Protection of Residual Renal Function and Nutritional Treatment: First Step Strategy for Reduction of Uremic Toxins in End-Stage Kidney Disease Patients
Abstract
:1. Introduction
2. Protection of Residual Kidney Function
3. Nutritional Treatment
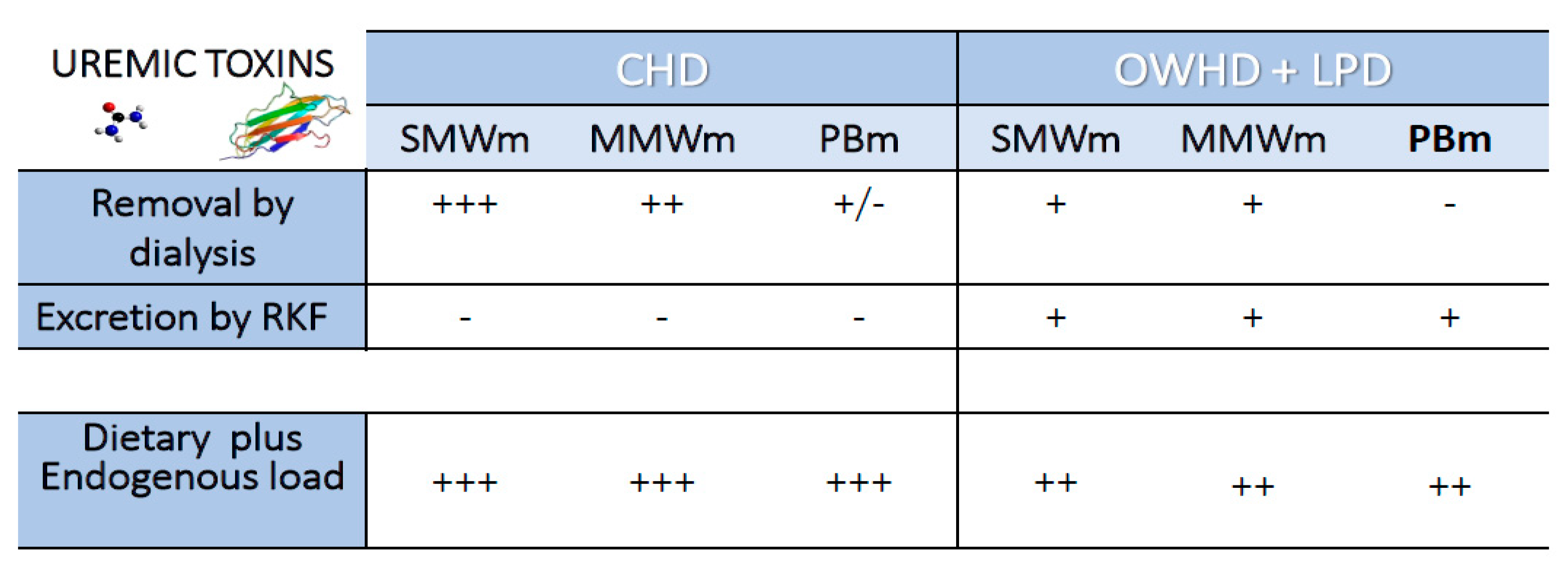
4. Once-Weekly Hemodialysis Plus Low-Protein Diet
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bergstrom, J.; Furst, P. Uremic toxins. Kidney Int. Suppl. 1978, 8, S9–S12. [Google Scholar]
- Vanholder, R.; De Smet, R.; Glorieux, G.; Argilès, A.; Baurmeister, U.; Brunet, P.; Clark, W.; Cohen, G.; De Deyn, P.P.; Deppish, R.; et al. Review on uremic toxins. Classification, concentration and inter-individual variability. Kidney Int. 2003, 63, 1934–1943. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clark, W.R.; Dehghani, N.L.; Narsimhan, V.; Ronco, C. Uremic Toxins and their Relation to Dialysis Efficacy. Blood Purif. 2019, 48, 299–314. [Google Scholar] [CrossRef]
- Koppe, L.; Soulage, C.O. Preservation of residual kidney function to reduce non-urea solutes toxicity in haemodialysis. Nephrol. Dial. Transplant. 2020, 35, 733–736. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vanholder, R.; Gryp, T.; Glorieux, G. Urea and chronic kidney disease: The comeback of the century? (in uraemia research). Nephrol. Dial. Transplant. 2018, 33, 4–12. [Google Scholar] [CrossRef] [Green Version]
- Cupisti, A.; Gallieni, M.; Avesani, C.M.; D’Alessandro, C.; Carrero, J.J.; Piccoli, G.B. Medical Nutritional Therapy for Patients with Chronic Kidney Disease not on Dialysis: The Low Protein Diet as a Medication. J. Clin. Med. 2020, 9, 3644. [Google Scholar] [CrossRef] [PubMed]
- Cupisti, A.; Brunori, G.; Di Iorio, B.R.; D’Alessandro, C.; Pasticci, F.; Cosola, C.; Bellizzi, V.; Bolasco, P.; Capitanini, A.; Fantuzzi, A.L.; et al. Nutritional treatment of advanced CKD: Twenty consensus statements. J. Nephrol. 2018, 31, 457–473. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalantar-Zadeh, K.; Fouque, D. Nutritional Management of Chronic Kidney Disease. N. Engl. J. Med. 2017, 377, 1765–1776. [Google Scholar] [CrossRef]
- Ikizler, T.A.; Burrowes, J.D.; Byham-Gray, L.D.; Campbell, K.L.; Carrero, J.J.; Chan, W.; Fouque, D.; Friedman, A.N.; Ghaddar, S.; Goldstein-Fuchs, D.J.; et al. KDOQI Clinical Practice Guideline for Nutrition in CKD: 2020 Update. Am. J. Kidney Dis. 2020, 76, S1–S107. [Google Scholar] [CrossRef]
- Madero, M.; Cano, KB.; Campos, I.; Tao, X.; Maheshwari, V.; Brown, J.; Cornejo, B.; Handelman, G.; Thijssen, S.; Kotanko, P. Removal of Protein-Bound Uremic Toxins during Hemodialysis Using a Binding Competitor. Clin. J. Am. Soc. Nephrol. 2019, 14, 394–402. [Google Scholar] [CrossRef]
- Böhringer, F.; Jankowski, V.; Gajjala, P.R.; Zidek, W.; Jankowski, J. Release of uremic retention solutes from protein binding by hypertonic predilution hemodiafiltration. ASAIO J. 2015, 61, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Schulman, G.; Berl, T.; Beck, G.J.; Remuzzi, G.; Ritz, E.; Arita, K.; Kato, A.; Shimizu, M. Randomized Placebo-Controlled EPPIC Trials of AST-120 in CKD. J. Am. Soc. Nephrol. 2015, 26, 1732–1746. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takkavatakarn, K.; Wuttiputinun, T.; Phannajit, J.; Praditpornsilpa, K.; Eiam-Ong, S.; Susantitaphong, P. Protein-bound uremic toxin lowering strategies in chronic kidney disease: A systematic review and meta-analysis. J. Nephrol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Ramezani, A.; Massy, Z.A.; Meijers, B.; Evenepoel, P.; Vanholder, R.; Raj, D.S. Role of the Gut Microbiome in Uremia: A Potential Therapeutic Target. Am. J. Kidney Dis. 2016, 67, 483–498. [Google Scholar] [CrossRef] [Green Version]
- Sekirov, I.; Russell, S.L.; Caetano, L.; Antunes, M.; Finlay, B.B. Gut Microbiota in Health and Disease. Physiol. Rev. 2010, 90, 859–904. [Google Scholar] [CrossRef] [Green Version]
- Evenepoel, P.; Meijers, B.K.I.; Bammens, B.R.M.; Verbeke, K. Uremic toxins originating from colonic microbial metabolism. Kidney Int. 2009, 76, S12–S19. [Google Scholar] [CrossRef] [Green Version]
- Vaziri, N.D.; Goshtasbi, N.; Yuan, J.; Jellbauer, S.; Moradi, H.; Raffatellu, M.; Kalantar-Zadeh, K. Uremic plasma impairs barrier function and depletes the tight junction protein constituents of intestinal epithelium. Am. J. Nephrol. 2012, 36, 438–443. [Google Scholar] [CrossRef] [Green Version]
- Koppe, L.; Fouque, D.; Soulage, CO. The Role of Gut Microbiota and Diet on Uremic Retention Solutes Production in the Context of Chronic Kidney Disease. Toxins 2018, 10, 155. [Google Scholar] [CrossRef] [Green Version]
- Mafra, D.; Borges, N.; Alvarenga, L.; Esgalhado, M.; Cardozo, L.; Lindholm, B.; Stenvinkel, P. Dietary Components That May Influence the Disturbed Gut Microbiota in Chronic Kidney Disease. Nutrients 2019, 11, 496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cosola, C.; Rocchetti, M.T.; Sabatino, A.; Fiaccadori, E.; Di Iorio, B.R.; Gesualdo, L. Microbiota issue in CKD: How promising are gut-targeted approaches? J. Nephrol. 2019, 32, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Sabatino, A.; Regolisti, G.; Brusasco, I.; Cabassi, A.; Morabito, S.; Fiaccadori, E. Alterations of intestinal barrier and microbiota in chronic kidney disease. Nephrol. Dial. Transplant. 2015, 30, 924–933. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krishnamurthy, V.M.R.; Wei, G.; Baird, B.C.; Murtaugh, M.; Chonchol, M.B.; Raphael, K.L.; Greene, T.; Beddhu, S. High dietary fiber intake is associated with decreased inflammation and all-cause mortality in patients with chronic kidney disease. Kidney Int. 2012, 81, 300–306. [Google Scholar] [CrossRef] [Green Version]
- Bammens, B.; Verbeke, K.; Vanrenterghem, Y.; Evenepoel, P. Evidence for impaired assimilation of protein in chronic renal failure. Kidney Int. 2003, 64, 2196–2203. [Google Scholar] [CrossRef] [PubMed]
- Bammens, B.; Evenepoel, P.; Verbeke, K.; Vanrenterghem, Y. Impairment of small intestinal assimilation in patients with end-stage renal disease: Extending the malnutrition-inflammation-atherosclerosis concept. Am. J. Clin. Nutr. 2004, 80, 1536–1543. [Google Scholar] [CrossRef] [PubMed]
- Hida, M.; Aiba, Y.; Sawamura, S.; Suzuki, N.; Satoh, T.; Koga, Y. Inhibition of the accumulation of uremic toxins in the blood and their precursors in the feces after oral administration of Lebenin, a lactic acid bacteria preparation, to uremic patients undergoing hemodialysis. Nephron 1996, 74, 349–355. [Google Scholar] [CrossRef]
- Itoh, Y.; Ezawa, A.; Kikuchi, K.; Tsuruta, Y.; Niwa, T. Protein-bound uremic toxins in hemodialysis patients measured by liquid chromatography/tandem mass spectrometry and their effects on endothelial ROS production. Anal. Bioanal. Chem. 2012, 403, 1841–1850. [Google Scholar] [CrossRef]
- Vanholder, R.; Schepers, E.; Pletinck, A.; Nagler, E.V.; Glorieux, G. The uremic toxicity of indoxyl sulfate and p-cresyl sulfate: A systematic review. J. Am. Soc. Nephrol. 2014, 25, 1897–1907. [Google Scholar] [CrossRef] [PubMed]
- Cosola, C.; Rocchetti, MT.; Cupisti, A.; Gesualdo, L. Microbiota metabolites: Pivotal players of cardiovascular damage in chronic kidney disease. Pharmacol. Res. 2018, 130, 132–142. [Google Scholar] [CrossRef]
- Sirich, T.L.; Funk, B.A.; Plummer, N.S.; Hostetter, T.H.; Meyer, T.W. Prominent Accumulation in Hemodialysis Patients of Solutes Normally Cleared by Tubular Secretion. J. Am. Soc. Nephrol. 2014, 25, 615–622. [Google Scholar] [CrossRef]
- Gryp, T.; De Paepe, K.; Vanholder, R.; Kerckhof, F.M.; Van Biesen, W.; Van de Wiele, T.; Verbeke, F.; Speeckaert, M.; Joossens, M.; Couttenye, M.M.; et al. Gut microbiota generation of protein-bound uremic toxins and related metabolites is not altered at different stages of chronic kidney disease. Kidney Int. 2020, 97, 1230–1242. [Google Scholar] [CrossRef] [Green Version]
- Tang, W.H.; Wang, Z.; Kennedy, D.J.; Wu, Y.; Buffa, J.A.; Agatisa-Boyle, B.; Li, X.S.; Levison, B.S.; Hazen, S.L. Gut microbiota-dependent trimethylamine N-oxide (TMAO) pathway contributes to both development of renal insufficiency and mortality risk in chronic kidney disease. Circ. Res. 2015, 116, 448–455. [Google Scholar] [CrossRef] [Green Version]
- Hai, X.; Landeras, V.; Dobre, M.A.; DeOreo, P.; Meyer, T.W.; Hostetter, T.H. Mechanism of prominent trimethylamine oxide (TMAO) accumulation in hemodialysis patients. PLoS ONE 2015, 10, e0143731. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Wilcox, C.S.; Lipkowitz, M.S.; Gordon-Cappitelli, J.; Dragoi, S. Rationale and Strategies for Preserving Residual Kidney Function in Dialysis Patients. Am. J. Nephrol. 2019, 50, 411–421. [Google Scholar] [CrossRef] [PubMed]
- Nongnuch, A.; Assanatham, M.; Panorchan, K.; Davenport, A. Strategies for preserving residual renal function in peritoneal dialysis patients. Clin. Kidney J. 2015, 8, 202–211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mathew, A.T.; Fishbane, S.; Obi, Y.; Kalantar-Zadeh, K. Preservation of residual Kidney function in hemodialysis patients: Reviving an old concept for contemporary practice. Kidney Int. 2016, 90, 262–271. [Google Scholar] [CrossRef] [Green Version]
- Shafi, T.; Jaar, B.G.; Plantinga, L.C.; Fink, N.E.; Sadler, J.H.; Parekh, S.R.; Powe, N.R.; Coresh, J. Association of residual urine output with mortality, quality of life, and inflammation in incident hemodialysis patients: The Choices for Healthy Outcomes in Caring for End-Stage Renal Disease (CHOICE) Study. Am. J. Kidney Dis. 2010, 56, 348–358. [Google Scholar] [CrossRef] [Green Version]
- Palomo-Piñón, S.; Mora-Villalpando, C.J.; Del Carmen Prado-Uribe, M.; Ceballos-Reyes, G.M.; De Jesús Ventura-García, M.; Ávila-Díaz, M.; Rodríguez, O.O.; Paniagua-Sierra, J.R. Inflammation and myocardial damage markers influence loss of residual renal function in peritoneal dialysis patients. Arch. Med. Res. 2014, 45, 484–488. [Google Scholar] [CrossRef]
- Wang, A.Y.; Wang, M.; Woo, J.; Wai-Kei Lam, C.W.; Lui, S.; Li, P.K.; Sanderson, J.E. Inflammation, residual kidney function, and cardiac hypertrophy are interrelated and combine adversely to enhance mortality and cardiovascular death risk of peritoneal dialysis patients. J. Am. Soc. Nephrol. 2004, 15, 2186–2194. [Google Scholar] [CrossRef] [Green Version]
- Moist, L.M.; Port, F.K.; Orzol, S.M.; Young, E.W.; Ostbye, T.; Wolfe, R.A.; Hulbert-Shearon, T.; Jones, C.A.; Bloembergen, W.E. Predictors of loss of residual renal function among new dialysis patients. J. Am. Soc. Nephrol. 2000, 11, 556–564. [Google Scholar]
- Jansen, M.A.M.; Hart, A.A.M.; Korevaar, J.C.; Dekker, F.W.; Boeschoten, E.W.; Krediet, R.T.; NECOSAD Study Group. Predictors of the rate of decline of residual renal function in incident dialysis patients. Kidney Int. 2002, 62, 1046–1053. [Google Scholar] [CrossRef] [Green Version]
- Hemodialysis Adequacy 2006 Work Group. Clinical practice guidelines for hemodialysis adequacy, update 2006. Am. J. Kidney Dis. 2006, 48, S2–S90. [Google Scholar] [CrossRef] [PubMed]
- Daugirdas, J.T.; Greene, T.; Rocco, M.V.; Kaysen, G.A.; Depner, T.A.; Levin, N.W.; Chertow, G.M.; Ornt, D.B.; Raimann, J.G.; Larive, B.; et al. Effect of frequent hemodialysis on residual kidney function. Kidney Int. 2013, 83, 949–958. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, M.; Wang, M.; Li, H.; Yu, P.; Yuan, L.; Hao, C.; Chen, J.; Kalantar-Zadeh, K. Association of initial twice-weekly hemodialysis treatment with preservation of residual kidney function in ESRD patients. Am. J. Nephrol. 2014, 40, 140–150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sandrini, M.; Vizzardi, V.; Valerio, F.; Ravera, S.; Manili, L.; Zubani, R.; Lucca, B.J.; Cancarini, G. Incremental peritoneal dialysis: A 10 year single-centre experience. J. Nephrol. 2016, 29, 871–879. [Google Scholar] [CrossRef] [Green Version]
- Lee, Y.; Chung, S.W.; Park, S.; Ryu, H.; Lee, H.; Kim, D.K.; Joo, K.W.; Ahn, C.; Lee, J.; Oh, K.H. Incremental Peritoneal Dialysis May be Beneficial for Preserving Residual Renal Function Compared to Full-dose Peritoneal Dialysis. Sci. Rep. 2019, 9, 10105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalantar-Zadeh, K.; Unruh, M.; Zager, P.G.; Kovesdy, C.P.; Bargman, J.M.; Chen, J.; Sankarasubbaiyan, S.; Shah, G.; Golper, T.; Sherman, R.A.; et al. Twice-weekly and incremental hemodialysis treatment for initiation of kidney replacement therapy. Am. J. Kidney Dis. 2014, 64, 181–186. [Google Scholar] [CrossRef] [Green Version]
- Garibotto, G.; Sofia, A.; Parodi, E.L.; Ansaldo, F.; Bonanni, A.; Picciotto, D.; Signori, A.; Vettore, M.; Tessari, P.; Verzola, D. Effects of Low-Protein, and Supplemented Very Low-Protein Diets, on Muscle Protein Turnover in Patients with CKD. Kidney Int. Rep. 2018, 3, 701–710. [Google Scholar] [CrossRef] [Green Version]
- Goodship, T.H.; Mitch, W.E.; Hoerr, R.A.; Wagner, D.A.; Steinman, T.I.; Young, V.R. Adaptation to low-protein diets in renal failure: Leucine turnover and nitrogen balance. J. Am. Soc. Nephrol. 1990, 1, 66–75. [Google Scholar]
- Jiang, N.; Qian, J.; Sun, W.; Lin, A.; Cao, L.; Wang, Q.; Ni, Z.; Wan, Y.; Linholm, B.; Axelsson, J.; et al. Better preservation of residual renal function in peritoneal dialysis patients treated with a low-protein diet supplemented with keto acids: A prospective, randomized trial. Nephrol. Dial. Transplant. 2009, 24, 2551–2558. [Google Scholar] [CrossRef] [Green Version]
- Mitch, W.E.; Sapir, D.G. Evaluation of reduced dialysis frequency using nutritional therapy. Kidney Int. 1981, 20, 122–126. [Google Scholar] [CrossRef] [Green Version]
- Bolasco, P.; Cupisti, A.; Locatelli, F.; Caria, S.; Kalantar-Zadeh, K. Dietary Management of Incremental Transition to Dialysis Therapy: Once-Weekly Hemodialysis Combined with Low-Protein Diet. J. Ren. Nutr. 2016, 26, 352–359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giovannetti, S.; Maggiore, Q. A low-nitrogen diet with proteins of high biological value for severe chronic uremia. Lancet 1964, 1, 1000–1003. [Google Scholar] [CrossRef]
- D’Alessandro, C.; Piccoli, G.B.; Calella, P.; Brunori, G.; Pasticci, F.; Egidi, M.F.; Capizzi, I.; Bellizzi, V.; Cupisti, A. “Dietaly”: Practical issues for the nutritional management of CKD patients in Italy. BMC Nephrol. 2016, 17, 102. [Google Scholar] [CrossRef] [PubMed]
- Lau, W.L.; Vaziri, N.D. Urea, a true uremic toxin: The empire strikes back. Clin. Sci. 2017, 131, 3–12. [Google Scholar] [CrossRef] [Green Version]
- Koppe, L.; Nyam, E.; Vivot, K.; Manning Fox, J.E.; Dai, X.Q.; Nguyen, B.N.; Trudel, D.; Attane, C.; Moulle, V.S.; MacDonald, P.E.; et al. Urea impairs beta cell glycolysis and insulin secretion in chronic kidney disease. J. Clin. Investig. 2016, 126, 3598–3612. [Google Scholar] [CrossRef] [Green Version]
- Delanghe, S.; Delanghe, J.R.; Speeckaert, R.; Van Biesen, W.; Speeckaert, M.M. Mechanisms and consequences of carbamylation. Nat. Rev. Nephrol. 2017, 13, 580–593. [Google Scholar] [CrossRef] [PubMed]
- Shaykh, M.; Pegoraro, A.A.; Mo, W.; Arruda, J.A.; Dunea, G.; Singh, A.K. Carbamylated proteins activate glomerular mesangial cells and stimulate collagen deposition. J. Lab. Clin. Med. 1999, 133, 302–308. [Google Scholar] [CrossRef]
- Sun, J.T.; Yang, K.; Lu, L.; Zhu, Z.B.; Zhu, J.Z.; Ni, J.W.; Han, H.; Chen, N.; Zhang, R.Y. Increased carbamylation level of hdl in end-stage renal disease: Carbamylated-hdl attenuated endothelial cell function. Am. J. Physiol. Ren. Physiol. 2016, 310, F511–F517. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berg, A.H.; Drechsler, C.; Wenger, J.; Buccafusca, R.; Hod, T.; Kalim, S.; Ramma, W.; Parikh, S.M.; Steen, H.; Friedman, D.J.; et al. Carbamylation of serum albumin as a risk factor for mortality in patients with kidney failure. Sci. Trans. Med. 2013, 5, 175ra29. [Google Scholar] [CrossRef] [Green Version]
- Kalim, S.; Trottier, C.A.; Wenger, J.B.; Wibecan, J.; Ahmed, R.; Ankers, E.; Karumanchi, S.A.; Thadhani, R.; Berg, A.H. Longitudinal Changes in Protein Carbamylation and Mortality Risk after Initiation of Hemodialysis. Clin. J. Am. Soc. Nephrol. 2016, 11, 1809–1816. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Di Iorio, B.R.; Marzocco, S.; Bellasi, A.; De Simone, E.; Dal Piaz, F.; Rocchetti, M.T.; Cosola, C.; Di Micco, L.; Gesualdo, L. Nutritional therapy reduces protein carbamylation through urea lowering in chronic kidney disease. Nephrol. Dial. Transplant. 2018, 33, 804–813. [Google Scholar] [CrossRef]
- El-Gamal, D.; Rao, S.P.; Holzer, M.; Hallstrom, S.; Haybaeck, J.; Gauster, M.; Wadsack, C.; Kozina, A.; Frank, S.; Schicho, R.; et al. The urea decomposition product cyanate promotes endothelial dysfunction. Kidney Int. 2014, 86, 923–931. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marzocco, S.; Dal Piaz, F.; Di Micco, L.; Torraca, S.; Sirico, M.L.; Tartaglia, D.; Autore, G.; Di Iorio, B. Very low protein diet reduces indoxyl sulfate levels in chronic kidney disease. Blood Purif. 2013, 35, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Black, A.P.; Anjos, J.S.; Cardozo, L.; Carmo, F.L.; Dolenga, C.J.; Nakao, L.S.; de Carvalho Ferreira, D.; Rosado, A.; Carraro Eduardo, J.C.; Mafra, D. Does Low-Protein Diet Influence the Uremic Toxin Serum Levels from the Gut Microbiota in Nondialysis Chronic Kidney Disease Patients? J. Ren. Nutr. 2018, 28, 208–214. [Google Scholar] [CrossRef]
- Bliss, D.Z.; Stein, T.P.; Schleifer, C.R.; Settle, R.G. Supplementation with gum arabic fiber increases fecal nitrogen excretion and lowers serum urea nitrogen concentration in chronic renal failure patients consuming a low-protein diet. Am. J. Clin. Nutr. 1996, 63, 392–398. [Google Scholar] [CrossRef]
- Meijers, B.K.I.; De Preter, V.; Verbeke, K.; Vanrenterghem, Y.; Evenepoel, P. p-Cresyl sulfate serum concentrations in haemodialysis patients are reduced by the prebiotic oligofructose-enriched inulin. Nephrol. Dial. Transplant. 2010, 25, 219–224. [Google Scholar] [CrossRef] [Green Version]
- Salmean, Y.A.; Segal, M.S.; Langkamp-Henken, B.; Canales, M.T.; Zello, G.A.; Dahl, W.J. Foods with added fiber lower serum creatinine levels in patients with chronic kidney disease. J. Ren. Nutr. 2013, 23, e29–e32. [Google Scholar] [CrossRef]
- Ward, R.A.; Schmidt, B.; Hullin, J.; Hillebrand, G.F.; Samtleben, W. A comparison of on-line hemodiafiltration and high-flux hemodialysis: A prospective clinical study. J. Am. Soc. Nephrol. 2000, 11, 2344–2350. [Google Scholar]
- Bakhtiary, M.; Morvaridzadeh, M.; Agah, S.; Rahimlou, M.; Christopher, E.; Zadro, J.R.; Heshmati, J. Effect of Probiotic, Prebiotic, and Synbiotic Supplementation on Cardiometabolic and Oxidative Stress Parameters in Patients with Chronic Kidney Disease: A Systematic Review and Meta-analysis. Clin. Ther. 2021, 43, e71–e96. [Google Scholar] [CrossRef] [PubMed]
- Morelli, E.; Baldi, R.; Barsotti, G.; Ciardella, F.; Cupisti, A.; Dani, L.; Mantovanelli, A.; Giovannetti, S. Combined therapy for selected patients: Infrequent hemodialysis and nutritional management. Nephron 1987, 47, 161–166. [Google Scholar] [CrossRef]
- Alatriste, P.V.M.; Arronte, R.U.; Espinosa, C.O.G.; Cuevas, M.A.E. Effect of probiotics on human blood urea levels in patients with chronic renal failure. Nutr. Hosp. 2014, 29, 582–590. [Google Scholar]
- Takayama, F.; Taki, K.; Niwa, T. Bifidobacterium in gastro-resistant seamless capsule reduces serum levels of indoxyl sulfate in patients on hemodialysis. Am. J. Kidney Dis. 2003, 41, S142–S145. [Google Scholar] [CrossRef]
- Nakabayashi, I.; Nakamura, M.; Kawakami, K.; Ohta, T.; Kato, I.; Uchida, K.; Yoshida, M. Effects of symbiotic treatment on serum level of p-cresol in hemodialysis patients: A preliminary study. Nephrol. Dial. Transplant. 2011, 26, 1094–1098. [Google Scholar] [CrossRef] [Green Version]
- Rossi, M.; Johnson, D.W.; Xu, H.; Carrero, J.J.; Pascoe, E.; French, C.; Campbell, K.L. Dietary protein-fiber ratio associates with circulating levels of indoxyl sulfate and p-cresyl sulfate in chronic kidney disease patients. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 860–865. [Google Scholar] [CrossRef] [PubMed]
- Keshaviah, P.R.; Emerson, P.F.; Nolph, K.D. Timely initiation of dialysis: A urea kinetic approach. Am. J. Kidney. Dis. 1999, 33, 344–348. [Google Scholar] [CrossRef]
- Duranton, F.; Depner, T.A.; Argilés, À. The saga of two centuries of urea: Nontoxic toxin or vice versa? Semin. Nephrol. 2014, 34, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Eloot, S.; Torremans, A.; De Smet, R.; Marescau, B.; De Wachter, D.; De Deyn, P.P.; Lameire, N.; Verdonk, P.; Vanholder, R. Kinetic behavior of urea is different from that of other water-soluble compounds: The case of the guanidino compounds. Kidney Int. 2005, 67, 1566–1575. [Google Scholar] [CrossRef] [Green Version]
- Caria, S.; Cupisti, A.; Sau, G.; Bolasco, P. The incremental treatment of ESRD: A low-protein diet combined with weekly hemodialysis may be beneficial for selected patients. BMC Nephrol. 2014, 15, 172. [Google Scholar] [CrossRef] [Green Version]
- Nakao, T.; Kanazawa, Y.; Takahashi, T. Once-weekly hemodialysis combined with low-protein and low-salt dietary treatment as a favorable therapeutic modality for selected patients with end-stage renal failure: A prospective observational study in Japanese patients. BMC Nephrol. 2018, 19, 151. [Google Scholar] [CrossRef] [Green Version]
- Kalim, S.; Wald, R.; Yan, A.T.; Goldstein, M.B.; Kiaii, M.; Xu, D.; Berg, D.H.; Clish, C.; Thadhani, R.; Rhee, E.P.; et al. Extended Duration Nocturnal Hemodialysis and Changes in Plasma Metabolite Profiles. Clin. J. Am. Soc. Nephrol. 2018, 13, 436–444. [Google Scholar] [CrossRef] [Green Version]
- Graboski, A.L.; Redinbo, M.R. Gut-Derived Protein-Bound Uremic Toxins. Toxins 2020, 12, 590. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Kestenbaum, B. Proximal Tubular Secretory Clearance: A Neglected Partner of Kidney Function. Clin. J. Am. Soc. Nephrol. 2018, 13, 1291–1296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Snauwaert, E.; Holvoet, E.; Van Biesen, W.; Raes, A.; Glorieux, G.; Vande Walle, J.; Roels, S.; Vanholder, R.; Askiti, V.; Azukaitis, K.; et al. Uremic Toxin Concentrations are Related to Residual Kidney Function in the Pediatric Hemodialysis Population. Toxins 2019, 11, 235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Locatelli, F.; Andrulli, S.; Pontoriero, G.; Di Filippo, S.; Bigi, M.C. Supplemented low-protein diet and once-weekly hemodialysis. Am. J. Kidney Dis. 1994, 24, 192–204. [Google Scholar] [CrossRef]
- Maroni, B.J.; Steinman, T.I.; Mitch, W.E. A method for estimating nitrogen intake of patients with chronic renal failure. Kidney Int. 1985, 27, 58–65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Daugirdas, J.T.; Greene, T.; Depner, T.A.; Leypoldt, J.; Gotch, F.; Schulman, G.; Star, R.; Hemodialysis Study Group. Factors that affect post-dialysis rebound in serum urea concentration, including the rate of dialysis: Results from the HEMO Study. J. Am. Soc. Nephrol. 2004, 15, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Bolasco, P.; Casula, L.; Contu, R.; Cadeddu, M.; Murtas, S. Evaluation of Residual Kidney Function during Once-Weekly Incremental Hemodialysis. Blood Purif. 2021, 50, 246–253. [Google Scholar] [CrossRef]
- Fukumoto, S. FGF23-related hypophosphatemic rickets/osteomalacia: Diagnosis and new treatment. J. Mol. Endocrinol. 2020, 66, R57–R65. [Google Scholar] [CrossRef]
| Reference | Intervention (No. Patients) | Type of Study | Outcome | Findings |
|---|---|---|---|---|
| Morelli E et al. 1987 [70] | OWHD+VLPD (17) vs. Control MHD (8) | Prospective controlled non randomized | Clinical findings and blood chemical abnormalities | Reduction of TAC of urea, phosphate and methylguanidine serum levels |
| Locatelli F et al, 1994 [84] | OWHD+VLPD (84) | Open Cohort Prospective | Nutritional, metabolic, and depurative adequacy. | Good metabolic and depurative adequacy; concerns about dietary adherence, nutritional status and neurological aspects |
| Caria S et al. 2014 [78] | OWHD+LPD (38) vs. Control MHD (30) | Prospective controlled non randomized | Protection of RKF, nutritional, metabolic-depurative Adequacy | Better preservation of RKF and urine volume and lower serum levels of phosphate, urea, β2-Microglobulin, and ERI; cost saving |
| Nakao et al. 2018 [79] | OWHD+LPD (112) vs. Control MHD (30) | Prospective controlled non randomized | Protection of RKF, nutritional- metabolic-depurative Adequacy, costs | Better preservation of RKF and urine volume, lower serum levels of phosphorus, urea, β2-microglobulin, and ERI; cost saving |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cupisti, A.; Bolasco, P.; D’Alessandro, C.; Giannese, D.; Sabatino, A.; Fiaccadori, E. Protection of Residual Renal Function and Nutritional Treatment: First Step Strategy for Reduction of Uremic Toxins in End-Stage Kidney Disease Patients. Toxins 2021, 13, 289. https://0-doi-org.brum.beds.ac.uk/10.3390/toxins13040289
Cupisti A, Bolasco P, D’Alessandro C, Giannese D, Sabatino A, Fiaccadori E. Protection of Residual Renal Function and Nutritional Treatment: First Step Strategy for Reduction of Uremic Toxins in End-Stage Kidney Disease Patients. Toxins. 2021; 13(4):289. https://0-doi-org.brum.beds.ac.uk/10.3390/toxins13040289
Chicago/Turabian StyleCupisti, Adamasco, Piergiorgio Bolasco, Claudia D’Alessandro, Domenico Giannese, Alice Sabatino, and Enrico Fiaccadori. 2021. "Protection of Residual Renal Function and Nutritional Treatment: First Step Strategy for Reduction of Uremic Toxins in End-Stage Kidney Disease Patients" Toxins 13, no. 4: 289. https://0-doi-org.brum.beds.ac.uk/10.3390/toxins13040289





