Immunogenicity Associated with Botulinum Toxin Treatment
Abstract
:1. Introduction
2. Definitions
2.1. Primary Non-Response
2.2. Secondary Non-Response
3. Botulinum Toxin Structure and Function
4. Botulinum Toxin Antibodies
5. Antibody Detection
6. Clinical Resistance Tests
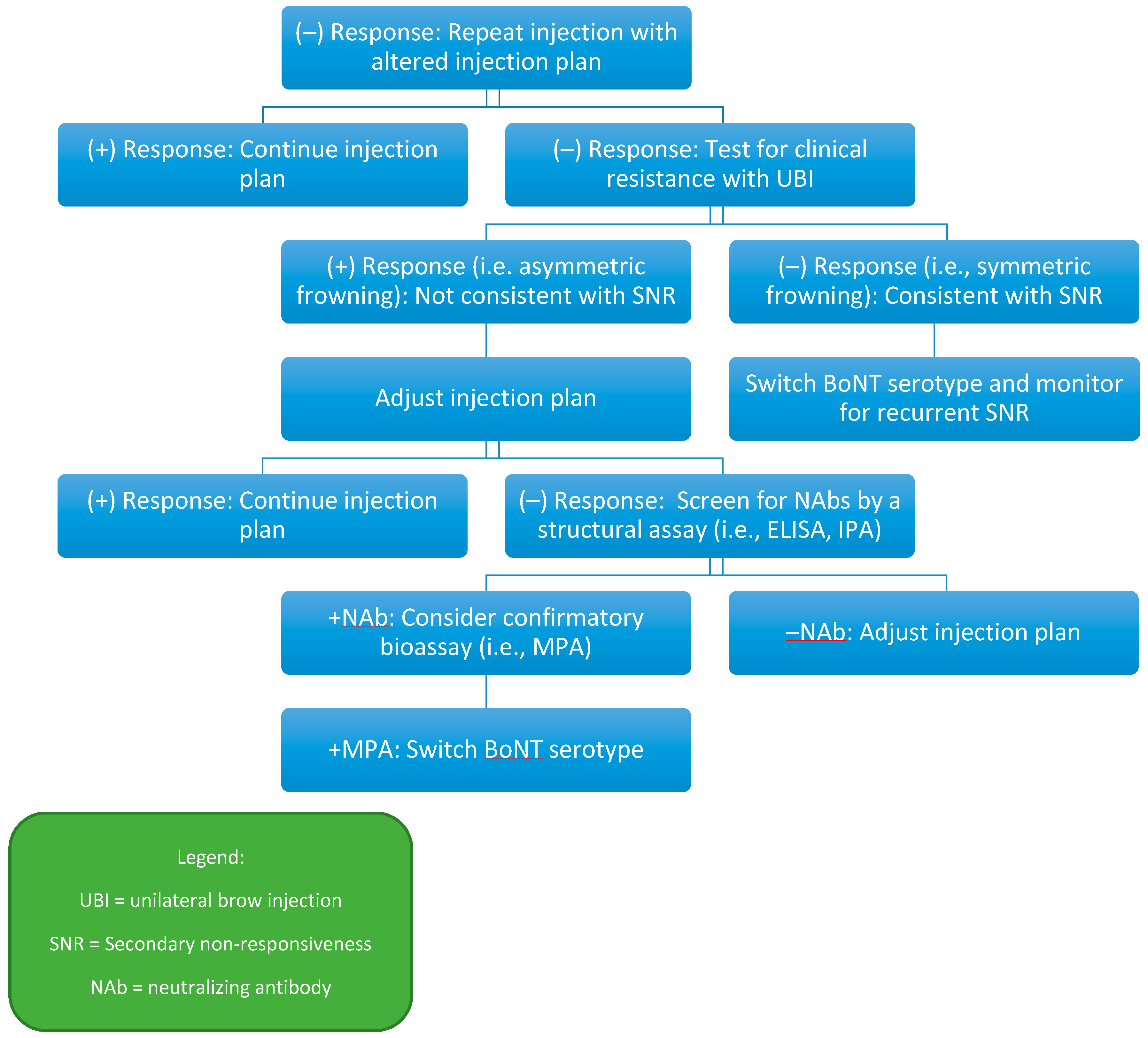
7. Immunogenicity by Indication
8. Immunogenicity by Formulation
8.1. OnabotulinumtoxinA
8.2. AbobotulinumtoxinA
8.3. RimabotulinumtoxinB
8.4. IncobotulinumtoxinA
9. Immunogenicity and Duration of Treatment
10. Discussion
11. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Jankovic, J. Botulinum Toxin: State of the Art. Mov. Disord. 2017, 32, 1131–1138. [Google Scholar] [CrossRef] [PubMed]
- Jankovic, J.; Orman, J. Botulinum A Toxin for Cranial-Cervical Dystonia: A Double-Blind, Placebo-Controlled Study. Neurology 1987, 37, 616–623. [Google Scholar] [CrossRef] [PubMed]
- Dressler, D. Clinical Presentation and Management of Antibody-Induced Failure of Botulinum Toxin Therapy. Mov. Disord. 2004, 19 (Suppl. 8), S92–S100. [Google Scholar] [CrossRef]
- Hsiung, G.Y.R.; Das, S.K.; Ranawaya, R.; Lafontaine, A.L.; Suchowersky, O. Long-Term Efficacy of Botulinum Toxin A in Treatment of Various Movement Disorders over a 10-Year Period. Mov. Disord. 2002, 17, 1288–1293. [Google Scholar] [CrossRef] [PubMed]
- Ramirez-Castaneda, J.; Jankovic, J. Long-Term Efficacy and Safety of Botulinum Toxin Injections in Dystonia. Toxins (Basel) 2013, 5, 249–266. [Google Scholar] [CrossRef] [PubMed]
- Pittman, P.R.; Hack, D.; Mangiafico, J.; Gibbs, P.; McKee, K.T.; Friedlander, A.M.; Sjogren, M.H. Antibody Response to a Delayed Booster Dose of Anthrax Vaccine and Botulinum Toxoid. Vaccine 2002, 20, 2107–2115. [Google Scholar] [CrossRef]
- Naumann, M.; Boo, L.M.; Ackerman, A.H.; Gallagher, C.J. Immunogenicity of Botulinum Toxins. J. Neural Transm. 2013, 120, 275–290. [Google Scholar] [CrossRef]
- BOTOX® [Package Insert]; Allergan, Inc.: Madison, NJ, USA, 2019.
- Trindade De Almeida, A.R.; Secco, L.C.; Carruthers, A. Handling Botulinum Toxins: An Updated Literature Review. Dermatol. Surg. 2011, 37, 1553–1565. [Google Scholar] [CrossRef]
- Gartlan, M.G.; Hoffman, H.T. Crystalline Preparation of Botulinum Toxin Type A (Botox): Degradation in Potency with Storage. Otolaryngol. Head. Neck Surg. 1993, 108, 135–140. [Google Scholar] [CrossRef]
- Albanese, A.; Bhatia, K.; Bressman, S.B.; Delong, M.R.; Fahn, S.; Fung, V.S.C.; Hallett, M.; Jankovic, J.; Jinnah, H.A.; Klein, C.; et al. Phenomenology and Classification of Dystonia: A Consensus Update. Mov. Disord. 2013, 28, 863–873. [Google Scholar] [CrossRef]
- Pirazzini, M.; Carle, S.; Barth, H.; Rossetto, O.; Montecucco, C. Primary Resistance of Human Patients to Botulinum Neurotoxins A and B. Ann. Clin. Transl. Neurol. 2018, 5, 971–975. [Google Scholar] [CrossRef] [PubMed]
- Oshima, M.; Deitiker, P.; Hastings-Ison, T.; Aoki, K.R.; Graham, H.K.; Atassi, M.Z. Antibody Responses to Botulinum Neurotoxin Type A of Toxin-Treated Spastic Equinus Children with Cerebral Palsy: A Randomized Clinical Trial Comparing Two Injection Schedules. J. Neuroimmunol. 2017, 306, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Atassi, M.Z.; Dolimbek, B.Z.; Jankovic, J.; Steward, L.E.; Aoki, K.R. Regions of Botulinum Neurotoxin A Light Chain Recognized by Human Anti-Toxin Antibodies from Cervical Dystonia Patients Immunoresistant to Toxin Treatment. The Antigenic Structure of the Active Toxin Recognized by Human Antibodies. Immunobiology 2011, 216, 782–792. [Google Scholar] [CrossRef] [PubMed]
- Baizabal-Carvallo, J.F.; Jankovic, J.; Feld, J. Flu-like Symptoms and Associated Immunological Response Following Therapy with Botulinum Toxins. Neurotox. Res. 2013, 24, 298–306. [Google Scholar] [CrossRef] [PubMed]
- Jankovic, J.; Schwartz, K. Response and Immunoresistance to Botulinum Toxin Injections. Neurology 1995, 45, 1743–1746. [Google Scholar] [CrossRef] [PubMed]
- Jinnah, H.A.; Goodmann, E.; Rosen, A.R.; Evatt, M.; Freeman, A.; Factor, S. Botulinum Toxin Treatment Failures in Cervical Dystonia: Causes, Management, and Outcomes. J. Neurol. 2016, 263, 1188–1194. [Google Scholar] [CrossRef] [PubMed]
- Brin, M.F.; Comella, C.L.; Jankovic, J.; Lai, F.; Naumann, M.; CD-017 BoNTA Study Group. Long-Term Treatment with Botulinum Toxin Type A in Cervical Dystonia Has Low Immunogenicity by Mouse Protection Assay. Mov. Disord. 2008, 23, 1353–1360. [Google Scholar] [CrossRef]
- Fabbri, M.; Leodori, G.; Fernandes, R.M.; Bhidayasiri, R.; Marti, M.J.; Colosimo, C.; Ferreira, J.J. Neutralizing Antibody and Botulinum Toxin Therapy: A Systematic Review and Meta-Analysis. Neurotox. Res. 2016, 29, 105–117. [Google Scholar] [CrossRef]
- Lange, O.; Bigalke, H.; Dengler, R.; Wegner, F.; DeGroot, M.; Wohlfarth, K. Neutralizing Antibodies and Secondary Therapy Failure after Treatment with Botulinum Toxin Type A: Much Ado about Nothing? Clin. Neuropharmacol. 2009, 32, 213–218. [Google Scholar] [CrossRef]
- Atassi, M.Z.; Dolimbek, B.Z.; Jankovic, J.; Steward, L.E.; Aoki, K.R. Molecular Recognition of Botulinum Neurotoxin B Heavy Chain by Human Antibodies from Cervical Dystonia Patients That Develop Immunoresistance to Toxin Treatment. Mol. Immunol. 2008, 45, 3878–3888. [Google Scholar] [CrossRef]
- Dressler, D.; Saberi, F.A. Safety of Botulinum Toxin Short Interval Therapy Using Incobotulinumtoxin A. J. Neural Transm. 2017, 124, 437–440. [Google Scholar] [CrossRef] [PubMed]
- Kessler, K.R.; Skutta, M.; Benecke, R.; German Dystonia Study Group. Long-Term Treatment of Cervical Dystonia with Botulinum Toxin A: Efficacy, Safety, and Antibody Frequency. J. Neurol. 1999, 246, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Dressler, D.; Bigalke, H. Immunological Aspects of Botulinum Toxin Therapy. Expert Rev. Neurother. 2017, 17, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Ojo, O.O.; Fernandez, H.H. Is It Time for Flexibility in Botulinum Inter-Injection Intervals? Toxicon 2015, 107, 72–76. [Google Scholar] [CrossRef] [PubMed]
- Sethi, K.D.; Rodriguez, R.; Olayinka, B. Satisfaction with Botulinum Toxin Treatment: A Cross-Sectional Survey of Patients with Cervical Dystonia. J. Med. Econ. 2012, 15, 419–423. [Google Scholar] [CrossRef] [PubMed]
- Evidente, V.G.H.; Fernandez, H.H.; LeDoux, M.S.; Brashear, A.; Grafe, S.; Hanschmann, A.; Comella, C.L. A Randomized, Double-Blind Study of Repeated IncobotulinumtoxinA (Xeomin(®)) in Cervical Dystonia. J. Neural Transm. 2013, 120, 1699–1707. [Google Scholar] [CrossRef]
- Truong, D.D.; Gollomp, S.M.; Jankovic, J.; LeWitt, P.A.; Marx, M.; Hanschmann, A.; Fernandez, H.H. Xeomin US Blepharospasm Study Group. Sustained Efficacy and Safety of Repeated IncobotulinumtoxinA (Xeomin(®)) Injections in Blepharospasm. J. Neural Transm. 2013, 120, 1345–1353. [Google Scholar] [CrossRef]
- Kukreja, R.V.; Singh, B.R. Comparative Role of Neurotoxin-Associated Proteins in the Structural Stability and Endopeptidase Activity of Botulinum Neurotoxin Complex Types A and E. Biochemistry 2007, 46, 14316–14324. [Google Scholar] [CrossRef]
- Dong, M.; Yeh, F.; Tepp, W.H.; Dean, C.; Johnson, E.A.; Janz, R.; Chapman, E.R. SV2 Is the Protein Receptor for Botulinum Neurotoxin A. Science 2006, 312, 592–596. [Google Scholar] [CrossRef]
- Pirazzini, M.; Rossetto, O.; Eleopra, R.; Montecucco, C. Botulinum Neurotoxins: Biology, Pharmacology, and Toxicology. Pharmacol. Rev. 2017, 69, 200–235. [Google Scholar] [CrossRef]
- Kukreja, R.; Chang, T.W.; Cai, S.; Lindo, P.; Riding, S.; Zhou, Y.; Ravichandran, E.; Singh, B.R. Immunological Characterization of the Subunits of Type A Botulinum Neurotoxin and Different Components of Its Associated Proteins. Toxicon 2009, 53, 616–624. [Google Scholar] [CrossRef]
- Frevert, J.; Dressler, D. Complexing Proteins in Botulinum Toxin Type A Drugs: A Help or a Hindrance? Biologics 2010, 4, 325–332. [Google Scholar] [CrossRef]
- Jankovic, J.; Truong, D.; Patel, A.T.; Brashear, A.; Evatt, M.; Rubio, R.G.; Oh, C.K.; Snyder, D.; Shears, G.; Comella, C. Injectable DaxibotulinumtoxinA in Cervical Dystonia: A Phase 2 Dose-Escalation Multicenter Study. Mov. Disord. Clin. Pract. 2018, 5, 273–282. [Google Scholar] [CrossRef]
- Dirk, D.; Mander, G.J.; Klaus, F. Equivalent Potency of Xeomin® and BOTOX®. Toxicon 2008, 51, 10. [Google Scholar] [CrossRef]
- Ranoux, D.; Gury, C.; Fondarai, J.; Mas, J.L.; Zuber, M. Respective Potencies of Botox and Dysport: A Double Blind, Randomised, Crossover Study in Cervical Dystonia. J. Neurol. Neurosurg. Psychiatry 2002, 72, 459–462. [Google Scholar] [CrossRef]
- Comella, C.L.; Jankovic, J.; Shannon, K.M.; Tsui, J.; Swenson, M.; Leurgans, S.; Fan, W.; Dystonia Study Group. Comparison of Botulinum Toxin Serotypes A and B for the Treatment of Cervical Dystonia. Neurology 2005, 65, 1423–1429. [Google Scholar] [CrossRef]
- Dressler, D.; Benecke, R. Autonomic Side Effects of Botulinum Toxin Type B Treatment of Cervical Dystonia and Hyperhidrosis. Eur. Neurol. 2003, 49, 34–38. [Google Scholar] [CrossRef]
- Carruthers, J.; Solish, N.; Humphrey, S.; Rosen, N.; Muhn, C.; Bertucci, V.; Swift, A.; Metelitsa, A.; Rubio, R.G.; Waugh, J.; et al. Injectable DaxibotulinumtoxinA for the Treatment of Glabellar Lines: A Phase 2, Randomized, Dose-Ranging, Double-Blind, Multicenter Comparison With OnabotulinumtoxinA and Placebo. Dermatol. Surg. 2017, 43, 1321–1331. [Google Scholar] [CrossRef]
- Oshima, M.; Deitiker, P.; Jankovic, J.; Atassi, M.Z. The Regions on the Light Chain of Botulinum Neurotoxin Type A Recognized by T Cells from Toxin-Treated Cervical Dystonia Patients. The Complete Human T-Cell Recognition Map of the Toxin Molecule. Immunol. Investig. 2018, 47, 18–39. [Google Scholar] [CrossRef]
- Sankhla, C.; Jankovic, J.; Duane, D. Variability of the Immunologic and Clinical Response in Dystonic Patients Immunoresistant to Botulinum Toxin Injections. Mov. Disord. 1998, 13, 150–154. [Google Scholar] [CrossRef]
- Dressler, D.; Bigalke, H. Botulinum Toxin Antibody Type A Titres after Cessation of Botulinum Toxin Therapy. Mov. Disord. 2002, 17, 170–173. [Google Scholar] [CrossRef]
- Dressler, D.; Pan, L.; Adib Saberi, F. Antibody-Induced Failure of Botulinum Toxin Therapy: Re-Start with Low-Antigenicity Drugs Offers a New Treatment Opportunity. J. Neural Transm. 2018, 125, 1481–1486. [Google Scholar] [CrossRef]
- Dressler, D.; Münchau, A.; Bhatia, K.P.; Quinn, N.P.; Bigalke, H. Antibody-Induced Botulinum Toxin Therapy Failure: Can It Be Overcome by Increased Botulinum Toxin Doses? Eur. Neurol. 2002, 47, 118–121. [Google Scholar] [CrossRef]
- Dressler, D.; Zettl, U.; Benecke, R.; Bigalke, H. Can Intravenous Immunoglobulin Improve Antibody-Mediated Botulinum Toxin Therapy Failure? Mov. Disord. 2000, 15, 1279–1281. [Google Scholar] [CrossRef]
- Dolimbek, B.Z.; Steward, L.E.; Aoki, K.R.; Atassi, M.Z. Location of the Synaptosome-Binding Regions on Botulinum Neurotoxin B. Biochemistry 2012, 51, 316–328. [Google Scholar] [CrossRef]
- Chen, R.; Karp, B.I.; Hallett, M. Botulinum Toxin Type F for Treatment of Dystonia: Long-Term Experience. Neurology 1998, 51, 1494–1496. [Google Scholar] [CrossRef]
- Joshi, S.G.; Elias, M.; Singh, A.; Al-Saleem, F.H.; Ancharski, D.; Nasser, Z.; Takahashi, T.; Simpson, L.L. Modulation of Botulinum Toxin-Induced Changes in Neuromuscular Function with Antibodies Directed against Recombinant Polypeptides or Fragments. Neuroscience 2011, 179, 208–222. [Google Scholar] [CrossRef]
- Yoon, S.; Kurnasov, O.; Natarajan, V.; Hong, M.; Gudkov, A.V.; Osterman, A.L.; Wilson, I.A. Structural Basis of TLR5-Flagellin Recognition and Signaling. Science 2012, 335, 859–864. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.C.; Yokota, K.; Arimitsu, H.; Hwang, H.J.; Sakaguchi, Y.; Cui, J.; Takeshi, K.; Watanabe, T.; Ohyama, T.; Oguma, K. Production of Anti-Neurotoxin Antibody Is Enhanced by Two Subcomponents, HA1 and HA3b, of Clostridium Botulinum Type B 16S Toxin-Haemagglutinin. Microbiology 2005, 151, 3739–3747. [Google Scholar] [CrossRef]
- Albrecht, P.; Jansen, A.; Lee, J.I.; Moll, M.; Ringelstein, M.; Rosenthal, D.; Bigalke, H.; Aktas, O.; Hartung, H.P.; Hefter, H. High Prevalence of Neutralizing Antibodies after Long-Term Botulinum Neurotoxin Therapy. Neurology 2019, 92, e48–e54. [Google Scholar] [CrossRef]
- Aoki, K.R.; Guyer, B. Botulinum Toxin Type A and Other Botulinum Toxin Serotypes: A Comparative Review of Biochemical and Pharmacological Actions. Eur. J. Neurol. 2001, 8 (Suppl. 5), 21–29. [Google Scholar] [CrossRef]
- Dressler, D.; Hallett, M. Immunological Aspects of Botox, Dysport and Myobloc/NeuroBloc. Eur. J. Neurol. 2006, 13 (Suppl. 1), 11–15. [Google Scholar] [CrossRef]
- Jankovic, J.; Vuong, K.D.; Ahsan, J. Comparison of Efficacy and Immunogenicity of Original versus Current Botulinum Toxin in Cervical Dystonia. Neurology 2003, 60, 1186–1188. [Google Scholar] [CrossRef]
- Callaway, J.E. Botulinum Toxin Type B (Myobloc): Pharmacology and Biochemistry. Clin. Dermatol. 2004, 22, 23–28. [Google Scholar] [CrossRef]
- Jankovic, J.; Hunter, C.; Dolimbek, B.Z.; Dolimbek, G.S.; Adler, C.H.; Brashear, A.; Comella, C.L.; Gordon, M.; Riley, D.E.; Sethi, K.; et al. Clinico-Immunologic Aspects of Botulinum Toxin Type B Treatment of Cervical Dystonia. Neurology 2006, 67, 2233–2235. [Google Scholar] [CrossRef]
- Gottlieb, S. Biosimilars: Policy, Clinical, and Regulatory Considerations. Am. J. Health. Syst. Pharm. 2008, 65, S2–S8. [Google Scholar] [CrossRef]
- Hanna, P.A.; Jankovic, J.; Vincent, A. Comparison of Mouse Bioassay and Immunoprecipitation Assay for Botulinum Toxin Antibodies. J. Neurol. Neurosurg. Psychiatry 1999, 66, 612–616. [Google Scholar] [CrossRef]
- Hanna, P.A.; Jankovic, J. Mouse Bioassay versus Western Blot Assay for Botulinum Toxin Antibodies: Correlation with Clinical Response. Neurology 1998. [Google Scholar] [CrossRef]
- Naumann, M.; Carruthers, A.; Carruthers, J.; Aurora, S.K.; Zafonte, R.; Abu-Shakra, S.; Boodhoo, T.; Miller-Messana, M.A.; Demos, G.; James, L.; et al. Meta-Analysis of Neutralizing Antibody Conversion with OnabotulinumtoxinA (BOTOX®) across Multiple Indications. Mov. Disord. 2010, 25, 2211–2218. [Google Scholar] [CrossRef]
- Dressler, D.; Dirnberger, G.; Bhatia, K.P.; Irmer, A.; Quinn, N.P.; Bigalke, H.; Marsden, C.D. Botulinum Toxin Antibody Testing: Comparison between the Mouse Protection Assay and the Mouse Lethality Assay. Mov. Disord. 2000, 15, 973–976. [Google Scholar] [CrossRef]
- Göschel, H.; Wohlfarth, K.; Frevert, J.; Dengler, R.; Bigalke, H. Botulinum A Toxin Therapy: Neutralizing and Nonneutralizing Antibodies—Therapeutic Consequences. Exp. Neurol. 1997, 147, 96–102. [Google Scholar] [CrossRef]
- Sesardic, D.; Jones, R.G.A.; Leung, T.; Alsop, T.; Tierney, R. Detection of Antibodies against Botulinum Toxins. Mov. Disord. 2004, 19, S85–S91. [Google Scholar] [CrossRef]
- Dressler, D.; Gessler, F.; Tacik, P.; Bigalke, H. An Enzyme-Linked Immunosorbent Assay for Detection of Botulinum Toxin-Antibodies. Mov. Disord. 2014, 29, 1322–1324. [Google Scholar] [CrossRef]
- Gordon, P.H.; Gooch, C.L.; Greene, P.E. Extensor Digitorum Brevis Test and Resistance to Botulinum Toxin Type A. Muscle Nerve 2002, 26, 828–831. [Google Scholar] [CrossRef]
- Cordivari, C.; Misra, V.P.; Vincent, A.; Catania, S.; Bhatia, K.P.; Lees, A.J. Secondary Nonresponsiveness to Botulinum Toxin A in Cervical Dystonia: The Role of Electromyogram-Guided Injections, Botulinum Toxin A Antibody Assay, and the Extensor Digitorum Brevis Test. Mov. Disord. 2006, 21, 1737–1741. [Google Scholar] [CrossRef]
- Dressler, D.; Bigalke, H.; Rothwell, J.C. The Sternocleidomastoid Test: An in Vivo Assay to Investigate Botulinum Toxin Antibody Formation in Humans. J. Neurol. 2000, 247, 630–632. [Google Scholar] [CrossRef]
- Voller, B.; Moraru, E.; Auff, E.; Benesch, M.; Poewe, W.; Wissel, J.; Müller, J.; Entner, T.; Bigalke, H.; Schnider, P. Ninhydrin Sweat Test: A Simple Method for Detecting Antibodies Neutralizing Botulinum Toxin Type A. Mov. Disord. 2004, 19, 943–947. [Google Scholar] [CrossRef]
- Kranz, G.S.; Sycha, T.; Voller, B.; Kranz, G.S.; Schnider, P.; Auff, E. Neutralizing Antibodies in Dystonic Patients Who Still Respond Well to Botulinum Toxin Type A. Neurology 2008, 70, 133–136. [Google Scholar] [CrossRef]
- Elovic, E.P.; Brashear, A.; Kaelin, D.; Liu, J.; Millis, S.R.; Barron, R.; Turkel, C. Repeated Treatments with Botulinum Toxin Type a Produce Sustained Decreases in the Limitations Associated with Focal Upper-Limb Poststroke Spasticity for Caregivers and Patients. Arch. Phys. Med. Rehabil. 2008, 89, 799–806. [Google Scholar] [CrossRef]
- Bakheit, A.M.O.; Fedorova, N.V.; Skoromets, A.A.; Timerbaeva, S.L.; Bhakta, B.B.; Coxon, L. The Beneficial Antispasticity Effect of Botulinum Toxin Type A Is Maintained after Repeated Treatment Cycles. J. Neurol. Neurosurg. Psychiatry 2004, 75, 1558–1561. [Google Scholar] [CrossRef]
- Wissel, J.; Bensmail, D.; Ferreira, J.J.; Molteni, F.; Satkunam, L.; Moraleda, S.; Rekand, T.; McGuire, J.; Scheschonka, A.; Flatau-Baqué, B.; et al. Safety and Efficacy of IncobotulinumtoxinA Doses up to 800 U in Limb Spasticity: The TOWER Study. Neurology 2017, 88, 1321–1328. [Google Scholar] [CrossRef]
- Cruz, F.; Herschorn, S.; Aliotta, P.; Brin, M.; Thompson, C.; Lam, W.; Daniell, G.; Heesakkers, J.; Haag-Molkenteller, C. Efficacy and Safety of OnabotulinumtoxinA in Patients with Urinary Incontinence Due to Neurogenic Detrusor Overactivity: A Randomised, Double-Blind, Placebo-Controlled Trial. Eur. Urol. 2011, 60, 742–750. [Google Scholar] [CrossRef]
- Schulte-Baukloh, H.; Bigalke, H.; Heine, G.; Pape, D.; Stuerzebecher, B.; Miller, K.; Knispel, H.H. Antibodies against Botulinum Neurotoxin Type A as a Cause of Treatment Failure after the First Detrusor Injection. Urology 2007, 69, 575.e13–575.e15. [Google Scholar] [CrossRef]
- Schulte-Baukloh, H.; Bigalke, H.; Miller, K.; Heine, G.; Pape, D.; Lehmann, J.; Knispel, H.H. Botulinum Neurotoxin Type A in Urology: Antibodies as a Cause of Therapy Failure. Int. J. Urol. 2008, 15, 407–415, discussion 415. [Google Scholar] [CrossRef]
- Kawashima, M.; Harii, K. An Open-Label, Randomized, 64-Week Study Repeating 10- and 20-U Doses of Botulinum Toxin Type A for Treatment of Glabellar Lines in Japanese Subjects. Int. J. Dermatol. 2009, 48, 768–776. [Google Scholar] [CrossRef]
- DYSPORT® [Package Insert]; Ipsen Biopharmaceuticals, Inc.: Basking Ridge, NJ, USA, 2016.
- Monheit, G.D.; Cohen, J.L.; Reloxin Investigational Group. Long-Term Safety of Repeated Administrations of a New Formulation of Botulinum Toxin Type A in the Treatment of Glabellar Lines: Interim Analysis from an Open-Label Extension Study. J. Am. Acad. Dermatol. 2009, 61, 421–425. [Google Scholar] [CrossRef]
- Moy, R.; Maas, C.; Monheit, G.; Huber, M.B.; Reloxin Investigational Group. Long-Term Safety and Efficacy of a New Botulinum Toxin Type A in Treating Glabellar Lines. Arch. Facial Plast. Surg. 2009, 11, 77–83. [Google Scholar] [CrossRef]
- Imhof, M.; Kühne, U. A Phase III Study of IncobotulinumtoxinA in the Treatment of Glabellar Frown Lines. J. Clin. Aesthet. Dermatol. 2011, 4, 28–34. [Google Scholar]
- Glaser, D.A.; Pariser, D.M.; Hebert, A.A.; Landells, I.; Somogyi, C.; Weng, E.; Brin, M.F.; Beddingfield, F. A Prospective, Nonrandomized, Open-Label Study of the Efficacy and Safety of OnabotulinumtoxinA in Adolescents with Primary Axillary Hyperhidrosis. Pediatr. Dermatol. 2015, 32, 609–617. [Google Scholar] [CrossRef]
- Lacroix-Desmazes, S.; Mouly, S.; Popoff, M.R.; Colosimo, C. Systematic Analysis of Botulinum Neurotoxin Type A Immunogenicity in Clinical Studies. Basal Ganglia 2017, 9, 12–17. [Google Scholar] [CrossRef]
- Truong, D.; Brodsky, M.; Lew, M.; Brashear, A.; Jankovic, J.; Molho, E.; Orlova, O.; Timerbaeva, S.; Global Dysport Cervical Dystonia Study Group. Long-Term Efficacy and Safety of Botulinum Toxin Type A (Dysport) in Cervical Dystonia. Parkinsonism Relat. Disord. 2010, 16, 316–323. [Google Scholar] [CrossRef]
- XEOMIN® [Package Insert]; Merz Pharmaceuticals: Raleigh, NC, USA, 2018.
- MYOBLOC® [Package Insert]; Solstice Neurosciences, Inc.: San Fransisco, CA, USA, 2009.
- Coleman, C.; Hubble, J.; Schwab, J.; Beffy, J.L.; Picaut, P.; Morte, C. Immunoresistance in Cervical Dystonia Patients after Treatment with AbobotulinumtoxinA. Int. J. Neurosci. 2012, 122, 358–362. [Google Scholar] [CrossRef]
- Haussermann, P.; Marczoch, S.; Klinger, C.; Landgrebe, M.; Conrad, B.; Ceballos-Baumann, A. Long-Term Follow-up of Cervical Dystonia Patients Treated with Botulinum Toxin A. Mov. Disord. 2004, 19, 303–308. [Google Scholar] [CrossRef]
- Field, M.; Splevins, A.; Picaut, P.; van der Schans, M.; Langenberg, J.; Noort, D.; Snyder, D.; Foster, K. AbobotulinumtoxinA (Dysport®), OnabotulinumtoxinA (Botox®), and IncobotulinumtoxinA (Xeomin®) Neurotoxin Content and Potential Implications for Duration of Response in Patients. Toxins (Basel) 2018, 10, 535. [Google Scholar] [CrossRef]
- Chinnapongse, R.B.; Lew, M.F.; Ferreira, J.J.; Gullo, K.L.; Nemeth, P.R.; Zhang, Y. Immunogenicity and Long-Term Efficacy of Botulinum Toxin Type B in the Treatment of Cervical Dystonia: Report of 4 Prospective, Multicenter Trials. Clin. Neuropharmacol. 2012, 35, 215–223. [Google Scholar] [CrossRef]
- Lamb, Y.N.; Scott, L.J. IncobotulinumtoxinA: A Review in Upper Limb Spasticity. Drugs 2016, 76, 1373–1379. [Google Scholar] [CrossRef]
- Evidente, V.G.H.; Truong, D.; Jankovic, J.; Comella, C.L.; Grafe, S.; Hanschmann, A. IncobotulinumtoxinA (Xeomin®) Injected for Blepharospasm or Cervical Dystonia According to Patient Needs Is Well Tolerated. J. Neurol. Sci. 2014, 346, 116–120. [Google Scholar] [CrossRef]
- Dressler, D.; Paus, S.; Seitzinger, A.; Gebhardt, B.; Kupsch, A. Long-Term Efficacy and Safety of IncobotulinumtoxinA Injections in Patients with Cervical Dystonia. J. Neurol. Neurosurg. Psychiatry 2013, 84, 1014–1019. [Google Scholar] [CrossRef]
- Hefter, H.; Spiess, C.; Rosenthal, D. Very Early Reduction in Efficacy of Botulinum Toxin Therapy for Cervical Dystonia in Patients with Subsequent Secondary Treatment Failure: A Retrospective Analysis. J. Neural Transm. 2014, 121, 513–519. [Google Scholar] [CrossRef]
- Hefter, H.; Rosenthal, D.; Moll, M. High Botulinum Toxin-Neutralizing Antibody Prevalence Under Long-Term Cervical Dystonia Treatment. Mov. Disord. Clin. Pract. 2016, 3, 500–506. [Google Scholar] [CrossRef] [Green Version]
- Mejia, N.I.; Vuong, K.D.; Jankovic, J. Long-Term Botulinum Toxin Efficacy, Safety, and Immunogenicity. Mov. Disord. 2005, 20, 592–597. [Google Scholar] [CrossRef]
- Charles, D.; Brashear, A.; Hauser, R.A.; Li, H.I.; Boo, L.M.; Brin, M.F.; CD 140 Study Group. Efficacy, Tolerability, and Immunogenicity of Onabotulinumtoxina in a Randomized, Double-Blind, Placebo-Controlled Trial for Cervical Dystonia. Clin. Neuropharmacol. 2012, 35, 208–214. [Google Scholar] [CrossRef]


| Mouse Protection Assay (MPA) |
| Mouse Hemidiaphragm Assay (MHDA) |
| Immunoprecipitation Assay (IPA) |
| Western Blot Assay (WBA) |
| Synaptosome Inhibition Assay (SIA) |
| Enzyme-Linked Immunosorbent Assay (ELISA) |
| Sternocleidomastoid test (SCM) |
| Electrical stimulation of injected muscle (EDB) |
| Other assays (e.g., sudomotor, ninhydrin sweat test) |
| Clinical tests (UBI, FTAT) |
| Test Name | Injection Site | Required Tools | Clinically Responsive Result |
|---|---|---|---|
| UBI | Medial eyebrow | None | Asymmetric frowning |
| FTAT | Frontalis | None | Asymmetric forehead wrinkling |
| EDB | Extensor digitorum brevis | EMG | >50% decrease in EDB CMAP |
| SCM | Sternocleidomastoid | EMG | Maximal contraction reduction % >2 SD below mean control reduction % |
| NST | Hypothenar eminence | Ninhydrin solution | Decreased anhidrotic area |
| BoNT Formulation | Trade Names | FDA-Approved Indications | Estimated Equivalent Dose (to ONA) | Immunogenicity Ranges | Notes |
|---|---|---|---|---|---|
| Ona (OLD) | Botox® | Not in use | 1 | 5–17% [18] | |
| Ona (New) | Botox® | CD, AH, BSP, ULS, OAB, CM, strabismus [8] | 1 | 0.2% [60]–3.6% [82] | Reduced amounts of inactive protein compared to older formulation |
| Abo | Dysport® | CD, GL, ULS (adults), LLS (children) [77] | 2.5 | 0.9% [83]–3.6% [77] | |
| Inco | Xeomin® | CD, BSP, GL, USL, sialorrhea [84] | 1 | 0% [51]–0.5% [19] | NAPs removed |
| Rima | Myobloc® (USA), NeuroBloc® | CD [85] | 50 | 18% [85]–42.4% [19] | B serotype, stronger autonomic effects |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bellows, S.; Jankovic, J. Immunogenicity Associated with Botulinum Toxin Treatment. Toxins 2019, 11, 491. https://0-doi-org.brum.beds.ac.uk/10.3390/toxins11090491
Bellows S, Jankovic J. Immunogenicity Associated with Botulinum Toxin Treatment. Toxins. 2019; 11(9):491. https://0-doi-org.brum.beds.ac.uk/10.3390/toxins11090491
Chicago/Turabian StyleBellows, Steven, and Joseph Jankovic. 2019. "Immunogenicity Associated with Botulinum Toxin Treatment" Toxins 11, no. 9: 491. https://0-doi-org.brum.beds.ac.uk/10.3390/toxins11090491




