [CrossRef]
- Dhesi, J.K.; Bearne, L.M.; Moniz, C.; Hurley, M.V.; Jackson, S.H.; Swift, C.G.; Allain, T.J. Neuromuscular and psychomotor function in elderly subjects who fall and the relationship with vitamin D status. J. Bone Miner. Res. 2002, 17, 891–897. [Google Scholar] [CrossRef]
- Gill, J.; Allum, J.H.; Carpenter, M.G.; Held-Ziolkowska, M.; Adkin, A.L.; Honegger, F.; Pierchala, K. Trunk sway measures of postural stability during clinical balance tests: Effects of age. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M438–M447. [Google Scholar] [CrossRef] [Green Version]
- Gmiat, A.; Jaworska, J.; Micielska, K.; Kortas, J.; Prusik, K.; Prusik, K.; Lipowski, M.; Radulska, A.; Szupryczynska, N.; Antosiewicz, J.; et al. Improvement of cognitive functions in response to a regular Nordic walking training in elderly women—A change dependent on the training experience. Exp. Gerontol. 2018, 104, 105–112. [Google Scholar] [CrossRef]
- Treleaven, J. Sensorimotor disturbances in neck disorders affecting postural stability, head and eye movement control. Man. Ther. 2008, 13, 2–11. [Google Scholar] [CrossRef]
- Minasyan, A.; Keisala, T.; Zou, J.; Zhang, Y.; Toppila, E.; Syvala, H.; Lou, Y.R.; Kalueff, A.V.; Pyykko, I.; Tuohimaa, P. Vestibular dysfunction in vitamin D receptor mutant mice. J. Steroid Biochem. Mol. Biol. 2009, 114, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Barker, T.; Henriksen, V.T.; Martins, T.B.; Hill, H.R.; Kjeldsberg, C.R.; Schneider, E.D.; Dixon, B.M.; Weaver, L.K. Higher serum 25-hydroxyvitamin D concentrations associate with a faster recovery of skeletal muscle strength after muscular injury. Nutrients 2013, 5, 1253–1275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, M.; Park, H.; Cho, S.; Lee, M. Vitamin D3 supplementation modulates inflammatory responses from the muscle damage induced by high-intensity exercise in SD rats. Cytokine 2013, 63, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Peolsson, A.; Vavruch, L.; Hedlund, R. Long-term randomised comparison between a carbon fibre cage and the Cloward procedure in the cervical spine. Eur. Spine J. 2007, 16, 173–178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hassan-Smith, Z.K.; Jenkinson, C.; Smith, D.J.; Hernandez, I.; Morgan, S.A.; Crabtree, N.J.; Gittoes, N.J.; Keevil, B.G.; Stewart, P.M.; Hewison, M. 25-hydroxyvitamin D3 and 1,25-dihydroxyvitamin D3 exert distinct effects on human skeletal muscle function and gene expression. PLoS ONE 2017, 12, e0170665. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Girgis, C.M.; Mokbel, N.; Cha, K.M.; Houweling, P.J.; Abboud, M.; Fraser, D.R.; Mason, R.S.; Clifton-Bligh, R.J.; Gunton, J.E. The vitamin D receptor (VDR) is expressed in skeletal muscle of male mice and modulates 25-hydroxyvitamin D (25OHD) uptake in myofibers. Endocrinology 2014, 155, 3227–3237. [Google Scholar] [CrossRef] [Green Version]
- Mieszkowski, J.; Stankiewicz, B.; Kochanowicz, A.; Niespodziński, B.; Kowalik, T.; Żmijewski, M.; Kowalski, K.; Rola, R.; Bieńkowski, T.; Antosiewicz, J. Ultra-Marathon-Induced Increase in Serum Levels of Vitamin D Metabolites: A Double-Blind Randomized Controlled Trial. Nutrients 2020, 12, 3629. [Google Scholar] [CrossRef]
| Week | Intervention |
|---|---|
| I | Instruction about ergonomics behavior during daily activities; instruction about keeping right position with correction of a head, shoulder, and pelvic girdle; and, also, deep trunk stabilization was led. Maintaining a neutral posture movement of the upper and lower limbs was performed. |
| II–III | The same exercise as above, but more difficulty was conducted. Exercises with a head’s laser for control movement of the head was applied. Shoulder’s girdle stabilization, with additional control of the key parts of the body, was carried out. Proprioception exercises were led with opened and closed eyes. Exercises in the closed chain on the wall in a standing position were performed, which were prepared with plank and balance exercises. |
| IV | Balancing exercises with sensorimotor discs with the control of body swaying were conducted. Learning tensions of the deep cervical flexors was managed. |
| V | Increasing the number of isometric contractions of stabilizing muscles exercises and changes in the sequence and time performed of the movement were applied. |
| VI–VII | At the beginning of the sixth week, independent head movements in the range to the threshold of pain in the cervical spines of patients were performed. In the next weeks, an increased intensity and difficulty of the exercises were applied. |
| VIII–X | From the eighth week, patients started plank exercises. After ten weeks of supervised rehabilitation, patients were encouraged to continue their activities at home. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Skrobot, W.; Perzanowska, E.; Krasowska, K.; Flis, D.J.; Dzik, K.P.; Kloc, W.; Kaczor, J.J.; Antosiewicz, J. Vitamin D Supplementation Improves the Effects of the Rehabilitation Program on Balance and Pressure Distribution in Patients after Anterior Cervical Interbody Fusion-Randomized Control Trial. Nutrients 2020, 12, 3874. https://0-doi-org.brum.beds.ac.uk/10.3390/nu12123874
Skrobot W, Perzanowska E, Krasowska K, Flis DJ, Dzik KP, Kloc W, Kaczor JJ, Antosiewicz J. Vitamin D Supplementation Improves the Effects of the Rehabilitation Program on Balance and Pressure Distribution in Patients after Anterior Cervical Interbody Fusion-Randomized Control Trial. Nutrients. 2020; 12(12):3874. https://0-doi-org.brum.beds.ac.uk/10.3390/nu12123874
Chicago/Turabian StyleSkrobot, Wojciech, Ewelina Perzanowska, Katarzyna Krasowska, Damian J. Flis, Katarzyna P. Dzik, Wojciech Kloc, Jan Jacek Kaczor, and Jędrzej Antosiewicz. 2020. "Vitamin D Supplementation Improves the Effects of the Rehabilitation Program on Balance and Pressure Distribution in Patients after Anterior Cervical Interbody Fusion-Randomized Control Trial" Nutrients 12, no. 12: 3874. https://0-doi-org.brum.beds.ac.uk/10.3390/nu12123874





