Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update
Abstract
:1. Introduction
2. Historical Background and Development
3. Chemistry and Types of PMMA
3.1. Heat-Cured PMMA
3.2. Microwave-Cured PMMA
3.3. Cold-Cured PMMA
3.4. Light-Cured PMMA
4. Manipulation
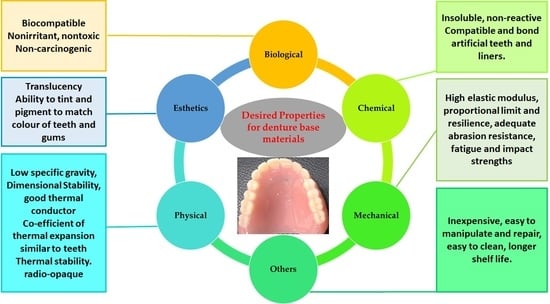
5. Properties of PMMA
5.1. Biological Properties of PMMA
5.2. Physical Properties of PMMA
5.3. Mechanical Properties of PMMA
5.4. Chemical Properties of PMMA
6. Applications of PMMA
6.1. Denture Bases, Liners, and Reliners
6.2. Artificial Teeth
6.3. Temporary Crowns and Bridges
6.4. Repair of Dentures
6.5. Obturators
6.6. Computer-Aided Design and Manufacturing (CAD/CAM) PMMA
6.7. Miscellaneous Applications
7. Modifications of PMMA
7.1. Mechanical Reinforcement Using Fibers
7.2. Mechanical Reinforcement Using Particles
7.3. Chemical Modification of PMMA
7.4. Antimicrobial Functionalization of PMMA
8. Conclusions and Future Trends
Funding
Acknowledgments
Conflicts of Interest
References
- Rokaya, D.; Srimaneepong, V.; Sapkota, J.; Qin, J.; Siraleartmukul, K.; Siriwongrungson, V. Polymeric materials and films in dentistry: An overview. J. Adv. Res. 2018, 14, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; He, L.; Zhu, B.; Li, J.; Li, J. Advances in polymeric materials for dental applications. Polym. Chem. 2017, 8, 807–823. [Google Scholar] [CrossRef]
- Imazato, S.; Ma, S.; Chen, J.; Xu, H.H.K. Therapeutic polymers for dental adhesives: Loading resins with bio-active components. Dent. Mater. 2014, 30, 97–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Najeeb, S.; Zafar, M.S.; Khurshid, Z.; Siddiqui, F. Applications of polyetheretherketone (PEEK) in oral implantology and prosthodontics. J. Prosthodont. Res. 2016, 60, 12–19. [Google Scholar] [CrossRef]
- Kwon, J.; Kim, Y.H.; Choi, E.H.; Kim, K. Development of ultra-hydrophilic and non-cytotoxic dental vinyl polysiloxane impression materials using a non-thermal atmospheric-pressure plasma jet. J. Phys. D 2013, 46, 195201. [Google Scholar] [CrossRef]
- Ohkawa, K.; Hayashi, S.; Kameyama, N.; Yamamoto, H.; Yamaguchi, M.; Kimoto, S.; Kurata, S.; Shinji, H. Synthesis of collagen-like sequential polypeptides containing O-phospho-L-hydroxyproline and preparation of electrospun composite fibers for possible dental application. Macromol. Biosci. 2009, 9, 79–92. [Google Scholar] [CrossRef]
- Deb, S. Polymers in dentistry. J. Eng. Med. 1998, 212, 453–464. [Google Scholar] [CrossRef]
- Alqurashi, H.; Khurshid, Z.; Azeem Ul Yaqin, S.; Rashid Habib, S.; Rokaya, D.; Sohail Zafar, M. Polyetherketoneketone (PEKK): An emerging biomaterial for oral implants and dental prostheses. J. Adv. Res. 2020, in press. [Google Scholar] [CrossRef]
- Hassan, M.; Asghar, M.; Din, S.U.; Zafar, M.S. Chapter 8. In Thermoset Polymethacrylate-Based Materials for Dental Applications; Elsevier: Amsterdam, The Netherlands, 2019; pp. 273–308. [Google Scholar]
- Nejatian, T.; Pezeshki, S.; Yaqin Syed, A.U. Acrylic denture base materials. In 5 Advanced Dental Biomaterials; Khurshid, Z., Najeeb, S., Zafar, M.S., Sefat, F., Eds.; Woodhead Publishing: Cambridge, UK, 2019; pp. 79–104. [Google Scholar]
- Sakaguchi, R.L.; Powers, J.M. Craig’s Restorative Dental Materials; Elsevier/Mosby: Philadelphia, PA, USA, 2012. [Google Scholar]
- Zafar, M.S.; Ahmed, N. Nano-mechanical evaluation of dental hard tissues using indentation technique. World Appl. Sci. J. 2013, 28, 1393–1399. [Google Scholar]
- Chang, M.; Hung, C.; Chen, W.; Tseng, S.; Chen, Y.; Wang, J. Effects of pontic span and fiber reinforcement on fracture strength of multi-unit provisional fixed partial dentures. J. Dent. Sci. 2019, 14, 309–317. [Google Scholar] [CrossRef]
- Al-Thobity, A.M. The impact of polymerization technique and glass-fiber reinforcement on the flexural properties of denture base resin material. Eur. J. Dent. 2020, 14, 92–99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moreno-Maldonado, V.; Acosta-Torres, L.; Barceló-Santana, F.; Vanegas-Lancón, R.; Plata-Rodríguez, M.; Castano, V. Fiber-reinforced nanopigmented poly (methyl methacrylate) as improved denture base. J. Appl. Polym. Sci. 2012, 126, 289–296. [Google Scholar] [CrossRef]
- Hamouda, I.M.; Beyari, M.M. Addition of glass fibers and titanium dioxide nanoparticles to the acrylic resin denture base material: Comparative study with the conventional and high impact types. Oral Health Dent. Manag. 2014, 13, 107–112. [Google Scholar] [PubMed]
- Ismaeel, I.J.; Alalwan, H.K.; Mustafa, M. The effect of the addition of silanated poly propylene fiber to polymethylmethacrylate denture base material on some of its mechanical properties. J. Baghdad Coll. Dent. 2015, 27, 40–47. [Google Scholar] [CrossRef]
- Chen, S.; Liang, W.; Yen, P. Reinforcement of acrylic denture base resin by incorporation of various fibers. J. Biomed. Mater. 2001, 58, 203–208. [Google Scholar] [CrossRef]
- Vallittu, P.K.; Lassila, V.P.; Lappalainen, R. Acrylic resin-fiber composite—Part I: The effect of fiber concentration on fracture resistance. J. Prosthet. Dent. 1994, 71, 607–612. [Google Scholar] [CrossRef]
- Manley, T.R.; Bowman, A.J.; Cook, M. Denture bases reinforced with carbon fibres. Br. Dent. J. 1979, 146, 25. [Google Scholar] [CrossRef]
- Yu, S.; Lee, Y.; Oh, S.; Cho, H.; Oda, Y.; Bae, J. Reinforcing effects of different fibers on denture base resin based on the fiber type, concentration, and combination. Dent. Mater. J. 2012, 31, 1039–1046. [Google Scholar] [CrossRef] [Green Version]
- Ladizesky, N.; Cheng, Y.; Chow, T.; Ward, I. Acrylic resin reinforced with chopped high performance polyethylene fiber-properties and denture construction. Dent. Mater. 1993, 9, 128–135. [Google Scholar] [CrossRef]
- Ghafari, T.; Hamedi, R.F.; Ezzati, B. Does addition of silver nanoparticles to denture base resin increase its thermal conductivity? J. Dent. Sch. 2014, 32, 144. [Google Scholar]
- Hamedi-Rad, F.; Ghaffari, T.; Rezaii, F.; Ramazani, A. Effect of nanosilver on thermal and mechanical properties of acrylic base complete dentures. J. Dent. (Tehran) 2014, 11, 495–505. [Google Scholar]
- Jasim, B.S.; Ismail, I.J. The effect of silanized alumina nano-fillers addition on some physical and mechanical properties of heat cured polymethyl methacrylate denture base material. J. Baghdad Coll. Dent. 2014, 26, 18–23. [Google Scholar] [CrossRef]
- Chaijareenont, P.; Takahashi, H.; Nishiyama, N.; Arksornnukit, M. Effect of different amounts of 3-methacryloxypropyltrimethoxysilane on the flexural properties and wear resistance of alumina reinforced PMMA. Dent. Mater. J. 2012, 31, 623–628. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tham, W.; Chow, W.; Ishak, Z.M. Simulated body fluid and water absorption effects on poly (methyl methacrylate)/hydroxyapatite denture base composites. Express Polym. Lett. 2010, 4, 517–528. [Google Scholar] [CrossRef]
- Aldabib, J.M.; Ishak, Z.A.M. Effect of hydroxyapatite filler concentration on mechanical properties of poly (methyl methacrylate) denture base. SN Appl. Sci. 2020, 2, 1–14. [Google Scholar] [CrossRef] [Green Version]
- De Souza Leão, R.; de Moraes, S.L.D.; de Luna Gomes, J.M.; Lemos, C.A.A.; da Silva Casado, B.G.; do Egito Vasconcelos, B.C.; Pellizzer, E.P. Influence of addition of zirconia on PMMA: A systematic review. Mater. Sci. Eng. C 2020, 106, 110292. [Google Scholar]
- Zidan, S.; Silikas, N.; Haider, J.; Alhotan, A.; Jahantigh, J.; Yates, J. Evaluation of equivalent flexural strength for complete removable dentures made of zirconia-impregnated PMMA nanocomposites. Materials 2020, 13, 2580. [Google Scholar] [CrossRef]
- Gad, M.M.; Rahoma, A.; Al-Thobity, A.M.; ArRejaie, A.S. Influence of incorporation of ZrO2 nanoparticles on the repair strength of polymethyl methacrylate denture bases. Int. J. Nanomed. 2016, 11, 5633–5643. [Google Scholar] [CrossRef] [Green Version]
- Salih, S.I.; Oleiwi, J.K.; Hamad, Q.A. Investigation of fatigue and compression strength for the PMMA reinforced by different system for denture applications. Int. J. Biomed. Mater. Res. 2015, 3, 5–13. [Google Scholar] [CrossRef]
- Gad, M.M.A.; Abualsaud, R.; Al-Thobity, A.M.; Almaskin, D.F.; AlZaher, Z.A.; Abushowmi, T.H.; Qaw, M.S.; Akhtar, S.; Al-Harbi, F.A. Effect of SiO2 nanoparticles addition on the flexural strength of repaired acrylic denture base. Eur. J. Dent. 2020, 14, 019–023. [Google Scholar] [CrossRef]
- Safi, I.N. Evaluation the effect of nano-fillers (TiO2, Al2O3, SiO2) addition on glass transition temperature, E-Moudulus and coefficient of thermal expansion of acrylic denture base material. J. Baghdad Coll. Dent. 2014, 26, 37–41. [Google Scholar] [CrossRef]
- Balos, S.; Puskar, T.; Potran, M.; Milekic, B.; Djurovic Koprivica, D.; Laban Terzija, J.; Gusic, I. Modulus, strength and cytotoxicity of PMMA-silica nanocomposites. Coatings 2020, 10, 583. [Google Scholar] [CrossRef]
- Balos, S.; Pilic, B.; Markovic, D.; Pavlicevic, J.; Luzanin, O. Poly (methyl-methacrylate) nanocomposites with low silica addition. J. Prosthet. Dent. 2014, 111, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Alamgir, M.; Mallick, A.; Nayak, G.; Tiwari, S.K. Development of PMMA/TiO2 nanocomposites as excellent dental materials. J. Mech. Sci. Technol. 2019, 33, 4755–4760. [Google Scholar] [CrossRef]
- Wang, R.; Tao, J.; Yu, B.; Dai, L. Characterization of multiwalled carbon nanotube-polymethyl methacrylate composite resins as denture base materials. J. Prosthet. Dent. 2014, 111, 318–326. [Google Scholar] [CrossRef]
- Qasim, S.B.; Al Kheraif, A.A.; Ramakrishaniah, R. An investigation into the impact and flexural strength of light cure denture resin reinforced with carbon nanotubes. World Appl. Sci. J. 2012, 18, 808–812. [Google Scholar]
- Mahmood, W.S. The effect of incorporating carbon nanotubes on impact, transverse strength, hardness, and roughness to high impact denture base material. J. Baghdad Coll. Dent. 2015, 27, 96–99. [Google Scholar] [CrossRef]
- Turagam, N.; Prasad Mudrakola, D. Effect of micro-additions of carbon nanotubes to polymethylmethacrylate on reduction in polymerization shrinkage. J. Prosthodont. Implant. Esthet. Reconstr. Dent. 2013, 22, 105–111. [Google Scholar] [CrossRef]
- Wang, R.; Kayacan, R.; Küçükeşmen, C. Nanotubes/polymethyl methacrylate composite resins as denture base materials. In Carbon Nanomaterials for Biomedical Applications; Springer: Berlin/Heidelberg, Germany, 2016; pp. 227–240. [Google Scholar]
- Andreopoulos, A.; Papanicolaou, G. Rubber-modified polymer composites. J. Mater. Sci. 1987, 22, 3417–3420. [Google Scholar] [CrossRef]
- Redtenbacher, J. Ueber die zerlegungsprodukte des glyceryloxydes durch trockene destillation. Justus Liebigs Ann. Chem. 1843, 47, 113–148. [Google Scholar] [CrossRef]
- Rueggeberg, F.A. From vulcanite to vinyl, a history of resins in restorative dentistry. J. Prosthet. Dent. 2002, 87, 364–379. [Google Scholar] [CrossRef] [PubMed]
- Neher, H.T. Acrylic resins. Ind. Eng. Chem. 1936, 28, 267–271. [Google Scholar] [CrossRef]
- Peyton, F.A. History of resins in dentistry. Dent. Clin. North Am. 1975, 19, 211–222. [Google Scholar] [PubMed]
- DiMaio, F.R. The science of bone cement: A historical review. Orthopedics 2002, 25, 1399–1407. [Google Scholar]
- Kraft, J. Polymethylmethacrylate—A review. J. Foot Surg. 1977, 16, 66–68. [Google Scholar]
- Frazer, R.Q.; Byron, R.T.; Osborne, P.B.; West, K.P. PMMA: An essential material in medicine and dentistry. J. Long. Term. Eff. Med. 2005, 15, 629–639. [Google Scholar] [CrossRef] [Green Version]
- Zidan, S.; Silikas, N.; Alhotan, A.; Haider, J.; Yates, J. Investigating the mechanical properties of ZrO2-impregnated PMMA nanocomposite for denture-based applications. Materials 2019, 12, 1344. [Google Scholar] [CrossRef] [Green Version]
- Chen, S.; Yang, J.; Jia, Y.; Lu, B.; Ren, L. TiO2 and PEEK reinforced 3D printing PMMA composite resin for dental denture base applications. Nanomaterials 2019, 9, 1049. [Google Scholar] [CrossRef] [Green Version]
- Shakeri, F.; Nodehi, A.; Atai, M. PMMA/double-modified organoclay nanocomposites as fillers for denture base materials with improved mechanical properties. J. Mech. Behav. Biomed. Mater. 2019, 90, 11–19. [Google Scholar] [CrossRef]
- Najeeb, S.; Khurshid, Z.; Agwan, A.S.; Zafar, M.S.; Alrahabi, M.; Qasim, S.B.; Sefat, F. Dental applications of nanodiamonds. Sci. Adv. Mater. 2016, 8, 2064–2070. [Google Scholar] [CrossRef] [Green Version]
- Johnson, W.W. The history of prosthetic dentistry. J. Prosthet. Dent. 1959, 9, 841–846. [Google Scholar] [CrossRef]
- Gautam, R.; Singh, R.D.; Sharma, V.P.; Siddhartha, R.; Chand, P.; Kumar, R. Biocompatibility of polymethylmethacrylate resins used in dentistry. J. Biomed. Mater. Res. Part B 2012, 100, 1444–1450. [Google Scholar] [CrossRef] [PubMed]
- Khindria, S.; Mittal, S.; Sukhija, U. Evolution of denture base materials. J. Indian Prosthodont. Soc. 2009, 9, 64. [Google Scholar]
- Kedjarune, U.; Charoenworaluk, N.; Koontongkaew, S. Release of methyl methacrylate from heat-curved and autopolymerized resins: Cytotoxicity testing related to residual monomer. Aust. Dent. J. 1999, 44, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Lang, B.R. The use of gold in construction of mandibular denture bases. J. Prosthet. Dent. 1974, 32, 398–404. [Google Scholar] [CrossRef]
- Murray, M.D.; Darvell, B.W. The evolution of the complete denture base. Theories of complete denture retention—A review. Part 1. Aust. Dent. J. 1993, 38, 216–219. [Google Scholar] [CrossRef]
- Komal, L.; Mahesh, V. 19th century denture base materials revisited. Off. Publ. Am. Acad. Hist. Dent. 2011, 59, 1–11. [Google Scholar]
- Young, B.C. A Comparison of Polymeric Denture Base Materials. Ph.D. Thesis, University of Glasgow, Glasgow, UK, 2010. [Google Scholar]
- Sasaki, H.; Hamanaka, I.; Takahashi, Y.; Kawaguchi, T. Effect of long-term water immersion or thermal shock on mechanical properties of high-impact acrylic denture base resins. Dent. Mater. J. 2016, 35, 204–209. [Google Scholar] [CrossRef] [Green Version]
- Takahashi, Y.; Hamanaka, I.; Shimizu, H. Flexural properties of denture base resins subjected to long-term water immersion. Acta Odontol. Scand. 2013, 71, 716–720. [Google Scholar] [CrossRef]
- Narva, K.K.; Lassila, L.V.; Vallittu, P.K. The static strength and modulus of fiber reinforced denture base polymer. Dent. Mater. 2005, 21, 421–428. [Google Scholar] [CrossRef]
- Nejatian, T.; Nathwani, N.; Taylor, L.; Sefat, F. Denture base composites: Effect of surface modified nano-and micro-particulates on mechanical properties of polymethyl methacrylate. Materials 2020, 13, 307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gad, M.M.; Abualsaud, R.; Al-Thobity, A.M.; Baba, N.Z.; Al-Harbi, F.A. Influence of addition of different nanoparticles on the surface properties of poly (methylmethacrylate) denture base material. J. Prosthodont. 2020, 29, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Gad, M.M.; Rahoma, A.; Abulsaud, R.; Al-Thobity, A.M.; Akhtar, S.; Helal, M.A.; AL-Harbi, F.A. Impact of different surface treatments and repair material reinforcement on the flexural strength of repaired PMMA denture base material. Dent. Mater. J. 2020, 2018–2436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Harbi, F.A.; Abdel-Halim, M.S.; Gad, M.M.; Fouda, S.M.; Baba, N.Z.; AlRumaih, H.S.; Akhtar, S. Effect of nanodiamond addition on flexural strength, impact strength, and surface roughness of PMMA denture base. J. Prosthodont. 2019, 28, e417–e425. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elshereksi, N.; Muchtar, A.; Azhari, C. Effects of nanobarium titanate on physical and mechanical properties of poly (methyl methacrylate) denture base nanocomposites. Polym. Polym. Compos. 2020. [Google Scholar] [CrossRef]
- Raszewski, Z.; Nowakowska-Toporowska, A.; Weżgowiec, J.; Nowakowska, D.; Więckiewicz, W. Influence of silanized silica and silanized feldspar addition on the mechanical behavior of polymethyl methacrylate resin denture teeth. J. Prosthet. Dent. 2020, 123, 647.e1–647.e7. [Google Scholar] [CrossRef]
- Abushowmi, T.H.; AlZaher, Z.A.; Almaskin, D.F.; Qaw, M.S.; Abualsaud, R.; Akhtar, S.; Al-Thobity, A.M.; Al-Harbi, F.A.; Gad, M.M.; Baba, N.Z. Comparative effect of glass fiber and nano-filler addition on denture repair strength. J. Prosthodont. 2020, 29, 261–268. [Google Scholar] [CrossRef]
- Alqahtani, M. Effect of hexagonal boron nitride nanopowder reinforcement and mixing methods on physical and mechanical properties of self-cured PMMA for dental applications. Materials 2020, 13, 2323. [Google Scholar] [CrossRef]
- Helal, M.A.; Yang, B.; Saad, E.; Abas, M.; Al-kholy, M.R.; Imam, A.Y.; Gad, M.M. Effect of SiO2 and Al2O3 nanoparticles on wear resistance of PMMA acrylic denture teeth. Braz. Dent. Sci. 2020, 23, 12. [Google Scholar]
- Jagger, D.; Harrison, A.; Jandt, K. The reinforcement of dentures. J. Oral Rehabil. 1999, 26, 185–194. [Google Scholar] [CrossRef]
- Alhareb, A.; Akil, H.; Ahmad, Z. Mechanical properties of PMMA denture base reinforced by nitrile rubber particles with Al2O3/YSZ fillers. Procedia Manuf. 2015, 2, 301–306. [Google Scholar] [CrossRef] [Green Version]
- Ali, U.; Karim, K.J.B.A.; Buang, N.A. A Review of the properties and applications of poly (methyl methacrylate) (PMMA). Polym. Rev. 2015, 55, 678–705. [Google Scholar] [CrossRef]
- Anusavice, K.J.; Shen, C.; Rawls, H.R. Phillips’ Science of Dental Materials; Elsevier Health Sciences: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Swaney, A.C.; Paffenbarger, G.C.; Caul, H.J.; Sweeney, W. American dental association specification No. 12 for denture base resin: Second revision. J. Am. Dent. Assoc. 1953, 46, 54–66. [Google Scholar] [CrossRef] [PubMed]
- Council on dental materials and devices. Revised american dental association specification no. 12 for denture base polymers. J. Am. Dent. Assoc. 1975, 90, 451–458. [Google Scholar] [CrossRef]
- ISO. ISO 20795–1:2013 Dentistry-Base Polymers-Part 1: Denture Base Polymers. Available online: https://www.iso.org/standard/62277.html (accessed on 5 October 2020).
- Alla, R.; Raghavendra, K.; Vyas, R.; Konakanchi, A. Conventional and contemporary polymers for the fabrication of denture prosthesis: Part I–overview, composition and properties. Int. J. Appl. Dent. Sci. 2015, 1, 82. [Google Scholar]
- Harrison, A.; Huggett, R. Effect of the curing cycle on residual monomer levels of acrylic resin denture base polymers. J. Dent. 1992, 20, 370–374. [Google Scholar] [CrossRef]
- Bartoloni, J.; Murchison, D.; Wofford, D.; Sarkar, N. Degree of conversion in denture base materials for varied polymerization techniques 1. J. Oral Rehabil. 2000, 27, 488–493. [Google Scholar] [CrossRef]
- Jerolimov, V.; Brooks, S.; Huggett, R.; Bates, J. Rapid curing of acrylic denture-base materials. Dent. Mater. 1989, 5, 18–22. [Google Scholar] [CrossRef]
- Memon, M.S.; Yunus, N.; Razak, A.A.A.; Memon, M.; Yunus, N.; Razak, A. Some mechanical properties of a highly cross-linked, microwave-polymerized, injection-molded denture base polymer. Int. J. Prosthodont. 2001, 14, 214–218. [Google Scholar]
- Tandon, R.; Gupta, S.; Agarwal, S.K. Denture base materials: From past to future. Indian J. Dent. Sci. 2010, 2, 33–39. [Google Scholar]
- McCabe, J.F.; Walls, A. Applied Dental Materials; John Wiley and Sons: Chichester, UK, 2013. [Google Scholar]
- van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, M. Mechanical properties enhancement of self-cured PMMA reinforced with zirconia and boron nitride nanopowders for high-performance dental materials. J. Mech. Behav. Biomed. Mater. 2020, 110, 103937. [Google Scholar] [CrossRef] [PubMed]
- Shintani, H.; Inoue, T.; Yamaki, M. Analysis of camphorquinone in visible light-cured composite resins. Dent. Mater. 1985, 1, 124–126. [Google Scholar] [CrossRef]
- Park, Y.J.; Chae, K.H.; Rawls, H.R. Development of a new photoinitiation system for dental light-cure composite resins. Dent. Mater. 1999, 15, 120–127. [Google Scholar] [CrossRef]
- Ogle, R.E.; Sorensen, S.E.; Lewis, E.A. A new visible light-cured resin system applied to removable prosthodontics. J. Prosthet. Dent. 1986, 56, 497–506. [Google Scholar] [CrossRef]
- Takamata, T.; Setcos, J.C. Resin denture bases: Review of accuracy and methods of polymerization. Int. J. Prosthodont. 1989, 2, 555–562. [Google Scholar]
- Skinner, E.W. Acrylic denture base materials: Their physical properties and manipulation. J. Prosthet. Dent. 1951, 1, 161–167. [Google Scholar] [CrossRef]
- Nogueira, S.S.; Ogle, R.E.; Davis, E.L. Comparison of accuracy between compression-and injection-molded complete dentures. J. Prosthet. Dent. 1999, 82, 291–300. [Google Scholar] [CrossRef]
- Gharechahi, J.; Asadzadeh, N.; Shahabian, F.; Gharechahi, M. Dimensional changes of acrylic resin denture bases: Conventional versus injection-molding technique. J. Dent. (Tehran) 2014, 11, 398–405. [Google Scholar]
- Zafar, M.S.; Ahmed, N. Nanoindentation and surface roughness profilometry of poly methyl methacrylate denture base materials. Technol. Health Care 2014, 22, 573–581. [Google Scholar] [CrossRef]
- Vallittu, P.K.; Miettinen, V.; Alakuijala, P. Residual monomer content and its release into water from denture base materials. Dent. Mater. 1995, 11, 338–342. [Google Scholar] [CrossRef]
- Elwakiel, N.; El-Sayed, Y.; Elkafrawy, H. Synthesis, Characterization of Ag and Sn2 complexes and their applications to improve the biological and mechanical properties of denture base materials. J. Mol. Struct. 2020, 1219, 128521. [Google Scholar] [CrossRef]
- Raszewski, Z. Influence of polymerization method on the cytotoxicity of three different denture base acrylic resins polymerized in different methods. Saudi J. Biol. Sci. 2020, 27, 2612–2616. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Su, Q.; Wang, C.; Cheng, G.; Zhu, R.; Shi, J.; Yao, K. Synthesis and biological evaluation of PMMA/MMT nanocomposite as denture base material. J. Mater. Sci. Mater. Med. 2011, 22, 1063–1071. [Google Scholar] [CrossRef]
- Soygun, K.; Bolayir, G.; Boztug, A. Mechanical and thermal properties of polyamide versus reinforced PMMA denture base materials. J. Adv. Prosthodont. 2013, 5, 153–160. [Google Scholar] [CrossRef] [Green Version]
- Asar, N.V.; Albayrak, H.; Korkmaz, T.; Turkyilmaz, I. Influence of various metal oxides on mechanical and physical properties of heat-cured polymethyl methacrylate denture base resins. J. Adv. Prosthodont. 2013, 5, 241–247. [Google Scholar] [CrossRef] [Green Version]
- Polychronakis, N.; Dimitriadi, M.; Ioannidis, A.; Papadopoulos, T. The effect of different cooling procedures on mechanical properties of denture base materials measured by instrumented indentation testing. J. Prosthodont. Res. 2020, 64, 326–331. [Google Scholar] [CrossRef]
- Rickman, L.J.; Padipatvuthikul, P.; Satterthwaite, J.D. Contemporary denture base resins: Part 1. Dent. Update 2012, 39, 25–30. [Google Scholar] [CrossRef] [Green Version]
- Mark, J.E. Physical Properties of Polymers Handbook, 1076; Springer: New York, NY, USA, 2007; pp. 3–8. [Google Scholar]
- Kutz, M. Handbook of Materials Selection; John Wiley and Sons: Hoboken, NJ, USA, 2002; p. 341. [Google Scholar]
- Braun, K.N.; Mello, J.N.; Rached, R.; Del Bel Cury, A. Surface texture and some properties of acrylic resins submitted to chemical polishing. J. Oral Rehabil. 2003, 30, 91–98. [Google Scholar] [CrossRef]
- Jorge, J.H.; Giampaolo, E.T.; Machado, A.L.; Vergani, C.E. Cytotoxicity of denture base acrylic resins: A literature review. J. Prosthet. Dent. 2003, 90, 190–193. [Google Scholar] [CrossRef]
- Lung, C.; Darvell, B. Minimization of the inevitable residual monomer in denture base acrylic. Dent. Mater. 2005, 21, 1119–1128. [Google Scholar] [CrossRef] [PubMed]
- Thaitammayanon, C.; Sirichompun, C.; Wiwatwarrapan, C. Ultrasonic treatment reduced residual monomer in methyl methacrylate-based orthodontic base-plate materials. Dent. Oral. Craniofac. Res. 2018, 4, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Vallittu, P.K.; Ruyter, I.E.; Buykuilmaz, S. Effect of polymerization temperature and time on the residual monomer content of denture base polymers. Eur. J. Oral Sci. 1998, 106, 588–593. [Google Scholar] [CrossRef]
- Doǧan, A.; Bek, B.; Cevik, N.; Usanmaz, A. The effect of preparation conditions of acrylic denture base materials on the level of residual monomer, mechanical properties and water absorption. J. Dent. 1995, 23, 313–318. [Google Scholar] [CrossRef]
- Leggat, P.A.; Kedjarune, U. Toxicity of methyl methacrylate in dentistry. Int. Dent. J. 2003, 53, 126–131. [Google Scholar] [CrossRef]
- Latief, A. Sorption and Solubility of a Denture Base Acrylic. Master’s Thesis, Cape Peninsula University of Technology, Cape Town, South Africa, 2012. [Google Scholar]
- Miettinen, V.M.; Vallittu, P.K. Water sorption and solubility of glass fiber-reinforced denture polymethyl methacrylate resin. J. Prosthet. Dent. 1997, 77, 531–534. [Google Scholar] [CrossRef]
- Bayraktar, G.; Guvener, B.; Bural, C.; Uresin, Y. Influence of polymerization method, curing process, and length of time of storage in water on the residual methyl methacrylate content in dental acrylic resins. J. Biomed. Mater. 2006, 76, 340–345. [Google Scholar] [CrossRef]
- Tuna, S.H.; Keyf, F.; Gumus, H.O.; Uzun, C. The evaluation of water sorption/solubility on various acrylic resins. Eur. J. Dent. 2008, 2, 191–197. [Google Scholar] [CrossRef] [Green Version]
- Saini, R.; Kotian, R.; Madhyastha, P.; Srikant, N. Comparative study of sorption and solubility of heat-cure and self-cure acrylic resins in different solutions. Indian J. Dent. Res. 2016, 27, 288–294. [Google Scholar]
- Van Noort, R.; Barbour, M.E. Introduction to Dental Materials 4; Elsevier Health Sciences: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Sagsoz, N.P.; Yanıkoglu, N.; Ulu, H.; Bayındır, F. Color changes of polyamid and polymetyhl methacrylate denture base materials. Open J. Stomatol. 2014, 4, 489–496. [Google Scholar] [CrossRef] [Green Version]
- Alp, G.; Johnston, W.M.; Yilmaz, B. Optical properties and surface roughness of prepolymerized poly (methyl methacrylate) denture base materials. J. Prosthet. Dent. 2019, 121, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Scotti, R.; Mascellani, S.C.; Forniti, F. The in vitro color stability of acrylic resins for provisional restorations. Int. J. Prosthodont. 1997, 10, 164–168. [Google Scholar] [PubMed]
- Ganzarolli, S.M.; Nunes de Mello, J.A.; Shinkai, R.S.; Del Bel Cury, A. A Internal adaptation and some physical properties of methacrylate-based denture base resins polymerized by different techniques. J. Biomed. Mater. 2007, 82, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Safarabadi, M.; Khansari, N.; Rezaei, A. An experimental investigation of HA/AL2O3 nanoparticles on mechanical properties of restoration materials. Eng. Solid Mech. 2014, 2, 173–182. [Google Scholar] [CrossRef]
- Chandler, H.; Bowen, R.; Paffenbarger, G. Development of a radiopaque denture base material. J. Biomed. Mater. Res. 1971, 5, 253–265. [Google Scholar] [CrossRef]
- McCabe, J.; Wilson, H. A radio-opaque denture material. J. Dent. 1976, 4, 211–217. [Google Scholar] [CrossRef]
- Aldabib, J. Reinforcement of poly (methyl methacrylate) denture base material. Dent. Med. J. 2020, 2, 46–53. [Google Scholar]
- Lang, L.A.; Mattie, P.A.; Rawis, H.R. The effect of triphenylbismuth on the radiopacity and performance properties of compression-and injection-molded denture resins. J. Prosthodont. 2000, 9, 23–29. [Google Scholar] [CrossRef]
- Alhareb, A.; Akil, H.; Ahmad, Z. Influence of Al2O3/Y-TSZ mixture as filler loading on the radiopacity of PMMA denture base composites. Procedia Chem. 2016, 19, 646–650. [Google Scholar] [CrossRef] [Green Version]
- Mattie, P.A.; Rawls, H.R.; Cabasso, I. Development of a radiopaque, autopolymerizing dental acrylic resin. J. Prosthodont. 1994, 3, 213–218. [Google Scholar] [CrossRef]
- Bloodworth, K.E.; Render, P.J. Dental acrylic resin radiopacity: Literature review and survey of practitioners’ attitudes. J. Prosthet. Dent. 1992, 67, 121–123. [Google Scholar] [CrossRef]
- Bangera, M.K.; Kotian, R.; Ravishankar, N. Effect of titanium dioxide nanoparticle reinforcement on flexural strength of denture base resin: A systematic review and meta-analysis. Jpn. Dent. Sci. Rev. 2020, 56, 68–76. [Google Scholar] [CrossRef] [PubMed]
- AlQahtani, M.; Haralur, S.B. Influence of different repair acrylic resin and thermocycling on the flexural strength of denture base resin. Medicina 2020, 56, 50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kawaguchi, T.; Lassila, L.V.; Baba, H.; Tashiro, S.; Hamanaka, I.; Takahashi, Y.; Vallittu, P.K. Effect of cellulose nanofiber content on flexural properties of a model, thermoplastic, injection-molded, polymethyl methacrylate denture base material. J. Mech. Behav. Biomed. Mater. 2020, 102, 103513. [Google Scholar] [CrossRef] [PubMed]
- Hannon, S.A.; Hussain, W.A.; Hussain, S.M. Studying the impact strength of layered denture base resin. Iraqi J. Phys. 2020, 18, 25–32. [Google Scholar] [CrossRef]
- Vallittu, P.K.; Vojtkova, H.; Lassila, V.P. Impact strength of denture polymethyl methacrylate reinforced with continuous glass fibers or metal wire. Acta Odontol. Scand. 1995, 53, 392–396. [Google Scholar] [CrossRef]
- Mowade, T.K.; Dange, S.P.; Thakre, M.B.; Kamble, V.D. Effect of fiber reinforcement on impact strength of heat polymerized polymethyl methacrylate denture base resin: In vitro study and SEM analysis. J. Adv. Prosthodont. 2012, 4, 30–36. [Google Scholar] [CrossRef] [Green Version]
- Faot, F.; Costa, M.A.; Cury, A.A.D.B.; Garcia, R.C.R. Impact strength and fracture morphology of denture acrylic resins. J. Prosthet. Dent. 2006, 96, 367–373. [Google Scholar] [CrossRef]
- Abdulrazzaq Naji, S.; Behroozibakhsh, M.; Jafarzadeh Kashi, T.S.; Eslami, H.; Masaeli, R.; Mahgoli, H.; Tahriri, M.; Ghavvami Lahiji, M.; Rakhshan, V. Effects of incorporation of 2.5 and 5 wt% TiO2 nanotubes on fracture toughness, flexural strength, and microhardness of denture base poly methyl methacrylate (PMMA). J. Adv. Prosthodont. 2018, 10, 113–121. [Google Scholar] [CrossRef]
- Abdel-Karim, U.M.; Kenawy, E.S. Synthesis of zirconia, organic and hybrid nanofibers for reinforcement of polymethyl methacrylate denture base: Evaluation of flexural strength and modulus, fracture toughness and impact strength. Tanta Dent. J. 2019, 16, 12–20. [Google Scholar]
- Mousavi, A.; Aliha, M.; Imani, D. Effects of biocompatible nanofillers on mixed-mode I and II fracture toughness of PMMA base dentures. J. Mech. Behav. Biomed. Mater. 2020, 103, 103566. [Google Scholar] [CrossRef] [PubMed]
- Ali, I.L.; Yunus, N.; Abu-Hassan, M.I. Hardness, flexural strength, and flexural modulus comparisons of three differently cured denture base systems. J. Prosthodont. 2008, 17, 545–549. [Google Scholar] [CrossRef] [PubMed]
- Vojdani, M.; Bagheri, R.; Khaledi, A.A.R. Effects of aluminum oxide addition on the flexural strength, surface hardness, and roughness of heat-polymerized acrylic resin. J. Dent. Sci. 2012, 7, 238–244. [Google Scholar] [CrossRef] [Green Version]
- Barbosa, D.B.; Souza, R.F. d.; Pero, A.C.; Marra, J.; Compagnoni, M.A. Flexural strength of acrylic resins polymerized by different cycles. J. Appl. Oral Sci. 2007, 15, 424–428. [Google Scholar] [CrossRef]
- Zappini, G.; Kammann, A.; Wachter, W. Comparison of fracture tests of denture base materials. J. Prosthet. Dent. 2003, 90, 578–585. [Google Scholar] [CrossRef]
- Stafford, G.; Huggett, R.; Causton, B. Fracture toughness of denture base acrylics. J. Biomed. Mater. Res. 1980, 14, 359–371. [Google Scholar] [CrossRef]
- Robinson, J.; McCabe, J. Impact strength of acrylic resin denture base materials with surface defects. Dent. Mater. 1993, 9, 355–360. [Google Scholar] [CrossRef]
- Zafar, M.S. Wear behavior of various dental restorative materials. Mater. Technol. 2018, 33, 25–31. [Google Scholar] [CrossRef]
- Zafar, M.S.; Ahmed, N. Effects of wear on hardness and stiffness of restorative dental materials. Life Sci. J. 2014, 11, 11–18. [Google Scholar]
- Zafar, M.S.; Amin, F.; Fareed, M.A.; Ghabbani, H.; Riaz, S.; Khurshid, Z.; Kumar, N. Biomimetic aspects of restorative dentistry biomaterials. Biomimetics 2020, 5, 34. [Google Scholar] [CrossRef]
- Gupta, A.; Kamra, M. An evaluation of the effect of water sorption on dimensional stability of the acrylic resin denture bases. Int. J. Contemp. Dent. 2011, 2. [Google Scholar]
- Arima, T.; Murata, H.; Hamad, T. The effects of cross-linking agents on the water sorption and solubility characteristics of denture base resin. J. Oral Rehabil. 1996, 23, 476–480. [Google Scholar] [CrossRef] [PubMed]
- Anonymous. Dental Materials and their Selection; Quintessence: Chicago, IL, USA; London, UK, 2002; p. 418. [Google Scholar]
- Atwood, D.A. Bone loss of edentulous alveolar ridges. J. Periodontol. 1979, 50, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Alsaggaf, A.; Fenlon, M.R. A case control study to investigate the effects of denture wear on residual alveolar ridge resorption in edentulous patients. J. Dent. 2020, 103373. [Google Scholar] [CrossRef] [PubMed]
- Atsu, S.; KeskIn, Y. Effect of silica coating and silane surface treatment on the bond strength of soft denture liner to denture base material. J. Appl. Oral Sci. 2013, 21, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Nowakowska-Toporowska, A.; Raszewski, Z.; Wieckiewicz, W. Color change of soft silicone relining materials after storage in artificial saliva. J. Prosthet. Dent. 2016, 115, 377–380. [Google Scholar] [CrossRef] [PubMed]
- Cavalcanti, Y.W.; Bertolini, M.M.; Cury, A.A.D.B.; da Silva, W.J. The effect of poly (methyl methacrylate) surface treatments on the adhesion of silicone-based resilient denture liners. J. Prosthet. Dent. 2014, 112, 1539–1544. [Google Scholar] [CrossRef]
- Bail, M.; Jorge, J.H.; Urban, V.M.; Campanha, N.H. Surface roughness of acrylic and silicone-based soft liners: In vivo study in a rat model. J. Prosthodont. 2014, 23, 146–151. [Google Scholar] [CrossRef]
- Habib, S.R.; Vohra, F.A. Replacing existing dentures by copy-denture technique for geriatric patients: A case report. J. Pak. Dent. Assoc. 2013, 22, 265–270. [Google Scholar]
- Patil, S.; Naveen, B.; Patil, N. Bonding acrylic teeth to acrylic resin denture bases: A review. Gerodontology 2006, 23, 131–139. [Google Scholar] [CrossRef]
- Huggett, R.; John, G.; Jagger, R.G.; Bates, J.F. Strength of the acrylic denture base tooth bond. Br. Dent. J. 1982, 153, 187–190. [Google Scholar] [CrossRef] [PubMed]
- Darbar, U.; Huggett, R.; Harrison, A. Denture fracture—A survey. Br. Dent. J. 1994, 176, 342–345. [Google Scholar] [CrossRef] [PubMed]
- Chung, K.; Chung, C.; Chung, C.; Chan, D. Effect of pre-processing surface treatments of acrylic teeth on bonding to the denture base. J. Oral Rehabil. 2008, 35, 268–275. [Google Scholar] [CrossRef] [PubMed]
- Saavedra, G.; Valandro, L.F.; Leite, F.P.P.; Amaral, R.; Özcan, M.; Bottino, M.A.; Kimpara, E.T. Bond strength of acrylic teeth to denture base resin after various surface conditioning methods before and after thermocycling. Int. J. Prosthodont. 2007, 20, 199–201. [Google Scholar]
- Goldin, E.B.; Boyd III, N.W.; Goldstein, G.R.; Hittelman, E.L.; Thompson, V.P. Marginal fit of leucite-glass pressable ceramic restorations and ceramic-pressed-to-metal restorations. J. Prosthet. Dent. 2005, 93, 143–147. [Google Scholar] [CrossRef]
- Alabdulkader, M.A.; Habib, S.R. Effect of cement application techniques on the adaptation and retention of provisional crowns. Technol. Health Care 2018, 26, 945–955. [Google Scholar] [CrossRef]
- Alt, V.; Hannig, M.; Wöstmann, B.; Balkenhol, M. Fracture strength of temporary fixed partial dentures: CAD/CAM versus directly fabricated restorations. Dent. Mater. 2011, 27, 339–347. [Google Scholar] [CrossRef]
- Yilmaz, A.; Baydas, S. Fracture resistance of various temporary crown materials. J. Contemp. Dent. Pract. 2007, 8, 44–51. [Google Scholar] [CrossRef] [Green Version]
- Kwon, S.; Park, Y.; Jun, S.; Ahn, J.; Lee, I.; Cho, B.; Son, H.; Seo, D. Thermal irritation of teeth during dental treatment procedures. Restor. Dent. Endod. 2013, 38, 105–112. [Google Scholar] [CrossRef] [Green Version]
- Bahrani, F.; Safari, A.; Vojdani, M.; Karampoor, G.; Patil, S. Comparison of hardness and surface roughness of two denture bases polymerized by different methods. World J. Dent. 2012, 3, 171–175. [Google Scholar] [CrossRef] [Green Version]
- Haas, S.; Brauer, G.; Dickson, G. A characterization of polymethylmethacrylate bone cement. J. Bone Jt. Surg. 1975, 57, 380–391. [Google Scholar] [CrossRef]
- Alkurt, M.; Duymuş, Z.Y.; Gundogdu, M. Effect of repair resin type and surface treatment on the repair strength of heat-polymerized denture base resin. J. Prosthet. Dent. 2014, 111, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Raszewski, Z.; Nowakowska, D. Mechanical properties of hot curing acrylic resin after reinforced with different kinds of fibers. Int. J. Biomed. Mat. Res. 2013, 1, 9–13. [Google Scholar] [CrossRef]
- Polyzois, G.L.; Andreopoulos, A.G.; Lagouvardos, P.E. Acrylic resin denture repair with adhesive resin and metal wires: Effects on strength parameters. J. Prosthet. Dent. 1996, 75, 381–387. [Google Scholar] [CrossRef]
- Polyzois, G.L.; Tarantili, P.A.; Frangou, M.J.; Andreopoulos, A.G. Fracture force, deflection at fracture, and toughness of repaired denture resin subjected to microwave polymerization or reinforced with wire or glass fiber. J. Prosthet. Dent. 2001, 86, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Al Baker, A.; Habib, S.R.; Al Amri, M.D. Preserving esthetics, occlusion and occlusal vertical dimension in a patient with fixed prostheses seeking dental implant treatment. Saudi Dent. J. 2016, 28, 203–208. [Google Scholar] [CrossRef] [Green Version]
- Agarwal, M.; Nayak, A.; Hallikerimath, R. A study to evaluate the transverse strength of repaired acrylic denture resins with conventional heat-cured, autopolymerizing and microwave-cured resins: An in vitro study. J. Indian Prosthodont. Soc. 2008, 8, 36–41. [Google Scholar] [CrossRef]
- Faot, F.; Da Silva, W.J.; Da Rosa, R.S.; Del Bel Cury, A.A.; Garcia, R.C.M.R. Strength of denture base resins repaired with auto-and visible light-polymerized materials. J. Prosthodont. Dent. 2009, 18, 496–502. [Google Scholar] [CrossRef]
- Murphy, W.; Huggett, R.; Handley, R.; Brooks, S. Rigid cold curing resins for direct use in the oral cavity. Br. Dent. J. 1986, 160, 391–394. [Google Scholar] [CrossRef]
- Shifman, A. Clinical applications of visible light-cured resin in maxillofacial prosthetics. part I: Denture base and reline material. J. Prosthet. Dent. 1990, 64, 578–582. [Google Scholar] [CrossRef]
- Fellman, S. Visible light-cured denture resin used in making dentures with conventional teeth. J. Prosthet. Dent. 1989, 62, 356–359. [Google Scholar] [CrossRef]
- Polyzois, G.L.; Handley, R.W.; Stafford, G.D. Repair strength of denture base resins using various methods. Eur. J. Prosthodont. Restor. Dent. 1995, 3, 183–186. [Google Scholar] [PubMed]
- Jacobsen, N.L.; Mitchell, D.L.; Johnson, D.L.; Holt, R.A. Lased and sandblasted denture base surface preparations affecting resilient liner bonding. J. Prosthet. Dent. 1997, 78, 153–158. [Google Scholar] [CrossRef]
- Jagger, R.G.; al-Athel, M.S.; Jagger, D.C.; Vowles, R.W. Some variables influencing the bond strength between PMMA and a silicone denture lining material. Int. J. Prosthodont. 2002, 15, 55–58. [Google Scholar]
- Vojdani, M.; Rezaei, S.; Zareeian, L. Effect of chemical surface treatments and repair material on transverse strength of repaired acrylic denture resin. Indian J. Dent. Res. 2008, 19, 2–5. [Google Scholar] [CrossRef]
- Vallittu, P.K.; Lassila, V.P.; Lappalainen, R. Wetting the repair surface with methyl methacrylate affects the transverse strength of repaired heat-polymerized resin. J. Prosthet. Dent. 1994, 72, 639–643. [Google Scholar] [CrossRef]
- Minami, H.; Suzuki, S.; Minesaki, Y.; Kurashige, H.; Tanaka, T. In vitro evaluation of the influence of repairing condition of denture base resin on the bonding of autopolymerizing resins. J. Prosthet. Dent. 2004, 91, 164–170. [Google Scholar] [CrossRef]
- Seó, R.S.; Neppelenbroek, K.H.; Filho, J.N.A. Factors affecting the strength of denture repairs. J. Prosthodont. 2007, 16, 302–310. [Google Scholar] [CrossRef]
- Ahmed, Z.U.; Flynn, J.; Riedel, E.R.; Huryn, J.M.; Rosen, E.B. Definitive maxillary obturator prosthesis: Timelines for fabrication and follow-up. Spec. Care Dent. 2020, 40, 315–319. [Google Scholar] [CrossRef]
- Molinero-Mourelle, P.; Helm, A.; Cobo-Vázquez, C.; Lam, W.Y.; Azevedo, L.; Pow, E.H.; Gómez-Polo, M. Treatment outcomes of implant-supported maxillary obturator prostheses in patients with maxillary defects: A systematic review. Int. J. Prosthodont. 2020, 33, 429–440. [Google Scholar] [CrossRef]
- Urechescu, H.; Pricop, M.; Bogdan, L.; Nes, C.S.; Pricop, C.; Rusu, L.C.; Rivis, M. Experimental compression and traction tests on heat-cured pmma used in maxillary obturator prostheses. Mat. Plast 2016, 53, 76. [Google Scholar]
- Urechescu, H.; Pricop, M.; Pricop, C.; Mateas, M.; Natanael, S.; Galatanu, S.V. Thermoplastic materials used for fabrication of maxillary obturator prostheses. Mat. Plast 2017, 54, 477. [Google Scholar] [CrossRef]
- Metwaly, A.F.; Taha, E.R. Evaluation of microbial adhesions and quality of life in maxillectomy patients rehabilitated with cobalt-chromium and thermoplastic obturators. Egypt. Dent. J. 2017, 63, 3639–3650. [Google Scholar] [CrossRef]
- Koyama, S.; Kato, H.; Harata, T.; Sasaki, K. A workflow for fabricating a hollow obturator by using 3D digital technologies. J. Prosthet. Dent. 2020, 123, 648–652. [Google Scholar] [CrossRef] [PubMed]
- Jang, W.; Lim, H.; Yun, K.; Park, C.; Yang, H. Fabrication of closed hollow obturator for hard palate defect patient undergone maxillectomy. J. Korean Acad. Prosthodont. 2020, 58, 30–34. [Google Scholar] [CrossRef]
- Sharma, P.; Mago, G. Rehabilitation of patient with hemimaxillectomy defect using a closed hollow bulb obturator: A case report. J. Adv. Med. Dent. Sci. Res. 2020, 8, 107–110. [Google Scholar]
- Ramasamy, T.V.; Chandra, J. An innovative sectional silicone obturator in a patient with partial maxillectomy: A Case report. J. Indian. Prosthodont. Soc. 2020, 20, 115–119. [Google Scholar] [CrossRef]
- Qoran, A.H.; Aminifar, S.; Adli, A.R.; Abachizadeh, H. Using a silicone core to reduce the weight of maxillary obturator prosthesis. J. Dent. Sch. 2012, 30, 136–142. [Google Scholar]
- Bidra, A.S.; Taylor, T.D.; Agar, J.R. Computer-aided technology for fabricating complete dentures: Systematic review of historical background, current status, and future perspectives. J. Prosthet. Dent. 2013, 109, 361–366. [Google Scholar] [CrossRef]
- Alp, G.; Murat, S.; Yilmaz, B. Comparison of Flexural Strength of Different CAD/CAM PMMA-Based Polymers. J. Prosthodont. 2019, 28, 491–495. [Google Scholar] [CrossRef]
- Al-Dwairi, Z.N.; Tahboub, K.Y.; Baba, N.Z.; Goodacre, C.J. A comparison of the flexural and impact strengths and flexural modulus of CAD/CAM and conventional heat-cured polymethyl methacrylate (PMMA). J. Prosthodont. 2020, 29, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Arslan, M.; Murat, S.; Alp, G.; Zaimoglu, A. Evaluation of flexural strength and surface properties of prepolymerized CAD/CAM PMMA-based polymers used for digital 3D complete dentures. Int. J. Comput. Dent. 2018, 21, 31–40. [Google Scholar] [PubMed]
- Al-Dwairi, Z.N.; Tahboub, K.Y.; Baba, N.Z.; Goodacre, C.J.; Özcan, M. A comparison of the surface properties of CAD/CAM and conventional polymethylmethacrylate (PMMA). J. Prosthodont. 2019, 28, 452–457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murat, S.; Alp, G.; Alatalı, C.; Uzun, M. In vitro evaluation of adhesion of candida albicans on CAD/CAM PMMA-based polymers. J. Prosthodont. 2019, 28, 873–879. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, M.; Gjengedal, H.; Cattani-Lorente, M.; Moussa, M.; Durual, S.; Schimmel, M.; Müller, F. CAD/CAM milled complete removable dental prostheses: An in vitro evaluation of biocompatibility, mechanical properties, and surface roughness. Dent. Mater. J. 2018, 2017–2207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, J.J.E.; Uy, C.E.; Plaksina, P.; Ramani, R.S.; Ganjigatti, R.; Waddell, J.N. Bond Strength of denture teeth to heat-cured, CAD/CAM and 3D printed denture acrylics. J. Prosthodont. 2020, 29, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Kalberer, N.; Mehl, A.; Schimmel, M.; Müller, F.; Srinivasan, M. CAD-CAM milled versus rapidly prototyped (3D-printed) complete dentures: An in vitro evaluation of trueness. J. Prosthet. Dent. 2019, 121, 637–643. [Google Scholar] [CrossRef]
- Davda, K.; Osnes, C.; Dillon, S.; Wu, J.; Hyde, T.; Keeling, A. An investigation into the trueness and precision of copy denture templates produced by rapid prototyping and conventional means. Eur. J. Prosthodont. Restor. Dent. 2017, 25, 186–192. [Google Scholar]
- Steinmassl, P.; Wiedemair, V.; Huck, C.; Klaunzer, F.; Steinmassl, O.; Grunert, I.; Dumfahrt, H. Do CAD/CAM dentures really release less monomer than conventional dentures? Clin. Oral Investig. 2017, 21, 1697–1705. [Google Scholar] [CrossRef] [Green Version]
- Quirynen, M.; Marechal, M.; Busscher, H.; Weerkamp, A.; Darius, P.; van Steenberghe, D. The influence of surface free energy and surface roughness on early plaque formation: An in vivo study in man. J. Clin. Periodontol. 1990, 17, 138–144. [Google Scholar] [CrossRef]
- Quirynen, M.v.; Van Der Mei, H.; Bollen, C.; Schotte, A.; Marechal, M.; Doornbusch, G.; Naert, I.; Busscher, H. v.; Van Steenberghe, D. An in vivo study of the influence of the surface roughness of implants on the microbiology of supra-and subgingival plaque. J. Dent. Res. 1993, 72, 1304–1309. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, Z.; Zafar, M.S. Role of antifungal medicaments added to tissue conditioners: A systematic review. J. Prosthodont. Res. 2016, 60, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Gendreau, L.; Loewy, Z.G. Epidemiology and etiology of denture stomatitis. J. Prosthodont. 2011, 20, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Hoshi, N.; Mori, H.; Taguchi, H.; Taniguchi, M.; Aoki, H.; Sawada, T.; Kawabata, M.; Kuwabara, A.; Oono, A.; Tanaka, K.; et al. Management of oral candidiasis in denture wearers. J. Prosthodont. Res. 2011, 55, 48–52. [Google Scholar] [CrossRef]
- de Oliveira, C.E.; Gasparoto, T.H.; Dionisio, T.J.; Porto, V.C.; Vieira, N.A.; Santos, C.F.; Lara, V.S. Candida albicans and denture stomatitis: Evaluation of its presence in the lesion, prosthesis, and blood. Int. J. Prosthodont. 2010, 23, 158–159. [Google Scholar]
- Amin, W.M.; Al-Ali, M.H.; Salim, N.A.; Al-Tarawneh, S.K. A new form of intraoral delivery of antifungal drugs for the treatment of denture-induced oral candidosis. Eur. J. Dent. 2009, 3, 257–266. [Google Scholar] [CrossRef] [Green Version]
- Huettig, F.; Prutscher, A.; Goldammer, C.; Kreutzer, C.A.; Weber, H. First clinical experiences with CAD/CAM-fabricated PMMA-based fixed dental prostheses as long-term temporaries. Clin. Oral Investig. 2016, 20, 161–168. [Google Scholar] [CrossRef]
- Moshkelgosha, V.; Shomali, M.; Momeni, M.A.S.O.O.M.E.H. Comparison of wear resistance of hawley and vacuum formed retainers: An in-vitro study. J. Dent. Biomater. 2016, 3, 248–253. [Google Scholar]
- Casey, J.; Dunn, W.J.; Wright, E. In vitro wear of various orthotic device materials. J. Prosthet. Dent. 2003, 90, 498–502. [Google Scholar] [CrossRef]
- Rantala, L.; Lastumäki, T.; Peltomäki, T.; Vallittu, P. Fatigue resistance of removable orthodontic appliance reinforced with glass fibre weave. J. Oral Rehabil. 2003, 30, 501–506. [Google Scholar] [CrossRef]
- Faltermeier, A.; Rosentritt, M.; Müssig, D. Acrylic removable appliances: Comparative evaluation of different postpolymerization methods. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 301.e16–301.e22. [Google Scholar] [CrossRef] [PubMed]
- Namura, Y.; Takamizawa, T.; Uchida, Y.; Inaba, M.; Noma, D.; Takemoto, T.; Miyazaki, M.; Motoyoshi, M. Effects of composition on the hardness of orthodontic adhesives. J. Oral Sci. 2020, 62, 48–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Habib, S.R.; Azad, A.A. Comparison of patient’s satisfaction with replacement complete dentures fabricated by copy denture technique versus conventional technique. J. Pak. Dent. Assoc. 2009, 18, 9–13. [Google Scholar]
- Habib, S.R.; Al Ajmi, M.G.; Al Dhafyan, M.; Jomah, A.; Abualsaud, H.; Almashali, M. Effect of margin designs on the marginal adaptation of zirconia copings. Acta Stomatol. Croat. 2017, 51, 179–187. [Google Scholar] [CrossRef]
- Habib, S.R.; Ali, M.; Al Hossan, A.; Majeed-Saidan, A.; Al Qahtani, M. Effect of cementation, cement type and vent holes on fit of zirconia copings. Saudi Dent. J. 2019, 31, 45–51. [Google Scholar] [CrossRef]
- Zafar, M.S.; Al-Samadani, K.H. Potential use of natural silk for bio-dental applications. J. Taibah Univ. Med. Sci. 2014, 9, 171–177. [Google Scholar] [CrossRef] [Green Version]
- Tsuchiya, H.; Hoshino, Y.; Tajima, K.; Takagi, N. Leaching and cytotoxicity of formaldehyde and methyl methacrylate from acrylic resin denture base materials. J. Prosthet. Dent. 1994, 71, 618–624. [Google Scholar] [CrossRef]
- Nandal, S.; Ghalaut, P.; Shekhawat, H.; Gulati, M.S. New era in denture base resins: A review. Dent. J. Adv. Stud. 2013, 1, 136–143. [Google Scholar] [CrossRef] [Green Version]
- Cierech, M.; Osica, I.; Kolenda, A.; Wojnarowicz, J.; Szmigiel, D.; Łojkowski, W.; Kurzydłowski, K.; Ariga, K.; Mierzwińska-Nastalska, E. Mechanical and physicochemical properties of newly formed ZnO-PMMA nanocomposites for denture bases. Nanomaterials 2018, 8, 305. [Google Scholar] [CrossRef] [Green Version]
- Khan, A.S.; Azam, M.T.; Khan, M.; Mian, S.A.; Rehman, I.U. An update on glass fiber dental restorative composites: A systematic review. Mater. Sci. Eng. C 2015, 47, 26–39. [Google Scholar] [CrossRef]
- Xu, H.; Schumacher, G.E.; Eichmiller, F.; Peterson, R.; Antonucci, J.M.; Mueller, H. Continuous-fiber preform reinforcement of dental resin composite restorations. Dent. Mater. 2003, 19, 523–530. [Google Scholar] [CrossRef]
- Petersen, R.C. Discontinuous fiber-reinforced composites above critical length. J. Dent. Res. 2005, 84, 365–370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hyer, M.W.; White, S.R. Stress Analysis of Fiber-Reinforced Composite Materials; DEStech Publications, Inc.: Lancaster, PA, USA, 2009. [Google Scholar]
- van Heumen, C.C.; Kreulen, C.M.; Bronkhorst, E.M.; Lesaffre, E.; Creugers, N.H. Fiber-reinforced dental composites in beam testing. Dent. Mater. 2008, 24, 1435–1443. [Google Scholar] [CrossRef]
- Butterworth, C.; Ellakwa, A.E.; Shortall, A. Fibre-reinforced composites in restorative dentistry. Dent. Update 2003, 30, 300–306. [Google Scholar] [CrossRef]
- Garoushi, S.; Vallittu, P.K.; Lassila, L.V. Depth of cure and surface microhardness of experimental short fiber-reinforced composite. Acta Odontol. Scand. 2008, 66, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Topouzi, M.; Kontonasaki, E.; Bikiaris, D.; Papadopoulou, L.; Paraskevopoulos, K.M.; Koidis, P. Reinforcement of a PMMA resin for interim fixed prostheses with silica nanoparticles. J. Mech. Behav. Biomed. Mater. 2017, 69, 213–222. [Google Scholar] [CrossRef]
- Ratanajanchai, M.; Kanchanavasita, W.; Suputtamongkol, K.; Wonglamsam, A.; Thamapipol, S.; Sae-Khow, O. Heat-cured poly(methyl methacrylate) resin incorporated with different food preservatives as an anti-microbial denture base material. J. Dent. Sci. 2020. [Google Scholar] [CrossRef]
- DeBoer, J.; Vermilyea, S.; Brady, R. The effect of carbon fiber orientation on the fatigue resistance and bending properties of two denture resins. J. Prosthet. Dent. 1984, 51, 119–121. [Google Scholar] [CrossRef]
- Alla, R.K.; Sajjan, S.; Alluri, V.R.; Ginjupalli, K.; Upadhya, N. Influence of fiber reinforcement on the properties of denture base resins. J. Biomater. Nanobiotechnol. 2013, 4, 91. [Google Scholar] [CrossRef] [Green Version]
- Kanie, T.; Fujii, K.; Arikawa, H.; Inoue, K. Flexural properties and impact strength of denture base polymer reinforced with woven glass fibers. Dent. Mater. 2000, 16, 150–158. [Google Scholar] [CrossRef]
- John, J.; Gangadhar, S.A.; Shah, I. Flexural strength of heat-polymerized polymethyl methacrylate denture resin reinforced with glass, aramid, or nylon fibers. J. Prosthet. Dent. 2001, 86, 424–427. [Google Scholar] [CrossRef] [PubMed]
- Ladizesky, N.H.; Chow, T.W.; Cheng, Y.Y. Denture base reinforcement using woven polyethylene fiber. Int. J. Prosthodont. 1994, 7, 307–314. [Google Scholar] [PubMed]
- Ladizesky, N.H.; Ho, C.F.; Chow, T.W. Reinforcement of complete denture bases with continuous high performance polyethylene fibers. J. Prosthet. Dent. 1992, 68, 934–939. [Google Scholar] [CrossRef]
- Singh, K.; Sharma, S.K.; Negi, P.; Kumar, M.; Rajpurohit, D.; Khobre, P. Comparative evaluation of flexural strength of heat polymerised denture base resins after reinforcement with glass fibres and nylon fibres: An in vitro study. Adv. Hum. Biol. 2016, 6, 91. [Google Scholar] [CrossRef]
- Farina, A.P.; Cecchin, D.; Soares, R.G.; Botelho, A.L.; Takahashi, J.M.F.K.; Mazzetto, M.O.; Mesquita, M.F. Evaluation of vickers hardness of different types of acrylic denture base resins with and without glass fibre reinforcement. Gerodontology 2012, 29, 155–160. [Google Scholar] [CrossRef]
- Vallittu, P.K. A review of fiber-reinforced denture base resins. J. Prosthodont. 1996, 5, 270–276. [Google Scholar] [CrossRef]
- Chong, K.; Chai, J. Strength and mode of failure of unidirectional and bidirectional glass fiber-reinforced composite materials. Int. J. Prosthodont. 2003, 16, 161–166. [Google Scholar]
- McDonough, W.G.; Antonucci, J.M.; Dunkers, J.P. Interfacial shear strengths of dental resin-glass fibers by the microbond test. Dent. Mater. 2001, 17, 492–498. [Google Scholar] [CrossRef]
- Matinlinna, J.P.; Lassila, L.V.; Özcan, M.; Yli-Urpo, A.; Vallittu, P.K. An introduction to silanes and their clinical applications in dentistry. Int. J. Prosthodont. 2004, 17, 155–164. [Google Scholar]
- Nejatian, T.; Johnson, A.; Van Noort, R. Reinforcement of denture base resin. In Advances in Science and Technology; Trans Tech Publ: Zurich, Switzerland, 2006; Volume 49, pp. 124–129. [Google Scholar]
- Kul, E.; Aladağ, L.İ.; Yesildal, R. Evaluation of thermal conductivity and flexural strength properties of poly (methyl methacrylate) denture base material reinforced with different fillers. J. Prosthet. Dent. 2016, 116, 803–810. [Google Scholar] [CrossRef]
- Mansour, M.M.; Wagner, W.C.; Chu, T.G. Effect of mica reinforcement on the flexural strength and microhardness of polymethyl methacrylate denture resin. J. Prosthodont. 2013, 22, 179–183. [Google Scholar] [CrossRef]
- Casemiro, L.A.; Martins, C.H.G.; Pires-de-Souza, F.d.C.; Panzeri, H. Antimicrobial and mechanical properties of acrylic resins with incorporated silver–zinc zeolite—Part I. Gerodontology 2008, 25, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Flores, J.C.; Garcia, R.; Villanueva, G.; Acosta-Torres, L. Antimicrobial poly (methyl methacrylate) with silver nanoparticles for dentistry: A systematic review. Appl. Sci. 2020, 10, 4007. [Google Scholar]
- Kurt, A.; Erkose-Genc, G.; Uzun, M.; Emrence, Z.; Ustek, D.; Isik-Ozkol, G. The antifungal activity and cytotoxicity of silver containing denture base material. Niger. J. Clin. Pract. 2017, 20, 290–295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Acosta-Torres, L.S.; Mendieta, I.; Nunez-Anita, R.E.; Cajero-Juarez, M.; Castano, V.M. Cytocompatible antifungal acrylic resin containing silver nanoparticles for dentures. Int. J. Nanomed. 2012, 7, 4777–4786. [Google Scholar]
- Monteiro, D.R.; Gorup, L.F.; Takamiya, A.S.; de Camargo, E.R.; Filho, A.C.R.; Barbosa, D.B. Silver distribution and release from an antimicrobial denture base resin containing silver colloidal nanoparticles. J. Prosthodont. 2012, 21, 7–15. [Google Scholar] [CrossRef]
- Sawada, T.; Sawada, T.; Kumasaka, T.; Hamada, N.; Shibata, T.; Nonami, T.; Kimoto, K. Self-cleaning effects of acrylic resin containing fluoridated apatite-coated titanium dioxide. Gerodontology 2014, 31, 68–75. [Google Scholar] [CrossRef]
- Shibata, T.; Hamada, N.; Kimoto, K.; Sawada, T.; Sawada, T.; Kumada, H.; Umemoto, T.; Toyoda, M. Antifungal effect of acrylic resin containing apatite-coated TiO2 photocatalyst. Dent. Mater. J. 2007, 26, 437–444. [Google Scholar] [CrossRef] [Green Version]
- Al-Bakri, I.; Harty, D.; Al-Omari, W.; Swain, M.; Chrzanowski, W.; Ellakwa, A. Surface characteristics and microbial adherence ability of modified polymethylmethacrylate by fluoridated glass fillers. Aust. Dent. J. 2014, 59, 482–489. [Google Scholar] [CrossRef]
- Tsutsumi, C.; Takakuda, K.; Wakabayashi, N. Reduction of Candida biofilm adhesion by incorporation of prereacted glass ionomer filler in denture base resin. J. Dent. 2016, 44, 37–43. [Google Scholar] [CrossRef]
- Lee, J.; El-Fiqi, A.; Jo, J.; Kim, D.; Kim, S.; Jun, S.; Kim, H.; Lee, H. Development of long-term antimicrobial poly (methyl methacrylate) by incorporating mesoporous silica nanocarriers. Dent. Mater. 2016, 32, 1564–1574. [Google Scholar] [CrossRef]
- Alwan, S.A.; Alameer, S.S. The effect of the addition of silanized nano titania fillers on some physical and mechanical properties of heat cured acrylic denture base materials. J. Baghdad Coll. Dent. 2015, 325, 1–12. [Google Scholar] [CrossRef]
- Bacali, C.; Badea, M.; Moldovan, M.; Sarosi, C.; Nastase, V.; Baldea, I.; Chiorean, R.S.; Constantiniuc, M. The influence of graphene in improvement of physico-mechanical properties in PMMA denture base resins. Materials 2019, 12, 2335. [Google Scholar] [CrossRef] [Green Version]
- Zafar, M.S.; Alnazzawi, A.A.; Alrahabi, M.; Fareed, M.A.; Najeeb, S.; Khurshid, Z. Nanotechnology and nanomaterials in dentistry. In Advanced Dental Biomaterials; Khurshid, Z., Najeeb, S., Zafar, M.S., Sefat, F., Eds.; Woodhead Publishing: Cambridge, UK, 2019; pp. 477–505. [Google Scholar]
- Yu, W.; Wang, X.; Tang, Q.; Guo, M.; Zhao, J. Reinforcement of denture base PMMA with ZrO2 nanotubes. J. Mech. Behav. Biomed. Mater. 2014, 32, 192–197. [Google Scholar] [CrossRef]
- Yadav, P.; Mittal, R.; Sood, V.K.; Garg, R. Effect of incorporation of silane-treated silver and aluminum microparticles on strength and thermal conductivity of PMMA. J. Prosthodont. 2012, 21, 546–551. [Google Scholar] [CrossRef]
- Aljafery, A.; MAH, B. Effect of addition ZrO2-Al2O3 nanoparticles mixture on some properties and denture base adaptation of heat cured acrylic resin denture base material. J. Baghdad Coll. Dent. 2015, 325, 1–15. [Google Scholar]
- Muklif, O.R.; Ismail, I.J. Studying the effect of addition a composite of silanized Nano-Al2O3 and plasma treated polypropylene fibers on some physical and mechanical properties of heat cured PMMA denture base material. J. Baghdad Coll. Dent. 2015, 325, 1–13. [Google Scholar] [CrossRef]
- Khurshid, Z.; Zafar, M.; Qasim, S.; Shahab, S.; Naseem, M.; AbuReqaiba, A. Advances in nanotechnology for restorative dentistry. Materials 2015, 8, 717–731. [Google Scholar] [CrossRef] [Green Version]
- Hari Prasad, A.; Kalavathy, M.; Mohammed, H. Effect of glass fiber and silane treated glass fiber reinforcement on impact strength of maxillary complete denture. Ann. Essen. Dent. 2011, 4, 7–12. [Google Scholar] [CrossRef] [Green Version]
- Salman, T.A.; Khalaf, H.A. The influence of adding of modified ZrO2-TiO2 nanoparticles on certain physical and mechanical properties of heat polymerized acrylic resin. J. Baghdad Coll. Dent. 2015, 325, 1–15. [Google Scholar]
- Abdulkareem, M.M.; Hatim, N.A. Evaluation the biological effect of adding aluminum oxide, silver nanoparticles into microwave treated PMMA powder. Int. J. Enhanc. Res. Sci. Technol. Eng. 2015, 4, 172–178. [Google Scholar]
- Bian, Y.M.; Zhang, X.Y.; Zhu, B.S.; Yu, W.Q.; Ruan, D.P.; Min, M. Influence of different amount of silane coupling agent on the flexural strength of PMMA/nanometer ZrO2 composites. Shanghai J. Stomatol. 2007, 16, 319–323. [Google Scholar]
- Asopa, V.; Suresh, S.; Khandelwal, M.; Sharma, V.; Asopa, S.S.; Kaira, L.S. A comparative evaluation of properties of zirconia reinforced high impact acrylic resin with that of high impact acrylic resin. Saudi J. Dent. Res. 2015, 6, 146–151. [Google Scholar] [CrossRef] [Green Version]
- Ahmed, M.A.; El-Shennawy, M.; Althomali, Y.M.; Omar, A.A. Effect of titanium dioxide nano particles incorporation on mechanical and physical properties on two different types of acrylic resin denture base. World J. Nano. Sci. Eng. 2016, 6, 111–119. [Google Scholar] [CrossRef] [Green Version]
- Elshereksi, N.; Mohamed, S.; Arifin, A.; Mohd Ishak, Z. Effect of filler incorporation on the fracture toughness properties of denture base poly (methyl methacrylate). J. Phys. Sci. 2009, 20, 1–12. [Google Scholar]
- Protopapa, P.; Kontonasaki, E.; Bikiaris, D.; Paraskevopoulos, K.M.; Koidis, P. Reinforcement of a PMMA resin for fixed interim prostheses with nanodiamonds. Dent. Mater. J. 2011, 30, 222–231. [Google Scholar] [CrossRef] [Green Version]
- Mangal, U.; Kim, J.; Seo, J.; Kwon, J.; Choi, S. Novel poly (methyl methacrylate) containing nanodiamond to improve the mechanical properties and fungal resistance. Materials 2019, 12, 3438. [Google Scholar] [CrossRef] [Green Version]
- Fouda, S.M.; Gad, M.M.; Ellakany, P.; Al-Thobity, A.M.; Al-Harbi, F.A.; Virtanen, J.I.; Raustia, A. The effect of nanodiamonds on candida albicans adhesion and surface characteristics of PMMA denture base material-an in vitro study. J. Appl. Oral Sci. 2019, 27, 20180779. [Google Scholar] [CrossRef] [Green Version]
- McNally, T.; Pötschke, P.; Halley, P.; Murphy, M.; Martin, D.; Bell, S.E.J.; Brennan, G.P.; Bein, D.; Lemoine, P.; Quinn, J.P. Polyethylene multiwalled carbon nanotube composites. Polymer 2005, 46, 8222–8232. [Google Scholar] [CrossRef]
- Collins, P.G.; Avouris, P. Nanotubes for electronics. Sci. Am. 2000, 283, 62–69. [Google Scholar] [CrossRef]
- Rodford, R. Further development and evaluation of high impact strength denture base materials. J. Dent. 1990, 18, 151–157. [Google Scholar] [CrossRef]
- Delfi, M.; Ghomi, M.; Zarrabi, A.; Mohammadinejad, R.; Taraghdari, Z.B.; Ashrafizadeh, M.; Zare, E.N.; Agarwal, T.; Padil, V.V.; Mokhtari, B. Functionalization of polymers and nanomaterials for biomedical applications: Antimicrobial platforms and drug carriers. Prosthesis 2020, 2, 117–139. [Google Scholar] [CrossRef]
- Rouabhia, M.; Chmielewski, W. Diseases associated with oral polymicrobial biofilms. Open Mycol. J. 2012, 6, 27–32. [Google Scholar] [CrossRef]
- Makvandi, P.; Gu, J.T.; Zare, E.N.; Ashtari, B.; Moeini, A.; Tay, F.R.; Niu, L. Polymeric and inorganic nanoscopical antimicrobial fillers in dentistry. Acta Biomater. 2020, 101, 69–101. [Google Scholar] [CrossRef]
- Akihiro Yoshihara, D.; Sakuma, P.S.; Kobayashi, P.S.; Miyazaki, P.H. Antimicrobial effect of fluoride mouthrinse on mutans streptococci and lactobacilli in saliva. Pediatr. Dent. 2001, 23, 113–117. [Google Scholar]
- Gad, M.M.; Al-Thobity, A.M.; Fouda, S.M.; Näpänkangas, R.; Raustia, A. Flexural and surface properties of PMMA denture base material modified with thymoquinone as an antifungal agent. J. Prosthodont. 2020, 29, 243–250. [Google Scholar] [CrossRef]
- Makvandi, P.; Jamaledin, R.; Jabbari, M.; Nikfarjam, N.; Borzacchiello, A. Antibacterial quaternary ammonium compounds in dental materials: A systematic review. Dent. Mater. 2018, 34, 851–867. [Google Scholar] [CrossRef]
- Makvandi, P.; Ghaemy, M.; Mohseni, M. Synthesis and characterization of photo-curable bis-quaternary ammonium dimethacrylate with antimicrobial activity for dental restoration materials. Eur. Polym. J. 2016, 74, 81–90. [Google Scholar] [CrossRef]
- Makvandi, P.; Ghaemy, M.; Ghadiri, A.; Mohseni, M. Photocurable, antimicrobial quaternary ammonium–modified nanosilica. J. Dent. Res. 2015, 94, 1401–1407. [Google Scholar] [CrossRef]
- Pesci-Bardon, C.; Fosse, T.; Serre, D.; Madinier, I. In vitro antiseptic properties of an ammonium compound combined with denture base acrylic resin. Gerodontology 2006, 23, 111–116. [Google Scholar] [CrossRef]
- Pesci-Bardon, C.; Fosse, T.; Madinier, I.; Serre, D. In vitro new dialysis protocol to assay the antiseptic properties of a quaternary ammonium compound polymerized with denture acrylic resin. Lett. Appl. Microbiol. 2004, 39, 226–231. [Google Scholar] [CrossRef] [PubMed]
- Mai, H.; Kim, D.; Hyun, D.C.; Park, J.H.; Lee, S.M.; Lee, D. A new antibacterial agent-releasing polydimethylsiloxane coating for polymethyl methacrylate dental restorations. J. Clin. Med. 2019, 8, 1831. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.; Jo, J.; Kim, D.; Patel, K.D.; Kim, H.; Lee, H. Nano-graphene oxide incorporated into PMMA resin to prevent microbial adhesion. Dent. Mater. 2018, 34, 63–72. [Google Scholar] [CrossRef] [PubMed]





| Year | Development | Reference |
|---|---|---|
| 1843 | Formation of acrylic acid by oxidation of acrolein was reported | [44] |
| 1931 | Harder PMMA became commercially available in sheet forms | [45] |
| 1936 | Otto Rohm developed industrial PMMA as credit of their research in the beginning of 20th century | [46] |
| 1937 | PMMA was firstly introduced in powder form for denture base fabrication | [47] |
| 1945 | PMMA was used extensively by neurosurgeons for cranioplasties | [48] |
| 1945 | Cold-cured (room temperature curing) PMMA became commercially available | [49] |
| 1946 | PMMA became the leading material for making dentures | [47] |
| 1950s | Orthopedic surgeon used PMMA for the cementation of femoral bones prostheses | [48] |
| 1950s to 1960s | PMMA’s use by dental professionals dramatically increased for a variety of applications, including dentures, temporary or provisional crowns, and maxillofacial prostheses | [50] |
| 21st century | Ongoing research and modifications of existing PMMA materials are improving the mechanical and physical properties | [51,52,53,54] |
| Material | Advantages | Disadvantages |
|---|---|---|
| Gold | Gold is known for its excellent biocompatibility and corrosion resistance. Denture base was historically fabricated using gold centuries ago [59,60,61]. | Expensive, poor aesthetics due to its color [60]. |
| Porcelain | Porcelain was introduced in the 18th century for denture fabrication [60]. | Very hard, high-density brittle materials with poor aesthetics [57]. |
| Vulcanite | Vulcanite is a cost-effective material that was introduced in the 19th century and used for several years; vulcanite is dimensionally stable, comfortable, low density, light weight, and is easily fabricated [60]. | Absence of chemical bonding with porcelain teeth and poor aesthetics [55]. |
| Aluminum | Aluminum was used to cast denture bases using a casting process during the 19th century [60], providing accurate fit and light weight [57]. | Casting aluminum was an expensive and sensitive technique [57]. |
| Celluloid | A polymeric material used in the 19th century; can be colored pink to mimic oral tissues [45]. | Color changes by staining from food and altered taste due to the presence of camphor [45]. |
| Bakelite | Used in the 20th century; had excellent aesthetics [57]. | Difficult manipulation, prone to staining, and brittle [57]. |
| Polyvinyl Chloride (PVC) | A co-polymer of acetate and vinyl chloride used for dentures in the 20th century [62]. | Poor mechanical properties and prone to discoloration [62]. |
| Base metal alloys | Nickel and cobalt chromium alloys have been used since early 20th century. Still used due to their excellent mechanical properties, low density, and cost-effectiveness [57]. | Poor aesthetics due to metallic color, very hard materials; difficult to cut, finish, and repair. There are allergy issues mainly due to the presence of nickel [57]. |
| Heat Cycles | Temperature | Time | Terminal Boiling | Reference |
|---|---|---|---|---|
| 1 | 74 °C | 8 h | None | [78] |
| 2 | 74 °C | 8 h | 1 h | [78] |
| 3 | 74°C | 3 h | 1 h | [78] |
| 4 | 73.9 °C | 12 h | None | [50] |
| 5 | 70 °C | 3 h | 1 h | [83] |
| 6 | 100 °C | 20 min | None | [84] |
| Property | Value | Reference |
|---|---|---|
| Elastic modulus (GPa) | 2.6 | [7] |
| 3.89 ± 1.320 | [98] | |
| Flexural strength (MPa) | 90 | [7] |
| Fracture toughness (MN/m3/2) | 2.53 | [7] |
| Fracture toughness (MPa.m1/2) | 1.86 ± 0.25 | [66] |
| Proportional limit (MPa) | 26 | [82] |
| Compressive strength (MPa) | 76 | [82] |
| Tensile strength (MPa) | 48–62 | [82] |
| 55 | [7] | |
| Elongation (%) | 1–2% | [82] |
| Impact strength (J) | 0.98–1.27 J | [66,82] |
| Knoop hardness (KHN) | 18–20 KHN | [82] |
| Rockwell hardness | M90–M100 | [107,108] |
| Vickers hardness (VHN) | 20 | [7] |
| Absolute hardness (MPa) | 297.72 ± 19.04 | [98] |
| Fatigue strength (MPa) | 1.5 × 106 cycles at 17.2 MPa | [82] |
| Biaxial flexural strength | 121 ± 12 | [66] |
| Thermal conductivity | 5.7 × 10−4 °C/cm | [82] |
| Coefficient of thermal expansion | 81 × 10−6 /°C | [82] |
| Linear thermal expansion (mm/mm.k) | 6.3 × 10−5 | [108] |
| Glass transition temperature | 125 °C | [7,82] |
| Curing shrinkage (%) | −0.50 to −0.58 | [95] |
| Density g/cm3 at room temperature | 1.18 | [107,108] |
| Sorption (mg/cm2) | 0.69 | [82] |
| Solubility (mg/cm2) | 0.02 (water), 0.04 (hydrocarbons) | [82] |
| Color | Transparent, colorless | [7] |
| Property | Conventional Heat-Cured PMMA | CAD/CAM PMMA | Reference |
|---|---|---|---|
| Chemistry | Similar | [208] | |
| Monomer leaching | No significant differences | [212] | |
| Biocompatibility | Similar | [208] | |
| Manipulation | Flask-pack-press’ | Rapid prototyping and milling techniques | [208] |
| Candida albicans adherence/stomatitis | Reduced | [207] | |
| Mechanical properties | Improved | [204,208] | |
| Hardness | Increased | [206] | |
| Flexural strength | Improved | [203,204,205] | |
| Flexural modulus and impact strength | Improved | [204] | |
| Durability | Improved | [204] | |
| Teeth bond strength | Higher; reduced with aging | Lower; less effect with aging | [209] |
| Hydrophobicity | Higher | [205,206,207] | |
| Contact angle | Lower | [205] | |
| Surface roughness | Similar | [205] | |
| Lower | [207] | ||
| Ra=0.2µm, which is below the threshold for plaque accumulation | [123] | ||
| Fiber type | Characteristic Description and Main Outcomes | Reference |
|---|---|---|
| Carbon | Enhancement of the mechanical properties, including tensile strength, flexibility, fracture resistance, and elastic modulus. | [20,242] |
| Reduced thermal expansion of modified PMMA materials. | [20] | |
| Poor aesthetic properties due to the color of fibers. | ||
| Aramid (Kevlar) | Polyamide fibers that have better wettability (coupling pre-treatment is not required) and improved mechanical properties, such as fracture resistance. | [243] |
| Poor aesthetics due to yellowish color; fibers exposed to the surface are irritable to patient’s tissues. Difficult to finish and polish the surface. | [18,75,244] | |
| Increasing the concentration of fibers reduced the hardness. | [18,75] | |
| Nylon | Adding nylon fibers improved the flexural strength. | [245] |
| Improved structural elasticity and fracture resistance. | [103] | |
| Polyethene and polypropylene | Adding surface-treated fibers improved the impact strength. | [21,139] |
| Superior toughness and ductility. | [22,246,247] | |
| In addition to impact strength, adding silanized fibers improved the tensile and transverse strengths of heat-cured PMMA, however wear resistance was poor. | [17] | |
| The aesthetic properties were not affected due to their white color. | [21,243] | |
| Technique was sensitive and required surface treatment, therefore is not used extensively. | [243] | |
| Glass | Glass fibers can be used in various forms (woven, loose); provide excellent reinforcement and aesthetics compared to other fibers. | [245] |
| A remarkable increase in the denture base toughness, Vickers hardness, impact strength, and flexural strength was observed. | [15,16,248,249] | |
| A remarkable reduction in the deformation (<1%). | [15] | |
| The silanized glass fibers enhanced the flexural strength, while the strength of modified PMMA may be influenced by the proportion and positioning of fibers. | [19] |
| Particles | Modification and Outcome | Reference |
|---|---|---|
| Alumina (Al2O3) | Addition of alumina Al2O3 nanoparticles to PMMA powder resulted in good biocompatibility. | [277] |
| Silane-treated aluminium particles remarkably improved the mechanical properties—mainly the compressive and flexural strengths, as well as the wear resistance. | [25,26] | |
| No significant effects on the water sorption or surface roughness of PMMA. | [145] | |
| Significantly improves the thermal conductivity of PMMA. | [255] | |
| The main limitation of the Al2O3 reinforcement is that it causes discoloration of the resin. | [25] | |
| Zirconia (ZrO2) | Significant improvement in mechanical properties, including fracture toughness, compressive and fatigue strengths. | [29,30,31,32] |
| Using silane coupling agent (3.5%) improved the PMMA–ZrO2 interface and flexural strength. | [278] | |
| ZrO2 nanoparticles (NPs) added to the PMMA improved the thermal conductivity. | [31] | |
| The ZrO2 nanotubes demonstrated superior reinforcing effects compared to ZrO2 particles. | [270] | |
| Increased the water sorption, however it remained within the limits. | [279] | |
| Titania (TiO2) | Adding TiO2 particles enhanced the thermal conductivity, fracture toughness, and hardness. | [254] |
| Increase in the impact strength. | [280] | |
| The addition of silanized TiO2 particles showed similar effects by improving the surface hardness, transverse and impact strengths. The water sorption and solubility were also reduced. | [267] | |
| The fluorapatite or apatite-coated TiO2 demonstrated antifungal effects and inhibited Candida growth. | [262,263] | |
| Due to poor wettability, there is a need for titanium coupling agent reinforcement in PMMA. The modification of PMMA by the incorporation of barium titanate (radiopacifier) reduced the fracture toughness. | [281] | |
| Silver | Due to their metallic nature, adding silver particles improved the compressive strength and thermal conductivity of PMMA. | [23,24] |
| Due to their antimicrobial properties, silver particles inhibit bacterial attachment. Dentures containing siliver nanoparticles have shown antifungal activity. | [257,258,259,260,261] | |
| The addition of silver and graphene nanoparticles to PMMA significantly enhanced the mechanical properties (tensile, compressive, and flexural strengths) and lowered the water absorption. | [268] | |
| No significant changes in the flexural strength of PMMA. | [255] | |
| Nanodiamond (ND) | The ND particles are bioactive and reinforce acrylic polymers. | [54,282] |
| Adding ND nanoclusters (20nm; ~0.83 wt%) to PMMA significantly improved the elastic modulus (~2.084GPa) and impact strength. | [282] | |
| Adding only 0.1 wt.% ND to PMMA remarkably increased the flexural strength, in addition to inhibiting the growth of Candida albicans fungal infection and salivary biofilm. | [283] | |
| Diminished Candida albicans attachment corresponding to the reduced surface roughness, therefore may benefit in the prevention of denture stomatitis. | [284] | |
| Hydroxyapatite (HA) | Inorganic HA improved the PMMA properties, including the elastic modulus and flexural strength. | [27,28] |
| Silica (SiO2) based particles | The SiO2 nanoparticles improved the mechanical properties of PMMA. | [33,34,35,36] |
| The PMMA modified by mica showed improved surface hardness, dimensional stability, and thermal properties. However, the flexural strength was compromised due to the weakening of mica bonding with the acrylic resin. | [256] | |
| The fluoride glass fillers containing PMMA inhibited the microbial adhesion but enhanced the surface roughness. | [264,265] | |
| The incorporation of mesoporous silica nanoparticles loaded with an antifungal drug (amphotericin B) resulted in long-term antifungal activity against Candida albicans. | [266] | |
| Increasing the concentration of nanosilica may lead to biocompatibility issues; however, at lower concentrations (less than 2%) there is no cytotoxicity. | [35] |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zafar, M.S. Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update. Polymers 2020, 12, 2299. https://0-doi-org.brum.beds.ac.uk/10.3390/polym12102299
Zafar MS. Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update. Polymers. 2020; 12(10):2299. https://0-doi-org.brum.beds.ac.uk/10.3390/polym12102299
Chicago/Turabian StyleZafar, Muhammad Sohail. 2020. "Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update" Polymers 12, no. 10: 2299. https://0-doi-org.brum.beds.ac.uk/10.3390/polym12102299