The Effect of Intra-articular Injection of Autologous Microfragmented Fat Tissue on Proteoglycan Synthesis in Patients with Knee Osteoarthritis
Abstract
:1. Introduction
2. Patients and Methods
2.1. Study Design
2.2. Blood and Synovial Specimen Collection and Processing
2.3. Transplantation and Processing of Microfragmented Adipose Tissue with Ad-MSCs
2.4. Immunoglobulin G Isolation from Plasma and Synovial Fluid Samples
2.5. N-glycan Release, Labeling and Analysis by Ultra-Performance Liquid Chromatography
2.6. Radiography
2.7. MR Imaging
2.8. dGEMRIC Protocol
2.9. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Safety and Chondrotoxicity Profile of Intra-Articular Injection of Autologous Microfragmented Adipose Tissue
3.3. Basic Clinical Outcomes: Visual Analogue Scale for Pain Assessment and C-Reactive Protein
3.4. N-Glycan Profile Analysis
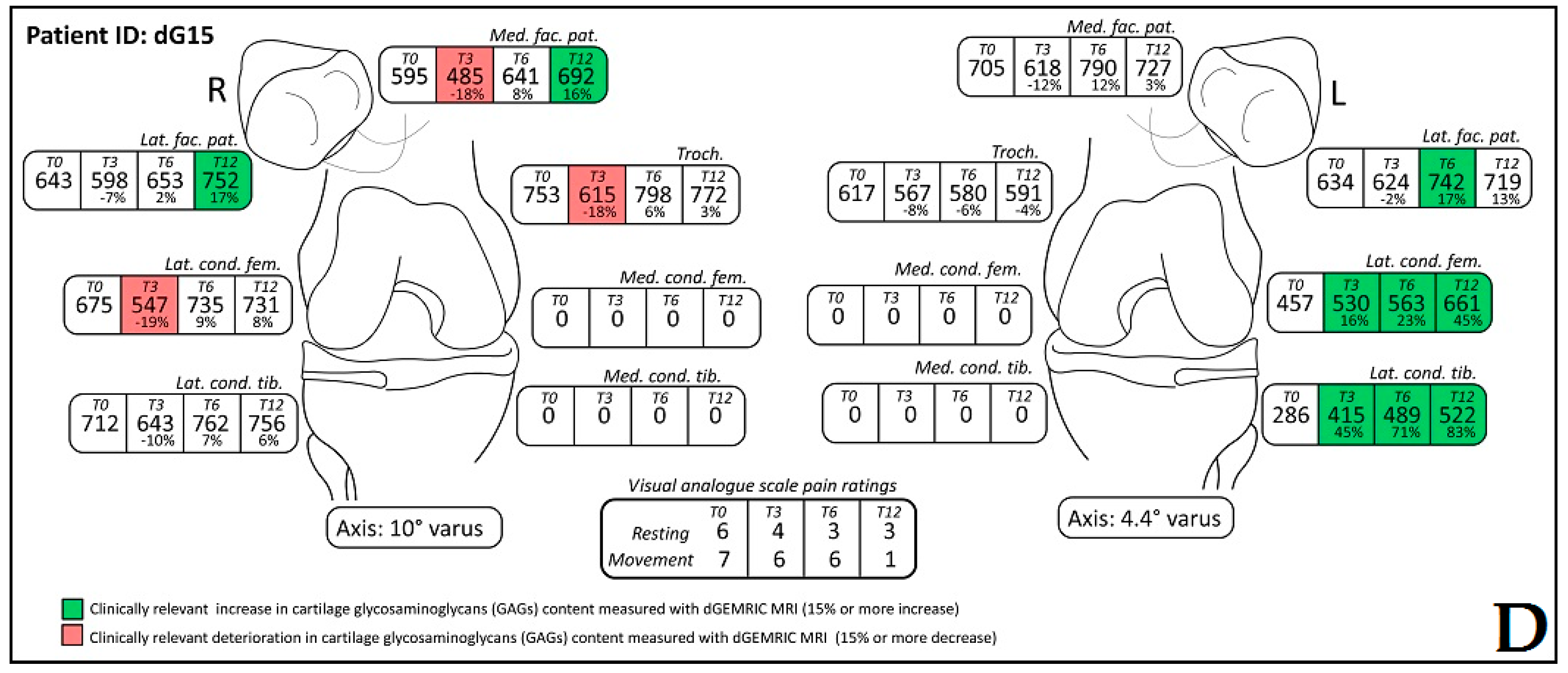
3.5. Delayed Gadolinium-Enhanced MRI of Cartilage (dGEMRIC)
4. Discussion
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Kurz, B.; Lemke, A.K.; Fay, J.; Pufe, T.; Grodzinsky, A.J.; Schunke, M. Pathomechanisms of cartilage destruction by mechanical injury. Ann. Anat. 2005, 187, 473–485. [Google Scholar] [CrossRef] [PubMed]
- Boshuizen, H.C.; Poos, M.J.; van den Akker, M.; van Boven, K.; Korevaar, J.C.; de Waal, M.W.; Biermans, M.C.; Hoeymans, N. Estimating incidence and prevalence rates of chronic diseases using disease modeling. Popul. Health Metr. 2017, 15, 13. [Google Scholar] [CrossRef] [PubMed]
- Hunter, D.J.; Schofield, D.; Callander, E. The individual and socioeconomic impact of osteoarthritis. Nat. Rev. Rheumatol. 2014, 10, 437–441. [Google Scholar] [CrossRef] [PubMed]
- Orchard, J.; Moen, M.H. Has reimbursement for knee osteoarthritis treatments now reached ‘postfact’ status? Br. J. Sports Med. 2017, 29, 2017-097605. [Google Scholar] [CrossRef] [PubMed]
- Primorac, D.; Stover, M.L.; Clark, S.H.; Rowe, D.W. Molecular basis of nanomelia, a heritable chondrodystrophy of chicken. Matrix Biol. 1994, 14, 297–305. [Google Scholar] [CrossRef]
- Primorac, D.; Johnson, C.V.; Lawrence, J.B.; McKinstry, M.B.; Stover, M.L.; Schanfield, M.S.; Andjelinovic, S.; Tadic, T.; Rowe, D.W. Premature termination codon in the aggrecan gene of nanomelia and its influence on mrna transport and stability. Croat. Med. J. 1999, 40, 528–532. [Google Scholar] [PubMed]
- Horton, W.E., Jr.; Bennion, P.; Yang, L. Cellular, molecular, and matrix changes in cartilage during aging and osteoarthritis. J. Musculoskelet. Neuronal Interact. 2006, 6, 379–381. [Google Scholar] [PubMed]
- Rahmati, M.; Nalesso, G.; Mobasheri, A.; Mozafari, M. Aging and osteoarthritis: Central role of the extracellular matrix. Ageing Res. Rev. 2017, 40, 20–30. [Google Scholar] [CrossRef] [PubMed]
- Brinker, M.R.; O’Connor, D.P. Articular tissues. In Review of Orthopaedics, 6th ed.; Miller, M., Thompson, S., Hart, J., Eds.; Elsevier Saunders: Philadelphia, PA, USA, 2012; pp. 39–48. [Google Scholar]
- Buckwalter, J.A.; Woo, S.L.; Goldberg, V.M.; Hadley, E.C.; Booth, F.; Oegema, T.R.; Eyre, D.R. Soft-tissue aging and musculoskeletal function. J. Bone Joint Surg. Am. 1993, 75, 1533–1548. [Google Scholar] [CrossRef] [PubMed]
- Mobasheri, A.; Matta, C.; Zakany, R.; Musumeci, G. Chondrosenescence: Definition, hallmarks and potential role in the pathogenesis of osteoarthritis. Maturitas 2015, 80, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Greene, M.A.; Loeser, R.F. Aging-related inflammation in osteoarthritis. Osteoarthr. Cartil. 2015, 23, 1966–1971. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, L.T.; Sharma, A.R.; Chakraborty, C.; Saibaba, B.; Ahn, M.E.; Lee, S.S. Review of prospects of biological fluid biomarkers in osteoarthritis. Int. J. Mol. Sci. 2017, 18, 601. [Google Scholar] [CrossRef] [PubMed]
- Mobasheri, A.; Henrotin, Y. Biomarkers of (osteo)arthritis. Biomarkers 2015, 20, 513–518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lauc, G.; Pezer, M.; Rudan, I.; Campbell, H. Mechanisms of disease: The human N-glycome. Biochim. Biophys. Acta 2016, 1860, 1574–1582. [Google Scholar] [CrossRef] [PubMed]
- Drake, P.M.; Cho, W.; Li, B.; Prakobphol, A.; Johansen, E.; Anderson, N.L.; Regnier, F.E.; Gibson, B.W.; Fisher, S.J. Sweetening the pot: Adding glycosylation to the biomarker discovery equation. Clin. Chem. 2010, 56, 223–236. [Google Scholar] [CrossRef] [PubMed]
- Evans, C.H.; Kraus, V.B.; Setton, L.A. Progress in intra-articular therapy. Nat. Rev. Rheumatol. 2014, 10, 11–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Derendorf, H.; Mollmann, H.; Gruner, A.; Haack, D.; Gyselby, G. Pharmacokinetics and pharmacodynamics of glucocorticoid suspensions after intra-articular administration. Clin. Pharmacol. Ther. 1986, 39, 313–317. [Google Scholar] [CrossRef] [PubMed]
- Fraser, J.R.; Kimpton, W.G.; Pierscionek, B.K.; Cahill, R.N. The kinetics of hyaluronan in normal and acutely inflamed synovial joints: Observations with experimental arthritis in sheep. Sem. Arthritis Rheum. 1993, 22, 9–17. [Google Scholar] [CrossRef]
- Caplan, A.I. Adult mesenchymal stem cells: When, where, and how. Stem Cells Int. 2015, 2015, 628767. [Google Scholar] [CrossRef] [PubMed]
- Cuti, T.; Antunovic, M.; Marijanovic, I.; Ivkovic, A.; Vukasovic, A.; Matic, I.; Pecina, M.; Hudetz, D. Capacity of muscle derived stem cells and pericytes to promote tendon graft integration and ligamentization following anterior cruciate ligament reconstruction. Int. Orthop. 2017, 41, 1189–1198. [Google Scholar] [CrossRef] [PubMed]
- Jo, C.H.; Lee, Y.G.; Shin, W.H.; Kim, H.; Chai, J.W.; Jeong, E.C.; Kim, J.E.; Shim, H.; Shin, J.S.; Shin, I.S.; et al. Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: A proof-of-concept clinical trial. Stem Cells 2014, 32, 1254–1266. [Google Scholar] [CrossRef] [PubMed]
- Pers, Y.M.; Rackwitz, L.; Ferreira, R.; Pullig, O.; Delfour, C.; Barry, F.; Sensebe, L.; Casteilla, L.; Fleury, S.; Bourin, P.; et al. Adipose mesenchymal stromal cell-based therapy for severe osteoarthritis of the knee: A phase I dose-escalation trial. Stem Cells Transl. Med. 2016, 5, 847–856. [Google Scholar] [CrossRef] [PubMed]
- Tremolada, C.; Colombo, V.; Ventura, C. Adipose tissue and mesenchymal stem cells: State of the art and Lipogems® technology development. Curr. Stem Cell Rep. 2016, 2, 304–312. [Google Scholar] [CrossRef] [PubMed]
- Schreiner, M.M.; Mlynarik, V.; Zbyn, S.; Szomolanyi, P.; Apprich, S.; Windhager, R.; Trattnig, S. New technology in imaging cartilage of the ankle. Cartilage 2017, 8, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Eagle, S.; Potter, H.G.; Koff, M.F. Morphologic and quantitative magnetic resonance imaging of knee articular cartilage for the assessment of post-traumatic osteoarthritis. J. Orthop. Res. 2017, 35, 412–423. [Google Scholar] [CrossRef] [PubMed]
- Tiderius, C.J.; Olsson, L.E.; Nyquist, F.; Dahlberg, L. Cartilage glycosaminoglycan loss in the acute phase after an anterior cruciate ligament injury: Delayed gadolinium-enhanced magnetic resonance imaging of cartilage and synovial fluid analysis. Arthritis Rheum. 2005, 52, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Young, A.A.; Stanwell, P.; Williams, A.; Rohrsheim, J.A.; Parker, D.A.; Giuffre, B.; Ellis, A.M. Glycosaminoglycan content of knee cartilage following posterior cruciate ligament rupture demonstrated by delayed gadolinium-enhanced magnetic resonance imaging of cartilage (dGEMRIC). A case report. J. Bone Joint Surg. Am. 2005, 87, 2763–2767. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.; Gillis, A.; McKenzie, C.; Po, B.; Sharma, L.; Micheli, L.; McKeon, B.; Burstein, D. Glycosaminoglycan distribution in cartilage as determined by delayed gadolinium-enhanced mri of cartilage (dGEMRIC): Potential clinical applications. AJR Am. J. Roentgenol. 2004, 182, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Burstein, D.; Velyvis, J.; Scott, K.T.; Stock, K.W.; Kim, Y.J.; Jaramillo, D.; Boutin, R.D.; Gray, M.L. Protocol issues for delayed Gd(DTPA)2--enhanced MRI (dGEMRIC) for clinical evaluation of articular cartilage. Magn. Reson. Med. 2001, 45, 36–41. [Google Scholar] [CrossRef]
- Tiderius, C.J.; Olsson, L.E.; Leander, P.; Ekberg, O.; Dahlberg, L. Delayed gadolinium-enhanced mri of cartilage (dGEMRIC) in early knee osteoarthritis. Magn. Reson. Med. 2003, 49, 488–492. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, F.; Maioli, M.; Leonardi, E.; Olivi, E.; Pasquinelli, G.; Valente, S.; Mendez, A.J.; Ricordi, C.; Raffaini, M.; Tremolada, C.; et al. A new nonenzymatic method and device to obtain a fat tissue derivative highly enriched in pericyte-like elements by mild mechanical forces from human lipoaspirates. Cell Transp. 2013, 22, 2063–2077. [Google Scholar] [CrossRef] [PubMed]
- Trbojevic-Akmacic, I.; Ugrina, I.; Lauc, G. Comparative analysis and validation of different steps in glycomics studies. Methods Enzymol. 2017, 586, 37–55. [Google Scholar] [PubMed]
- Pucic, M.; Knezevic, A.; Vidic, J.; Adamczyk, B.; Novokmet, M.; Polasek, O.; Gornik, O.; Supraha-Goreta, S.; Wormald, M.R.; Redzic, I.; et al. High throughput isolation and glycosylation analysis of IgG-variability and heritability of the IgG glycome in three isolated human populations. Mol. Cell. Proteom. 2011, 10, M111.010090. [Google Scholar] [CrossRef] [PubMed]
- Kellgren, J.H.; Lawrence, J.S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef] [PubMed]
- Crema, M.D.; Roemer, F.W.; Marra, M.D.; Burstein, D.; Gold, G.E.; Eckstein, F.; Baum, T.; Mosher, T.J.; Carrino, J.A.; Guermazi, A. Articular cartilage in the knee: Current mr imaging techniques and applications in clinical practice and research. Radiographics 2011, 31, 37–61. [Google Scholar] [CrossRef] [PubMed]
- Sonin, A.H.; Pensy, R.A.; Mulligan, M.E.; Hatem, S. Grading articular cartilage of the knee using fast spin-echo proton density-weighted mr imaging without fat suppression. AJR Am. J. Roentgenol. 2002, 179, 1159–1166. [Google Scholar] [CrossRef] [PubMed]
- Tiderius, C.J.; Tjornstrand, J.; Akeson, P.; Sodersten, K.; Dahlberg, L.; Leander, P. Delayed gadolinium-enhanced mri of cartilage (dGEMRIC): Intra- and interobserver variability in standardized drawing of regions of interest. Acta Radiol. 2004, 45, 628–634. [Google Scholar] [CrossRef] [PubMed]
- Bittersohl, B.; Hosalkar, H.S.; Haamberg, T.; Kim, Y.J.; Werlen, S.; Siebenrock, K.A.; Mamisch, T.C. Reproducibility of dgemric in assessment of hip joint cartilage: A prospective study. J. Magn. Reson. Imag. 2009, 30, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Barry, F.; Murphy, M. Mesenchymal stem cells in joint disease and repair. Nat. Rev. Rheumatol. 2013, 9, 584–594. [Google Scholar] [CrossRef] [PubMed]
- Caplan, A.I.; Dennis, J.E. Mesenchymal stem cells as trophic mediators. J. Cell. Biochem. 2006, 98, 1076–1084. [Google Scholar] [CrossRef] [PubMed]
- Mokbel, A.N.; El Tookhy, O.S.; Shamaa, A.A.; Rashed, L.A.; Sabry, D.; El Sayed, A.M. Homing and reparative effect of intra-articular injection of autologus mesenchymal stem cells in osteoarthritic animal model. BMC Musculoskelet. Disord. 2011, 12, 259. [Google Scholar] [CrossRef] [PubMed]
- Sato, K.; Moy, O.J.; Peimer, C.A.; Nakamura, T.; Howard, C.; Ko, S.H.; Lee, T.C.; Nishiwaki, Y. An experimental study on costal osteochondral graft. Osteoarthr. Cartil. 2012, 20, 172–183. [Google Scholar] [CrossRef] [PubMed]
- Caplan, A.I.; Correa, D. The msc: An injury drugstore. Cell Stem Cell 2011, 9, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Goldring, S.R.; Goldring, M.B. The role of cytokines in cartilage matrix degeneration in osteoarthritis. Clin. Orthop. Relat. Res. 2004, S27–S36. [Google Scholar] [CrossRef]
- Roughley, P.J.; Mort, J.S. The role of aggrecan in normal and osteoarthritic cartilage. J. Exp. Orthop. 2014, 1, 8. [Google Scholar] [CrossRef] [PubMed]
- Gray, M.L.; Burstein, D.; Kim, Y.J.; Maroudas, A. 2007 elizabeth winston lanier award winner. Magnetic resonance imaging of cartilage glycosaminoglycan: Basic principles, imaging technique, and clinical applications. J. Orthop. Res. 2008, 26, 281–291. [Google Scholar] [CrossRef] [PubMed]
- Rohrer, M.; Bauer, H.; Mintorovitch, J.; Requardt, M.; Weinmann, H.J. Comparison of magnetic properties of mri contrast media solutions at different magnetic field strengths. Investig. Radiol. 2005, 40, 715–724. [Google Scholar] [CrossRef]
- Franceschi, C.; Bonafe, M.; Valensin, S.; Olivieri, F.; De Luca, M.; Ottaviani, E.; De Benedictis, G. Inflamm-aging. An evolutionary perspective on immunosenescence. Ann. N. Y. Acad. Sci. 2000, 908, 244–254. [Google Scholar] [CrossRef] [PubMed]
- Novokmet, M.; Lukic, E.; Vuckovic, F.; Ethuric, Z.; Keser, T.; Rajsl, K.; Remondini, D.; Castellani, G.; Gasparovic, H.; Gornik, O.; et al. Changes in IgG and total plasma protein glycomes in acute systemic inflammation. Sci. Rep. 2014, 4, 4347. [Google Scholar] [CrossRef] [PubMed]
- Gornik, O.; Lauc, G. Glycosylation of serum proteins in inflammatory diseases. Dis. Markers 2008, 25, 267–278. [Google Scholar] [CrossRef] [PubMed]



| Initial (M0) | First Follow-up (M3) | Second Follow-up (M6) | Third Follow-up (M12) | p * (M0–M3) | p * (M0–M6) | p * (M0–M12) | |
|---|---|---|---|---|---|---|---|
| C-reactive protein (CRP); mean ± SD (min-max) | 6.54 ± 7.83 (1–20.3) | - | 3.86 ± 3.71 (0.6–12) | 5.17 ± 5.83 (0.6–23.1) | - | 0.158 | 0.330 |
| Visual analogue scale pain rating, resting; mean ± SD (min-max) | 3.94 ± 2.56 (0–8) | 1.24 ± 1.48 (0–4) | 1.17 ± 1.62 (0–5) | 0.56 ± 1.2 (0–4) | 0.001 | <0.001 | <0.001 |
| Visual analogue scale pain rating, movement; mean ± SD (min-max) | 7.33 ± 1.72 (4–10) | 3.82 ± 2.07 (1–7) | 3.67 ± 2.03 (0–7) | 3.17 ± 1.98 (0–7) | <0.001 | <0.001 | <0.001 |
| Glycan | Initial Measurement (M0) | First Follow-up (M6) | Second Follow-up (M12) | p * (M0–M6) | p * (M0–M12) |
|---|---|---|---|---|---|
| GP1 | 0.125 ± 0.063 (0.046–0.277) | 0.138 ± 0.055 (0.083–0.258) | 0.127 ± 0.052 (0.044–0.254) | 0.417 | 0.996 |
| GP2 | 1.458 ± 0.97 (0.255–4.007) | 1.131 ± 0.632 (0.249–2.167) | 1.424 ± 0.955 (0.283–3.999) | 0.769 | 0.523 |
| GP3 | 0.113 ± 0.02 (0.09–0.151) | 0.121 ± 0.021 (0.099–0.161) | 0.12 ± 0.023 (0.085–0.162) | 0.065 | 0.142 |
| GP4 | 27.9 ± 8.246 (12.755–46.784) | 29.926 ± 7.142 (22.454–43.436) | 28.143 ± 7.034 (14.145–43.06) | 0.861 | 0.957 |
| GP5 | 0.168 ± 0.028 (0.136–0.218) | 0.167 ± 0.027 (0.139–0.21) | 0.172 ± 0.032 (0.132–0.237) | 0.793 | 0.366 |
| GP6 | 7.135 ± 1.299 (4.313–9.109) | 7.157 ± 1.683 (4.274–10.042) | 7.545 ± 1.663 (4.196–10.429) | 0.142 | 0.050 |
| GP7 | 0.728 ± 0.679 (0.137–2.773) | 0.506 ± 0.207 (0.14–0.759) | 0.709 ± 0.634 (0.203–2.717) | 0.667 | 0.575 |
| GP8 | 18.487 ± 2.753 (13.198–24.336) | 17.622 ± 2.368 (13.641–20.534) | 18.142 ± 2.626 (13.685–23.972) | 0.315 | 0.074 |
| GP9 | 9.416 ± 1.873 (7.167–14.423) | 9.299 ± 2.26 (7.039–14.446) | 9.377 ± 1.8 (6.998–14.379) | 0.611 | 0.562 |
| GP10 | 4.974 ± 0.983 (4.049–7.72) | 5.031 ± 1.159 (3.922–7.585) | 5.145 ± 0.991 (4.072–7.557) | 0.742 | 0.374 |
| GP11 | 0.657 ± 0.082 (0.476–0.756) | 0.672 ± 0.093 (0.526–0.785) | 0.695 ± 0.13 (0.47–0.977) | 0.753 | 0.169 |
| GP12 | 0.973 ± 0.773 (0.186–3.166) | 0.712 ± 0.298 (0.189–1.078) | 0.953 ± 0.732 (0.265–3.121) | 0.600 | 0.152 |
| GP13 | 0.276 ± 0.049 (0.2–0.356) | 0.251 ± 0.041 (0.189–0.31) | 0.275 ± 0.046 (0.207–0.37) | 0.034 | 0.841 |
| GP14 | 10.123 ± 3.266 (3.746–15.708) | 9.512 ± 3.073 (4.507–13.431) | 9.94 ± 2.932 (4.349–14.829) | 0.550 | 0.691 |
| GP15 | 1.506 ± 0.27 (0.999–1.974) | 1.475 ± 0.253 (1.092–1.867) | 1.517 ± 0.221 (1.158–1.875) | 0.197 | 0.786 |
| GP16 | 2.939 ± 0.592 (2.209–4.089) | 2.929 ± 0.613 (2.248–4.007) | 2.878 ± 0.547 (2.263–3.912) | 0.057 | 0.143 |
| GP17 | 0.956 ± 0.186 (0.611–1.159) | 0.904 ± 0.181 (0.664–1.186) | 0.939 ± 0.194 (0.658–1.232) | 0.198 | 0.992 |
| GP18 | 6.668 ± 1.498 (3.225–8.798) | 6.682 ± 1.786 (3.503–9.145) | 6.566 ± 1.449 (3.412–9.026) | 0.822 | 0.961 |
| GP19 | 1.675 ± 0.534 (0.487–2.582) | 1.802 ± 0.366 (1.271–2.326) | 1.682 ± 0.482 (0.481–2.416) | 0.941 | 0.755 |
| GP20 | 0.283 ± 0.066 (0.138–0.393) | 0.257 ± 0.055 (0.169–0.33) | 0.274 ± 0.06 (0.14–0.343) | 0.100 | 0.460 |
| GP21 | 0.48 ± 0.106 (0.312–0.577) | 0.477 ± 0.114 (0.286–0.647) | 0.458 ± 0.091 (0.27–0.578) | 0.886 | 0.151 |
| GP22 | 0.133 ± 0.049 (0.041–0.191) | 0.129 ± 0.037 (0.079–0.19) | 0.131 ± 0.04 (0.046–0.178) | 0.164 | 0.765 |
| GP23 | 1.278 ± 0.414 (0.48–2.001) | 1.375 ± 0.432 (0.753–2.048) | 1.243 ± 0.437 (0.489–1.996) | 0.331 | 0.903 |
| GP24 | 1.55 ± 0.542 (0.427–2.266) | 1.723 ± 0.39 (1.076–2.238) | 1.544 ± 0.521 (0.407–2.515) | 0.453 | 0.748 |
| Glycan | Initial Measurement (M0) | Final Measurement (M12) | p * |
|---|---|---|---|
| GP1 | 0.16 ± 0.06 (0.09–0.29) | 0.16 ± 0.05 (0.09–0.26) | 0.698 |
| GP2 | 1.22 ± 0.61 (0.23–2.06) | 1.15 ± 0.51 (0.26–1.91) | 0.146 |
| GP3 | 0.13 ± 0.02 (0.11–0.17) | 0.14 ± 0.02 (0.1–0.17) | 0.620 |
| GP4 | 31.05 ± 6.46 (22.45–46.8) | 30.45 ± 6.74 (22.52–45.05) | 0.945 |
| GP5 | 0.17 ± 0.03 (0.13–0.26) | 0.18 ± 0.03 (0.14–0.27) | 0.171 |
| GP6 | 7.43 ± 1.47 (4.26–10.88) | 7.68 ± 1.62 (4.29–10.53) | 0.049 |
| GP7 | 0.52 ± 0.21 (0.12–0.77) | 0.51 ± 0.19 (0.15–0.79) | 0.514 |
| GP8 | 17.39 ± 1.98 (13.2–20.59) | 17.66 ± 2.2 (13.4–20.54) | 0.980 |
| GP9 | 9.41 ± 1.69 (7.19–14.29) | 9.06 ± 1.97 (7.11–14.55) | 0.105 |
| GP10 | 4.89 ± 0.99 (4.08–7.73) | 5.3 ± 1.23 (4.02–7.6) | 0.158 |
| GP11 | 0.71 ± 0.11 (0.53–0.99) | 0.73 ± 0.12 (0.53–0.98) | 0.045 |
| GP12 | 0.72 ± 0.33 (0.16–1.2) | 0.72 ± 0.32 (0.18–1.18) | 0.562 |
| GP13 | 0.28 ± 0.06 (0.18–0.43) | 0.28 ± 0.06 (0.18–0.42) | 0.541 |
| GP14 | 8.96 ± 2.58 (3.78–13.55) | 9.28 ± 2.76 (4.01–13.61) | 0.928 |
| GP15 | 1.45 ± 0.26 (1.03–2.08) | 1.5 ± 0.28 (1.11–1.94) | 0.576 |
| GP16 | 3.01 ± 0.57 (2.27–4.19) | 2.85 ± 0.58 (2.25–4.04) | 0.152 |
| GP17 | 0.95 ± 0.17 (0.67–1.21) | 0.94 ± 0.18 (0.68–1.31) | 0.975 |
| GP18 | 5.96 ± 1.38 (3.15–8.54) | 6 ± 1.52 (3.01–8.26) | 0.895 |
| GP19 | 1.82 ± 0.34 (1.25–2.38) | 1.75 ± 0.28 (1.25–2.16) | 0.232 |
| GP20 | 0.31 ± 0.06 (0.22–0.41) | 0.33 ± 0.1 (0.2–0.48) | 0.664 |
| GP21 | 0.45 ± 0.07 (0.32–0.55) | 0.47 ± 0.18 (0.24–0.94) | 0.675 |
| GP22 | 0.15 ± 0.04 (0.1–0.2) | 0.15 ± 0.04 (0.1–0.22) | 0.943 |
| GP23 | 1.17 ± 0.35 (0.57–1.77) | 1.07 ± 0.37 (0.53–1.78) | 0.015 |
| GP24 | 1.71 ± 0.4 (1.04–2.33) | 1.63 ± 0.36 (1.01–2.35) | 0.501 |
| Cut-off | n (Improvements) | n (Deteriorations) | Chi-Square for Randomness |
|---|---|---|---|
| 0.07 | 175 | 37 | 2.60 × 10−21 |
| 0.15 | 123 | 13 | 4.01 × 10−21 |
| 0.20 | 77 | 8 | 7.20 × 10−14 |
| 0.25 | 57 | 6 | 1.32 × 10−10 |
| 0.30 | 45 | 4 | 4.71 × 10−9 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hudetz, D.; Borić, I.; Rod, E.; Jeleč, Ž.; Radić, A.; Vrdoljak, T.; Skelin, A.; Lauc, G.; Trbojević-Akmačić, I.; Plečko, M.; et al. The Effect of Intra-articular Injection of Autologous Microfragmented Fat Tissue on Proteoglycan Synthesis in Patients with Knee Osteoarthritis. Genes 2017, 8, 270. https://0-doi-org.brum.beds.ac.uk/10.3390/genes8100270
Hudetz D, Borić I, Rod E, Jeleč Ž, Radić A, Vrdoljak T, Skelin A, Lauc G, Trbojević-Akmačić I, Plečko M, et al. The Effect of Intra-articular Injection of Autologous Microfragmented Fat Tissue on Proteoglycan Synthesis in Patients with Knee Osteoarthritis. Genes. 2017; 8(10):270. https://0-doi-org.brum.beds.ac.uk/10.3390/genes8100270
Chicago/Turabian StyleHudetz, Damir, Igor Borić, Eduard Rod, Željko Jeleč, Andrej Radić, Trpimir Vrdoljak, Andrea Skelin, Gordan Lauc, Irena Trbojević-Akmačić, Mihovil Plečko, and et al. 2017. "The Effect of Intra-articular Injection of Autologous Microfragmented Fat Tissue on Proteoglycan Synthesis in Patients with Knee Osteoarthritis" Genes 8, no. 10: 270. https://0-doi-org.brum.beds.ac.uk/10.3390/genes8100270






