Biological Activity of Berberine—A Summary Update
Abstract
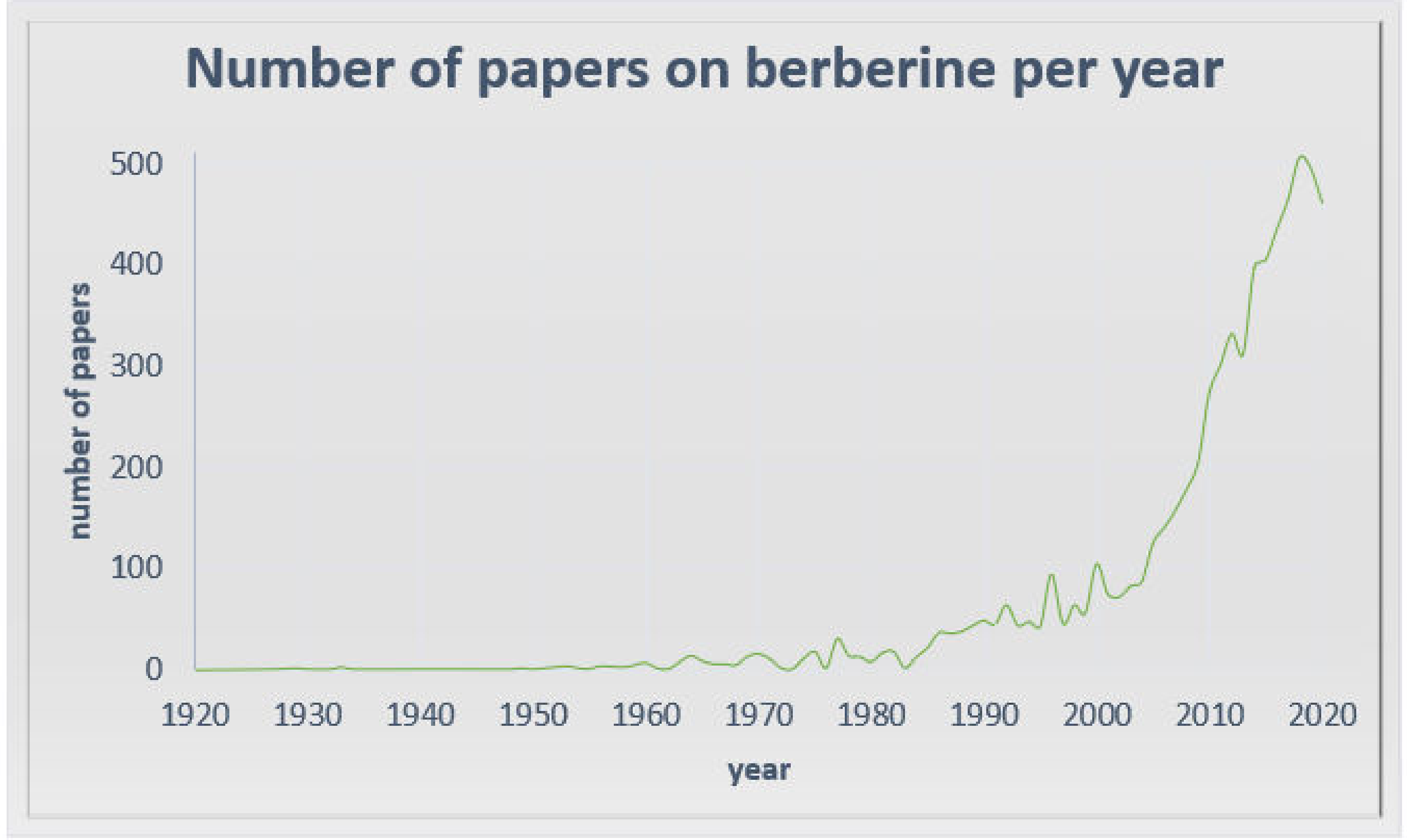
:1. Introduction
2. Berberine in Cardiovascular and Metabolic Diseases
2.1. Cholesterol-Lowering Effect
2.2. Antidiabetic Action
2.3. Antiobesity Action
3. Berberine in Neurodegenerative and Neuropsychiatric Disorders
4. Anticancer Activity of Berberine
4.1. Cell Cycle Arrest
4.2. Apoptosis Induction
4.3. Influence on MAPK
4.4. Trancription Regulation
4.5. Inhibition of Metastasis
4.6. Inhibition of Angiogenesis
4.7. Inhibition of Epithelial-To-Mesenchymal Transition
4.8. Anti-Inflammatory Activity
4.9. β-Catenin Expression
4.10. Inhibition of Carcinogenesis Combined with Metabolism of Lipids
5. Supportive Action of Berberine—Sensitization and Drug Resistance
6. Preventive Action of Berberine
7. Challenge to New Derivatives and Formulations of Berberine
8. Berberine in Clinical Trials
9. Summary
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Feng, X.; Sureda, A.; Jafari, S.; Memariani, Z.; Tewari, D.; Annunziata, G.; Barrea, L.; Hassan, S.T.S.; Šmejkal, K.; Malaník, M.; et al. Berberine in Cardiovascular and Metabolic Diseases: From Mechanisms to Therapeutics. Theranostics 2019, 9, 1923–1951. [Google Scholar] [CrossRef]
- Wang, Y.; Zidichouski, J.A. Update on the Benefits and Mechanisms of Action of the Bioactive Vegetal Alkaloid Berberine on Lipid Metabolism and Homeostasis. Cholesterol 2018, 2018, 7173920. [Google Scholar] [CrossRef]
- Fan, J.; Zhang, K.; Jin, Y.; Li, B.; Gao, S.; Zhu, J.; Cui, R. Pharmacological effects of berberine on mood disorders. J. Cell. Mol. Med. 2019, 23, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Zeng, X.-H.; Zeng, X.-J.; Li, Y.-Y. Efficacy and safety of berberine for congestive heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am. J. Cardiol. 2003, 92, 173–176. [Google Scholar] [CrossRef]
- Barrios, V.; Escobar, C.; Cicero, A.F.G.; Burke, D.; Fasching, P.; Banach, M.; Bruckert, E. A nutraceutical approach (Armolipid Plus) to reduce total and LDL cholesterol in individuals with mild to moderate dyslipidemia: Review of the clinical evidence. Atheroscler. Suppl. 2017, 24, 1–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, X.-Y.; Zhao, Z.-X.; Huang, M.; Feng, R.; He, C.-Y.; Ma, C.; Luo, S.-H.; Fu, J.; Wen, B.-Y.; Ren, L.; et al. Effect of Berberine on promoting the excretion of cholesterol in high-fat diet-induced hyperlipidemic hamsters. J. Transl. Med. 2015, 13, 278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brusq, J.-M.; Ancellin, N.; Grondin, P.; Guillard, R.; Martin, S.; Saintillan, Y.; Issandou, M. Inhibition of lipid synthesis through activation of AMP kinase: An additional mechanism for the hypolipidemic effects of berberine. J. Lipid Res. 2006, 47, 1281–1288. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.; Peng, L.; Wei, G.; Ge, H. Therapeutic Effects of Berberine Capsule on Patients with Mild Hyperlipidemia. Zhongguo Zhong Xi Yi Jie He Za Zhi Zhongguo Zhongxiyi Jiehe Zazhi Chin. J. Integr. Tradit. West. Med. 2016, 36, 681–684. [Google Scholar]
- Wang, H.; Zhu, C.; Ying, Y.; Luo, L.; Huang, D.; Luo, Z. Metformin and berberine, two versatile drugs in treatment of common metabolic diseases. Oncotarget 2017, 9, 10135–10146. [Google Scholar] [CrossRef] [Green Version]
- An, Y.; Sun, Z.; Zhang, Y.; Liu, B.; Guan, Y.; Lu, M. The use of berberine for women with polycystic ovary syndrome undergoing IVF treatment. Clin. Endocrinol. 2014, 80, 425–431. [Google Scholar] [CrossRef]
- Li, C.; Guan, X.-M.; Wang, R.-Y.; Xie, Y.-S.; Zhou, H.; Ni, W.-J.; Tang, L.-Q. Berberine mitigates high glucose-induced podocyte apoptosis by modulating autophagy via the mTOR/P70S6K/4EBP1 pathway. Life Sci. 2020, 243, 117277. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Kuang, H.; Shen, W.; Ma, H.; Zhang, Y.; Stener-Victorin, E.; Hung, E.; Ng, Y.; Liu, J.; Kuang, H.; et al. Letrozole, berberine, or their combination for anovulatory infertility in women with polycystic ovary syndrome: Study design of a double-blind randomised controlled trial. BMJ Open 2013, 3, e003934. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, M.-F.; Zhou, X.-M.; Li, X.-L. The Effect of Berberine on Polycystic Ovary Syndrome Patients with Insulin Resistance (PCOS-IR): A Meta-Analysis and Systematic Review. Evid. Based Complement. Altern. Med. 2018, 2018, 2532935. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, X.-K.; Wang, Y.-Y.; Liu, J.-P.; Hou, L.-H.; Gao, Y.-Q.; Du, S.-M.; Yan, Y.; Zhang, J.-F.; Xue, H.-Y.; Li, W.-L.; et al. Letrozole, berberine, or a combination for infertility in Chinese women with polycystic ovary syndrome: A multicentre, randomised, double-blind, placebo-controlled trial. Lancet 2015, 386, S70. [Google Scholar] [CrossRef] [Green Version]
- Cicero, A.F.G.; Reggi, A.; Parini, A.; Morbini, M.; Rosticci, M.; Grandi, E.; Borghi, C. Berberine and Monacolin Effects on the Cardiovascular Risk Profile of Women with Oestroprogestin-Induced Hypercholesterolemia. High Blood Press. Cardiovasc. Prev. 2014, 21, 221–226. [Google Scholar] [CrossRef]
- Hu, X.; Zhang, Y.; Xue, Y.; Zhang, Z.; Wang, J. Berberine is a potential therapeutic agent for metabolic syndrome via brown adipose tissue activation and metabolism regulation. Am. J. Transl. Res. 2018, 10, 3322–3329. [Google Scholar]
- Kumar, R.; Awasthi, M.; Sharma, A.; Padwad, Y.; Sharma, R. Berberine induces dose-dependent quiescence and apoptosis in A549 cancer cells by modulating cell cyclins and inflammation independent of mTOR pathway. Life Sci. 2020, 244, 117346. [Google Scholar] [CrossRef]
- Bogoyevitch, M.A.; Boehm, I.; Oakley, A.; Ketterman, A.J.; Barr, R.K. Targeting the JNK MAPK cascade for inhibition: Basic science and therapeutic potential. Biochim. Biophys. Acta 2004, 1697, 89–101. [Google Scholar] [CrossRef]
- Li, H.-L.; Wu, H.; Zhang, B.-B.; Shi, H.-L.; Wu, X.-J. MAPK pathways are involved in the inhibitory effect of berberine hydrochloride on gastric cancer MGC 803 cell proliferation and IL-8 secretion in vitro and in vivo. Mol. Med. Rep. 2016, 14, 1430–1438. [Google Scholar] [CrossRef]
- Zheng, F.; Tang, Q.; Wu, J.; Zhao, S.; Liang, Z.; Li, L.; Wu, W.; Hann, S. p38α MAPK-mediated induction and interaction of FOXO3a and p53 contribute to the inhibited-growth and induced-apoptosis of human lung adenocarcinoma cells by berberine. J. Exp. Clin. Cancer Res. 2014, 33, 36. [Google Scholar] [CrossRef] [Green Version]
- Chen, Q.; Shi, J.; Ding, Z.; Xia, Q.; Zheng, T.; Ren, Y.; Li, M.; Fan, L. Berberine induces apoptosis in non-small-cell lung cancer cells by upregulating miR-19a targeting tissue factor. Cancer Manag. Res. 2019, 11, 9005–9015. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhou, M.; Shang, D. Berberine inhibits human gastric cancer cell growth via deactivation of p38/JNK pathway, induction of mitochondrial-mediated apoptosis, caspase activation and NF-κB inhibition. J. BUON Off. J. Balk. Union Oncol. 2020, 25, 314–318. [Google Scholar]
- Lin, X.; Zhang, N. Berberine: Pathways to protect neurons. Phytother. Res. 2018, 32, 1501–1510. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.; Sharma, B. Toxicological Effects of Berberine and Sanguinarine. Front. Mol. Biosci. 2018, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kulkarni, S.K.; Dhir, A. Berberine: A plant alkaloid with therapeutic potential for central nervous system disorders. Phytother. Res. 2010, 24, 317–324. [Google Scholar] [CrossRef]
- Ahmed, T.; Gilani, A.-H.; Abdollahi, M.; Daglia, M.; Nabavi, S.F.; Nabavi, S.M. Berberine and neurodegeneration: A review of literature. Pharmacol. Rep. 2015, 67, 970–979. [Google Scholar] [CrossRef]
- Song, B.; Tang, X.; Wang, X.; Huang, X.; Ye, Y.; Lu, X.; Wei, X.; Zeng, Y. Bererine induces peripheral lymphocytes immune regulations to realize its neuroprotective effects in the cerebral ischemia/reperfusion mice. Cell. Immunol. 2012, 276, 91–100. [Google Scholar] [CrossRef]
- Kysenius, K.; Brunello, C.A.; Huttunen, H.J. Mitochondria and NMDA Receptor-Dependent Toxicity of Berberine Sensitizes Neurons to Glutamate and Rotenone Injury. PLoS ONE 2014, 9, e107129. [Google Scholar] [CrossRef]
- Ayati, S.H.; Fazeli, B.; Momtazi-borojeni, A.A.; Cicero, A.F.G.; Pirro, M.; Sahebkar, A. Regulatory effects of berberine on microRNome in Cancer and other conditions. Crit. Rev. Oncol. Hematol. 2017, 116, 147–158. [Google Scholar] [CrossRef]
- Imenshahidi, M.; Hosseinzadeh, H. Berberis Vulgaris and Berberine: An Update Review. Phytother. Res. 2016, 30, 1745–1764. [Google Scholar] [CrossRef]
- Lee, B.; Yang, C.H.; Hahm, D.-H.; Choe, E.S.; Lee, H.-J.; Pyun, K.-H.; Shim, I. Inhibitory Effects of Coptidis rhizoma and Berberine on Cocaine-Induced Sensitization. eCAM 2009, 6, 85–90. [Google Scholar] [PubMed] [Green Version]
- Wang, M.X.; Huo, L.M.; Yang, H.C.; Gao, Y.J. An experimental study on the photodynamic activity of berberine in vitro on cancer cells. J. Tradit. Chin. Med. Chung Tsa Chih Ying Wen Pan 1986, 6, 125–127. [Google Scholar]
- Lin, C.-C.; Kao, S.-T.; Chen, G.-W.; Ho, H.-C.; Chung, J.-G. Apoptosis of Human Leukemia HL-60 Cells and Murine Leukemia WEHI-3 Cells Induced by Berberine through the Activation of Caspase-3. Anticancer Res. 2006, 26, 227–242. [Google Scholar] [PubMed]
- Och, A.; Zalewski, D.; Komsta, Ł.; Kołodziej, P.; Kocki, J.; Bogucka-Kocka, A. Cytotoxic and Proapoptotic Activity of Sanguinarine, Berberine, and Extracts of Chelidonium majus L. and Berberis thunbergii DC. toward Hematopoietic Cancer Cell Lines. Toxins 2019, 11, 485. [Google Scholar] [CrossRef] [Green Version]
- Jantová, S.; Čipák, L.; Čerňáková, M.; Košt‘álová, D. Effect of berberine on proliferation, cell cycle and apoptosis in HeLa and L1210 cells. J. Pharm. Pharmacol. 2003, 55, 1143–1149. [Google Scholar] [CrossRef]
- Kettmann, V.; Košťálová, D.; Jantová, S.; Čerňáková, M.; DřímalInstitute of Experimental Pharmacology, Slovak Academy of Sciences, J. In vitro cytotoxicity of berberine against HeLa and L1210 cancer cell lines. Pharm. Int. J. Pharm. Sci. 2004, 59, 548–551. [Google Scholar]
- Yu, F.-S.; Yang, J.-S.; Lin, H.-J.; Yu, C.-S.; Tan, T.-W.; Lin, Y.-T.; Lin, C.-C.; Lu, H.-F.; Chung, J.-G. Berberine Inhibits WEHI-3 Leukemia Cells In Vivo. In Vivo 2007, 21, 407–412. [Google Scholar]
- Pazhang, Y.; Ahmadian, S.; Mahmoudian, M.; Shafiezadeh, M. Berberine-induced apoptosis via decreasing the survivin protein in K562 cell line. Med. Oncol. 2011, 28, 1577–1583. [Google Scholar] [CrossRef]
- Lin, J.G.; Chung, J.G.; Wu, L.T.; Chen, G.W.; Chang, H.L.; Wang, T.F. Effects of Berberine on Arylamine N-Acetyltransferase Activity in Human Colon Tumor Cells. Am. J. Chin. Med. 1999, 27, 265–275. [Google Scholar] [CrossRef]
- Tai, W.; Luo, H. The inhibit effect of berberine on human colon cell line cyclooxygenase-2. Zhonghua Nei Ke Za Zhi 2003, 42, 558–560. [Google Scholar]
- Chung, J.G.; Wu, L.T.; Chu, C.B.; Jan, J.Y.; Ho, C.C.; Tsou, M.F.; Lu, H.F.; Chen, G.W.; Lin, J.G.; Wang, T.F. Effects of berberine on arylamine N-acetyltransferase activity in human bladder tumour cells. Food Chem. Toxicol. 1999, 37, 319–326. [Google Scholar] [CrossRef]
- Liu, Y.; Yu, H.; Zhang, C.; Cheng, Y.; Hu, L.; Meng, X.; Zhao, Y. Protective effects of berberine on radiation-induced lung injury via intercellular adhesion molecular-1 and transforming growth factor-beta-1 in patients with lung cancer. Eur. J. Cancer 2008, 44, 2425–2432. [Google Scholar] [CrossRef] [PubMed]
- Noriyasu, M.; Murakami, K.; Yamaura, T.; Ikeda, T.; Saiki, I. Inhibitory effect of berberine on the mediastinal lymph node metastasis produced by orthotopic implantation of Lewis lung carcinoma. Cancer Lett. 2001, 165, 35–42. [Google Scholar]
- Wang, D.Y.; Yeh, C.C.; Lee, J.H.; Hung, C.F.; Chung, J.G. Berberine Inhibited Arylamine N-Acetyltransferase Activity and Gene Expression and DNA Adduct Formation in Human Malignant Astrocytoma (G9T/VGH) and Brain Glioblastoma Multiforms (GBM 8401) Cells. Neurochem. Res. 2002, 27, 883–889. [Google Scholar] [CrossRef] [PubMed]
- Letašiová, S.; Jantová, S.; Čipák, L.; Múčková, M. Berberine—Antiproliferative activity in vitro and induction of apoptosis/necrosis of the U937 and B16 cells. Cancer Lett. 2006, 239, 254–262. [Google Scholar] [CrossRef]
- Palmieri, A.; Scapoli, L.; Iapichino, A.; Mercolini, L.; Mandrone, M.; Poli, F.; Giannì, A.B.; Baserga, C.; Martinelli, M. Berberine and Tinospora cordifolia exert a potential anticancer effect on colon cancer cells by acting on specific pathways. Int. J. Immunopathol. Pharmacol. 2019, 33. [Google Scholar] [CrossRef] [Green Version]
- Liu, D.; Meng, X.; Wu, D.; Qiu, Z.; Luo, H. A Natural Isoquinoline Alkaloid With Antitumor Activity: Studies of the Biological Activities of Berberine. Front. Pharmacol. 2019, 10. [Google Scholar] [CrossRef] [Green Version]
- Yang, M.; Yang, Y.; Cui, H.; Guan, Z.; Yang, Y.; Zhang, H.; Chen, X.; Zhu, H.; Yang, X.; Cai, J.; et al. The Natural Compound Gambogic Acid Radiosensitizes Nasopharyngeal Carcinoma Cells under Hypoxic Conditions. Tumori J. 2016, 102, 135–143. [Google Scholar] [CrossRef]
- Li, L.; Wang, X.; Sharvan, R.; Gao, J.; Qu, S. Berberine could inhibit thyroid carcinoma cells by inducing mitochondrial apoptosis, G0/G1 cell cycle arrest and suppressing migration via PI3K-AKT and MAPK signaling pathways. Biomed. Pharmacother. 2017, 95, 1225–1231. [Google Scholar] [CrossRef]
- Yan, K.; Zhang, C.; Feng, J.; Hou, L.; Yan, L.; Zhou, Z.; Liu, Z.; Liu, C.; Fan, Y.; Zheng, B.; et al. Induction of G1 cell cycle arrest and apoptosis by berberine in bladder cancer cells. Eur. J. Pharmacol. 2011, 661, 1–7. [Google Scholar] [CrossRef]
- Gong, C.; Hu, X.; Xu, Y.; Yang, J.; Zong, L.; Wang, C.; Zhu, J.; Li, Z.; Lu, D. Berberine inhibits proliferation and migration of colorectal cancer cells by downregulation of GRP78. Anticancer. Drugs 2020, 31, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Dai, W.; Mu, L.; Cui, Y.; Li, Y.; Chen, P.; Xie, H.; Wang, X. Long non-coding RNA CASC2 enhances berberine-induced cytotoxicity in colorectal cancer cells by silencing BCL2. Mol. Med. Rep. 2019, 20, 995–1006. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Y.; Hua, W.; Li, Y.; Xian, X.; Zhao, Z.; Liu, C.; Zou, J.; Li, J.; Fang, X.; Zhu, Y. Berberine suppresses colon cancer cell proliferation by inhibiting the SCAP/SREBP-1 signaling pathway-mediated lipogenesis. Biochem. Pharmacol. 2020, 174, 113776. [Google Scholar] [CrossRef] [PubMed]
- Farooqi, A.A.; Qureshi, M.Z.; Khalid, S.; Attar, R.; Martinelli, C.; Sabitaliyevich, U.Y.; Nurmurzayevich, S.B.; Taverna, S.; Poltronieri, P.; Xu, B. Regulation of Cell Signaling Pathways by Berberine in Different Cancers: Searching for Missing Pieces of an Incomplete Jig-Saw Puzzle for an Effective Cancer Therapy. Cancers 2019, 11, 478. [Google Scholar] [CrossRef] [Green Version]
- Hu, X.; Wu, X.; Huang, Y.; Tong, Q.; Takeda, S.; Qing, Y. Berberine induces double-strand DNA breaks in Rev3 deficient cells. Mol. Med. Rep. 2014, 9, 1883–1888. [Google Scholar] [CrossRef] [Green Version]
- Chidambara Murthy, K.N.; Jayaprakasha, G.K.; Patil, B.S. The natural alkaloid berberine targets multiple pathways to induce cell death in cultured human colon cancer cells. Eur. J. Pharmacol. 2012, 688, 14–21. [Google Scholar] [CrossRef]
- Kalaiarasi, A.; Anusha, C.; Sankar, R.; Rajasekaran, S.; John Marshal, J.; Muthusamy, K.; Ravikumar, V. Plant Isoquinoline Alkaloid Berberine Exhibits Chromatin Remodeling by Modulation of Histone Deacetylase To Induce Growth Arrest and Apoptosis in the A549 Cell Line. J. Agric. Food Chem. 2016, 64, 9542–9550. [Google Scholar] [CrossRef]
- Su, Y.-H.; Tang, W.-C.; Cheng, Y.-W.; Sia, P.; Huang, C.-C.; Lee, Y.-C.; Jiang, H.-Y.; Wu, M.-H.; Lai, I.-L.; Lee, J.-W.; et al. Targeting of multiple oncogenic signaling pathways by Hsp90 inhibitor alone or in combination with berberine for treatment of colorectal cancer. Biochim. Biophys. Acta BBA Mol. Cell Res. 2015, 1853, 2261–2272. [Google Scholar] [CrossRef] [Green Version]
- Sanna, L.; Marchesi, I.; Melone, M.A.B.; Bagella, L. The role of enhancer of zeste homolog 2: From viral epigenetics to the carcinogenesis of hepatocellular carcinoma. J. Cell. Physiol. 2018, 233, 6508–6517. [Google Scholar] [CrossRef]
- Refaat, A.; Abdelhamed, S.; Yagita, H.; Inoue, H.; Yokoyama, S.; Hayakawa, Y.; Saiki, I. Berberine enhances tumor necrosis factor-related apoptosis-inducing ligand-mediated apoptosis in breast cancer. Oncol. Lett. 2013, 6, 840–844. [Google Scholar] [CrossRef] [Green Version]
- Hsu, W.-H.; Hsieh, Y.-S.; Kuo, H.-C.; Teng, C.-Y.; Huang, H.-I.; Wang, C.-J.; Yang, S.-F.; Liou, Y.-S.; Kuo, W.-H. Berberine induces apoptosis in SW620 human colonic carcinoma cells through generation of reactive oxygen species and activation of JNK/p38 MAPK and FasL. Arch. Toxicol. 2007, 81, 719–728. [Google Scholar] [CrossRef] [PubMed]
- Lu, B.; Hu, M.; Liu, K.; Peng, J. Cytotoxicity of berberine on human cervical carcinoma HeLa cells through mitochondria, death receptor and MAPK pathways, and in-silico drug-target prediction. Toxicol. Vitr. 2010, 24, 1482–1490. [Google Scholar] [CrossRef] [PubMed]
- Zarubin, T.; Han, J. Activation and signaling of the p38 MAP kinase pathway. Cell Res. 2005, 15, 11–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Renault, V.M.; Thekkat, P.U.; Hoang, K.L.; White, J.L.; Brady, C.A.; Kenzelmann Broz, D.; Venturelli, O.S.; Johnson, T.M.; Oskoui, P.R.; Xuan, Z.; et al. The pro-longevity gene FoxO3 is a direct target of the p53 tumor suppressor. Oncogene 2011, 30, 3207–3221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Macleod, K.F.; Sherry, N.; Hannon, G.; Beach, D.; Tokino, T.; Kinzler, K.; Vogelstein, B.; Jacks, T. p53-dependent and independent expression of p21 during cell growth, differentiation, and DNA damage. Genes Dev. 1995, 9, 935–944. [Google Scholar] [CrossRef] [Green Version]
- Hauck, L.; Harms, C.; Grothe, D.; An, J.; Gertz, K.; Kronenberg, G.; Dietz, R.; Endres, M.; von Harsdorf, R. Critical Role for FoxO3a-Dependent Regulation of p21CIP1/WAF1 in Response to Statin Signaling in Cardiac Myocytes. Circ. Res. 2007, 100, 50–60. [Google Scholar] [CrossRef] [Green Version]
- Brunet, A.; Bonni, A.; Zigmond, M.J.; Lin, M.Z.; Juo, P.; Hu, L.S.; Anderson, M.J.; Arden, K.C.; Blenis, J.; Greenberg, M.E. Akt Promotes Cell Survival by Phosphorylating and Inhibiting a Forkhead Transcription Factor. Cell 1999, 96, 857–868. [Google Scholar] [CrossRef] [Green Version]
- Schmidt, M.; de Mattos, S.F.; van der Horst, A.; Klompmaker, R.; Kops, G.J.P.L.; Lam, E.W.-F.; Burgering, B.M.T.; Medema, R.H. Cell Cycle Inhibition by FoxO Forkhead Transcription Factors Involves Downregulation of Cyclin D. Mol. Cell. Biol. 2002, 22, 7842–7852. [Google Scholar] [CrossRef] [Green Version]
- Yang, J.-Y.; Zong, C.S.; Xia, W.; Yamaguchi, H.; Ding, Q.; Xie, X.; Lang, J.-Y.; Lai, C.-C.; Chang, C.-J.; Huang, W.-C.; et al. ERK promotes tumorigenesis by inhibiting FOXO3a via MDM2-mediated degradation. Nat. Cell Biol. 2008, 10, 138–148. [Google Scholar] [CrossRef] [Green Version]
- Gazon, H.; Barbeau, B.; Mesnard, J.-M.; Peloponese, J.-M.J. Hijacking of the AP-1 Signaling Pathway during Development of ATL. Front. Microbiol. 2018, 8. [Google Scholar] [CrossRef] [Green Version]
- Abate, C.; Curran, T. Encounters with Fos and Jun on the road to AP-1. Semin. Cancer Biol. 1990, 1, 19–26. [Google Scholar] [PubMed]
- Neyns, B.; Vermeij, J.K.; Bourgain, C.; Vandamme, B.; Amfo, K.; Lissens, W.; DeSutter, P.; Hooghe-Peters, E.; DeGrève, J. Expression of the jun family of genes in human ovarian cancer and normal ovarian surface epithelium. Oncogene 1996, 12, 1247–1257. [Google Scholar] [PubMed]
- Langer, S.; Singer, C.F.; Hudelist, G.; Dampier, B.; Kaserer, K.; Vinatzer, U.; Pehamberger, H.; Zielinski, C.; Kubista, E.; Schreibner, M. Jun and Fos family protein expression in human breast cancer: Correlation of protein expression and clinicopathological parameters. Eur. J. Gynaecol. Oncol. 2006, 27, 345–352. [Google Scholar]
- Kharman-Biz, A.; Gao, H.; Ghiasvand, R.; Zhao, C.; Zendehdel, K.; Dahlman-Wright, K. Expression of activator protein-1 (AP-1) family members in breast cancer. BMC Cancer 2013, 13, 441. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drakos, E.; Leventaki, V.; Schlette, E.J.; Jones, D.; Lin, P.; Jeffrey Medeiros, L.; Rassidakis, G.Z. c-Jun Expression and Activation are Restricted to CD30+ Lymphoproliferative Disorders. Am. J. Surg. Pathol. 2007, 31, 447–453. [Google Scholar] [CrossRef]
- Mao, X.; Orchard, G.; Russell-Jones, R.; Whittaker, S. Abnormal activator protein 1 transcription factor expression in CD30-positive cutaneous large-cell lymphomas. Br. J. Dermatol. 2007, 157, 914–921. [Google Scholar] [CrossRef]
- Tulchinsky, E. Fos family members: Regulation, structure and role in oncogenic transformation. Histol. Histopathol. 2000. [Google Scholar] [CrossRef]
- Fukuda, K.; Hibiya, Y.; Mutoh, M.; Koshiji, M.; Akao, S.; Fujiwara, H. Inhibition by berberine of cyclooxygenase-2 transcriptional activity in human colon cancer cells. J. Ethnopharmacol. 1999, 66, 227–233. [Google Scholar] [CrossRef]
- Björklund, M.; Koivunen, E. Gelatinase-mediated migration and invasion of cancer cells. Biochim. Biophys. Acta 2005, 1755, 37–69. [Google Scholar] [CrossRef] [Green Version]
- Mook, O.R.F.; Frederiks, W.M.; Van Noorden, C.J.F. The role of gelatinases in colorectal cancer progression and metastasis. Biochim. Biophys. Acta 2004, 1705, 69–89. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, A.M.; Reisfeld, R.A.; Cheresh, D.A. Integrin alpha v beta 3 rescues melanoma cells from apoptosis in three-dimensional dermal collagen. Proc. Natl. Acad. Sci. USA 1994, 91, 8856–8860. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamsa, T.P.; Kuttan, G. Antiangiogenic activity of berberine is mediated through the downregulation of hypoxia-inducible factor-1, VEGF, and proinflammatory mediators. Drug Chem. Toxicol. 2012, 35, 57–70. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Ji, Q.; Ye, N.; Sui, H.; Zhou, L.; Zhu, H.; Fan, Z.; Cai, J.; Li, Q. Berberine Inhibits Invasion and Metastasis of Colorectal Cancer Cells via COX-2/PGE2 Mediated JAK2/STAT3 Signaling Pathway. PLoS ONE 2015, 10, e0123478. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Zhang, Y.; Gong, Z.; Sheng, X.; Li, Z.; Zhang, W.; Qin, Y. Berberine inhibits 3T3-L1 adipocyte differentiation through the PPARgamma pathway. Biochem. Biophys. Res. Commun. 2006, 348, 571–578. [Google Scholar] [CrossRef]
- Rojiani, M.V.; Alidina, J.; Esposito, N.; Rojiani, A.M. Expression of MMP-2 correlates with increased angiogenesis in CNS metastasis of lung carcinoma. Int. J. Clin. Exp. Pathol. 2010, 3, 775–781. [Google Scholar]
- Hwang, J.-M.; Kuo, H.-C.; Tseng, T.-H.; Liu, J.-Y.; Chu, C.-Y. Berberine induces apoptosis through a mitochondria/caspases pathway in human hepatoma cells. Arch. Toxicol. 2006, 80, 62–73. [Google Scholar] [CrossRef]
- Yount, G.; Qian, Y.; Moore, D.; Basila, D.; West, J.; Aldape, K.; Arvold, N.; Shalev, N.; Haas-Kogan, D. Berberine sensitizes human glioma cells, but not normal glial cells, to ionizing radiation in vitro. J. Exp. Ther. Oncol. 2004, 4, 137–143. [Google Scholar]
- Qi, H.; Xin, L.; Xu, X.; Ji, X.; Fan, L. Epithelial-to-mesenchymal transition markers to predict response of Berberine in suppressing lung cancer invasion and metastasis. J. Transl. Med. 2014, 12, 22. [Google Scholar] [CrossRef] [Green Version]
- Gialeli, C.; Theocharis, A.D.; Karamanos, N.K. Roles of matrix metalloproteinases in cancer progression and their pharmacological targeting. FEBS J. 2011, 278, 16–27. [Google Scholar] [CrossRef]
- McCawley, L.J.; Matrisian, L.M. Matrix metalloproteinases: Multifunctional contributors to tumor progression. Mol. Med. Today 2000, 6, 149–156. [Google Scholar] [CrossRef]
- Detry, B.; Erpicum, C.; Paupert, J.; Blacher, S.; Maillard, C.; Bruyère, F.; Pendeville, H.; Remacle, T.; Lambert, V.; Balsat, C.; et al. Matrix metalloproteinase-2 governs lymphatic vessel formation as an interstitial collagenase. Blood 2012, 119, 5048–5056. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Massagué, J. TGFbeta in Cancer. Cell 2008, 134, 215–230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, L.; Peng, Z.; Hu, Q.; Xu, L.; Zou, X.; Yu, Y.; Huang, D.; Yi, P. Berberine Suppressed Tumor Growth through Regulating Fatty Acid Metabolism and Triggering Cell Apoptosis via Targeting FABPs. Evid. Based Complement. Alternat. Med. 2020, 2020, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, Y.; Wang, W.; Tong, Y. Berberine Inhibits Proliferative Ability of Breast Cancer Cells by Reducing Metadherin. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2019, 25, 9058–9066. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Zhang, C. Berberine Inhibits MDA-MB-231 Cells by Attenuating Their Inflammatory Responses. BioMed Res. Int. 2020, 2020, 3617514. [Google Scholar] [CrossRef] [Green Version]
- Lopes, T.Z.; de Moraes, F.R.; Tedesco, A.C.; Arni, R.K.; Rahal, P.; Calmon, M.F. Berberine associated photodynamic therapy promotes autophagy and apoptosis via ROS generation in renal carcinoma cells. Biomed. Pharmacother. Biomed. Pharmacother. 2020, 123, 109794. [Google Scholar] [CrossRef]
- You, X.; Cao, X.; Lin, Y. Berberine enhances the radiosensitivity of hepatoma cells by Nrf2 pathway. Front. Biosci. Landmark Ed. 2019, 24, 1190–1202. [Google Scholar]
- Ashrafizadeh, M.; Fekri, H.S.; Ahmadi, Z.; Farkhondeh, T.; Samarghandian, S. Therapeutic and biological activities of berberine: The involvement of Nrf2 signaling pathway. J. Cell. Biochem. 2020, 121, 1575–1585. [Google Scholar] [CrossRef]
- Gao, X.; Wang, J.; Li, M.; Wang, J.; Lv, J.; Zhang, L.; Sun, C.; Ji, J.; Yang, W.; Zhao, Z.; et al. Berberine attenuates XRCC1-mediated base excision repair and sensitizes breast cancer cells to the chemotherapeutic drugs. J. Cell. Mol. Med. 2019, 23, 6797–6804. [Google Scholar] [CrossRef]
- Liu, L.; Fan, J.; Ai, G.; Liu, J.; Luo, N.; Li, C.; Cheng, Z. Berberine in combination with cisplatin induces necroptosis and apoptosis in ovarian cancer cells. Biol. Res. 2019, 52. [Google Scholar] [CrossRef] [Green Version]
- Zheng, F.; Li, J.; Ma, C.; Tang, X.; Tang, Q.; Wu, J.; Chai, X.; Xie, J.; Yang, X.-B.; Hann, S.S. Novel regulation of miR-34a-5p and HOTAIR by the combination of berberine and gefitinib leading to inhibition of EMT in human lung cancer. J. Cell. Mol. Med. 2020, 24, 5578–5592. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Jia, Y.; Zheng, X.; Shao, D.; Zhao, Y.; Wang, Z.; Dawulieti, J.; Liu, W.; Sun, M.; Sun, W.; et al. Janus nanocarrier-based co-delivery of doxorubicin and berberine weakens chemotherapy-exacerbated hepatocellular carcinoma recurrence. Acta Biomater. 2019, 100, 352–364. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Zhu, Z.; Liu, Y.; Wei, L.; Li, B.; Mao, F.; Zhang, J.; Wang, Y.; Liu, Y. MDM2 inhibition-mediated autophagy contributes to the pro-apoptotic effect of berberine in p53-null leukemic cells. Life Sci. 2020, 242, 117228. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Liu, Y.; Du, X.; Ma, H.; Yao, J. Berberine Reverses Doxorubicin Resistance by Inhibiting Autophagy Through the PTEN/Akt/mTOR Signaling Pathway in Breast Cancer. OncoTargets Ther. 2020, 13, 1909–1919. [Google Scholar] [CrossRef] [Green Version]
- Khan, I.; Joshi, G.; Nakhate, K.T.; Kumar, R.; Gupta, U. Nano-Co-Delivery of Berberine and Anticancer Drug Using PLGA Nanoparticles: Exploration of Better Anticancer Activity and In Vivo Kinetics. Pharm. Res. 2019, 36, 149. [Google Scholar] [CrossRef]
- Maiti, P.; Plemmons, A.; Dunbar, G.L. Combination treatment of berberine and solid lipid curcumin particles increased cell death and inhibited PI3K/Akt/mTOR pathway of human cultured glioblastoma cells more effectively than did individual treatments. PLoS ONE 2019, 14, e0225660. [Google Scholar] [CrossRef]
- Qin, Q.-P.; Wang, Z.-F.; Huang, X.-L.; Tan, M.-X.; Luo, Z.-H.; Wang, S.-L.; Zou, B.-Q.; Liang, H. Two telomerase-targeting Pt(II) complexes of jatrorrhizine and berberine derivatives induce apoptosis in human bladder tumor cells. Dalton Trans. 2019, 48, 15247–15254. [Google Scholar] [CrossRef]
- Li, X.-D.; Wang, Z.; Wang, X.-R.; Shao, D.; Zhang, X.; Li, L.; Ge, M.-F.; Chang, Z.-M.; Dong, W.-F. Berberine-loaded Janus gold mesoporous silica nanocarriers for chemo/radio/photothermal therapy of liver cancer and radiation-induced injury inhibition. Int. J. Nanomed. 2019, 14, 3967–3982. [Google Scholar] [CrossRef] [Green Version]
- Suganthi, S.; Sivaraj, R.; Enoch, I.V.M.V. Molecular encapsulation of berberine by a modified β-cyclodextrin and binding of host: Guest complex to G-quadruplex DNA. Nucleosides Nucleotides Nucleic Acids 2019, 38, 858–873. [Google Scholar] [CrossRef]
- De Francesco, E.M.; Ózsvári, B.; Sotgia, F.; Lisanti, M.P. Dodecyl-TPP Targets Mitochondria and Potently Eradicates Cancer Stem Cells (CSCs): Synergy With FDA-Approved Drugs and Natural Compounds (Vitamin C and Berberine). Front. Oncol. 2019, 9. [Google Scholar] [CrossRef] [Green Version]
- Xu, L.; Zhang, Y.; Xue, X.; Liu, J.; Li, Z.-S.; Yang, G.-Y.; Song, Y.; Pan, Y.; Ma, Y.; Hu, S.; et al. A Phase I Trial of Berberine in Chinese with Ulcerative Colitis. Cancer Prev. Res. 2020, 13, 117–126. [Google Scholar] [CrossRef] [Green Version]
- Hallajzadeh, J.; Maleki Dana, P.; Mobini, M.; Asemi, Z.; Mansournia, M.A.; Sharifi, M.; Yousefi, B. Targeting of oncogenic signaling pathways by berberine for treatment of colorectal cancer. Med. Oncol. 2020, 37, 49. [Google Scholar] [CrossRef]
- Wang, B.; Deng, A.-J.; Li, Z.-H.; Wang, N.; Qin, H.-L. Syntheses and Structure–Activity Relationships in Growth Inhibition Activity against Human Cancer Cell Lines of 12 Substituted Berberine Derivatives. Molecules 2020, 25, 1871. [Google Scholar] [CrossRef]
- Zhang, C.; Sheng, J.; Li, G.; Zhao, L.; Wang, Y.; Yang, W.; Yao, X.; Sun, L.; Zhang, Z.; Cui, R. Effects of Berberine and Its Derivatives on Cancer: A Systems Pharmacology Review. Front. Pharmacol. 2020, 10. [Google Scholar] [CrossRef] [Green Version]
- Jin, H.; Ko, Y.S.; Park, S.W.; Chang, K.C.; Kim, H.J. 13-Ethylberberine Induces Apoptosis through the Mitochondria-Related Apoptotic Pathway in Radiotherapy-Resistant Breast Cancer Cells. Molecules 2019, 24, 2448. [Google Scholar] [CrossRef] [Green Version]
- Milata, V.; Svedova, A.; Barbierikova, Z.; Holubkova, E.; Cipakova, I.; Cholujova, D.; Jakubikova, J.; Panik, M.; Jantova, S.; Brezova, V.; et al. Synthesis and Anticancer Activity of Novel 9-O-Substituted Berberine Derivatives. Int. J. Mol. Sci. 2019, 20, 2169. [Google Scholar] [CrossRef] [Green Version]
- Wang, Z.-C.; Wang, J.; Chen, H.; Tang, J.; Bian, A.-W.; Liu, T.; Yu, L.-F.; Yi, Z.; Yang, F. Synthesis and anticancer activity of novel 9,13-disubstituted berberine derivatives. Bioorg. Med. Chem. Lett. 2020, 30, 126821. [Google Scholar] [CrossRef]
- Lin, H.-J.; Ho, J.-H.; Tsai, L.-C.; Yang, F.-Y.; Yang, L.-L.; Kuo, C.-D.; Chen, L.-G.; Liu, Y.-W.; Wu, J.-Y. Synthesis and In Vitro Photocytotoxicity of 9-/13-Lipophilic Substituted Berberine Derivatives as Potential Anticancer Agents. Molecules 2020, 25, 677. [Google Scholar] [CrossRef] [Green Version]
- Li, G.; Ren, Y.; Zhang, X.; Zhao, S.; Wang, Y.; Wu, J.; Peng, S.; Zhao, M. 13-[CH2CO-Cys-(Bzl)-OBzl]-Berberine: Exploring The Correlation Of Anti-Tumor Efficacy With ROS And Apoptosis Protein. OncoTargets Ther. 2019, 12, 10651–10662. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.; Zhu, K.; Cao, L.; Xie, Z.; Gu, M.; Lü, W.; Li, J.; Nan, F. Berberine derivatives with a long alkyl chain branched by hydroxyl group and methoxycarbonyl group at 9-position show improved anti-proliferation activity and membrane permeability in A549 cells. Acta Pharmacol. Sin. 2020, 41, 813–824. [Google Scholar] [CrossRef]
- Du, P.; Yan, J.; Long, S.; Xiong, H.; Wen, N.; Cai, S.; Wang, Y.; Peng, D.; Liu, Z.; Liu, Y. Tumor microenvironment and NIR laser dual-responsive release of berberine 9-O-pyrazole alkyl derivative loaded in graphene oxide nanosheets for chemo-photothermal synergetic cancer therapy. J. Mater. Chem. B 2020, 8, 4046–4055. [Google Scholar] [CrossRef] [PubMed]
- Leyva-Peralta, M.A.; Robles-Zepeda, R.E.; Razo-Hernández, R.S.; Berber, L.P.Á.; Lara, K.O.; Ruiz-Bustos, E.; Gálvez-Ruíz, J.C. Berberine as Source of Antiproliferative Hybrid Compounds: In Vitro Antiproliferative Activity and Quantitative Structure-activity Relationship. Anticancer Agents Med. Chem. 2019, 19, 1820–1834. [Google Scholar] [CrossRef] [PubMed]
- Home—ClinicalTrials.gov. Available online: https://clinicaltrials.gov/ (accessed on 6 September 2020).
- Wei, X.; Zhu, L.; Wang, C. Efficacy and Safety of Berberine in Patients with Type 2 Diabetes Mellitus: A Meta-Analysis. Chin. Herb. Med. 2015, 7, 344–353. [Google Scholar] [CrossRef]
- Derosa, G.; D’Angelo, A.; Vanelli, A.; Maffioli, P. An Evaluation of a Nutraceutical with Berberine, Curcumin, Inositol, Banaba and Chromium Picolinate in Patients with Fasting Dysglycemia. Diabetes Metab. Syndr. Obes. Targets Ther. 2020, 13, 653–661. [Google Scholar] [CrossRef] [Green Version]
- Pérez-Rubio, K.G.; González-Ortiz, M.; Martínez-Abundis, E.; Robles-Cervantes, J.A.; Espinel-Bermúdez, M.C. Effect of Berberine Administration on Metabolic Syndrome, Insulin Sensitivity, and Insulin Secretion. Metab. Syndr. Relat. Disord. 2013, 11, 366–369. [Google Scholar] [CrossRef]
- Chen, Y.-X.; Gao, Q.-Y.; Zou, T.-H.; Wang, B.-M.; Liu, S.-D.; Sheng, J.-Q.; Ren, J.-L.; Zou, X.-P.; Liu, Z.-J.; Song, Y.-Y.; et al. Berberine versus placebo for the prevention of recurrence of colorectal adenoma: A multicentre, double-blinded, randomised controlled study. Lancet Gastroenterol. Hepatol. 2020, 5, 267–275. [Google Scholar] [CrossRef]
- Gonnelli, S.; Caffarelli, C.; Stolakis, K.; Cuda, C.; Giordano, N.; Nuti, R. Efficacy and Tolerability of a Nutraceutical Combination (Red Yeast Rice, Policosanols, and Berberine) in Patients with Low-Moderate Risk Hypercholesterolemia: A Double-Blind, Placebo-Controlled Study. Curr. Ther. Res. 2015, 77, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Yan, H.-M.; Xia, M.-F.; Wang, Y.; Chang, X.-X.; Yao, X.-Z.; Rao, S.-X.; Zeng, M.-S.; Tu, Y.-F.; Feng, R.; Jia, W.-P.; et al. Efficacy of Berberine in Patients with Non-Alcoholic Fatty Liver Disease. PLoS ONE 2015, 10, e0134172. [Google Scholar] [CrossRef] [Green Version]
- Cereda, E.; Cappello, S.; Caraccia, M.; Turri, A.; Masi, S.; Nappi, R.; Caccialanza, R. SUN-PO004: Nutraceutical Intervention with Berberine, Chlorogenic Acid and Tocotrienols for Menopause-Associated Dyslipidemia: A Pilot, Single-ARM Trial. Clin. Nutr. 2019, 38, S60. [Google Scholar] [CrossRef]
- Zhang, D.; Ke, L.; Ni, Z.; Chen, Y.; Zhang, L.-H.; Zhu, S.-H.; Li, C.-J.; Shang, L.; Liang, J.; Shi, Y.-Q. Berberine containing quadruple therapy for initial Helicobacter pylori eradication. Medicine 2017, 96. [Google Scholar] [CrossRef]
- Mirhadi, E.; Rezaee, M.; Malaekeh-Nikouei, B. Nano strategies for berberine delivery, a natural alkaloid of Berberis. Biomed. Pharmacother. 2018, 104, 465–473. [Google Scholar] [CrossRef] [PubMed]
| Activity | Molecular Targets | References |
|---|---|---|
| Cell cycle arrest | ||
| Induced G0/G1 phase arrest | [47,51,52,53] | |
| ↓cyclin B1 expression | ||
| Induced G1 phase arrest | ||
| ↑geneBTG2 expression | ||
| ↑p53 protein expression | [47,48,49] | |
| ↓cyclin B1 expression | ||
| ↑Weel1 expression | [47,54] | |
| ↓cyclin D1 expression | [47] | |
| Induced G2 phase arrest | ||
| ↓cyclin B1 expression | ||
| ↑Weel1 expression | [47,54] | |
| Induced G2/M phase arrest | ||
| REV3-gene dependent | [55,56] | |
| Apoptosis induction | ||
| genes | ||
| ↑CASP3 expression | ||
| ↑CASP8 expression | ||
| ↑CASP9 expression | ||
| ↑BAX expression | ||
| ↑BAK1 expression | ||
| ↑BIK expression | ||
| ↓BNIP3 expression | ||
| ↓BNIP1 expression | ||
| ↓BCL2 expression | ||
| ↓BCL2L2 expression | [43] | |
| proteins | ||
| ↑caspase-3 expression | ||
| ↑caspase-9 expression | ||
| ↑Bax expression | [33,45] | |
| ↓Bcl-2 expression | [33] | |
| ↑p-53 expression | ||
| ↑ Rb expression | ||
| ↑ATM expression | ||
| Caspase-8 expression | ||
| ↑BID expression | ||
| ↑TNF expression | ||
| ↓c-IAP1 expression | ||
| ↓XIAP expression | ||
| ↓Bcl-X expression | ||
| ↓Survivin expression | [22,58,59] | |
| TNF-alpha receptors | ||
| ↑DR4 activation | ||
| ↑DR5 activation | [54,60] | |
| Influence on MAPK | ||
| cell type depending | ↑MAPK activity | [20,21,61] |
| ↑miR-19a/TF/MAPK pathway activity | ||
| ↑miR-19a level | ||
| ↓TF level | [21] | |
| ↑ERK1/2 phosphorylation | [62] | |
| ↓ERK1/2 phosphorylation | [19] | |
| ↓p38 MAPK phosphorylation | [19,62] | |
| ↑JNK phosphorylation | [62] | |
| ↓JNK phosphorylation | [19] | |
| ↓JNK/p38 MAPK pathway activity | [22] | |
| ↑JNK/p38 MAPK pathway activity | [20] | |
| ↑cell cycle inhibitor p21 (CIP1/WAF1) induction | ||
| ↑p53 level | [20] | |
| ↑FOXO3a induction | ||
| Transcription Regulation | ||
| ↑/↓AP-1 protein activity (cell type depending) | [39,43,78] | |
| ↓ C-fos proto-oncogene expression | [54] | |
| Inhibition of metastasis | ||
| proteins | ||
| ↓MMP-2 level | ||
| ↓MMP-9 level | [54,82,83] | |
| ↓p-STAT3 phosphorylation | ||
| ↓p-STAT3 transfer to nucleus | ||
| ↓p-JAK2 phosphorylation | ||
| Interruption of COX2/JAK/STAT signaling pathway | [23,29] | |
| Inhibition of angiogenesis | ||
| genes | ||
| ↓VEGF expression | ||
| ↓COX-2 expression | ||
| ↓HIF expression | [58] | |
| proteins | ||
| ↓VEGR expression and activity | ||
| ↓IL-1β activity | ||
| ↓IL-6 activity | ||
| ↓TNF-α activity | ||
| ↓GM-CSF activity | ||
| ↓NF-κB activity | ||
| ↓c-Fos activity | ||
| ↓CREB activity | [54,82] | |
| ↓PI-3K/AKT pathway | [84] | |
| Inhibition of epithelial-to-mesenchymal transition | ||
| ↓TGF-β1 release | ||
| ↑E-cadherin level | [90,91,92] | |
| Anti-inflammatory activity | ||
| genes | ||
| ↓IL-1 transcription | [29] | |
| ↓TNF transcription | ||
| ↓IL-6 transcription | ||
| proteins | ||
| ↓COX2 expression | [29] | |
| ↓COX2 transcriptional activity | [78] | |
| ↓IL-8 tumor cells production | [58] | |
| ↓NF-κB signaling pathway | [22,58] | |
| ↓NO elevation | ||
| ↓TNF-α elevation | [29,82] | |
| Inhibition of carcinogenesis combined with metabolism of lipids | ||
| ↓levels of fatty acids in cancer cells | [93] | |
| ↓SCAP/SREBP-1 pathway | ||
| ↓activity of lipogenic enzymes | ||
| ↓JNK phosphorylation | ||
| ↓lipid synthesis | [53] | |
| Title | Status | Conditions | Interventions | Phase | Measures | Enrollment | Age (Years) | Completion: |
|---|---|---|---|---|---|---|---|---|
| A Research of Berberine Hydrochloride to Prevent Colorectal Adenomas in Patients with Previous Colorectal Cancer | Recruiting | Colorectal Adenomas | Berberine hydrochloride and Placebo | Phase 2 Phase 3 |
| 1000 | 18–80 | March 2021 |
| Comparison of Berberine and Metformin for the Treatment for MS in Schizophrenia Patients | Recruiting | Schizophrenia Metabolic Syndrome | Berberine Metformin | Phase 4 |
| 100 | 18–65 | December 2019 |
| Primary Chemoprevention of Familial Adenomatous Polyposis with Berberine Hydrochloride | Recruiting | Colorectal Adenomas | Berberine hydrochloride Placebo | Phase 2 Phase 3 | Cumulative numbers and diameters of colorectal adenomas during Berberine hydrochloride or placebo treatment in patients with familial adenomatous polyposis | 100 | 18–65 | December 2020 |
| Effect of Berberine Versus Metformin on Glycemic Control, Insulin Sensitivity and Insulin Secretion in Prediabetes | Active, not recruiting | Prediabetes Impaired Fasting Glucose Impaired Glucose Tolerance | Berberine Metformin | Phase 4 |
| 28 | 31–60 | August 2020 |
| Effect of Berberine for Endothelial Function and Intestinal Microflora in Patients with Coronary Artery Disease | Active, not recruiting | Stable Coronary Artery Disease Percutaneous Coronary Intervention | Berberine Aspirin Clopidogrel Statin | Phase 1 Phase 2 |
| 24 | 18–75 | December 2020 |
| A Mechanistic Randomized Controlled Trial on the Cardiovascular Effect of Berberine | Recruiting | Cardiovascular Risk Factor | Berberine Placebo | Phase 2 Phase 3 |
| 84 | 20–65 | June 2020 |
| Combination of Danazole With Berberine in the Treatment of ITP | Active, not recruiting | Corticosteroid-resistant or Relapsed ITP | Berberine plus danazol | Phase 2 |
| 55 | 18–80 | June 2021 |
| Antiplatelet Effect of Berberine in Patients After Percutaneous Coronary Intervention | Recruiting | Coronary Artery Disease Percutaneous Coronary Intervention | Berberine Standard treatment Aspirin Clopidogrel | Phase 4 | P2Y12 reaction unit
| 64 | 18–70 | December 2020 |
| Berberine Chloride in Preventing Colorectal Cancer in Patients with Ulcerative Colitis in Remission | Active, not recruiting | Ulcerative Colitis | Berberine Chloride Placebo | Phase 1 |
| 18 | 18–70 | December 2020 |
| Berberine Prevent Contrast-induced Nephropathy in Patients With Diabetes | Recruiting | Diabetes Mellitus Chronic Kidney Disease | Berberine | Phase 4 |
| 800 | 18 and older | December 2020 |
| Berberine as Adjuvant Treatment for Schizophrenia Patients | Recruiting | Schizophrenia Spectrum and Other Psychotic Disorders Metabolic Syndrome x | Berberine Placebos Antipsychotic Agents | Phase 2 Phase 3 | Weight gain
| 120 | 18–65 | May 2021 |
| Evaluating the Tolerability and Effects of Berberine on Major Metabolic Biomarkers: A Pilot Study | Recruiting | Metabolic Syndrome | Berberine Identical Placebo | Not Applicable | LDL Cholesterol
| 40 | 18 and older | December 2021 |
| Efficacy and Safety of Berberine in Non-alcoholic Steatohepatitis | Recruiting | Non-alcoholic Steatohepatitis | Behavioral: Lifestyle Placebo | Phase 4 |
| 120 | 18–75 | July 2021 |
| Study on the Efficacy and Gut Microbiota of Berberine and Probiotics in Patients with Newly Diagnosed Type 2 Diabetes | Active, not recruiting | Type 2 Diabetes | Berberine hydrochloride ProMetS probiotics powder | Phase 3 |
| 400 | 20–69 | May 2019 |
| Effect of Mebo Dressing Versus Standard Care on Managing Donor and Recipient Sites of Split-thickness Skin Graft | Recruiting | Burns | Moist Exposed Burn Ointment (MEBO-sesame oil, beta-sitosterol, berberine and other small quantities of plant ingredients) | Phase 1 | Wound Healing Assessment Recovery Time
| 40 | 2–60 | July 2019 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Och, A.; Podgórski, R.; Nowak, R. Biological Activity of Berberine—A Summary Update. Toxins 2020, 12, 713. https://0-doi-org.brum.beds.ac.uk/10.3390/toxins12110713
Och A, Podgórski R, Nowak R. Biological Activity of Berberine—A Summary Update. Toxins. 2020; 12(11):713. https://0-doi-org.brum.beds.ac.uk/10.3390/toxins12110713
Chicago/Turabian StyleOch, Anna, Rafał Podgórski, and Renata Nowak. 2020. "Biological Activity of Berberine—A Summary Update" Toxins 12, no. 11: 713. https://0-doi-org.brum.beds.ac.uk/10.3390/toxins12110713





