The Expanding Therapeutic Utility of Botulinum Neurotoxins
Abstract
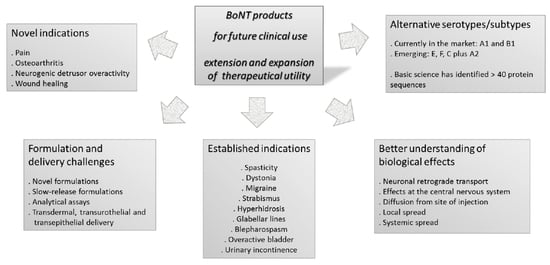
:1. Current Therapeutic Landscape
2. Alternative Serotypes, Broadening the Therapeutic Landscape
3. Novel Indications
3.1. Pain and Migraine
3.2. Osteoarthritis
3.3. Overactive Bladder and Neurogenic Detrusor Overactivity
3.4. Wound Healing
4. BoNT Effects Remote from the Site of Injection
4.1. Neuronal Retrograde Transport and Central Effects
4.2. Diffusion within the Injected Muscle, Local Spread and Contributing Factors
4.3. Systemic Spread and Contributing Factors
4.4. New BoNT Therapeutics with Decreased Spread
5. Novel Formulations
5.1. Current Products and Challenges Associated with Formulation of BoNTs
5.2. Slow-Release Formulations
5.3. Analytical Challenges
6. Novel Delivery Methods
6.1. Transdermal Delivery
6.2. Transurothelial Delivery
6.3. Transepithelial Delivery
7. Conclusions
Author Contributions
Conflicts of Interest
References
- Zhang, S.; Masuyer, G.; Zhang, J.; Shen, Y.; Lundin, D.; Henriksson, L.; Miyashita, S.-I.; Martínez-Carranza, M.; Dong, M.; Stenmark, P. Identification and characterization of a novel botulinum neurotoxin. Nat. Commun. 2017, 8, 14130. [Google Scholar] [CrossRef] [PubMed]
- Hill, K.K.; Smith, T.J. Genetic diversity within Clostridium botulinum serotypes, botulinum neurotoxin gene clusters and toxin subtypes. In Botulinum Neurotoxins; Springer: Berlin, Germany, 2012; pp. 1–20. [Google Scholar]
- Peng, L.; Berntsson, R.P.-A.; Tepp, W.H.; Pitkin, R.M.; Johnson, E.A.; Stenmark, P.; Dong, M. Botulinum neurotoxin DC uses synaptotagmin I and II as receptors, and human synaptotagmin II is not an effective receptor for type B, DC and G toxins. J. Cell Sci. 2012, 125, 3233–3242. [Google Scholar] [CrossRef] [PubMed]
- Strotmeier, J.; Willjes, G.; Binz, T.; Rummel, A. Human synaptotagmin-II is not a high affinity receptor for botulinum neurotoxin B and G: Increased therapeutic dosage and immunogenicity. FEBS Lett. 2012, 586, 310–313. [Google Scholar] [CrossRef] [PubMed]
- Dressler, D.; Bigalke, H.; Benecke, R. Botulinum toxin type B in antibody-induced botulinum toxin type A therapy failure. J. Neurol. 2003, 250, 967–969. [Google Scholar] [CrossRef] [PubMed]
- Tao, L.; Peng, L.; Berntsson, R.P.-A.; Liu, S.M.; Park, S.; Yu, F.; Boone, C.; Palan, S.; Beard, M.; Chabrier, P.-E. Engineered botulinum neurotoxin B with improved efficacy for targeting human receptors. Nat. Commun. 2017, 8, 53. [Google Scholar] [CrossRef] [PubMed]
- Brin, M.F.; James, C.; Maltman, J. Botulinum toxin type A products are not interchangeable: A review of the evidence. Biol. Targets Ther. 2014, 8, 227. [Google Scholar] [CrossRef] [PubMed]
- Frevert, J. Content of botulinum neurotoxin in botox®/vistabel®, dysport®/azzalure®, and xeomin®/bocouture®. Drugs R D 2010, 10, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Pickett, A. Botulinum toxin as a clinical product: Manufacture and pharmacology. In Clinical Applications of Botulinum Neurotoxin; Foster, K., Ed.; Springer: Berlin, Germany, 2014; pp. 7–49. [Google Scholar]
- Ludlow, C.; Hallett, M.; Rhew, K.; Cole, R.; Shimizu, T.; Bagley, J.; Schulz, G.; Yin, S.; Koda, J. Therapeutic use of type F botulinum toxin. N. Engl. J. Med. 1992, 326, 349–350. [Google Scholar] [PubMed]
- Greene, P.E.; Fahn, S. Use of botulinum toxin type F injections to treat torticollis in patients with immunity to botulinum toxin type A. Mov. Disord. 1993, 8, 479–483. [Google Scholar] [CrossRef] [PubMed]
- Greene, P.E.; Fahn, S. Response to botulinum toxin F in seronegative botulinum toxin A—Resistant patients. Mov. Disord. 1996, 11, 181–184. [Google Scholar] [CrossRef] [PubMed]
- Mezaki, T.; Kaji, R.; Kohara, N.; Fujii, H.; Katayama, M.; Shimizu, T.; Kimura, J.; Brin, M. Comparison of Therapeutic Efficacies of Type A and F Botulinum Toxins for Blepharospasm A double-blind, controlled study. Neurology 1995, 45, 506–508. [Google Scholar] [CrossRef] [PubMed]
- Houser, M.; Sheean, G.; Lees, A. Further studies using higher doses of botulinum toxin type F for torticollis resistant to botulinum toxin type A. J. Neurol. Neurosurg. Psychiatry 1998, 64, 577–580. [Google Scholar] [CrossRef] [PubMed]
- Sheean, G.; Lees, A. Botulinum toxin F in the treatment of torticollis clinically resistant to botulinum toxin A. J. Neurol. Neurosurg. Psychiatry 1995, 59, 601–607. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Karp, B.I.; Hallett, M. Botulinum toxin type F for treatment of dystonia Long-term experience. Neurology 1998, 51, 1494–1496. [Google Scholar] [CrossRef] [PubMed]
- Billante, C.R.; Zealear, D.L.; Billante, M.; Reyes, J.H.; Sant’Anna, G.; Rodriguez, R.; Stone, R. Comparison of neuromuscular blockade and recovery with botulinum toxins A and F. Muscle Nerve 2002, 26, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Eleopra, R.; Tugnoli, V.; Rossetto, O.; De Grandis, D.; Montecucco, C. Different time courses of recovery after poisoning with botulinum neurotoxin serotypes A and E in humans. Neurosci. Lett. 1998, 256, 135–138. [Google Scholar] [CrossRef]
- Adler, M.; Keller, J.E.; Sheridan, R.E.; Deshpande, S.S. Persistence of botulinum neurotoxin A demonstrated by sequential administration of serotypes A and E in rat EDL muscle. Toxicon 2001, 39, 233–243. [Google Scholar] [CrossRef]
- Whitemarsh, R.C.M.; Tepp, W.H.; Johnson, E.A.; Pellett, S. Persistence of botulinum neurotoxin a subtypes 1–5 in primary rat spinal cord cells. PLoS ONE 2014, 9, e90252. [Google Scholar] [CrossRef] [PubMed]
- Antonucci, F.; Rossi, C.; Gianfranceschi, L.; Rossetto, O.; Caleo, M. Long-distance retrograde effects of botulinum neurotoxin A. J. Neurosci. 2008, 28, 3689–3696. [Google Scholar] [CrossRef] [PubMed]
- Scheps, D.; de la Paz, M.L.; Jurk, M.; Hofmann, F.; Frevert, J. Design of modified botulinum neurotoxin A1 variants with a shorter persistence of paralysis and duration of action. Toxicon 2017, 139, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Costantin, L.; Bozzi, Y.; Richichi, C.; Viegi, A.; Antonucci, F.; Funicello, M.; Gobbi, M.; Mennini, T.; Rossetto, O.; Montecucco, C. Antiepileptic effects of botulinum neurotoxin E. J. Neurosci. 2005, 25, 1943–1951. [Google Scholar] [CrossRef] [PubMed]
- Eleopra, R.; Tugnoli, V.; Rossetto, O.; Montecucco, C.; De Grandis, D. Botulinum neurotoxin serotype C: A novel effective botulinum toxin therapy in human. Neurosci. Lett. 1997, 224, 91–94. [Google Scholar] [CrossRef]
- Eleopra, R.; Tugnoli, V.; Quatrale, R.; Gastaldo, E.; Rossetto, O.; De Grandis, D.; Montecucco, C. Botulinum neurotoxin serotypes A and C do not affect motor units survival in humans: An electrophysiological study by motor units counting. Clin. Neurophysiol. 2002, 113, 1258–1264. [Google Scholar] [CrossRef]
- Eleopra, R.; Tugnoli, V.; De Grandis, D.; Montecucco, C. Botulinum toxin serotype C treatment in subjects affected by focal dystonia and resistant to botulinum toxin serotype A. Neurology 1998, 50, A72. [Google Scholar]
- Eleopra, R.; Tugnoli, V.; Quatrale, R.; Rossetto, O.; Montecucco, C.; Dressler, D. Clinical use of non-A botulinum toxins: Botulinum toxin type C and botulinum toxin type F. Neurotox. Res. 2006, 9, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Pellett, S.; Tepp, W.H.; Whitemarsh, R.C.; Bradshaw, M.; Johnson, E.A. In vivo onset and duration of action varies for botulinum neurotoxin A subtypes 1–5. Toxicon 2015, 107, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Whitemarsh, R.C.; Tepp, W.H.; Bradshaw, M.; Lin, G.; Pier, C.L.; Scherf, J.M.; Johnson, E.A.; Pellett, S. Characterization of botulinum neurotoxin A subtypes 1 through 5 by investigation of activities in mice, in neuronal cell cultures, and in vitro. Infect. Immun. 2013, 81, 3894–3902. [Google Scholar] [CrossRef] [PubMed]
- Pier, C.L.; Chen, C.; Tepp, W.H.; Lin, G.; Janda, K.D.; Barbieri, J.T.; Pellett, S.; Johnson, E.A. Botulinum neurotoxin subtype A2 enters neuronal cells faster than subtype A1. FEBS Lett. 2011, 585, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Akaike, N.; Shin, M.C.; Wakita, M.; Torii, Y.; Harakawa, T.; Ginnaga, A.; Kato, K.; Kaji, R.; Kozaki, S. Transsynaptic inhibition of spinal transmission by A2 botulinum toxin. J. Physiol. 2013, 591, 1031–1043. [Google Scholar] [CrossRef] [PubMed]
- Torii, Y.; Kiyota, N.; Sugimoto, N.; Mori, Y.; Goto, Y.; Harakawa, T.; Nakahira, S.; Kaji, R.; Kozaki, S.; Ginnaga, A. Comparison of effects of botulinum toxin subtype A1 and A2 using twitch tension assay and rat grip strength test. Toxicon 2011, 57, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Kroken, A.R.; Blum, F.C.; Zuverink, M.; Barbieri, J.T. Entry of Botulinum neurotoxin subtypes A1 and A2 into neurons. Infect. Immun. 2017, 85, e00795-16. [Google Scholar] [CrossRef] [PubMed]
- Benoit, R.M.; Schärer, M.A.; Wieser, M.M.; Li, X.; Frey, D.; Kammerer, R.A. Crystal structure of the BoNT/A2 receptor-binding domain in complex with the luminal domain of its neuronal receptor SV2C. Sci. Rep. 2017, 7, 43588. [Google Scholar] [CrossRef] [PubMed]
- Tepp, W.H.; Lin, G.; Johnson, E.A. Purification and characterization of a novel subtype A3 botulinum neurotoxin. Appl. Environ. Microbiol. 2012, 78, 3108–3113. [Google Scholar] [CrossRef] [PubMed]
- Torii, Y.; Goto, Y.; Nakahira, S.; Kozaki, S.; Ginnaga, A. Comparison of the immunogenicity of botulinum toxin type A and the efficacy of A1 and A2 neurotoxins in animals with A1 toxin antibodies. Toxicon 2014, 77, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Mukai, Y.; Shimatani, Y.; Sako, W.; Asanuma, K.; Nodera, H.; Sakamoto, T.; Izumi, Y.; Kohda, T.; Kozaki, S.; Kaji, R. Comparison between botulinum neurotoxin type A2 and type A1 by electrophysiological study in healthy individuals. Toxicon 2014, 81, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Kaji, R. Clinical differences between A1 and A2 botulinum toxin subtypes. Toxicon 2015, 107, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Itakura, M.; Kohda, T.; Kubo, T.; Semi, Y.; Azuma, Y.-T.; Nakajima, H.; Kozaki, S.; Takeuchi, T. Botulinum neurotoxin A subtype 2 reduces pathological behaviors more effectively than subtype 1 in a rat Parkinson’s disease model. Biochem. Biophys. Res. Commun. 2014, 447, 311–314. [Google Scholar] [CrossRef] [PubMed]
- Shin, M.-C.; Yukihira, T.; Ito, Y.; Akaike, N. Antinociceptive effects of A1 and A2 type botulinum toxins on carrageenan-induced hyperalgesia in rat. Toxicon 2013, 64, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Nagai, J.; Sekino, Y.; Goto, Y.; Nakahira, S.; Ueda, H. Single Application of A2 NTX, a Botulinum Toxin A2 Subunit, Prevents Chronic Pain Over Long Periods in Both Diabetic and Spinal Cord Injury–Induced Neuropathic Pain Models. J. Pharmacol. Sci. 2012, 119, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Debono, D.J.; Hoeksema, L.J.; Hobbs, R.D. Caring for patients with chronic pain: Pearls and pitfalls. J. Am. Osteopath. Assoc. 2013, 113, 620–627. [Google Scholar] [CrossRef] [PubMed]
- Van Hecke, O.; Torrance, N.; Smith, B.H. Chronic pain epidemiology—Where do lifestyle factors fit in? Br. J. Pain 2013, 7, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Reid, K.J.; Harker, J.; Bala, M.M.; Truyers, C.; Kellen, E.; Bekkering, G.E.; Kleijnen, J. Epidemiology of chronic non-cancer pain in Europe: Narrative review of prevalence, pain treatments and pain impact. Curr. Med. Res. Opin. 2011, 27, 449–462. [Google Scholar] [CrossRef] [PubMed]
- Woolf, C.J. Overcoming obstacles to developing new analgesics. Nat. Med. 2010, 16, 1241–1247. [Google Scholar] [CrossRef] [PubMed]
- Kissin, I. The development of new analgesics over the past 50 years: A lack of real breakthrough drugs. Anesth. Analg. 2010, 110, 780–789. [Google Scholar] [CrossRef] [PubMed]
- Tarsy, D.; First, E.R. Painful cervical dystonia: Clinical features and response to treatment with botulinum toxin. Mov. Disord. 1999, 14, 1043–1045. [Google Scholar] [CrossRef]
- Freund, B.; Schwartz, M. Temporal relationship of muscle weakness and pain reduction in subjects treated with botulinum toxin A. J. Pain 2003, 4, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Bomba-Warczak, E.; Vevea, J.D.; Brittain, J.M.; Figueroa-Bernier, A.; Tepp, W.H.; Johnson, E.A.; Yeh, F.L.; Chapman, E.R. Interneuronal Transfer and Distal Action of Tetanus Toxin and Botulinum Neurotoxins A and D in Central Neurons. Cell Rep. 2016, 16, 1974–1987. [Google Scholar] [CrossRef] [PubMed]
- Cocco, A.; Albanese, A. Recent developments in clinical trials of bont. Toxicon 2017, 123, S89. [Google Scholar]
- Caleo, M.; Restani, L. Direct central nervous system effects of botulinum neurotoxin. Toxicon 2017, 147, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Marinelli, S.; Vacca, V.; Ricordy, R.; Uggenti, C.; Tata, A.M.; Luvisetto, S.; Pavone, F. The analgesic effect on neuropathic pain of retrogradely transported botulinum neurotoxin A involves Schwann cells and astrocytes. PLoS ONE 2012, 7, e47977. [Google Scholar] [CrossRef] [PubMed]
- Silva, L.B.D.; Poulsen, J.N.; Arendt-Nielsen, L.; Gazerani, P. Botulinum neurotoxin type A modulates vesicular release of glutamate from satellite glial cells. J. Cell. Mol. Med. 2015, 19, 1900–1909. [Google Scholar] [CrossRef] [PubMed]
- Zychowska, M.; Rojewska, E.; Makuch, W.; Luvisetto, S.; Pavone, F.; Marinelli, S.; Przewlocka, B.; Mika, J. Participation of pro-and anti-nociceptive interleukins in botulinum toxin A-induced analgesia in a rat model of neuropathic pain. Eur. J. Pharmacol. 2016, 791, 377–388. [Google Scholar] [CrossRef] [PubMed]
- Aurora, S.; Dodick, D.W.; Turkel, C.; DeGryse, R.; Silberstein, S.; Lipton, R.; Diener, H.; Brin, M. OnabotulinumtoxinA for treatment of chronic migraine: Results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 1 trial. Cephalalgia 2010, 30, 793–803. [Google Scholar] [CrossRef] [PubMed]
- Silberstein, S.D.; Dodick, D.W.; Aurora, S.K.; Diener, H.-C.; DeGryse, R.E.; Lipton, R.B.; Turkel, C.C. Per cent of patients with chronic migraine who responded per onabotulinumtoxinA treatment cycle: PREEMPT. J. Neurol. Neurosurg. Psychiatry 2015, 86, 996–1001. [Google Scholar] [CrossRef] [PubMed]
- Simpson, D.M.; Hallett, M.; Ashman, E.J.; Comella, C.L.; Green, M.W.; Gronseth, G.S.; Armstrong, M.J.; Gloss, D.; Potrebic, S.; Jankovic, J. Practice guideline update summary: Botulinum neurotoxin for the treatment of blepharospasm, cervical dystonia, adult spasticity, and headache Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology 2016, 86, 1818–1826. [Google Scholar] [CrossRef] [PubMed]
- Relja, M.; Telarović, S. Botulinum toxin in tension-type headache. J. Neurol. 2004, 251, i12–i14. [Google Scholar] [CrossRef] [PubMed]
- Padberg, M.; De Bruijn, S.; De Haan, R.; Tavy, D. Treatment of chronic tension-type headache with botulinum toxin: A double-blind, placebo-controlled clinical trial. Cephalalgia 2004, 24, 675–680. [Google Scholar] [CrossRef] [PubMed]
- Schulte-Mattler, W.J.; Krack, P.; Group, B.S. Treatment of chronic tension-type headache with botulinum toxin A: A randomized, double-blind, placebo-controlled multicenter study. Pain 2004, 109, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Silberstein, S.D.; Göbel, H.; Jensen, R.; Elkind, A.H.; Degryse, R.; Walcott, J.M.; Turkel, C. Botulinum toxin type A in the prophylactic treatment of chronic tension-type headache: A multicentre, double-blind, randomized, placebo-controlled, parallel-group study. Cephalalgia 2006, 26, 790–800. [Google Scholar] [CrossRef] [PubMed]
- Khenioui, H.; Houvenagel, E.; Catanzariti, J.F.; Guyot, M.A.; Agnani, O.; Donze, C. Usefulness of intra-articular botulinum toxin injections. A systematic review. Jt. Bone Spine 2016, 83, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Heikkilä, H.; Hielm-Björkman, A.; Morelius, M.; Larsen, S.; Honkavaara, J.; Innes, J.; Laitinen-Vapaavuori, O. Intra-articular botulinum toxin A for the treatment of osteoarthritic joint pain in dogs: A randomized, double-blinded, placebo-controlled clinical trial. Vet. J. 2014, 200, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Vilhegas, S.; Cassu, R.; Barbero, R.; Crociolli, G.; Rocha, T.; Gomes, D. Botulinum toxin type A as an adjunct in postoperative pain management in dogs undergoing radical mastectomy. Vet. Rec. 2015, 177, 391. [Google Scholar] [CrossRef] [PubMed]
- Mittal, S.; Machado, D.G.; Jabbari, B. OnabotulinumtoxinA for treatment of focal cancer pain after surgery and/or radiation. Pain Med. 2012, 13, 1029–1033. [Google Scholar] [CrossRef] [PubMed]
- Lacković, Z.; Filipović, B.; Matak, I.; Helyes, Z. Activity of botulinum toxin type A in cranial dura: Implications for treatment of migraine and other headaches. Br. J. Pharmacol. 2016, 173, 279–291. [Google Scholar] [CrossRef] [PubMed]
- Drinovac Vlah, V.; Filipović, B.; Bach-Rojecky, L.; Lacković, Z. Role of central versus peripheral opioid system in antinociceptive and anti-inflammatory effect of botulinum toxin type A in trigeminal region. Eur. J. Pain 2017, 22, 583–591. [Google Scholar] [CrossRef] [PubMed]
- Nelson, A.E. Osteoarthritis year in review 2017: Clinical. Osteoarthr. Cartil. 2018, 26, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Kidd, B.L. Osteoarthritis and joint pain. Pain 2006, 123, 6–9. [Google Scholar] [CrossRef] [PubMed]
- Martell-Pelletier, J.; Barr, A.J.; Cicuttini, F.M.; Conaghan, P.G.; Cooper, C.; Goldring, M.B.; Goldring, S.R.; Jones, G.; Teichthal, A.J.; Pelletier, J. Osteoarthritis. Nat. Rev. Dis. Prim. 2016, 2, 16072. [Google Scholar] [CrossRef] [PubMed]
- Ivanusic, J.J. Molecular Mechanisms That Contribute to Bone Marrow Pain. Front. Neurol. 2017, 8, 458. [Google Scholar] [CrossRef] [PubMed]
- Schaible, H.-G.; Ebersberger, A.; Von Banchet, G.S. Mechanisms of Pain in Arthritis. Ann. N. Y. Acad. Sci. 2002, 966, 343–354. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, L.-F.; Wu, C.-W.; Chou, C.-C.; Yang, S.-W.; Wu, S.-H.; Lin, Y.-J.; Hsu, W.-C. Effects of botulinum toxin landmark-guided intra-articular injection in subjects with knee osteoarthritis. PM&R 2016, 8, 1127–1135. [Google Scholar]
- Arendt-Nielsen, L.; Jiang, G.; DeGryse, R.; Turkel, C. Intra-articular onabotulinumtoxinA in osteoarthritis knee pain: Effect on human mechanistic pain biomarkers and clinical pain. Scand. J. Rheumatol. 2017, 46, 303–316. [Google Scholar] [CrossRef] [PubMed]
- Krug, H.E.; Frizelle, S.; McGarraugh, P.; Mahowald, M.L. Pain behavior measures to quantitate joint pain and response to neurotoxin treatment in murine models of arthritis. Pain Med. 2009, 10, 1218–1228. [Google Scholar] [CrossRef] [PubMed]
- Anderson, S.; Krug, H.; Dorman, C.; McGarraugh, P.; Frizelle, S.; Mahowald, M. Analgesic effects of intra-articular botulinum toxin Type B in a murine model of chronic degenerative knee arthritis pain. J. Pain Res. 2010, 3, 161. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Wang, K.; Chu, X.; Li, T.; Shen, N.; Fan, C.; Niu, Z.; Zhang, X.; Hu, L. Intra-articular injection of Botulinum toxin A reduces neurogenic inflammation in CFA-induced arthritic rat model. Toxicon 2017, 126, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Yoo, K.Y.; Lee, H.S.; Cho, Y.K.; Lim, Y.S.; Kim, Y.S.; Koo, J.H.; Yoon, S.J.; Lee, J.H.; Jang, K.H.; Song, S.H. Anti-inflammatory Effects of Botulinum Toxin Type A in a Complete Freund’s Adjuvant-Induced Arthritic Knee Joint of Hind Leg on Rat Model. Neurotox. Res. 2014, 26, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Chapple, C. Chapter 2: Pathophysiology of neurogenic detrusor overactivity and the symptom complex of “overactive bladder”. Neurourol. Urodyn. 2014, 33 (Suppl. S3), S6–S13. [Google Scholar] [CrossRef] [PubMed]
- Merrill, L.; Gonzalez, E.J.; Girard, B.M.; Vizzard, M.A. Receptors, channels, and signalling in the urothelial sensory system in the bladder. Nat. Rev. Urol. 2016, 13, 193–204. [Google Scholar] [CrossRef] [PubMed]
- Traini, C.; Fausssone-Pellegrini, M.S.; Guasti, D.; Del Popolo, G.; Frizzi, J.; Serni, S.; Vannucchi, M.G. Adaptive changes of telocytes in the urinary bladder of patients affected by neurogenic detrusor overactivity. J. Cell. Mol. Med. 2018, 22, 195–206. [Google Scholar] [CrossRef] [PubMed]
- Schurch, B.; Stohrer, M.; Kramer, G.; Schmid, D.M.; Gaul, G.; Hauri, D. Botulinum-A toxin for treating detrusor hyperreflexia in spinal cord injured patients: A new alternative to anticholinergic drugs? Preliminary results. J. Urol. 2000, 164, 692–697. [Google Scholar] [CrossRef]
- Khera, M.; Somogyi, G.T.; Kiss, S.; Boone, T.B.; Smith, C.P. Botulinum toxin A inhibits ATP release from bladder urothelium after chronic spinal cord injury. Neurochem. Int. 2004, 45, 987–993. [Google Scholar] [CrossRef] [PubMed]
- Collins, V.M.; Daly, D.M.; Liaskos, M.; McKay, N.G.; Sellers, D.; Chapple, C.; Grundy, D. OnabotulinumtoxinA significantly attenuates bladder afferent nerve firing and inhibits ATP release from the urothelium. BJU Int. 2013, 112, 1018–1026. [Google Scholar] [CrossRef] [PubMed]
- Lucioni, A.; Bales, G.T.; Lotan, T.L.; McGehee, D.S.; Cook, S.P.; Rapp, D.E. Botulinum toxin type A inhibits sensory neuropeptide release in rat bladder models of acute injury and chronic inflammation. BJU Int. 2008, 101, 366–370. [Google Scholar] [CrossRef] [PubMed]
- Jhang, J.F.; Kuo, H.C. Botulinum Toxin A and Lower Urinary Tract Dysfunction: Pathophysiology and Mechanisms of Action. Toxins (Basel) 2016, 8, 120. [Google Scholar] [CrossRef] [PubMed]
- Giannantoni, A.; Conte, A.; Farfariello, V.; Proietti, S.; Vianello, A.; Nardicchi, V.; Santoni, G.; Amantini, C. Onabotulinumtoxin-A intradetrusorial injections modulate bladder expression of NGF, TrkA, p75 and TRPV1 in patients with detrusor overactivity. Pharmacol. Res. 2013, 68, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Loiseau, C.; Iezhova, T.; Valkiunas, G.; Chasar, A.; Hutchinson, A.; Buermann, W.; Smith, T.B.; Sehgal, R.N. Spatial variation of haemosporidian parasite infection in African rainforest bird species. J. Parasitol. 2010, 96, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Maignel-Ludop, J.; Huchet, M.; Krupp, J. Botulinum Neurotoxins Serotypes A and B induce paralysis of mouse striated and smooth muscles with different potencies. Pharmacol. Res. Perspect. 2017, 5, e00289. [Google Scholar] [CrossRef] [PubMed]
- Coelho, A.; Dinis, P.; Pinto, R.; Gorgal, T.; Silva, C.; Silva, A.; Silva, J.; Cruz, C.D.; Cruz, F.; Avelino, A. Distribution of the high-affinity binding site and intracellular target of botulinum toxin type A in the human bladder. Eur. Urol. 2010, 57, 884–890. [Google Scholar] [CrossRef] [PubMed]
- Coelho, A.; Oliveira, R.; Cruz, F.; Cruz, C.D. Impairment of sensory afferents by intrathecal administration of botulinum toxin A improves neurogenic detrusor overactivity in chronic spinal cord injured rats. Exp. Neurol. 2016, 285, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Eming, S.A.; Martin, P.; Tomic-Canic, M. Wound repair and regeneration: Mechanisms, signaling, and translation. Sci. Transl. Med. 2014, 6, 265sr266. [Google Scholar] [CrossRef] [PubMed]
- Lebeda, F.J.; Dembek, Z.F.; Adler, M. Kinetic and reaction pathway analysis in the application of botulinum toxin A for wound healing. J. Toxicol. 2012, 2012, 159726. [Google Scholar] [CrossRef] [PubMed]
- Ziade, M.; Domergue, S.; Batifol, D.; Jreige, R.; Sebbane, M.; Goudot, P.; Yachouh, J. Use of botulinum toxin type A to improve treatment of facial wounds: A prospective randomised study. JPRAS 2013, 66, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Prodromidou, A.; Frountzas, M.; Vlachos, D.-E.G.; Vlachos, G.D.; Bakoyiannis, I.; Perrea, D.; Pergialiotis, V. Botulinum toxin for the prevention and healing of wound scars: A systematic review of the literature. Plast. Surg. 2015, 23, 260–264. [Google Scholar] [CrossRef]
- Lee, B.-J.; Jeong, J.-H.; Wang, S.-G.; Lee, J.-C.; Goh, E.-K.; Kim, H.-W. Effect of botulinum toxin type a on a rat surgical wound model. Clin. Exp. Otorhinolaryngol. 2009, 2, 20. [Google Scholar] [CrossRef] [PubMed]
- Kiritsi, D.; Nyström, A. The role of TGFβ in wound healing pathologies. Mech. Ageing Dev. 2017. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Z.; Zhang, F.; Lin, W.; Zhang, M.; Liu, Y. Effect of botulinum toxin type A on transforming growth factor beta1 in fibroblasts derived from hypertrophic scar: A preliminary report. Aesth. Plast. Surg. 2010, 34, 424–427. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Z.; Zhang, M.; Liu, Y.; Ren, L. Botulinum toxin type a inhibits connective tissue growth factor expression in fibroblasts derived from hypertrophic scar. Aesth. Plast. Surg. 2011, 35, 802–807. [Google Scholar] [CrossRef] [PubMed]
- Pirazzini, M.; Rossetto, O.; Eleopra, R.; Montecucco, C. Botulinum Neurotoxins: Biology, Pharmacology, and Toxicology. Pharmacol. Rev. 2017, 69, 200–235. [Google Scholar] [CrossRef] [PubMed]
- Popoff, M.R.; Poulain, B. Bacterial toxins and the nervous system: Neurotoxins and multipotential toxins interacting with neuronal cells. Toxins (Basel) 2010, 2, 683–737. [Google Scholar] [CrossRef] [PubMed]
- Poulain, B. How do the Botulinum Neurotoxins block neurotransmitter release: From botulism to the molecular mechanism of action. Botulinum J. 2008, 1, 14–87. [Google Scholar] [CrossRef]
- Rossetto, O. Botulinum Toxins: Molecular Structures and Synaptic Physiology. Botulinum Toxin Treat. Clin. Med. 2018, 1–12. [Google Scholar] [CrossRef]
- Rossetto, O.; Pirazzini, M.; Montecucco, C. Botulinum neurotoxins: Genetic, structural and mechanistic insights. Nat. Rev. Microbiol. 2014, 12, 535–549. [Google Scholar] [CrossRef] [PubMed]
- Rummel, A. The long journey of botulinum neurotoxins into the synapse. Toxicon 2015, 107, 9–24. [Google Scholar] [CrossRef] [PubMed]
- Matak, I.; Lackovic, Z.; Relja, M. Botulinum toxin type A in motor nervous system: Unexplained observations and new challenges. J. Neural Transm. (Vienna) 2016, 123, 1415–1421. [Google Scholar] [CrossRef] [PubMed]
- Mazzocchio, R.; Caleo, M. More than at the neuromuscular synapse: Actions of botulinum neurotoxin A in the central nervous system. Neuroscientist 2015, 21, 44–61. [Google Scholar] [CrossRef] [PubMed]
- Kanovsky, P.; Streitova, H.; Dufek, J.; Znojil, V.; Daniel, P.; Rektor, I. Change in lateralization of the P22/N30 cortical component of median nerve somatosensory evoked potentials in patients with cervical dystonia after successful treatment with botulinum toxin A. Mov. Disord. 1998, 13, 108–117. [Google Scholar] [CrossRef] [PubMed]
- Delnooz, C.C.; Pasman, J.W.; van de Warrenburg, B.P. Dynamic cortical gray matter volume changes after botulinum toxin in cervical dystonia. Neurobiol. Dis. 2015, 73, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Behari, M.; Raju, G.B. Electrophysiological studies in patients with blepharospasm before and after botulinum toxin A therapy. J. Neurol. Sci. 1996, 135, 74–77. [Google Scholar] [CrossRef]
- Bielamowicz, S.; Ludlow, C.L. Effects of botulinum toxin on pathophysiology in spasmodic dysphonia. Ann. Otol. Rhinol. Laryngol. 2000, 109, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Marchand-Pauvert, V.; Aymard, C.; Giboin, L.S.; Dominici, F.; Rossi, A.; Mazzocchio, R. Beyond muscular effects: Depression of spinal recurrent inhibition after botulinum neurotoxin A. J. Physiol. 2013, 591, 1017–1029. [Google Scholar] [CrossRef] [PubMed]
- Aymard, C.; Giboin, L.S.; Lackmy-Vallee, A.; Marchand-Pauvert, V. Spinal plasticity in stroke patients after botulinum neurotoxin A injection in ankle plantar flexors. Physiol. Rep. 2013, 1, e00173. [Google Scholar] [CrossRef] [PubMed]
- Clowry, G.J.; Walker, L.; Davies, P. The effects of botulinum neurotoxin A induced muscle paresis during a critical period upon muscle and spinal cord development in the rat. Exp. Neurol. 2006, 202, 456–469. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Forero, D.; Pastor, A.M.; Geiman, E.J.; Benitez-Temino, B.; Alvarez, F.J. Regulation of gephyrin cluster size and inhibitory synaptic currents on Renshaw cells by motor axon excitatory inputs. J. Neurosci. 2005, 25, 417–429. [Google Scholar] [CrossRef] [PubMed]
- Cai, B.B.; Francis, J.; Brin, M.F.; Broide, R.S. Botulinum neurotoxin type A-cleaved SNAP25 is confined to primary motor neurons and localized on the plasma membrane following intramuscular toxin injection. Neuroscience 2017, 352, 155–169. [Google Scholar] [CrossRef] [PubMed]
- Koizumi, H.; Goto, S.; Okita, S.; Morigaki, R.; Akaike, N.; Torii, Y.; Harakawa, T.; Ginnaga, A.; Kaji, R. Spinal Central Effects of Peripherally Applied Botulinum Neurotoxin A in Comparison between Its Subtypes A1 and A2. Front. Neurol. 2014, 5, 98. [Google Scholar] [CrossRef] [PubMed]
- Matak, I.; Riederer, P.; Lackovic, Z. Botulinum toxin’s axonal transport from periphery to the spinal cord. Neurochem. Int. 2012, 61, 236–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Filipovic, B.; Matak, I.; Bach-Rojecky, L.; Lackovic, Z. Central action of peripherally applied botulinum toxin type A on pain and dural protein extravasation in rat model of trigeminal neuropathy. PLoS ONE 2012, 7, e29803. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Restani, L.; Giribaldi, F.; Manich, M.; Bercsenyi, K.; Menendez, G.; Rossetto, O.; Caleo, M.; Schiavo, G. Botulinum neurotoxins A and E undergo retrograde axonal transport in primary motor neurons. PLoS Pathog. 2012, 8, e1003087. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Xie, N.; Lian, Y.; Xu, H.; Chen, C.; Zheng, Y.; Chen, Y.; Zhang, H. Central antinociceptive activity of peripherally applied botulinum toxin type A in lab rat model of trigeminal neuralgia. Springerplus 2016, 5, 431. [Google Scholar] [CrossRef] [PubMed]
- Restani, L.; Novelli, E.; Bottari, D.; Leone, P.; Barone, I.; Galli-Resta, L.; Strettoi, E.; Caleo, M. Botulinum neurotoxin A impairs neurotransmission following retrograde transynaptic transport. Traffic 2012, 13, 1083–1089. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Martin, S.; Papadopulos, A.; Harper, C.B.; Mavlyutov, T.A.; Niranjan, D.; Glass, N.R.; Cooper-White, J.J.; Sibarita, J.B.; Choquet, D.; et al. Control of autophagosome axonal retrograde flux by presynaptic activity unveiled using botulinum neurotoxin type A. J. Neurosci. 2015, 35, 6179–6194. [Google Scholar] [CrossRef] [PubMed]
- Harper, C.B.; Papadopulos, A.; Martin, S.; Matthews, D.R.; Morgan, G.P.; Nguyen, T.H.; Wang, T.; Nair, D.; Choquet, D.; Meunier, F.A. Botulinum neurotoxin type-A enters a non-recycling pool of synaptic vesicles. Sci. Rep. 2016, 6, 19654. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, G.W.; Ovsepian, S.V.; Wang, J.; Aoki, K.R.; Dolly, J.O. Extravesicular intraneuronal migration of internalized botulinum neurotoxins without detectable inhibition of distal neurotransmission. Biochem. J. 2012, 441, 443–452. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, R.; Lam, C.; Yaksh, T.L. Botulinum toxin in migraine: Role of transport in trigemino-somatic and trigemino-vascular afferents. Neurobiol. Dis. 2015, 79, 111–122. [Google Scholar] [CrossRef] [PubMed]
- Bentivoglio, A.R.; Fasano, A.; Ialongo, T.; Soleti, F.; Lo Fermo, S.; Albanese, A. Fifteen-year experience in treating blepharospasm with Botox or Dysport: Same toxin, two drugs. Neurotox. Res. 2009, 15, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Wu, T.; Hu, X.; Wang, T. Efficacy and safety of botulinum toxin type A for upper limb spasticity after stroke or traumatic brain injury: A systematic review with meta-analysis and trial sequential analysis. Eur. J. Phys. Rehabil. Med. 2017, 53, 256–267. [Google Scholar] [PubMed]
- Gu, H.Y.; Song, J.K.; Zhang, W.J.; Xie, J.; Yao, Q.S.; Zeng, W.J.; Zhang, C.; Niu, Y.M. A systematic review and meta-analysis of effectiveness and safety of therapy for overactive bladder using botulinum toxin A at different dosages. Oncotarget 2017, 8, 90338–90350. [Google Scholar] [CrossRef] [PubMed]
- Naumann, M.; Jankovic, J. Safety of botulinum toxin type A: A systematic review and meta-analysis. Curr. Med. Res. Opin. 2004, 20, 981–990. [Google Scholar] [CrossRef] [PubMed]
- Shaari, C.M.; George, E.; Wu, B.L.; Biller, H.F.; Sanders, I. Quantifying the spread of botulinum toxin through muscle fascia. Laryngoscope 1991, 101, 960–964. [Google Scholar] [CrossRef] [PubMed]
- Yaraskavitch, M.; Leonard, T.; Herzog, W. Botox produces functional weakness in non-injected muscles adjacent to the target muscle. J. Biomech. 2008, 41, 897–902. [Google Scholar] [CrossRef] [PubMed]
- Arezzo, J.C. NeuroBloc/Myobloc: Unique features and findings. Toxicon 2009, 54, 690–696. [Google Scholar] [CrossRef] [PubMed]
- Borodic, G.E.; Joseph, M.; Fay, L.; Cozzolino, D.; Ferrante, R.J. Botulinum A toxin for the treatment of spasmodic torticollis: Dysphagia and regional toxin spread. Head Neck 1990, 12, 392–399. [Google Scholar] [CrossRef] [PubMed]
- Carli, L.; Montecucco, C.; Rossetto, O. Assay of diffusion of different botulinum neurotoxin type a formulations injected in the mouse leg. Muscle Nerve 2009, 40, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Hsu, T.S.; Dover, J.S.; Arndt, K.A. Effect of volume and concentration on the diffusion of botulinum exotoxin A. Arch. Dermatol. 2004, 140, 1351–1354. [Google Scholar] [CrossRef] [PubMed]
- Wohlfarth, K.; Schwandt, I.; Wegner, F.; Jurgens, T.; Gelbrich, G.; Wagner, A.; Bogdahn, U.; Schulte-Mattler, W. Biological activity of two botulinum toxin type A complexes (Dysport and Botox) in volunteers: A double-blind, randomized, dose-ranging study. J. Neurol. 2008, 255, 1932–1939. [Google Scholar] [CrossRef] [PubMed]
- Brodsky, M.A.; Swope, D.M.; Grimes, D. Diffusion of botulinum toxins. Tremor Other Hyperkinet. Mov. 2012, 2. [Google Scholar] [CrossRef]
- Bakheit, A.M.; Ward, C.D.; McLellan, D.L. Generalised botulism-like syndrome after intramuscular injections of botulinum toxin type A: A report of two cases. J. Neurol. Neurosurg. Psychiatry 1997, 62, 198. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, K.P.; Munchau, A.; Thompson, P.D.; Houser, M.; Chauhan, V.S.; Hutchinson, M.; Shapira, A.H.; Marsden, C.D. Generalised muscular weakness after botulinum toxin injections for dystonia: A report of three cases. J. Neurol. Neurosurg. Psychiatry 1999, 67, 90–93. [Google Scholar] [CrossRef] [PubMed]
- Ramirez-Castaneda, J.; Jankovic, J.; Comella, C.; Dashtipour, K.; Fernandez, H.H.; Mari, Z. Diffusion, spread, and migration of botulinum toxin. Mov. Disord. 2013, 28, 1775–1783. [Google Scholar] [CrossRef] [PubMed]
- Aoki, R.K. Botulinum neurotoxin serotypes A and B preparations have different safety margins in preclinical models of muscle weakening efficacy and systemic safety. Toxicon 2002, 40, 923–928. [Google Scholar] [CrossRef]
- Torii, Y.; Goto, Y.; Takahashi, M.; Ishida, S.; Harakawa, T.; Sakamoto, T.; Kaji, R.; Kozaki, S.; Ginnaga, A. Quantitative determination of biological activity of botulinum toxins utilizing compound muscle action potentials (CMAP), and comparison of neuromuscular transmission blockage and muscle flaccidity among toxins. Toxicon 2010, 55, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Johnson, E.A.; Tepp, W.H.; Lin, G. Purification, Characterization, and Use of Clostridium Botulinum Neurotoxin BoNT/A3. Patent WO2013049139, 4 April 2013. [Google Scholar]
- Torii, Y.; Goto, Y.; Nakahira, S.; Kozaki, S.; Kaji, R.; Ginnaga, A. Comparison of systemic toxicity between botulinum toxin subtypes A1 and A2 in mice and rats. Basic Clin. Pharmacol. Toxicol. 2015, 116, 524–528. [Google Scholar] [CrossRef] [PubMed]
- Schantz, E.J.; Johnson, E.A. Properties and Use of Botulinum Toxin and Other Microbial Neurotoxins in Medicine. Microbiol. Rev. 1992, 56, 80–99. [Google Scholar] [PubMed]
- Frokjaer, S.; Otzen, D.E. Protein drug stability: A formulation challenge. Nature 2005, 298–306. [Google Scholar] [CrossRef] [PubMed]
- Ascher, B.; Kestemont, P.; Boineau, D.; Bodokh, I.; Stein, A.; Heckmann, M.; Dendorfer, M.; Pavicic, T.; Volteau, M.; Tse, A.; et al. Liquid Formulation of AbobotulinumtoxinA Exhibits a Favorable Efficacy and Safety Profile in Moderate to Severe Glabellar Lines: A Randomized, Double-Blind, Placebo- and Active Comparator-Controlled Trial. Aesthet. Surg. J. 2018, 38, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Jankovic, J. Botulinum toxin in clinical practice. J. Neurol. Neurosurg. Psychiatry 2004, 75, 951–957. [Google Scholar] [CrossRef] [PubMed]
- Bagramyan, K.; Barash, J.R.; Arnon, S.S.; Kalkum, M. Attomolar Detection of Botulinum Toxin Type A in Complex Biological Matrices. PLoS ONE 2008. [Google Scholar] [CrossRef] [PubMed]
- Mason, J.T.; Xu, L.; Sheng, Z.-M.; He, J.; O’Leary, T.J. Liposome polymerase chain reaction assay for the sub-attomolar detection of cholera toxin and botulinum toxin type A. Nat. Protocol. 2006, 1, 2003–2011. [Google Scholar] [CrossRef] [PubMed]
- Prausnitz, M.R.; Langer, R. Transdermal drug delivery. Nat. Biotechnol. 2008, 26, 1261–1268. [Google Scholar] [CrossRef] [PubMed]
- Waugh, J.M.; Lee, J.; Dake, M.D.; Browne, D. Nonclinical and clinical experiences with CPP-based self-assembling peptide systems in topical drug development. Cell Penetr. Pept. Methods Protocol. 2011, 553–572. [Google Scholar]
- Jones, T.; Jeremy Scott, C.; Tranowski, D.; Joshi, T. Safety and Tolerability of Topical Botulinum Toxin Type A in Healthy Adults. In Proceedings of the 69th Annual Meeting of the Society for Investigative Dermatology, Montreal, QC, Canada, 6–9 May 2009. [Google Scholar]
- Brandt, F.; O’connell, C.; Cazzaniga, A.; Waugh, J.M. Efficacy and safety evaluation of a novel botulinum toxin topical gel for the treatment of moderate to severe lateral canthal lines. Dermatol. Surg. 2010, 36, 2111–2118. [Google Scholar] [CrossRef] [PubMed]
- Glogau, R.; Brandt, F.; Kane, M.; Monheit, G.D.; Waugh, J.M. Results of a randomized, double-blind, placebo-controlled study to evaluate the efficacy and safety of a botulinum toxin type A topical gel for the treatment of moderate-to-severe lateral canthal lines. J. Drugs Dermatol. 2012, 11, 38–45. [Google Scholar] [PubMed]
- Glogau, R.G. Topically applied botulinum toxin type A for the treatment of primary axillary hyperhidrosis: Results of a randomized, blinded, vehicle-controlled study. Dermatol. Surg. 2007, 33, S76–S80. [Google Scholar] [CrossRef] [PubMed]
- Chajchir, I.; Modi, P.; Chajchir, A. Novel topical BoNTA (CosmeTox, toxin type A) cream used to treat hyperfunctional wrinkles of the face, mouth, and neck. Aesthet. Plast. Surg. 2008, 32, 715–722. [Google Scholar] [CrossRef] [PubMed]
- Carmichael, N.M.; Dostrovsky, J.O.; Charlton, M.P. Peptide-mediated transdermal delivery of botulinum neurotoxin type A reduces neurogenic inflammation in the skin. Pain 2010, 149, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Saffarian, P.; Peerayeh, S.N.; Amani, J.; Ebrahimi, F.; Sedighian, H.; Halabian, R.; Fooladi, A.A.I. TAT-BoNT/A (1–448), a novel fusion protein as a therapeutic agent: Analysis of transcutaneous delivery and enzyme activity. Appl. Microbiol. Biotechnol. 2016, 100, 2785–2795. [Google Scholar] [CrossRef] [PubMed]
- Saffarian, P.; Peerayeh, S.N.; Amani, J.; Ebrahimi, F.; Sedighianrad, H.; Halabian, R.; Imani Fooladi, A.A. Expression and purification of recombinant TAT-BoNT/A (1–448) under denaturing and native conditions. Bioengineered 2016, 7, 478–483. [Google Scholar] [CrossRef] [PubMed]
- Chow, A.; Wilder-Smith, E. Effect of transdermal botulinum toxin on sweat secretion in subjects with idiopathic palmar hyperhidrosis. Br. J. Dermatol. 2009, 160, 721–722. [Google Scholar] [CrossRef] [PubMed]
- Kavanagh, G.M.; Shams, K. Botulinum toxin type A by iontophoresis for primary palmar hyperhidrosis. J. Am. Acad. Dermatol. 2006, 55, S115–S117. [Google Scholar] [CrossRef] [PubMed]
- Pacini, S.; Gulisano, M.; Punzi, T.; Ruggiero, M. Transdermal delivery of Clostridium botulinum toxin type A by pulsed current iontophoresis. J. Am. Acad. Dermatol. 2007, 57, 1097–1099. [Google Scholar] [CrossRef] [PubMed]
- Iannitti, T.; Palmieri, B.; Aspiro, A.; Di Cerbo, A. A preliminary study of painless and effective transdermal botulinum toxin A delivery by jet nebulization for treatment of primary hyperhidrosis. Drug Des. Dev. Ther. 2014, 8, 931. [Google Scholar] [CrossRef] [PubMed]
- Bariya, S.H.; Gohel, M.C.; Mehta, T.A.; Sharma, O.P. Microneedles: An emerging transdermal drug delivery system. J. Pharm. Pharmacol. 2012, 64, 11–29. [Google Scholar] [CrossRef] [PubMed]
- Torrisi, B.M.; Zarnitsyn, V.; Prausnitz, M.; Anstey, A.; Gateley, C.; Birchall, J.C.; Coulman, S. Pocketed microneedles for rapid delivery of a liquid-state botulinum toxin A formulation into human skin. J. Control. Release 2013, 165, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Tyagi, P.; Kashyap, M.; Yoshimura, N.; Chancellor, M.; Chermansky, C.J. Past, Present and Future of Chemodenervation with Botulinum Toxin in the Treatment of Overactive Bladder. J. Urol. 2017, 197, 982–990. [Google Scholar] [CrossRef] [PubMed]
- Khera, M.; Somogyi, G.T.; Salas, N.A.; Kiss, S.; Boone, T.B.; Smith, C.P. In vivo effects of botulinum toxin A on visceral sensory function in chronic spinal cord-injured rats. Urology 2005, 66, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, S.; Wheeler, M.; Saito, M.; Weiss, R.; Hittelman, A. 907 Effect of intravesical botulinum toxin a delivery (using dmso) in rat overactive bladder model. J. Urol. 2012, 187, e370. [Google Scholar] [CrossRef]
- Petrou, S.P.; Parker, A.S.; Crook, J.E.; Rogers, A.; Metz-Kudashick, D.; Thiel, D.D. Botulinum a toxin/dimethyl sulfoxide bladder instillations for women with refractory idiopathic detrusor overactivity: A phase 1/2 study. Mayo Clin. Proc. 2009, 84, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Vemulakonda, V.M.; Somogyi, G.T.; Kiss, S.; Salas, N.A.; Boone, T.B.; Smith, C.P. Inhibitory effect of intravesically applied botulinum toxin A in chronic bladder inflammation. J. Urol. 2005, 173, 621–624. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, D.; O’Leary, M.; Erickson, J.; Marx, S.; Chancellor, M. Safety and efficacy with bladder botulinum toxin in elderly patients. In Proceedings of the International Continence Society Annual Meeting, Montreal, QC, Canada, 28 August–2 September 2005. [Google Scholar]
- Chuang, Y.-C.; Yoshimura, N.; Huang, C.-C.; Wu, M.; Chiang, P.-H.; Chancellor, M.B. Intravesical botulinum toxin A administration inhibits COX-2 and EP4 expression and suppresses bladder hyperactivity in cyclophosphamide-induced cystitis in rats. Eur. Urol. 2009, 56, 159–167. [Google Scholar] [CrossRef] [PubMed]
- El Shatoury, M.; Di Young, L.; Turley, E.; Yazdani, A.; Dave, S. Early experimental results of using a novel delivery carrier, hyaluronan-phosphatidylethanolamine (HA-PE), which may allow simple bladder instillation of botulinum toxin A as effectively as direct detrusor muscle injection. J. Pediatr. Urol. 2017. [Google Scholar] [CrossRef] [PubMed]
- Krhut, J.; Navratilova, M.; Sykora, R.; Jurakova, M.; Gärtner, M.; Mika, D.; Pavliska, L.; Zvara, P. Intravesical instillation of onabotulinum toxin A embedded in inert hydrogel in the treatment of idiopathic overactive bladder: A double-blind randomized pilot study. Scand. J. Urol. 2016, 50, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Chuang, Y.-C.; Tyagi, P.; Huang, C.-C.; Yoshimura, N.; Wu, M.; Kaufman, J.; Chancellor, M.B. Urodynamic and immunohistochemical evaluation of intravesical botulinum toxin A delivery using liposomes. J. Urol. 2009, 182, 786–792. [Google Scholar] [CrossRef] [PubMed]
- Chuang, Y.-C.; Kaufmann, J.H.; Chancellor, D.D.; Chancellor, M.B.; Kuo, H.-C. Bladder instillation of liposome encapsulated onabotulinumtoxina improves overactive bladder symptoms: A prospective, multicenter, double-blind, randomized trial. J. Urol. 2014, 192, 1743–1749. [Google Scholar] [CrossRef] [PubMed]
- Chuang, Y.-C.; Huang, T.-L.; Tyagi, P.; Huang, C.-C. Urodynamic and immunohistochemical evaluation of intravesical botulinum toxin A delivery using low energy shock waves. J. Urol. 2016, 196, 599–608. [Google Scholar] [CrossRef] [PubMed]
- Kajbafzadeh, A.-M.; Montaser-Kouhsari, L.; Ahmadi, H.; Sotoudeh, M. Intravesical electromotive botulinum toxin type A administration: Part I—Experimental study. Urology 2011, 77, 1460–1464. [Google Scholar] [CrossRef] [PubMed]
- Schiotz, H.A.; Mai, H.T.; Zabielska, R. Intravesical Electromotive Botulinum Toxin in Women with Overactive Bladder—A Pilot Study. ARC J. Gynecol. Obs. 2017, 2, 4–10. [Google Scholar]
- Kajbafzadeh, A.-M.; Ahmadi, H.; Montaser-Kouhsari, L.; Sharifi-Rad, L.; Nejat, F.; Bazargan-Hejazi, S. Intravesical electromotive botulinum toxin type A administration—Part II: Clinical application. Urology 2011, 77, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Ladi-Seyedian, S.-S.; Sharifi-Rad, L.; Kajbafzadeh, A.-M. Intravesical Electromotive Botulinum Toxin Type “A” Administration for Management of Urinary Incontinence Secondary to Neuropathic Detrusor Overactivity in Children: Long-Term Follow-up. Urology 2017, in press. [Google Scholar] [CrossRef] [PubMed]
- Kajbafzadeh, A.-M.; Sharifi-Rad, L.; Ladi-Seyedian, S.-S. Intravesical electromotive botulinum toxin type A administration for management of concomitant neuropathic bowel and bladder dysfunction in children. Int. J. Colorectal Dis. 2016, 31, 1397–1399. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.; Stone, H.F.; Thach, T.Q.; Garcia, L.; Ruegg, C.L. A novel botulinum neurotoxin topical gel: Treatment of allergic rhinitis in rats and comparative safety profile. Am. J. Rhinol. Allergy 2012, 26, 450–454. [Google Scholar] [CrossRef] [PubMed]
- Rohrbach, S.; Junghans, K.; Köhler, S.; Laskawi, R. Minimally invasive application of botulinum toxin A in patients with idiopathic rhinitis. Head Face Med. 2009, 5, 18. [Google Scholar] [CrossRef] [PubMed]



| AboA 1 | IncoA 2 | OnaA 3 | RimaB 4 | |
|---|---|---|---|---|
| 1st Approval | 1991 | 2005 | 1989 | 2000 |
| Serotype | A1 | A1 | A1 | B |
| Strain | Hall | Hall | Hall | Bean |
| Purification Method s | Chromatography | Unpublished | Crystallization | Chromatography |
| Complex Size | >500 kD | 150 kD | 900 kD | 700 kD |
| Excipients | HSA (125 µg) Lactose | HSA (1 mg) Sucrose | HSA (500 µg) Sodium chloride | HSA (500 µg/mL) Sodium succinate Sodium chloride |
| Stabilization | Lyophilization | Lyophilization | Vacuum drying | Solution |
| Solubilization | Normal saline | Normal saline | Normal saline | N/A |
| pH | ~7 | ~7 | ~7 | 5.6 |
| Unitage (U/vial) | 300, 500 | 100, 200 | 100, 200 | 2500, 5000, 10,000 |
| Shelf Life (months) | 24 | 36 | 36 | 24 |
| Neurotoxin Protein (ng/vial) † | 4.35 | 0.6 | 5 | ~25, 50, 100 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fonfria, E.; Maignel, J.; Lezmi, S.; Martin, V.; Splevins, A.; Shubber, S.; Kalinichev, M.; Foster, K.; Picaut, P.; Krupp, J. The Expanding Therapeutic Utility of Botulinum Neurotoxins. Toxins 2018, 10, 208. https://0-doi-org.brum.beds.ac.uk/10.3390/toxins10050208
Fonfria E, Maignel J, Lezmi S, Martin V, Splevins A, Shubber S, Kalinichev M, Foster K, Picaut P, Krupp J. The Expanding Therapeutic Utility of Botulinum Neurotoxins. Toxins. 2018; 10(5):208. https://0-doi-org.brum.beds.ac.uk/10.3390/toxins10050208
Chicago/Turabian StyleFonfria, Elena, Jacquie Maignel, Stephane Lezmi, Vincent Martin, Andrew Splevins, Saif Shubber, Mikhail Kalinichev, Keith Foster, Philippe Picaut, and Johannes Krupp. 2018. "The Expanding Therapeutic Utility of Botulinum Neurotoxins" Toxins 10, no. 5: 208. https://0-doi-org.brum.beds.ac.uk/10.3390/toxins10050208