Influence of Polymeric Restorative Materials on the Stress Distribution in Posterior Fixed Partial Dentures: 3D Finite Element Analysis
Abstract
:1. Introduction
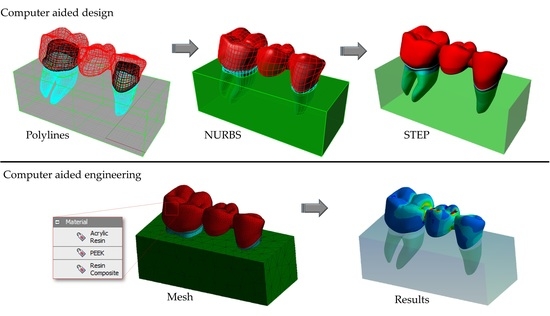
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dayan, C.; Kiseri, B.; Gencel, B.; Kurt, H.; Tuncer, N. Wear resistance and microhardness of various interim fixed prosthesis materials. J. Oral Sci. 2019, 61, 447–453. [Google Scholar] [CrossRef] [Green Version]
- Hahnel, S.; Krifka, S.; Behr, M.; Kolbeck, C.; Lang, R.; Rosentritt, M. Performance of resin materials for temporary fixed denture prostheses. J. Oral Sci. 2019, 61, 270–275. [Google Scholar] [CrossRef] [Green Version]
- Lo Giudice, R.; Famà, F. Health Care and Health Service Digital Revolution. Int. J. Environ. Res. Public Health 2020, 17, 4913. [Google Scholar] [CrossRef]
- Burke, F.J.T.; Murray, M.C.; Shortall, A.C.C. Trends in indirect dentistry: 6. Provisional restorations, more than just a temporary. Dent. Update 2005, 32, 443–452. [Google Scholar] [CrossRef]
- John, P.; Muthukumar, B.; Kumar, M.V. Comparison of the Effect of Dentin Bonding, Dentin Sealing Agents on the Microleakage of Provisional Crowns Fabricated with Direct and Indirect Technique-An Invitro Study. J. Clin. Diagn. Res. 2015, 9, 54–57. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; Borges, A.L.S.; Silva-Concílio, L.R.; Bottino, M.A.; Özcan, M. Effect of Restorative Material on Mechanical Response of Provisional Endocrowns: A 3D—FEA Study. Materials 2021, 14, 649. [Google Scholar] [CrossRef] [PubMed]
- Klur, T.; Hasan, I.; Ottersbach, K.; Stark, H.; Fichte, M.; Dirk, C.; Bourauel, C. PEKK-made indirect temporary crowns and bridges: A clinical pilot study. Clin. Oral Investig. 2019, 23, 771–777. [Google Scholar] [CrossRef] [PubMed]
- Schwantz, J.K.; Oliveira-Ogliari, A.; Meereis, C.T.; Leal, F.B.; Ogliari, F.A.; Moraes, R.R. Characterization of Bis-Acryl Resin composites for Provisional Restorations. Braz. Dent. J. 2017, 28, 354–361. [Google Scholar] [CrossRef] [Green Version]
- Zafar, M.S. Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update. Polymers 2020, 12, 2299. [Google Scholar] [CrossRef] [PubMed]
- Balkenhol, M.; Ferger, P.; Mautner, M.C.; Wöstmann, B. Provisional crown and fixed partial denture materials: Mechanical properties and degree of conversion. Dent. Mater. 2007, 23, 1574–1583. [Google Scholar] [CrossRef]
- Vaidyanathan, T.; Vaidyanathan, J.; Manasse, M. Analysis of stress relaxation in temporization materials in dentistry. Dent. Mater. 2015, 31, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Knobloch, L.A.; Kerby, R.E.; Pulido, T.; Johnston, W.M. Relative fracture toughness of bis-acryl interim resin materials. J. Prosthet. Dent. 2011, 106, 118–125. [Google Scholar] [CrossRef]
- Yao, J.; Li, J.; Wang, Y.; Huang, H. Comparison of the flexural strength and marginal accuracy of traditional and CAD/CAM interim materials before and after thermal cycling. J. Prosthet. Dent. 2014, 112, 649–657. [Google Scholar] [CrossRef]
- Bayindir, F.; Kürklü, D.; Yanikoğlu, N.D. The effect of staining solutions on the color stability of provisional prosthodontic materials. J. Dent. 2012, 40, 41–46. [Google Scholar] [CrossRef]
- Lauvahutanon, S.; Takahashi, H.; Shiozawa, M.; Iwasaki, N.; Asakawa, Y.; Oki, M.; Finger, W.J.; Arksornnukit, M. Mechanical properties of composite resin blocks for CAD/CAM. Dent. Mater. J. 2014, 33, 705–710. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ma, R.; Tang, T. Current strategies to improve the bioactivity of PEEK. Int. J. Mol. Sci. 2014, 15, 26–45. [Google Scholar] [CrossRef] [Green Version]
- Skirbutis, G.; Dzingutė, A.; Masiliūnaitė, V.; Šulcaitė, G.; Žilinskas, J. A review of PEEK polymer’s properties and its use in prosthodontics. Stomatologija 2017, 19, 19–23. [Google Scholar] [PubMed]
- Garcia Gonzalez, D.; Rusinek, A.; Jankowiak, T.; Arias, A. Mechanical impact behavior of polyether-ether-ketone (PEEK). Compos. Struct. 2015, 124, 88–99. [Google Scholar] [CrossRef] [Green Version]
- Tetelman, E.D.; Babbush, C.A. A new transitional abutment for immediate aesthetics and function. Implant Dent. 2008, 17, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Noiset, O.; Schneider, Y.J.; Marchand-Brynaert, J. Adhesion and growth of CaCo2 cells on surface-modified PEEK substrate. J. Biomater. Sci. Polym. Ed. 2000, 11, 767–786. [Google Scholar] [CrossRef] [PubMed]
- Stawarczyk, B.; Beuer, F.; Wimmer, T.; Jahn, D.; Sener, B.; Roos, M.; Schmidlin, P.R. Polyetheretherketone—A suitable material for fixed dental prostheses? J. Biomed. Mater. Res. Part B Appl. Biomater. 2013, 101, 1209–1216. [Google Scholar] [CrossRef]
- Villefort, R.F.; Tribst, J.P.M.; Dal Piva, A.M.O.; Borges, A.L.; Binda, N.C.; Ferreira, C.E.A.; Bottino, M.A.; von Zeidler, S.L.V. Stress distribution on different bar materials in implant-retained palatal obturator. PLoS ONE 2020, 15, e0241589. [Google Scholar] [CrossRef]
- Kurtz, S.M.; Devine, J.N. PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials 2007, 28, 4845–4869. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Najeeb, S.; Zafar, M.S.; Khurshid, Z.; Siddiqui, F. Applications of polyetheretherketone (PEEK) in oral implantology and prosthodontics. J. Prosthodont. Res. 2016, 60, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Kolbeck, C.; Behr, M.; Rosentritt, M.; Handel, G. Fracture force of tooth–tooth- and implant–tooth-supported all-ceramic fixed partial dentures using titanium vs. customised zirconia implant abutments. Clin. Oral Implant. Res. 2008, 19, 1049–1053. [Google Scholar] [CrossRef] [PubMed]
- Stawarczyk, B.; Eichberger, M.; Uhrenbacher, J.; Wimmer, T.; Edelhoff, D.; Schmidlin, P.R. Three-unit reinforced polyetheretherketone composite FDPs: Influence of fabrication method on load-bearing capacity and failure types. Dent. Mater. J. 2015, 34, 7–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kassem, Y.M.; Alshimy, A.M.; El-Shabrawy, S.M. Mechanical Evaluation of Polyetheretherketone Compared with Zirconia as a Dental Implant Material. Alex. Dent. J. 2019, 44, 61–66. [Google Scholar] [CrossRef] [Green Version]
- Khalesi, R.; Abbasi, M.; Shahidi, Z.; Tabatabaei, M.H.; Moradi, Z. Interfacial Fracture Toughness Comparison of Three Indirect Resin Composites to Dentin and Polyether Ether Ketone Polymer. Eur. J. Dent. 2020, 14, 456–461. [Google Scholar]
- Ausiello, P.; Apicella, A.; Davidson, C.L.; Rengo, S. 3D-finite element analyses of cusp movements in a human upper premolar, restored with adhesive resin-based composites. J. Biomech. 2001, 34, 1269–1277. [Google Scholar] [CrossRef]
- Prado, F.B.; Rossi, A.C.; Freire, A.R.; Ferreira Caria, P.H. The application of finite element analysis in the skull biomechanics and dentistry. Indian J. Dent. Res. 2014, 25, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Dal Piva, A.M.O.; Tribst, J.P.M.; Saavedra, G.S.F.A.; Souza, R.O.A.; de Melo, R.M.; Borges, A.L.S.; Özcan, M. Short communication: Influence of retainer configuration and loading direction on the stress distribution of lithium disilicate resin-bonded fixed dental prostheses: 3D finite element analysis. J. Mech. Behav. Biomed. Mater. 2019, 100, 103389. [Google Scholar] [CrossRef]
- Penteado, M.M.; Tribst, J.P.M.; Dal Piva, A.M.; Ausiello, P.; Zarone, F.; Garcia-Godoy, F.; Borges, A.L.S. Mechanical behavior of conceptual posterior dental crowns with functional elasticity gradient. Am. J. Dent. 2019, 32, 165–168. [Google Scholar]
- da Fonseca, G.F.; Dal Piva, A.M.; Tribst, J.P.; Borges, A.L. Influence of Restoration Height and Masticatory Load Orientation on Ceramic Endocrowns. J. Contemp. Dent. Pract. 2018, 19, 1052–1057. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.M.; Dal Piva, A.M.O.; Penteado, M.M.; Borges, A.L.S.; Bottino, M.A. Influence of ceramic material, thickness of restoration and cement layer on stress distribution of occlusal veneers. Braz. Oral Res. 2018, 32, e118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monteiro, J.B.; Dal Piva, A.M.O.; Tribst, J.P.M.; Borges, A.L.S.; Tango, R.N. The Effect of Resection Angle on Stress Distribution after Root-End Surgery. Iran. Endod. J. 2018, 13, 188–194. [Google Scholar]
- Shibasaki, S.; Takamizawa, T.; Suzuki, T.; Nojiri, K.; Tsujimoto, A.; Barkmeier, W.W.; Latta, M.A.; Miyazaki, M. Influence of Different Curing Modes on Polymerization Behavior and Mechanical Properties of Dual-Cured Provisional Resins. Oper. Dent. 2017, 42, 526–536. [Google Scholar] [CrossRef]
- Dejak, B.; Młotkowski, A. A comparison of mvM stress of inlays, onlays and endocrowns made from various materials and their bonding with molars in a computer simulation of mastication—FEA. Dent. Mater. 2020, 36, 854–864. [Google Scholar] [CrossRef]
- Helal, M.A.; Wang, Z. Biomechanical Assessment of Restored Mandibular Molar by Endocrown in Comparison to a Glass Fiber Post-Retained Conventional Crown: 3D Finite Element Analysis. J. Prosthodont. 2019, 28, 988–996. [Google Scholar] [CrossRef] [PubMed]
- Nagai, E.; Otani, K.; Satoh, Y.; Suzuki, S. Repair of denture base resin using woven metal and glass fiber: Effect of methylene chloride pretreatment. J. Prosthet. Dent. 2001, 85, 496–500. [Google Scholar] [CrossRef]
- Srirekha, A.; Bashetty, K. A comparative analysis of restorative materials used in abfraction lesions in tooth with and without occlusal restoration: Three-dimensional finite element analysis. J. Conserv. Dent. 2013, 16, 157–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qin, L.; Yao, S.; Zhao, J.; Zhou, C.; Oates, T.W.; Weir, M.D.; Wu, J.; Xu, H.H.K. Review on Development and Dental Applications of Polyetheretherketone-Based Biomaterials and Restorations. Materials 2021, 14, 408. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.L.; Lai, Y.L.; Chou, I.C.; Hu, C.J.; Lee, S.Y. Shear bond strength of provisional restoration materials repaired with light-cured resins. Oper. Dent. 2008, 33, 508–515. [Google Scholar] [CrossRef]
- Goodacre, C.J.; Bernal, G.; Rungcharassaeng, K.; Kan, J.Y. Clinical complications in fixed prosthodontics. J. Prosthet. Dent. 2003, 90, 31–41. [Google Scholar] [CrossRef] [Green Version]
- Papazoglou, E.; Vasilas, A.I. Shear bond strengths for composite and autopolymerized acrylic resins bonded to acrylic resin denture teeth. J. Prosthet. Dent. 1999, 82, 573–578. [Google Scholar] [CrossRef]
- Correia, A.M.O.; Andrade, M.R.; Tribst, J.P.M.; Borges, A.L.S.; Caneppele, T.M.F. Influence of Bulk-fill Restoration on Polymerization Shrinkage Stress and Marginal Gap Formation in Class V Restorations. Oper. Dent. 2020, 45, E207–E216. [Google Scholar] [CrossRef]
- Burns, D.R.; Beck, D.A.; Nelson, S.K. A review of selected dental literature on contemporary provisional fixed prosthodontic treatment: Report of the Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. J. Prosthet. Dent. 2003, 90, 474–497. [Google Scholar] [CrossRef]
- Rauch, A.; Hahnel, S.; Günther, E.; Bidmon, W.; Schierz, O. Tooth-Colored CAD/CAM Materials for Application in 3-Unit Fixed Dental Prostheses in the Molar Area: An Illustrated Clinical Comparison. Materials 2020, 13, 5588. [Google Scholar] [CrossRef]
- Niem, T.; Youssef, N.; Wöstmann, B. Energy dissipation capacities of CAD-CAM restorative materials: A comparative evaluation of resilience and toughness. J. Prosthet. Dent. 2019, 121, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Niem, T.; Youssef, N.; Wöstmann, B. Influence of accelerated ageing on the physical properties of CAD/CAM restorative materials. Clin. Oral Investig. 2020, 24, 2415–2425. [Google Scholar] [CrossRef] [PubMed]
- Dal Piva, A.M.O.; Tribst, J.P.M.; Borges, A.L.S.; Souza, R.O.A.E.; Bottino, M.A. CAD-FEA modeling and analysis of different full crown monolithic restorations. Dent. Mater. 2018, 34, 1342–1350. [Google Scholar] [CrossRef] [Green Version]
- Yamaguchi, S.; Kani, R.; Kawakami, K.; Tsuji, M.; Inoue, S.; Lee, C.; Kiba, W.; Imazato, S. Fatigue behavior and crack initiation of CAD/CAM resin composite molar crowns. Dent. Mater. 2018, 34, 1578–1584. [Google Scholar] [CrossRef]
- Harshitha Gowda, B.H.; Satish Babu, C.L. Connector design in a long-span-fixed dental prosthesis: A three-dimensional finite element analysis. Indian J. Dent. Res. 2013, 24, 178–182. [Google Scholar] [CrossRef]
- Hill, E.E.; Lott, J. A clinically focused discussion of luting materials. Aust. Dent. J. 2011, 56, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Carmello, J.C.; Fais, L.M.G.; Ribeiro, L.N.M.; Claro Neto, S.; Guaglianoni, D.G.; Pinelli, L.A.P. Diametral tensile strength and film thickness of an experimental dental luting agent derived from castor oil. J. Appl. Oral Sci. 2012, 20, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Scribante, A.; Gallo, S.; Scarantino, S.; Dagna, A.; Poggio, C.; Colombo, M. Exposure of Biomimetic Composite Materials to Acidic Challenges: Influence on Flexural Resistance and Elastic Modulus. Biomimetics 2020, 5, 56. [Google Scholar] [CrossRef]
- Iconaru, S.L.; Prodan, A.M.; Turculet, C.S.; Beuran, M.; Ghita, R.V.; Costescu, A.; Groza, A.; Chifiriuc, M.C.; Chapon, P.; Gaiaschi, S.; et al. Enamel Based Composite Layers Deposited on Titanium Substrate with Antifungal Activity. J. Spectrosc. 2016, 2016, 1–13. [Google Scholar] [CrossRef]
- Groza, A.; Ciobanu, C.S.; Popa, C.L.; Iconaru, S.L.; Chapon, P.; Luculescu, C.; Ganciu, M.; Predoi, D. Structural Properties and Antifungal Activity against Candida albicans Biofilm of Different Composite Layers Based on Ag/Zn Doped Hydroxyapatite-Polydimethylsiloxanes. Polymers 2016, 8, 131. [Google Scholar] [CrossRef] [Green Version]
- Colombo, M.; Gallo, S.; Poggio, C.; Ricaldone, V.; Arciola, C.R.; Scribante, A. New Resin-Based Bulk-Fill Composites: In vitro Evaluation of Micro-Hardness and Depth of Cure as Infection Risk Indexes. Materials 2020, 13, 1308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gloria, A.; Maietta, S.; Martorelli, M.; Lanzotti, A.; Watts, D.C.; Ausiello, P. FE analysis of conceptual hybrid composite endodontic post designs in anterior teeth. Dent. Mater. 2018, 34, 1063–1071. [Google Scholar] [CrossRef] [Green Version]
- Ausiello, P.; Ciaramella, S.; De Benedictis, A.; Lanzotti, A.; Tribst, J.P.M.; Watts, D.C. The use of different adhesive filling material and mass combinations to restore class II cavities under loading and shrinkage effects: A 3D-FEA. Comput. Methods Biomech. Biomed. Eng. 2020, 22, 1–11. [Google Scholar] [CrossRef] [PubMed]






| Material/ Structure | Composition | Elastic Modulus (GPa) * | Poisson Ratio |
|---|---|---|---|
| Enamel | - | 80 | 0.30 |
| Dentin | - | 18 | 0.23 |
| Fixation cylinder | Polyurethane resin | 3.6 | 0.30 |
| Cement | Zinc oxide-based cement | 1.35 | 0.30 |
| Acrylic resin | Polymethyl methacrylate, diethyl phthalate, benzoyl peroxide, titanium dioxide | 2.2 | 0.30 |
| PEEK | 100% Polyetheretherketone | 3.0 | 0.30 |
| Resin composite | UDMA, Bis-GMA, Bis-EMA, TEGDMA, Silica and fillers. | 8.0 | 0.25 |
| Prostheses | Cement | |||
|---|---|---|---|---|
| Material | Molar Connector | Premolar Connector | Molar Abutment | Premolar Abutment |
| AR | 114.6 | 69.4 | 21.8 | 21.5 |
| PEEK | 123.1 | 78.5 | 21.5 | 15.5 |
| RC | 129.4 | 88.5 | 14.9 | 14.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Campaner, L.M.; Silveira, M.P.M.; de Andrade, G.S.; Borges, A.L.S.; Bottino, M.A.; Dal Piva, A.M.d.O.; Lo Giudice, R.; Ausiello, P.; Tribst, J.P.M. Influence of Polymeric Restorative Materials on the Stress Distribution in Posterior Fixed Partial Dentures: 3D Finite Element Analysis. Polymers 2021, 13, 758. https://0-doi-org.brum.beds.ac.uk/10.3390/polym13050758
Campaner LM, Silveira MPM, de Andrade GS, Borges ALS, Bottino MA, Dal Piva AMdO, Lo Giudice R, Ausiello P, Tribst JPM. Influence of Polymeric Restorative Materials on the Stress Distribution in Posterior Fixed Partial Dentures: 3D Finite Element Analysis. Polymers. 2021; 13(5):758. https://0-doi-org.brum.beds.ac.uk/10.3390/polym13050758
Chicago/Turabian StyleCampaner, Larissa Mendes, Marcos Paulo Motta Silveira, Guilherme Schmitt de Andrade, Alexandre Luiz Souto Borges, Marco Antonio Bottino, Amanda Maria de Oliveira Dal Piva, Roberto Lo Giudice, Pietro Ausiello, and João Paulo Mendes Tribst. 2021. "Influence of Polymeric Restorative Materials on the Stress Distribution in Posterior Fixed Partial Dentures: 3D Finite Element Analysis" Polymers 13, no. 5: 758. https://0-doi-org.brum.beds.ac.uk/10.3390/polym13050758