Healthy Lifestyle Management of Pediatric Obesity with a Hybrid System of Customized Mobile Technology: The PediaFit Pilot Project
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
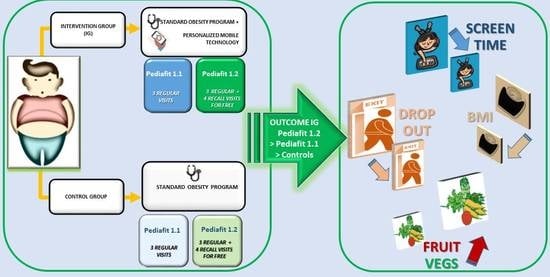
2.2. Study Design
2.3. Messaging Program and Recalls
2.4. Data Collection
2.5. Statistical Data Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A


Appendix B
| Week | Self-Monitoring | Information and Training |
|---|---|---|
| week 1 Sugary drinks | Hi!!! Question of the day: Did you drink sugary drinks yesterday (fruit juices, sodas, iced tea)? | Tip of the day: Did you know that a can of soda contains about eight teaspoons of sugar? So much sugar in addition to being an enemy to your diet is harmful to the whole body. Always prefer a nice glass of fresh water, or homemade plain fruit-iced tea which is good for you and quenches your thirst much more! (with attached photo of a can of soda with the equivalent in sugar) |
| week 2 Physical activity | Hello xxx. Question of the day: did you exercise yesterday? If so, how many hours or minutes? | Tip of the day: Exercise is necessary! Do not use the elevator- taking the stairs or walking to school are great ways to get moving. Try to exercise for at least 30–60 min a day, you will feel better and lose the excess pounds much faster. |
| week 3 Breakfast | Question of the day: did you have breakfast this morning? If so, what did you eat? | Tip of the day: Never skipping breakfast makes your metabolism more efficient and decreases hunger throughout the day. It has also been shown that those who eat breakfast have a lower risk of developing overweight and obesity! A healthy breakfast every morning is essential. For your weight loss journey, always prefer healthy foods and limit packaged ones like snacks and cookies. |
| week 4 Screen-time | Hello!!! Question of the day: how many hours did you spend yesterday in front of TV, mobile phone and computer? | Tip of the day: Try to limit the use of tablets/PCs/TVs to one hour a day. A sedentary lifestyle is one of the most important risk factors for weight gain; try to do physical activity instead of spending time near screens!!! |
| week 5 Sleep | Good morning! Question of the day: how many hours did you sleep last night? | Tip of the day. During sleep, in addition to recovering the energy lost during the day, you produce hormones that you need to grow. Moreover, those who sleep regularly tend to eat less and not accumulate weight excess! During growth it is important to sleep at least 9/10 h a night. A good habit is to always go to sleep at the same time and not use PCs, mobile phones and tablets before falling asleep. |
| week 6 Fruits and vegetables | Question of the day: How many servings of fruit and vegetables did you eat yesterday? | Tip of the day: if you want to lose weight permanently it is important to eat five portions of fruit every day, combining them with vegetables whenever possible! In this way, the right amount of vitamins and minerals is introduced. It is also essential to vary the fruit and vegetables eaten, preferring the one that is part of the green list, with a lower sugar content. |
| Settimana | Automonitoraggio | Informazione E Formazione |
|---|---|---|
| Settimana 1 Bevande zuccherate | Ciao!!! Domanda del giorno: Ieri hai bevuto bevande zuccherate (succhi di frutta, coca cola, Fanta, Thè)? | Consiglio del giorno: Sapevi che una lattina di Coca Cola o di Fanta contengono circa 8 cucchiaini di zucchero? Così tanto zucchero oltre ad essere un nemico per la tua dieta è dannoso per tutto l’organismo. preferisci sempre un bel bicchiere d’acqua fresco, che fa bene e ti disseta molto di più! [con foto allegata di una lattina di Fanta con il corrispettivo in zucchero] |
| Settimana 2 Attività fisica | Ciao xxx. Domanda del giorno: hai fatto attività fisica ieri? Se si, quante ore o minuti? | Buongiorno. Consiglio del giorno: Fare movimento è necessario! Non usare l’ascensore ma prendere le scale o andare a scuola a piedi sono degli ottimi modi per fare movimento. Cerca di fare attività fisica almeno 60 minuti al giorno, ti sentirai meglio e perderai i chili in eccesso molto più velocemente. |
| Settimana 3 Colazione | Domanda del giorno: hai fatto colazione stamattina? Se si, cosa hai mangiato? | Consiglio del giorno: non saltare mai la colazione rende il tuo metabolismo più efficiente e diminuisce la fame durante il giorno. Inoltre, è stato dimostrato che chi fa colazione ha minor rischio di sviluppare sovrappeso e obesità! È fondamentale una colazione sana ogni mattina; per il tuo percorso verso la perdita di peso, preferisci sempre alimenti salutari e limita quelli confezionati come merendine e biscotti. |
| Settimana 4 Screen-time | Ciao!!! Domanda del giorno: quante ore hai passato ieri davanti a tv, cellulare e computer | Consiglio del giorno: Cerca di limitare l’uso di tablet/pc/tv ad un’ora al giorno. La sedentarietà è uno dei più importanti fattori di rischio per l’aumento di peso, prova a fare attività fisica invece di passare tempo vicino agli schermi!!! |
| Settimana 5 Sonno | Buongiorno! Domanda del giorno: quante ore hai dormito ieri notte? | Consiglio del giorno. Durante il sonno, oltre a recuperare l’energia persa durante la giornata, produci ormoni che ti servono per crescere e memorizzi le informazioni che hai ricevuto durante il giorno. Inoltre chi dorme in modo regolare tende a mangiare di meno e non accumulare chili in eccesso! Durante la crescita è importante dormire almeno 9/10 ore per notte. Una buona abitudine è quella di andare a dormire sempre allo stesso orario e non usare pc, cellulari e tablet prima di addormentarsi. |
| Settimana 6 Frutta e verdura | Domanda del giorno: Quante porzioni di frutta e verdura hai mangiato ieri? | Consiglio del giorno: se si vuole perdere peso in modo permanente è importante mangiare cinque porzioni di frutta ogni giorno, associandole quando possibile alla verdura! In questo modo si introduce la giusta quota di vitamine e minerali. E’ fondamentale, inoltre, variare spesso la frutta e la verdura mangiata, preferendo sempre quella che fa parte della lista verde, con minor contenuto di zuccheri. |
Appendix C
| Week | Challenges | Information and Training |
|---|---|---|
| week 1 Sugary drinks | First challenge: Goodbye sugar!!! No fruit juices, sodas, canned tea, for a whole week. Get the whole family involved and let me know every day or in a week how many days you passed the challenge! | Before the next challenge I wanted to remind you why sugary drinks should be avoided; they quickly increase blood sugar levels and this causes the pancreas to produce a huge amount of insulin, the hormone that brings sugar into cells. In the long run it induces a dysfunction of the pancreas which first leads the body to be resistant to your own insulin and subsequently to diabetes! The challenge is over but continuing to avoid these drinks can only do you good! |
| week 2 Physical activity | Second challenge: jump rope! The challenges get complicate but I know you will still succeed! Have you ever tried to jump rope? Try it every day and let me know how you do. You will need to train every day this week, even if only for 15 min. Try it please, let me know how many jumps you do per minute! Good luck. | Hi! Challenge over! How did it go?Did you know that jumping rope allows you to burn a lot of calories and train all the muscles in the body? With this activity you burn twice the calories that you burn with running: 15 min of jumping rope corresponds to 30 min of running! Isn’t it convenient? Rope is an excellent ally for training and staying in shape in these last months of school when time for sports or walks is always short. Now let’s catch our breath and on Monday we start with the next challenge! |
| week 3 Breakfast | Third challenge: Chef breakfast! This is a cooking challenge, by Sunday you will have to prepare a delicious but also very healthy breakfast, then you will send me photos, ingredients and recipe! | The challenge is finished and you have been great with your healthy and tasty breakfast! As you well know it is important to eat healthily but we must not give up on taste!!! Here is another idea for a super tasty breakfast, Yogurt and strawberry smoothie: 125 g of 0% fat white Greek yogurt with no added sugar; 100 gr of strawberries; ½ orange; ½ teaspoon of cinnamon powder. The recipe is very simple, just blend all the ingredients to have a fantastic breakfast! |
| week 4 Fruits and vegetables | Challenge of the Week: Vegetables!Now the costume test is upon us and we certainly cannot be caught unprepared! What’s better than eating lots of fruit and vegetables? You will have to eat at least 5 portions of fruits and vegetables a day until the weekend... let me know how many days you did it. I already know that you will be very good this time too! | Hi!!! So, this challenge? As you already know it is important to eat five servings of fruit and vegetables every day; in this way you introduce the right amount of vitamins and minerals. It is also essential to often vary the fruit and vegetables eaten, always preferring those that are part of the green list with a lower sugar content. |
| week 5 Screen-time | Challenge of the week: LET’S REDUCE THE SCREEN-TIME! This challenge will be a little more difficult for you than usual. You will have to minimize the screen-time (TV, tablet, PC, mobile phone) for a whole week! I give you a maximum of 2 h a day, but every day try to tell me how long you’ve been doing screen-time! | Challenge finished! How did it go? Were you able to reduce the screen-time? A very recent study has highlighted how a sedentary lifestyle (and therefore screen-time) is one of the factors most related to weight gain, even more than an incorrect diet! Try to keep making more limited use of it! |
| week 6 Sleep | Challenge of the week: sleep is good for you! The new challenge is about regular sleep: you will have to try to go to sleep and always wake up at the same time, sleeping about 9 h a night. So if for example you wake up at 7/7.30 you will have to go to sleep at the latest at 22/22.30. It would be ideal to mark the time you go to sleep and the time you wake up for this week so that at the weekend we can make a good final balance together. | Do you know that at any age it is necessary to sleep a certain number of hours? In your case, 8 to 10 h of sleep are needed per night. Sleeping is necessary and you don’t have to stay up late and wake up too early to go to school! An insufficient amount of sleep can promote, along with other factors, the onset of diseases such as hypertension, diabetes, obesity. So I recommend engaging in this seemingly trivial challenge and try to keep this habit! |
| Settimana | Sfida | Informazione E Formazione |
|---|---|---|
| Settimana 1 Bevande zuccherate | Prima sfida: Addio zucchero!!! Niente succhi di frutta, coca-cola, thè confezionati. Per una settimana intera. Coinvolgi tutta la famiglia e fammi sapere ogni giorno o tra una settimana per quanti giorni hai superato la sfida! | Prima della prossima sfida volevo ricordarti perché le bevande zuccherate vanno evitate; fanno aumentare velocemente i livelli di zucchero nel sangue e questo induce in pancreas a produrre un’enorme quantità di insulina, l’ormone che porta lo zucchero nelle cellule. A lungo andare si induce una disfunzione del pancreas che prima porta l’organismo ad essere insulino-resistente e successivamente al diabete!! La sfida è finita ma continuare ad evitare queste bevande può farti solo bene! |
| Settimana 2 Attività fisica | Seconda sfida: salto alla corda! Le sfide si complicano ma so che tu ci riuscirai lo stesso! Hai mai provato a saltare la corda? Provaci ogni giorno e fammi sapere come te la cavi. Dovrai allenarti tutti i giorni in questa settimana, anche solo per 15 minuti. Provaci mi raccomando, fammi sapere poi quanti salti fai al minuto! In bocca al lupo. | Ciao! Sfida finita! Com’è andata?Lo sapevi che il salto alla corda permette di bruciare molte calorie e di allenare tutti i muscoli del corpo? Con la corda si brucia il doppio delle calorie che si bruciano con la corsa: 15 minuti di salto alla corda corrispondono a 30 minuti di corsa!! Conviene no? La corda è un’ottima alleata per allenarsi e restare in forma in questi ultimi mesi di scuola in cui il tempo per fare sport o passeggiate è sempre poco. Adesso riprendiamo fiato e lunedì si parte con la prossima sfida! |
| Settimana 3 Colazione | Terza sfida: Colazione chef! Questa è una sfida di cucina, entro domenica dovrai preparare una colazione buonissima ma anche tanto sana. poi mi invierai foto, ingredienti e ricetta! | La sfida è finita e tu sei stata bravissima con la tua colazione sana e gustosa! Come ben sai è importante mangiare in modo sano ma non per questo dobbiamo rinunciare al gusto!!! Ecco a te un’altra idea per una colazione super gustosa, Frullato di yogurt e fragole: −125 gr di yogurt greco bianco 0%grassi senza zuccheri aggiunti; −100 gr di fragole; −½ arancia; −½ cucchiaino di cannella in polvere. La ricetta è semplicissima, basta frullare tutti gli ingredienti per avere una colazione fantastica! |
| Settimana 4 Frutta e verdura | Sfida della settimana: Verdure!Ormai la prova costume è alle porte e di certo non possiamo farci trovare impreparati! Cosa c’è di meglio di mangiare tanta frutta e verdura? Dovrai mangiare almeno 5 porzioni tra frutta e verdura al giorno fino a fine settimana. fammi sapere per quanti giorni ci sei riuscita. Già so che sarai bravissima anche questa volta! | Ciao!!! Allora questa sfida? Come già sai è importante mangiare cinque porzioni di frutta e verdura ogni giorno, in questo modo si introduce la giusta quota di vitamine e minerali. È fondamentale, inoltre, variare spesso la frutta e la verdura mangiata, preferendo sempre quella che fa parte della lista verde con un minor contenuto di zuccheri. |
| Settimana 5 Screen-time | Sfida della settimana: RIDUCIAMO LO SCREE-TIME! Questa sfida sarà per te un po’ più difficile del solito. dovrai ridurre al minimo lo screen-time (tv, tablet, pc, cellulare) per una settimana intera! Ti concedo al massimo 2 ore al giorno, però ogni giorno prova a dirmi per quanto tempo hai fatto screen-time! | Sfida terminata! Com’è andata? Sei riuscita a ridurre lo screen-time? Uno studio recentissimo ha messo in evidenza come la sedentarietà (e quindi lo screen-time) sia uno dei fattori maggiormente correlati all’aumento di peso, anche più di un’alimentazione scorretta! Prova a continuare a farne un utilizzo più limitato! |
| Settimana 6 Sonno | Sfida della settimana: dormire fa bene! La nuova sfida riguarda il sonno regolare: dovrai cercare di andare a dormire e svegliarti sempre alla stessa ora, dormendo circa 9 ore per notte. Quindi se ad esempio di svegli alle 7/7.30 dovrai andare a dormire al massimo alle 22/22.30. Sarebbe l’ideale segnare per questa settimana l’orario in cui vai a dormire e l’orario in cui ti svegli così che a fine settimana possiamo fare insieme un bel bilancio finale. | Sai che ad ogni età è necessario dormire un determinato numero di ore? Nel tuo caso sono necessarie dalle 8 alle 10 ore di sonno per notte. Dormire è necessario e non bisogna fare le ore piccole e svegliarsi troppo presto la mattina per andare a scuola! Una quantità insufficiente di sonno può favorire, insieme ad altri fattori, la comparsa di malattie quali l’ipertensione, il diabete, l’obesità. Quindi mi raccomando impegnati in questa sfida apparentemente banale e cerca di mantenere quest’abitudine! |
References
- Vasileva, L.; Marchev, A.S.; Georgiev, M.I. Causes and solutions to “globesity”: The new fa(s)t alarming global epidemic. Food Chem. Toxicol. 2018, 121, 173–193. [Google Scholar] [CrossRef]
- Nobles, J.; Griffiths, C.; Pringle, A.; Gately, P.; Pringle, A. Design programmes to maximise participant engagement: A predictive study of programme and participant characteristics associated with engagement in paediatric weight management. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 76. [Google Scholar] [CrossRef] [Green Version]
- Park, J.; Woo, S.; Ju, Y.-S.; Seo, Y.-G.; Lim, H.; Kim, Y.; Noh, H.-M.; Lee, H.-J.; Park, S.I.; Park, K.H. Factors associated with dropout in a lifestyle modification program for weight management in children and adolescents. Obes. Res. Clin. Pract. 2020, 14, 566–572. [Google Scholar] [CrossRef] [PubMed]
- Ball, G.D.C.; Sebastianski, M.; Wijesundera, J.; Keto-Lambert, D.; Ho, J.; Zenlea, I.; Perez, A.; Nobles, J.; Skelton, J.A. Strategies to reduce attrition in managing paediatric obesity: A systematic review. Pediatr. Obes. 2020, 22, 12733. [Google Scholar] [CrossRef]
- Svetkey, L.P.; Stevens, V.J.; Brantley, P.J.; Appel, L.J.; Hollis, J.F.; Loria, C.M.; Vollmer, W.M.; Gullion, C.M.; Funk, K.; Smith, P.; et al. Comparison of Strategies for Sustaining Weight LossThe Weight Loss Maintenance Randomized Controlled Trial. JAMA 2008, 299, 1139–1148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verdaguer, S.; Mateo, K.F.; Wyka, K.; Dennis-Tiwary, T.A.; Leung, M.M.; Riiser, K.; Taki, S.; Bruton, Y.P.; Wright, J. A Web-Based Interactive Tool to Reduce Childhood Obesity Risk in Urban Minority Youth: Usability Testing Study. JMIR Form. Res. 2018, 2, e21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leung, M.M.; Mateo, K.F.; Verdaguer, S.; Wyka, K. Testing a Web-Based Interactive Comic Tool to Decrease Obesity Risk Among Minority Preadolescents: Protocol for a Pilot Randomized Control Trial. JMIR Res. Protoc. 2018, 7, e10682. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Staiano, A.E.; Marker, A.M.; Beyl, R.A.; Hsia, D.S.; Katzmarzyk, P.T.; Newton, R.L. A randomized controlled trial of dance exergaming for exercise training in overweight and obese adolescent girls. Pediatr. Obes. 2017, 12, 120–128. [Google Scholar] [CrossRef] [Green Version]
- Dias, J.D.; Domingues, A.N.; Tibes, C.M.; Zem-Mascarenhas, S.H.; Fonseca, L.M.M. Serious games as an educational strategy to control childhood obesity: A systematic literature review 1. Rev. Latino-Am. Enferm. 2018, 26, 26. [Google Scholar] [CrossRef]
- Charlier, N.; Zupancic, N.; Fieuws, S.; Denhaerynck, K.; Zaman, B.; Moons, P. Serious games for improving knowledge and self-management in young people with chronic conditions: A systematic review and meta-analysis. J. Am. Med Inform. Assoc. 2016, 23, 230–239. [Google Scholar] [CrossRef] [Green Version]
- Kalantari, N.; Mohammadi, N.K.; Rafieifar, S.; Eini-Zinab, H.; Aminifard, A.; Malmir, H.; Ashoori, N.; Abdi, S.; Gholamalizadeh, M.; Doaei, S. Indicator for Success of Obesity Reduction Programs in Adolescents: Body Composition or Body Mass Index? Evaluating a School-based Health Promotion Project after 12 Weeks of Intervention. Int. J. Prev. Med. 2017, 8, 8. [Google Scholar]
- Rahelić, V.; Głąbska, D.; Guzek, D.; Pavić, E.; Rumora, S.I.; Bogdanić, A.; Špehar, U.A.; Rojnić, P.N.; Krnić, N. Role of Parents in Body Mass Reduction in Children with Obesity—Adherence and Success of 1-Year Participation in an Intervention Program. Medicina 2020, 56, 168. [Google Scholar] [CrossRef] [Green Version]
- Wong, W.W.; Barlow, S.E.; Mikhail, C.; Wilson, T.A.; Hernandez, P.M.; Shypailo, R.J.; Abrams, S.H. A Residential Summer Camp Can Reduce Body Fat and Improve Health-related Quality of Life in Obese Children. J. Pediatr. Gastroenterol. Nutr. 2013, 56, 83–85. [Google Scholar] [CrossRef]
- Bergmann, K.; Mestre, Z.; Strong, D.; Eichen, D.M.; Rhee, K.; Crow, S.; Wilfley, D.; Boutelle, K.N. Comparison of Two Models of Family-Based Treatment for Childhood Obesity: A Pilot Study. Child. Obes. 2019, 15, 116–122. [Google Scholar] [CrossRef]
- Song, M.; Lee, C.S.; Lyons, K.S.; Stoyles, S.; Winters-Stone, K.M. Assessing the feasibility of parent participation in a commercial weight loss program to improve child body mass index and weight-related health behaviors. SAGE Open Med. 2018, 6, 2050312118801220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.; Piao, M.; Byun, A.; Kim, J. A Systematic Review and Meta-Analysis of Intervention for Pediatric Obesity Using Mobile Technology. Stud. Heal. Technol. Inform. 2016, 225, 491–494. [Google Scholar]
- Nyström, C.D.; Sandin, S.; Henriksson, P.; Trolle-Lagerros, Y.; Larsson, C.; Maddison, R.; Ortega, F.B.; Pomeroy, J.; Ruiz, J.R.; Silfvernagel, K.; et al. Mobile-based intervention intended to stop obesity in preschool-aged children: The MINISTOP randomized controlled trial. Am. J. Clin. Nutr. 2017, 105, 1327–1335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ek, A.; Nyström, C.D.; Chirita-Emandi, A.; Tur, J.A.; Nordin, K.; Bouzas, C.; Argelich, E.; Martinez, J.A.; Frost, G.; Garcia-Perez, I.; et al. A randomized controlled trial for overweight and obesity in preschoolers: The More and Less Europe study—An intervention within the STOP project. BMC Public Health 2019, 19, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gabrielli, S.; Dianti, M.; Maimone, R.; Betta, M.; Filippi, L.; Ghezzi, M.; Forti, S. Design of a Mobile App for Nutrition Education (TreC-LifeStyle) and Formative Evaluation with Families of Overweight Children. JMIR mHealth uHealth 2017, 5, e48. [Google Scholar] [CrossRef]
- Chen, J.L.; Guedes, C.M.; Cooper, B.A.; Lung, A.E. Short-Term Efficacy of an Innovative Mobile Phone Technology-Based Intervention for Weight Management for Overweight and Obese Adolescents: Pilot Study. Interact. J. Med. Res. 2017, 6, e12. [Google Scholar] [CrossRef] [PubMed]
- Chaplais, E.; Naughton, G.A.; Thivel, D.; Courteix, D.; Greene, A.D. Smartphone Interventions for Weight Treatment and Behavioral Change in Pediatric Obesity: A Systematic Review. Telemed. e-Health 2015, 21, 822–830. [Google Scholar] [CrossRef]
- Vidmar, A.P.; Salvy, S.J.; Pretlow, R.; Mittelman, S.D.; Wee, C.P.; Fink, C.; Fox, D.S.; Raymond, J.K. An addiction-based mobile health weight loss intervention: Protocol of a randomized controlled trial. Contemp. Clin. Trials 2019, 78, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Turner, T.; Spruijt-Metz, D.; Wen, C.K.F.; Hingle, M.D. Prevention and treatment of pediatric obesity using mobile and wireless technologies: A systematic review. Pediatr. Obes. 2015, 10, 403–409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Darling, K.E.; Sato, A.F. Systematic Review and Meta-Analysis Examining the Effectiveness of Mobile Health Technologies in Using Self-Monitoring for Pediatric Weight Management. Child. Obes. 2017, 13, 347–355. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention, National Center for Health Statistics. Clinical Growth Charts. Percentile Data Files with LMS Values. Available online: https://www.cdc.gov/growthcharts/clinical_charts.htm (accessed on 10 January 2021).
- Rickham, P.P. Human experimentation. Code of ethics of the world medical association. Declaration of Helsinki. BMJ 1964, 2, 177. [Google Scholar] [PubMed] [Green Version]
- Sorg, M.J.; Yehle, K.S.; Coddington, J.A.; Ahmed, A.H. Implementing family-based childhood obesity interventions. Nurse Pract. 2013, 38, 14–21. [Google Scholar] [CrossRef]

| Intervention Group Mean (SD) | Control Group Mean (SD) | |
|---|---|---|
| Variable a | First Visit n = 54 (24 M; age 9.7 years) | First Visit n = 49 (25 M; 10.4 years) |
| BMI (kg/m2) | 29.2 (4.6) | 30.4 (6.1) |
| BMI-zs | 2.97 (0.5) | 2.0 (0.8) |
| WC (cm) | 85.1(10.2) | 86.3 (19.3) |
| NC (cm) | 33.1 (2.9) | 33.5 (4.8) |
| SBP (mmHg) | 115.2(13.2) | 112.2 (15.2) |
| DBP (mmHg) | 66.9 (12.2) | 65.7 (12.0) |
| AN (grade) | 1.5 (0.9) | 1.33 (1.0) |
| F&V (portions/day) | 1.2 (1.1) | 1.5 (1.09) |
| SuD (mL/week) | 894.3(514.0) | 1441.6(1424.0) |
| Screen T (min/day) | 199.4(110.0) | 245 (126.9) |
| PA (min/week) | 69.3(125.7) | 80 (100.8) |
| Sleep (h/night) | 8.2 (1.22) | 7.8 (1.2) |
| Time | Compliant Patients N (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| IG 1.1 | CG 1.1 | p Value | IG 1.2 | CG 1.2 | p Value | IG 1.1 + 1.2 | CG 1.1 + 1.2 | p Value | |
| First visit (N) | 24 | 25 | 30 | 24 | 54 | 49 | |||
| Regular visit at 3 Months | 12 (50%) | 6 (24%) | 0.079 | 28 (93%) | 7 (29%) | <0.0001 | 40 (74%) | 13 (26%) | <0.0001 |
| Regular visit at 6 Months | 9 (38%) | 2 (8%) | 0.018 | 27 (90%) | 3 (12%) | <0.0001 | 36 (66%) | 5 (10%) | <0.0001 |
| At least one check | 14 (58%) | 6 (24%) | 0.021 | 28 (93%) | 8 (33%) | 0.00025 | 41 (75%) | 16 (32%) | 0.00001 |
| Variable | 3 Months, Mean (SD) | 6 Months, Mean (SD) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group | IG 1.1 | CG 1.1 | p Value | IG 1.2 | CG 1.2 | p Value | IG 1.1 | CG 1.1 | p Value | IG 1.2 | CG 1.2 | p Value |
| n | 24 | 25 | 30 | 24 | 24 | 25 | 30 | 24 | ||||
| BMI Kg/m2 | −2.36 (1.29) | −0.94 (1.10) | 0.026 | −2.2 (0.9) | −1.18 (1.6) | 0.04 | −2.99 (2.96) | 1 (0.42) | 0.12 | −4.6 (1.8) | +2.7 (2.8) | 0.003 |
| BMI zs | −0.28 (0.15) | −0.10 (0.11) | 0.018 | −1.29 (1.3) | −0.1 (0.2) | 0.04 | −0.33 (0.32) | 0.06 (0.16) | 0.14 | −1.8 (0.7) | −0.2 (0.3) | 0.2 |
| Ex WC% | −36.11 (38.12) | 3.20 (19.99) | 0.02 | −30.9 (23.83) | −20.83 (15.94) | 0.33 | −28.89 (43.65) | 0 (0) | 0.39 | −34.19 (27.07) | −5.00 (7.07) | 0.15 |
| Ex NC% | −59.58 (42.20) | 1.42 (25.80) | 0.004 | −38.41 (40.23) | −20.83 (18.00) | 0.30 | −54.03 (67.19) | 21.25 (58.33) | 0.199 | −57.18 (44.52) | −12.50 (17.67) | 0.18 |
| SBP mmHg | −9.58 (9.87) | −5.00 (17.32) | 0.453 | −14.03 (8.5) | −3.5 (13.7) | 0.02 | −6.25 (14.33) | −5.00 (7.07) | 0.911 | −24.64 (25.79) | −3.5 (2.12) | 0.27 |
| DBP mmHg | −3.63 (7.10) | −1.25 (13.15) | 0.92 | −11.59 (15.36) | +5.2 (6.4) | 0.02 | −1.88 (10.67) | 7.50 (10.61) | 0.29 | −2.37 (17.26) | −5.00 (0.0) | 0.79 |
| AN grade | −0.41 (0.51) | 0.00 (0.63) | 0.13 | −0.8 (0.5) | +0.3 (0.5) | 0.00 | −0.75 (0.89) | 0.00 (1.41) | 0.36 | −1.0 (0.6) | +1.0 (0.0) | 0.0003 |
| Variable | 3 Months, Mean SD | 6 Months, Mean SD | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IG 1.1 (n = 12) | CG1.1 (n = 6) | p Value | IG1.2 (n = 12) | CG1.2 (n = 6) | p Value | IG1.1 (n = 9) | CG1.1 (n = 2) | p Value | IG 1.2 (n = 9) | CG1.2 (n = 2) | p Value | |
| SuD (mL/week) | −673.5 (487.5) | −57 (419.75) | 0.002 | −587.0 (367.8) | −35.7 (18.9) | 0.02 | −860.0 (586) | 0.0 (424.3) | 0.17 | −718.0 (504.2) | −683. 3 (500.2) | 0.67 |
| ScreenT (min/die) | −45.0 (101.05) | 6.67 (30.76) | 0.38 | −83.8 (93.0) | −8.5 (80.7) | 0.02 | −81.4 (95.9) | 15 (63.6) | 0.39 | −118.7 (100.2) | 20.0 (124.9) | 0.04 |
| Sleep (h/night) | 0.3 (0.5) | 0.0 (0.0) | 0.22 | 0.6 (0.9) | 0.85 (1.1) | 0.55 | −0.58 (1.65) | 0.0 (0.0) | 0.65 | 1.18 (1.5) | 1.33 (1.52) | 0.8 |
| F&V (portion/die) | 1.25 (1.09) | 0.2 (0.4) | 0.040 | 1.18 (1.6) | 0.00 (0.5) | 0.04 | 2.03 (1.2) | 0.33 (0.57) | 0.19 | 2.57 (1.1) | 0.66 (1.15) | 0.02 |
| PA (min/week) | 0.76 (12.55) | 20 (36.17) | 0.09 | 71.85 (118.0) | −30 (111.0) | 0.03 | 11.2 (63.59) | 15.0 (21.2) | 0.59 | 112.2 (113.1) | 133.3 (23.09) | 0.7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delli Bovi, A.P.; Manco Cesari, G.; Rocco, M.C.; Di Michele, L.; Rimauro, I.; Lugiero, A.; Mottola, S.; De Anseris, A.G.E.; Nazzaro, L.; Massa, G.; et al. Healthy Lifestyle Management of Pediatric Obesity with a Hybrid System of Customized Mobile Technology: The PediaFit Pilot Project. Nutrients 2021, 13, 631. https://0-doi-org.brum.beds.ac.uk/10.3390/nu13020631
Delli Bovi AP, Manco Cesari G, Rocco MC, Di Michele L, Rimauro I, Lugiero A, Mottola S, De Anseris AGE, Nazzaro L, Massa G, et al. Healthy Lifestyle Management of Pediatric Obesity with a Hybrid System of Customized Mobile Technology: The PediaFit Pilot Project. Nutrients. 2021; 13(2):631. https://0-doi-org.brum.beds.ac.uk/10.3390/nu13020631
Chicago/Turabian StyleDelli Bovi, Anna Pia, Giorgia Manco Cesari, Maria Chiara Rocco, Laura Di Michele, Ida Rimauro, Anna Lugiero, Silvia Mottola, Anna Giulia Elena De Anseris, Lucia Nazzaro, Grazia Massa, and et al. 2021. "Healthy Lifestyle Management of Pediatric Obesity with a Hybrid System of Customized Mobile Technology: The PediaFit Pilot Project" Nutrients 13, no. 2: 631. https://0-doi-org.brum.beds.ac.uk/10.3390/nu13020631